12/11/2023
Revue des moyens d'hémostase des hémorragies non compressibles
Perspectives on the management of non-compressible torso hemorrhage: A narrative review
Leclerc S et Al. Journal of Military, Veteran and Family Health 8(s2) 2022: 73-36
Hemorrhage is one of the leading causes of death after trauma. A significant proportion of these fatalities could be prevented with appropriate bleeding control. This is more easily achieved with direct pressure in compressible areas such as the extremities or major joints. However, bleeding in the chest, abdomen, or pelvis cannot be as easily controlled without advanced procedures that are only available in hospitals. This article describes several technologies to control bleeding in the chest, abdomen, and pelvis that are potentially applicable in combat and pre-hospital settings. However, a review of existing studies quickly shows that convincing clinical evidence is lacking to support most pre-existing technologies, and the majority of studies are in the investigational stage. A universal, effective, and life-saving solution has not yet been identified. Accordingly, research in this area should continue to focus on both refining existing technologies and developing new approaches.
More than 50% of combat casualty deaths on the battlefield occur minutes to hours after a person has been wounded. Approximately 25% of those fatalities could potentially be prevented if rapid hemorrhage control or temporization were feasible. Despite several technologies to temporize non-compressible torso hemorrhage (NCTH), an ideal device and method have not yet been developed, particularly for Role 1 military medical treatment facilities and civilian pre-hospital settings. This article summarizes the devices and adjunct methods currently available to temporize NCTH when surgical and interventional radiology control are not readily accessible. New technologies under investigation are also discussed.
09/11/2023
Trop simplifier: Pas forcément bon, l'exemple de la ventilation
Comparison of Airway Control Methods and Ventilation Success With an Automatic Resuscitator
Rodriguez D. et Al. J Spec Oper Med. 2012; 12(2):65-70.
Mechanical ventilation in an austere environment is difficult owing to logistics, training, and environmental conditions. We evaluated the ability of professional caregivers to provide ventilatory support to a simulated patient using the Simplified Automated Ventilator (SAVe) with a mask hand attended ventilation, mask with single strap unattended ventilation, and supraglottic airway (King LT) ventilation.
All three methods were performed using a SAVe with a set tidal volume of 600 mL and respiratory rate of 10 breaths per minute. The simulator consisted of a head and upper torso with anatomically correct upper airway structures, trachea, esophagus, and lung that also measured the delivered tidal volume, respiratory rate, inspiratory flow, and airway pressures. Volunteers used each airway control method to provide ventilation for 10 minutes in random order. Success of each technique was judged as a mean delivered tidal volume of > 500 mL. The major finding of this study was that medical professionals using the SAVe resuscitator and the manufacturer-supplied face mask with single head strap failed to ventilate the airway model in every case
24/10/2023
Chirurgie à l'avant. L'histoire enseigne de petites structures proches des combats
Surgery on the battlefield: Mobile surgical units in the Second World War and the memoirs they produced
Venables KM J Med Biogr. 2023 Aug; 31(3): 202–211.
In the Second World War, there was a flowering of the battlefield surgery pioneered in the Spanish Civil War. There were small, mobile surgical units in all the theatres of the War, working close behind the fighting and deployed flexibly according to the nature of the conflict. With equipment transported by truck, jeep or mule, they operated in tents, bunkers and requisitioned buildings and carried out abdominal, thoracic, head and neck, and limb surgery. Their role was to save life and to ensure that wounded soldiers were stable for casualty evacuation back down the line to a base hospital.

There is a handful of memoirs by British doctors who worked in these units and they make enthralling reading. Casualty evacuation by air replaced the use of mobile surgical units in later wars, throwing into doubt their future relevance in the management of battle wounds. But recent re-evaluations by military planners suggest that their mobility still gives them a place, so the wartime memoirs may have more value than simply as war stories.
03/04/2023
Sang de banque sur pied: Mieux si on est entraîné
A prospective assessment of the medic autologous blood transfusion skills for field transfusion preparation
Steven G Schauer SG et Al. Transfusion. 2023 Mar 27. doi: 10.1111/trf.17325.
Background: Data demonstrate benefit from blood product administration near point-of-injury (POI). Fresh whole blood transfusion from a pre-screened donor provides a source of blood at the POI when resources are constrained. We captured transfusion skills data for medics performing autologous blood transfusion training.
