03/07/2015
Fibrinogène avec le TXA ?: Plutôt oui
Association of Cryoprecipitate and Tranexamic Acid With Improved Survival Following Wartime Injury: Findings From the MATTERs II Study
Morrison JJ et Al. JAMA Surg. 2013;148(3):218-225.
Objective To quantify the impact of fibrinogen-containing cryoprecipitate in addition to the antifibrinolytic tranexamic acid on survival in combat injured.
Design Retrospective observational study comparing the mortality of 4 groups: tranexamic acid only, cryoprecipitate only, tranexamic acid and cryoprecipitate, and neither tranexamic acid nor cryoprecipitate. To balance comparisons, propensity scores were developed and added as covariates to logistic regression models predicting mortality.
Setting A Role 3 Combat Surgical Hospital in southern Afghanistan.
Patients A total of 1332 patients were identified from prospectively collected UK and US trauma registries who required 1 U or more of packed red blood cells and composed the following groups: tranexamic acid (n = 148), cryoprecipitate (n = 168), tranexamic acid/cryoprecipitate (n = 258), and no tranexamic acid/cryoprecipitate (n = 758).
Main Outcome Measure In-hospital mortality.
Results Injury Severity Scores were highest in the cryoprecipitate (mean [SD], 28.3 [15.7]) and tranexamic acid/cryoprecipitate (mean [SD], 26 [14.9]) groups compared with the tranexamic acid (mean [SD], 23.0 [19.2]) and no tranexamic acid/cryoprecipitate (mean [SD], 21.2 [18.5]) (P < .001) groups. Despite greater Injury Severity Scores and packed red blood cell requirements, mortality was lowest in the tranexamic acid/cryoprecipitate (11.6%) and tranexamic acid (18.2%) groups compared with the cryoprecipitate (21.4%) and no tranexamic acid/cryoprecipitate (23.6%) groups. Tranexamic acid and cryoprecipitate were independently associated with a similarly reduced mortality (odds ratio, 0.61; 95% CI, 0.42-0.89; P = .01 and odds ratio, 0.61; 95% CI, 0.40-0.94; P = .02, respectively). The combined tranexamic acid and cryoprecipitate effect vs neither in a synergy model had an odds ratio of 0.34 (95% CI, 0.20-0.58; P < .001), reflecting nonsignificant interaction (P = .21).
Conclusions Cryoprecipitate may independently add to the survival benefit of tranexamic acid in the seriously injured requiring transfusion. Additional study is necessary to define the role of fibrinogen in resuscitation from hemorrhagic shock.
| Tags : coagulopathie
21/06/2015
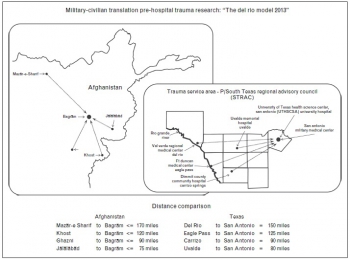
Military Trauma System: Pour le civil ?
Military trauma system in Afghanistan: lessons for civil systems?
Bailey JA et Al. Curr Opin Crit Care. 2013 Dec;19(6):569-77
PURPOSE OF REVIEW:
This review focuses on development and maturation of the tactical evacuation and en route care capabilities of the military trauma system in Afghanistan and discusses hard-learned lessons that may have enduring relevance to civilian trauma systems.
RECENT FINDINGS:
Implementation of an evidence-based, data-driven performance improvement programme in the tactical evacuation and en route care elements of the military trauma system in Afghanistan has delivered measured improvements in casualty care outcomes.
SUMMARY:
Transfer of the lessons learned in the military trauma system operating in Afghanistan to civilian trauma systems with a comparable burden of prolonged evacuation times may be realized in improved patient outcomes in these systems.
Un nouveau concept de triage ?