Methods: We conducted a prospective, observational study of medics with varying levels of experience. Inexperienced medics were those with minimal or no reported experience learning the autologous transfusion procedures, versus reported experience among special operations medics. When available, medics were debriefed after the procedure for qualitative feedback. We followed them up to 7 days for adverse events.
Results: The median number of attempts for inexperienced and experienced medics was 1 versus 1 (interquartile range 1-1 for both, p=0.260). The inexperienced medics had a slower median time to needle venipuncture access for donation of 7.3 versus 1.5 minutes, needle removal after clamping time of 0.3 versus 0.2 minutes, time to bag preparation of 1.9 versus 1.0 minutes, time to IV access for reinfusion of 6.0 versus 3.0 minutes, time to transfusion completion of 17.3 versus 11.0 minutes, and time to IV removal of 0.9 versus 0.3 minutes (all p<0.05). We noted one administrative safety event in which allogeneic transfusion occurred. No major adverse events occurred. Qualitative data saturated around the need for quarterly training.
Conclusions: Inexperienced medics have longer procedure times when training autologous whole blood transfusion skills. This data will help establish training measures of performance for skills optimization when learning this procedure.
01/04/2023
Trauma des voies aériennes
Blunt and Penetrating Airway Trauma
Duggan LV et Al.. Emerg Med Clin North Am. 2023 Feb;41(1S):e1-e15.
-----------------------------
C'est une chose compliquée, pas simple surtout en condition de combat et qui justifie la maîtrise d'un abord chirurgical du cou. Ce document est, je trouve, excellent.
-----------------------------
Airway injury, be that penetrating or blunt, is a high-stakes high-stress management challenge for any airway manager and their team. Penetrating and blunt airway injury vary in injury patterns requiring prepracticed skills and protocols coordinating care between specialties. Variables including patient cooperation, coexisting injuries, cardiorespiratory stability, care location (remote vs tertiary care center), and anticipated course of airway injury (eg, oxygenating well and comfortable vs increasing subcutaneous emphysema) all play a role in determining airway if and when airway management is required. Direct airway trauma is relatively infrequent, but its presence should be accompanied by in-person or virtual otolaryngology support.
| Tags : airway
16/02/2023
Guerre hybrides: Le système sanitaire, une cible
Russia's Hybrid Warfare in Ukraine Threatens Both Healthcare & Health Protections Provided by International Law
Baker MS et Al., Ann Glob Health. 2023 Jan 23;89(1):3.
Hybrid Warfare is on display because of the unjustified Russian invasion of Ukraine. This is characterized by numerous crimes against civilians as seen vividly during the occupation of the town of Bucha where rape, torture, murder, and looting seem to reflect Russian military policy, leadership, and command guidance. Of particular concern is the threat to hospitals and health care as well as vital life support. Numerous hospitals have been damaged and destroyed. Hospitals are not tactical military targets and targeting health care facilities and personnel ignores traditional jus in bello and ignores numerous conventions established to stabilize the global order. The Russian-proclaimed "special operation" in Ukraine has been characterized by barbarian warfare in which the Russian military uses weapons against the civilian population and civilian infrastructure. The aggressors have embarked on a purposeful terror campaign through infrastructure attacks, which are of little military value except to demoralize the nation's people. This is evident with Russian missile and drone attacks on electric, water, and health care in Ukraine. Warfare now and in the future may be increasingly aimed at demoralizing civilian populations and reducing the will of the people and their government to resist. The Ukrainian invasion clearly shows that this use of hybrid warfare should be met with a strong reaction of the international community at the earliest possible stage, especially the supposedly peace-loving neutral countries, or else the future is expanded unlawful and barbaric military conflict.
Guerre Hybride: Position du problème
Hybrid warfare and counter-terrorism medicine
Derrick Tin D et Al.. Eur J Trauma Emerg Surg. 2023 Feb 10;1-5.
Introduction:
March 9, 2022. An airstrike by Russian forces destroying a maternity hospital in Mariupol, Ukraine. The image of a severely injured pregnant woman covered in blood being stretchered away against the backdrop of destroyed buildings. Mutterings of the use of chemical weapons. This paper is a primer for healthcare personnel and health systems on hybrid warfare and counter-terrorism medicine.