Medical evacuation and triage of combat casualties in Helmand Province, Afghanistan: October 2010-April 2011
Clarke JE et Al. Mil Med. 2012 Nov;177(11):1261-6
--------------------------------------------------------------------
Un article de synthèse sur l'organisation de la chaîne de prise en charge des blessés par nos confrères anglais, avec notamment l'emploi d'une évolution majeure pour le un système anglo-saxon (lire ce document): le recours à des EVASAN médicalisées par des personnels ayant une pratique régulière de la prise en charge de patients en état critique. Cet article est intéressant car il insiste sur l'importance du triage et le rôe prééminent que peuvent jouer les role 2 notamment si les élongations sont importantes.
--------------------------------------------------------------------
Medical evacuation of combat casualties in Operation Enduring Freedom-Afghanistan is achieved primarily by helicopter, because of distances involved as well as ground-based threats. In Helmand Province, evacuation from the point of injury may occur on a variety of helicopter evacuation platforms with disparate levels of attendant medical expertise. Furthermore, triage to a medical treatment facility may involve varying echelons of care before definitive management. Consequently, considerable differences in medical care may be encountered between point of injury and definitive treatment. We discuss the role of helicopter-based medical evacuation in Helmand, Afghanistan, as well as triage and timelines to the most appropriate medical facilities. Based on our experience and available evidence, we have made recommendations to regional commanders which favor the utilization of prehospital critical care teams aboard helicopter-based evacuation platforms and direct triage to the highest echelon of care available when feasible
06/06/2015
Prise en charge d'un blessé: Ce n'est pas le SAMU, ni la catastrophe
Tactical medicine: a joint forces field algorithm.
Waldman M et Al. Mil Med. 2014 Oct;179(10):1056-61
20/03/2015
Guidelines for field management of combat related head trauma
07/03/2015
Mise en place du TCCC: Le point 2014
| Tags : tccc
06/03/2015
Mise en place du TCCC: Le point 2013
| Tags : tccc
27/02/2015
Plaies par armes blanches
23/02/2015
Pneumo suffocant: Oui
Clic sur l'image pour accéder au document
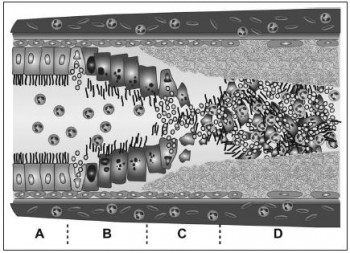
Pneumothorax compressif, sous tension, tamponnade gazeuse. Autant de termes utilisés pour cette situation clinique à laquelle est souvent associé l'existence d'une hypotension artérielle, en fait surtout présente chez les patients ventilés. La détresse respiratoire est souvent au premier plan che le blessé non ventilé et le terme de pneumothorax suffocant adapté. Le document proposé est un peu ancien mais apporte une vision relativement didactique de la problématique séméiologique et physiopathologique.
| Tags : pneumothorax
13/01/2015
Attentats: Importance du garrot
The Initial Response to the Boston Marathon Bombing. Lessons Learned to Prepare for the Next Disaster
Gates JD et AL. Ann Surg. 2014 Dec;260(6):960-6
-----------------------------------------------------------------------------------
Le concept du garrot tactique est familier aux équipes militaires. L'expérience rapportée montre que ce concept doit également le devenir dans le monde de la médecine préhospitalière. 26 soit près de 10% blessés pris en charge ont fait l'objet d'une pose de garrot. Ainsi en cas d'attentat la pose précoce d'un garrot en cas d'hémorragie des membres est elle une mesure fondamentale de mise en condition de survie.
-----------------------------------------------------------------------------------
OBJECTIVE:
We discuss the strengths of the medical response to the Boston Marathon bombings that led to the excellent outcomes. Potential shortcomings were recognized, and lessons learned will provide a foundation for further improvements applicable to all institutions.
BACKGROUND:
Multiple casualty incidents from natural or man-made incidents remain a constant global threat. Adequate preparation and the appropriate alignment of resources with immediate needs remain the key to optimal outcomes.
METHODS:
A collaborative effort among Boston's trauma centers (2 level I adult, 3 combined level I adult/pediatric, 1 freestanding level I pediatric) examined the details and outcomes of the initial response. Each center entered its respective data into a central database (REDCap), and the data were analyzed to determine various prehospital and early in-hospital clinical and logistical parameters that collectively define the citywide medical response to the terrorist attack.
RESULTS:
A total of 281 people were injured, and 127 patients received care at the participating trauma centers on that day. There were 3 (1%) immediate fatalities at the scene and no in-hospital mortality. A majority of the patients admitted (66.6%) suffered lower extremity soft tissue and bony injuries, and 31 had evidence for exsanguinating hemorrhage, with field tourniquets in place in 26 patients. Of the 75 patients admitted, 54 underwent urgent surgical intervention and 12 (22%) underwent amputation of a lower extremity.
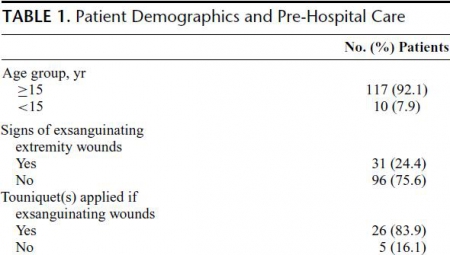
CONCLUSIONS:
Adequate preparation, rapid logistical response, short transport times, immediate access to operating rooms, methodical multidisciplinary care delivery, and good fortune contributed to excellent outcomes.
| Tags : tourniquet, garrot, hémorragie
12/12/2014
HEA: Possible pour les trauma ouverts
Differences between blunt and penetrating trauma after resuscitation with hydroxyethyl starch
Casey JA et Al. J Trauma Acute Care Surg. 2014;77: 859-864
----------------------------------------------------------------
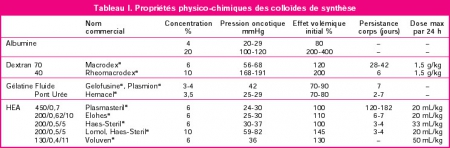
Ce travail effectué avec un HEA ancien (450/07: Hetastarch®, Hextent®) suggère que l'emploi des HEA lors de la prise en charge de trauma ouvert n'est pas associé à un risque accru de décès ou d'insuffisance rénale. On rappelle qu'il ne s'agit pas de la même classe d'HEA que celle que nous avons l'habitude d'utiliser (130/0.4: Voluven)
 ----------------------------------------------------------------
----------------------------------------------------------------
BACKGROUND: The purpose of this study was to test the hypothesis that a single bolus of 6% hydroxyethyl starch (HES 450/0.7 in lactated electrolyte injection) during initial resuscitation has a differential effect in blunt and penetrating trauma patients.
METHODS: Consecutive admissions to the trauma service were reviewed. Patients who died within 24 hours were excluded. Multivariate analysis defined individual predictors for the primary outcomes, acute kidney injury (AKI) and mortality within 90 days. Data were expressed as mean T SD, and significance was assessed at p G 0.05.
RESULTS: Therewere 1,410 patients (76% male; mean T SD, age 43 T 18 years; 68% blunt trauma; mean T SD Injury Severity Score [ISS] 14 T 11; AKI, 4.4%; and mortality, 3.4%). HES (0.5-1.5 L) was administered to 216 patients (15.3%). After multiple logistic regression, HES remained a significant independent predictor of AKI after blunt trauma (odds ratio [OR], 2.54; 95% confidence interval [CI], 1.24-5.19; area under the receiver operating characteristic curve [AUROC], 0.809) but not penetrating
trauma (OR, 0.90; 95% CI, 0.23-3.60; AUROC, 0.849). In separate logistic regression models, HES was a significant predictor of mortality after blunt trauma (OR, 3.77; 95% CI, 0.91-0.97; AUROC, 0.921) but not penetrating trauma (OR, 0.72; 95% CI, 0.13-3.94; AUROC, 0.904).
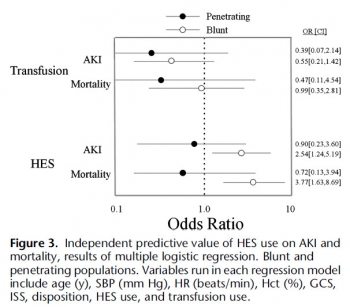
CONCLUSION: HES is an independent risk factor for AKI and death after blunt, but not penetrating, trauma, which underscores a fundamental difference between these two injury types.
| Tags : remplissage
Prehospital management of chest injuries
The prehospital management of chest injuries: a consensus statement. Faculty of Pre-hospital Care, Royal College of Surgeons of Edinburgh
Lee C. et AL. Emerg Med J 2007;24:220–224
---------------------------------------------------------------------------
Un document un peu ancien des nos confrères britanniques mais qui reste d'actualité.