Discussion:
While recent events and images arising from conflicts around the world represent a cruel hallmark in today's history, attacks against healthcare facilities and innocent civilians are not new and continue to be perpetrated around the world. In war, the Geneva Convention protects civilians and healthcare institutions from harm but when war crimes are being committed and civilians knowingly targeted, parallels from a healthcare perspective can be drawn with terrorism events. Increasingly, civilian institutions and in particular the healthcare sector, are drawn into such conflicts and understanding the health system impact of hybrid warfare and other asymmetrical attack methods is of great importance.
Conclusion:
The field of Counter-Terrorism Medicine (CTM) explores the healthcare impacts of intentional, man-made attacks and much recent research and discussions around this topic are extremely relevant and applicable not just to the ongoing hybrid war in Ukraine, but to today's threat climate all around us.
19/01/2023
Le drone: Incontournable !
Drones reduce the treatment-free interval in search and rescue operations with telemedical support – A randomized control trial
Van Veelen MJ et Al. https://doi.org/10.1016/j.ajem.2023.01.020
------------------------------------
Un outil sans nul doute à maîtriser à la lumière des événements ukrainiens
------------------------------------
Introduction
Response to medical incidents in mountainous areas is delayed due to the remote and challenging terrain. Drones could assist in a quicker search for patients and can facilitate earlier treatment through delivery of medical equipment. We aim to assess the effects of drone deployment in search and rescue (SAR) operations in challenging terrain. We hypothesize that drones can reduce the search time and treatment-free interval of patients through initiation of telemedicine in a single mission.
Methods
In this randomized control trial with a cross-over design two methods of searching for and initiating treatment of a patient were compared. The primary outcome was a comparison of the times for locating a patient through visual contact and starting treatment on-site between the drone assisted intervention arm and the conventional ground rescue control arm. A linear mixed model (LMM) was used to evaluate the effect of using a drone on search and start of treatment times.
Results
Twenty-four SAR missions, performed by six SAR teams each with four team members, were analyzed. The mean time to locate the patient was 14.6 min (95% CI 11.3–17.9) in the drone assisted intervention arm and 20.6 min (95% CI 17.3–23.9) in the control arm. The mean time to start treatment was 15.7 min (95% CI 12.4–19.0) in the drone assisted arm and 22.4 min (95% CI 19.1–25.7) in the control arm ( p < 0.01 for both comparisons).

Conclusion
Drone deployment in SAR operations leads to a reduction in search time and treatment-free interval of patients in challenging terrain, which could improve outcomes in patients suffering from traumatic injuries, the most commonly occurring incident requiring mountain rescue deployment.
| Tags : drone
14/11/2022
Plaidoyer AUSSIE pour + de technicité à l'avant
Treatment at point of injury—A proposal for an enhanced combat first aider and health technician skillset
Pilgrim C. et Al. JMVH 2022, oncline first
Management of trauma in the future operating environment might be significantly different from the recent experience in the Middle East Region if it were to occur in the context of hostilities between coalition, including Australian forces and a near-peer or peer-level threat. Specifically, reliance on rotary-wing aeromedical evacuation may be compromised if air superiority is degraded or denied.
Two alternative approaches may be considered in the context of constrained evacuation capability. First, enhanced treatment of the injured soldier on the ground at or near the point of injury by first responders may broaden the window during which a patient may survive on the battlefield awaiting evacuation. Alternatively, moving the surgical resources to the casualty may also improve the chances of survival for an injured soldier. However, this comes at the cost of risking higher-level assets. The first of these approaches is considered here with an exploration of what life-saving interventions (LSI) can be delivered by first responder soldiers. Numerically dropping as a result of tactical combat casualty care principles but persisting as causes of preventable battlefield death, exsanguinating extremity haemorrhage, tension pneumothorax and airway obstruction are areas where future gains may be possible with an expanded skillset deliverable by combat first aiders and health technicians.
Earlier administration of blood products by health technicians to casualties with exsanguinating haemorrhage would align military trauma management principles with the civilian world, where blood products can now be administered en route by trained paramedics. Similarly, there is a shift towards managing tension pneumothorax with finger thoracostomy in preference to needle decompression in the hospital and pre-hospital environment in the civilian sector.