---------------------------------------------------------------------------
This paper provides a guideline for the management of prehospital chest injuries after a consensus meeting held by the
Faculty of Prehospital Care, Royal College of Surgeons of Edinburgh, Edinburgh, UK, in January 2005. An overview of
the prehospital assessment, diagnosis and interventions for life threatening chest injury are discussed, with the application of
skills depending on the training, experience and competence of the individual practitioner
| Tags : thorax
30/11/2014
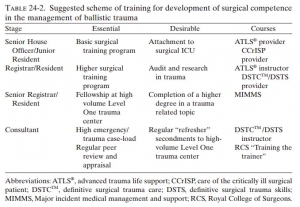
ATLS ? Peut être mais pas pour les seniors !
Training to Manage Ballistic Trauma
Boffard KG et Al. in Ballistic Trauma A Practical Guide
La prise en charge d'un polytraumatisé nécessite une approche très structurée et coordonnée qui fait intervenir de multiples professionnels de la médecine d'urgence. L'ATLS est un cours qui fait référence en matière de traumatologie notamment dans les pays anglo-saxons. Son apport réel est discuté notamment dans les pays qui bénéficie d'un environnement hospitalier conséquent (1, 2). L'intérêt réel de cette formation est en train de se repositionner notamment du fait de nouveaux concepts de prise en charge et l'apparition des formation en équipe par simulation en mode immersif. Le document proposé fait le point sur les démarches actuelles de formation à un tel type de prise en charge. Il présente l'ATLS comme une formation plutôt destinée aux plus jeunes, l'expertise nécessaire tant individuelle que collective devant faire appel des des enseignements beaucoup plus conséquents.
Clic sur l'image pour accéder au document
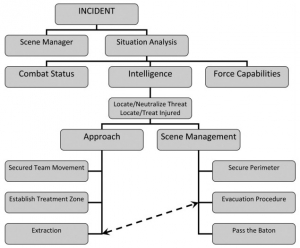
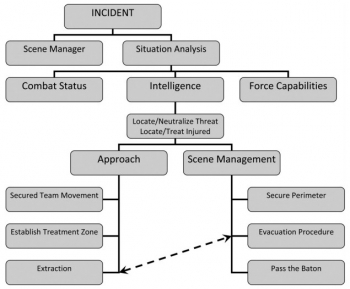
Soutien médical des interventions à risque
Tactical Medicine: A Joint Forces Field Algorithm
Waldman M et Al. Military Medicine, 179, 10:1056, 2014
Les forces de l'ordre interviennent de plus en plus dans un contexte de violence extrême qui impose la planification du soutien médical de ces opérations selon des principes militaires. Une telle approche est fait par les équipes israélienne. Le document proposé détaille l'algorithme proposé ci dessous.
clic sur l'image pour accéder au document
17/11/2014
Pneumothorax et vol en altitude : Possible ?
Cleared for takeoff: The effects of hypobaric conditions on traumatic pneumothoraces
Majercik S. et All. J Trauma Acute Care Surg. 2014;77: 729-733
| Tags : pneumothorax
12/06/2014
Traumatisé de guerre: Cela évolue
Systematic review of the prevalence and characteristics of battle casualties from NATO coalition forces in Iraq and Afghanistan
Hoencamp R. et All. Injury, Int. J. Care Injured 45 (2014) 1028–1034
13/05/2014
Lésions rachidiennes: Plus fréquentes qu'envisagé
Spinal Injuries in United States Military Personnel Deployed to Iraq and Afghanistan
An Epidemiological Investigation Involving 7877 Combat Casualties From 2005 to 2009
Schoenfeld AJ et All. Spine 2013;38:1770–1778
Les lésions du rachis sont plus fréquentes que ce qui était supposé. Ce travail rapporte qu'une atteinte du rachis est présente dans 11% des cas. Une des explications est que l'amélioration des conditions de prise en charge permet la survie de blessés plus graves qu'auparavant, qui autrefois ne survivait pas à leurs blessures.