Of much greater complexity, management of non-compressible truncal haemorrhage remains problematic on the battlefield. A highly specialised intervention with significant haemodynamic consequences that nevertheless has been shown to be achievable in both military and civilian contexts is REBOA (resuscitative endovascular balloon occlusion of the aorta). This technique is encumbered with a significant training burden but warrants discussion and is most relevant when evacuation times are expected to fall between 1 and 6 hours. Expanding the skillset deliverable by combat first aiders and health technicians may offset delays in evacuation and maintain battlefield casualty survival in the future operating environment and may be obtained leveraging existing Defence training programs.
12/11/2022
Triage: Encore + d'expertise à l'avant
JTS Analyzes Search and Rescue After Action Reports to Uncover Deficiencies,
Develops Performance Improvement Metrics
https://prolongedfieldcare.org/2022/03/18/joint-trauma-system-newsletter-update/
The JTS PI and CTS Operations branches published in-depth review of after action reports (AARs) from over 252 search and rescue (SAR) missions from 2018 - 2021. The report is in response to the U.S. Navy SAR’s request that JTS assess its operations. It analyzes the context in which Naval SAR operations oc- curred as well as medical procedures and patient demographics. JTS identified deficiencies in equipment, personnel, and documentation and developed a list of PI metrics. The need for standardization is keenly felt in the field. AAR comments reinforce the need for standardized equipment like cardiac kits, medication kits, and advanced life support tools. For example, SAR crews report they do not have the equipment or skills to perform rapid intubation of patients. The report was unable to conclude whether or not standardized medication kits are available to SAR teams. The report did find skills of attendant medical personal vary considerably across SAR missions. Thirty-one percent of missions were executed by a single EMT-B, while 19% were executed by a single EMP-P, and 17% were executed by two medical attendants. In some cases, both a registered nurse and physician were present, while other times only one was pre- sent.
JTS identified opportunities for improving documentation. Vague or incomplete information in the after action reports makes it more difficult to conduct accurate assessments. Accurate information is critical for mission success. Casualty classification was one area of deficiency. The report found that there is only an 81% overall accuracy in the SAR Rescuer Skill Type
casualty classification. This puts casualty classification high on the list of performance improvement (PI) priorities. Casualty classification includes all the critical information of the patient, most notably the type and severity of injury and location of the patient. It is imperative that patients are accurately classified at the start of the mission, since this determines everything from prioritizing patient care to the medical and logistical resources. A key metric for success is the comparison between the dispatched category and the assessed category of the casualty. Dispatch’s casualty classification should match the classification assessed upon the arrival at the mission destination. Having accurate information upfront is critical for SAR teams to accurately triage the casualty in advance, which dictates urgency, timing, equipment, and all other areas of mission prep. Inconsistent SAR documentation impacts the ability for SAR teams to record accurate information. For example, the DA4700 form has a list of specific mechanisms of injury (MOI), which are tailored towards battlefield en route care and not necessarily applicable to SAR operations. JTS reported roughly one fifth (55 out of 252 cases) of SAR cases recorded the MOI as either “other” or left blank. “Other” or left unchecked ultimately makes the data less useful and harder to interpret. In cases of hypothermia, the patient’s temperature was only recorded in 13% of cases. An emphasis on documentation training may
fill the gaps in SAR documentation.
The situation is further complicated by the fragmented nature of the available guidance for SAR teams. JTS discovered SAR teams rely on guidelines from multiple sources, bringing into question source credibility and guidance consistency.
The lack of training is at the root of the deficiencies. Additionally, actual mission engagements do not provide for redundancy which would lead to proficiency, proving that personnel training is of paramount importance. For instance, in one exercise, Special Operations assets had to be utilized for Casualty Evacuation (CASEVAC) purposes because the CASEVAC plan proved insufficient during the course of the exercise. The AARs recommended regular testing and evaluation of CASEVAC plans.