-----------------------------------------------------------
In the years 2005 to 2009, 872 (11.1%) casualties with spine injuries were identified among a total of 7877 combat wounded. The mean age of spine casualties was 26.6 years. Spine fractures were the most common injury morphology, comprising 83% of all spinal wounds. The incidence of combat-related spinal trauma was 4.4 per 10,000, whereas that of spine fractures was 4.0 per 10,000. Spinal cord injuries occurred at a rate of 4.0 per 100,000.
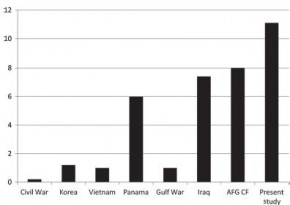
Spinal cord injuries were most likely to occur in Afghanistan (incident rate ratio: 1.96; 95% confi dence interval: 1.68–2.28), among Army personnel (incident rate ratio: 16.85; 95% confidence interval: 8.39–33.84), and in the year 2007 (incident rate ratio: 1.90; 95% confi dence interval: 1.55–2.32). Spinal injuries from gunshot were significantly more likely to occur in Iraq (17%) than in Afghanistan (10%, P = 0.02).
-----------------------------------------------------------
| Tags : rachis
10/02/2014
Inhalation de fumées: Héparine en aérosol ?
Inhaled Anticoagulation Regimens for the Treatment of Smoke Inhalation–Associated Acute Lung Injury: A Systematic Review*
Miller AC et Al. Crit Care Med 2014; 42:413–419
----------------------------------------------------------------------------------------------
L'inhalation de fumées est fréquentes lors de la prise en charge de victilmes par explosion. Laprise en charge de brNébiliser 5000 à 1000U d'héparine inhalé avec 3ml de NacétylCystéine et de l'albuterol améliorerait la survie
----------------------------------------------------------------------------------------------
OBJECTIVE:
Inhaled anticoagulation regimens are increasingly being used to manage smoke inhalation-associated acute lung injury. We systematically reviewed published and unpublished preclinical and clinical trial data to elucidate the effects of these regimens on lung injury severity, airway obstruction, ventilation, oxygenation, pulmonary infections, bleeding complications, and survival.
DATA SOURCES:
PubMed, Scopus, EMBASE, and Web of Science were searched to identify relevant published studies. Relevant unpublished studies were identified by searching the Australian and New Zealand Clinical Trials Registry, World Health Organization International Clinical Trials Registry Platform, Cochrane Library, ClinicalTrials.gov, MINDCULL.com, Current Controlled Trials, and Google.
STUDY SELECTION:
Inclusion criteria were any preclinical or clinical study in which 1) animals or subjects experienced smoke inhalation exposure, 2) they were treated with nebulized or aerosolized anticoagulation regimens, including heparin, heparinoids, antithrombins, or fibrinolytics (e.g., tissue plasminogen activator), 3) a control and/or sham group was described for preclinical studies, and 4) a concurrent or historical control group described for clinical studies. Exclusion criteria were 1) the absence of a group treated with a nebulized or aerosolized anticoagulation regimen, 2) the absence of a control or sham group, and 3) case reports.
DATA EXTRACTION:
Ninety-nine potentially relevant references were identified. Twenty-seven references met inclusion criteria including 19 preclinical references reporting 18 studies and eight clinical references reporting five clinical studies.
DATA SYNTHESIS:
A systematic review of the literature is provided. Both clinical and methodological diversity precluded combining these studies in a meta-analysis.
CONCLUSIONS:
The high mortality associated with smoke inhalation-associated acute lung injury results from airway damage, mucosal dysfunction, neutrophil infiltration, airway coagulopathy with cast formation, ventilation-perfusion mismatching with shunt, and barotrauma. Inhaled anticoagulation regimens in both preclinical and clinical studies improve survival and decrease morbidity without altering systemic markers of clotting and anticoagulation. In some preclinical and clinical studies, inhaled anticoagulants were associated with a favorable effect on survival. This approach appears sufficiently promising to merit a well-designed prospective study to validate its use in patients with severe smoke inhalation-associated acute lung injury requiring mechanical ventilation.
| Tags : brûlure
21/11/2013
Le plasma lyophilisé: Bon pour le cerveau du traumatisé qui saigne
Early treatment with lyophilized plasma protects the brain in a large animal model of combined traumatic brain injury and hemorrhagic shock
Imam AM et Al. J Trauma Acute Care Surg. 2013;75: 976-983
accéder aux abstracts de la WTA publiés dans J trauma Acute care
_____________________________________
Bien sûr une étude animale, mais une de plus qui milite pour un emploi précoce du plasma lyophylisé.
_____________________________________
BACKGROUND: Combination of traumatic brain injury (TBI) and hemorrhagic shock (HS) can result in significant morbidity and mortality. We have previously shown that early administration of fresh frozen plasma (FFP) in a large animal model of TBI and HS reduces the size of the brain lesion as well as the associated edema. However, FFP is a perishable product that is not well suited for use in the austere prehospital settings. In this study, we tested whether a shelf-stable, low-volume, lyophilized plasma (LSP) product was as effective as FFP.
METHODS:
Yorkshire swine (42-50 kg) were instrumented to measure hemodynamic parameters, intracranial pressure, and brain tissue oxygenation. A prototype, computerized, cortical impact device was used to create TBI through a 20-mm craniotomy: 15-mm cylindrical tipimpactor at 4 m/s velocity, 100-millisecond dwell time, and 12-mm penetration depth. Volume-controlled hemorrhage was induced(40-45% total blood volume) concurrent with the TBI. After 2 hours of shock, animals were treated with (1) normal saline (NS, n = 5), (2) FFP (n = 5), and (3) LSP (n = 5). The volume of FFP and LSP matched the shed blood volume, whereas NS was 3 times the volume. Six hours after resuscitation, brains were sectioned and stained with TTC (2, 3, 5-Triphenyltetrazolium chloride), and lesion size (mm3) and swelling (percent change in volume compared with the contralateral, uninjured side) were measured.
RESULTS:
This protocol resulted in a highly reproducible brain injury, with clinically relevant changes in blood pressure, cardiac output, tissue hypoperfusion, intracranial pressure, and brain tissue oxygenation. Compared with NS, treatment with LSP significantly ( p G 0.05) decreased brain lesion size and swelling (51% and 54%, respectively).
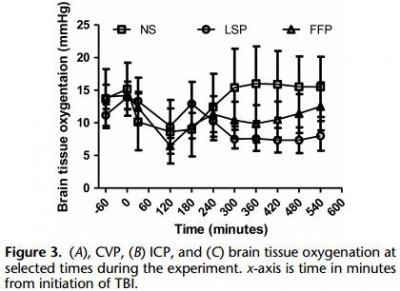
CONCLUSION: In a clinically realistic combined TBI + HS model, early administration of plasma products decreases brain lesion size and edema. LSP is as effective as FFP, while offering many logistic advantages.
| Tags : tbi, coagulopathie
07/09/2013
Blast des membres
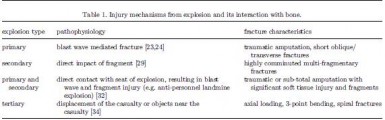
Blast-related fracture patterns: a forensic biomechanical approach
Ramasamy A. et All. J. R. Soc. Interface (2011) 8, 689–698
Dehors et dedans, ce n'est pas la même chose
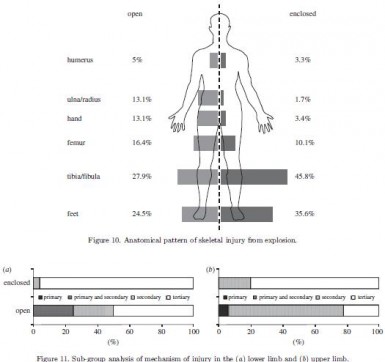
Les lésions dépendent du type de blast
| Tags : blast