Response to the JTS SAR report has been positive and supportive. LCDR Paul Roszko, Director of Emergency Medical Services, Navy Medical Forces, called the report “excellent” and viewed the findings as an opportunity to improve trauma training across the Services. The report prompted Rosko to question why there is not standardized casualty cards or simulations. He would like to take real-life cases and turn them into vignettes or simulations for squadron training. JTS does include an example of a SAR casualty vignette as a tool to improve SAR training. “The data is clear that the SAR community does a lot more than just treat trauma patients,” said Rozko. “Perhaps identifying a few common medical cases or other types of commonly encountered injuries and specifying what our "standard of care" reference point is would allow the JTS PI team to provide more feedback on the quality of care provided.”
23/10/2022
Drone: Pour quoi faire ?
| Tags : drone
21/10/2022
Plyo intraosseux ? Pas si simple
Intraosseous administration of freeze-dried plasma in the prehospital setting
Rittblat M et Al. Isr Med Assoc J. 2022 Sep;24(9):591-595.
Background:
Freeze dried plasma (FDP) is a commonly used replacement fluid in the prehospital setting when blood products are unavailable. It is normally administered via a peripheral intravenous (PIV) line. However, in severe casualties, when establishing a PIV is difficult, administration via intraosseous vascular access is a practical alternative, particularly under field conditions.
Objectives:
To evaluate the indications and success rate of intraosseous administration of FDP in casualties treated by the Israel Defense Forces (IDF).
Methods:
A retrospective analysis of data from the IDF-Trauma Registry was conducted. It included all casualties treated with FDP via intraosseous from 2013 to 2019 with additional data on the technical aspects of deployment collected from the caregivers of each case.
Results:
Of 7223 casualties treated during the study period, intravascular access was attempted in 1744; intraosseous in 87 of those. FDP via intraosseous was attempted in 15 (0.86% of all casualties requiring intravascular access). The complication rate was 73% (11/15 of casualties).
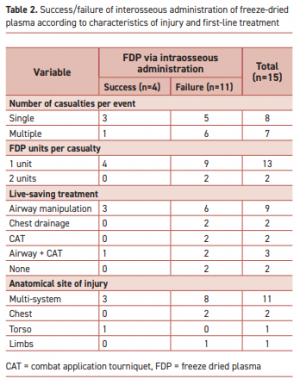
"According to the manufacturer’s specifications, the reconstituted lyophilized plasma product is delivered from a glass bottle with the rate of infusion determined primarily by gravity. This procedure precludes the care providers from applying external pressure to increase the plasma infusion rate. Therefore, the pressure gradient is determined primarily by gravity with respect to height of the bottle."
Complications were more frequent when the event included multiple casualties or when the injury included multiple organs. Of the 11 failed attempts, 5 were reported as due to slow flow of the FDP through the intraosseous apparatus. Complications in the remaining six were associated with deployment of the intraosseous device.
Conclusions:
Administration of FDP via intraosseous access in the field requires a high skill level.
| Tags : intraosseux
16/09/2022
La chirurgie: Encore plus à l'avant
Treatment at Point of Injury. Forward movement of surgical assets to address non compressible truncal haemorrhage
Pilgrim CHC et Al. JMVH 2022, 30: 41-50.
-----------------------------------------------------
C'est la chirurgie qui va sauver les blessés du tronc. Encore faut il que ces blessés soient pris en charge par une équipe chirurgicale. D'où le principe de constituer de petites équipes chirurgicales mettant en oeuvre des techniques choisies et limitées dans un environnement très austère au plus près des combats. C'est le principe du module de chirurgie vitale. Les combats actuels (haute intensité mais avec des effectifs plutôt limités) prônent pour le développement de cette stratégie. Le document présenté est une réflexion australienne en la matière.
-----------------------------------------------------
Contemporary battlefield trauma surgery in the Middle East Region has been characterised by aeromedical evacuation by rotatory wing (RWAME) with relative impunity. Therefore, future health planning needs to consider an environment whereby RWAME movement may be degraded or denied by a near-peer, peer or superior threat. To that end, an exploration of alternative approaches to surgical management of injured personnel is pertinent. Life-saving surgical intervention may be delivered by deploying mobile surgical assets forward rather than
relying on evacuation of casualty rearward. Shortly after the arrival of surgical resources to the point of injury, temporising damage control procedures may begin, removing the delay associated with casualty preparation, package and transfer. Essentially, the concept is to significantly augment Role 1 activities for a time-limited period to increase the evacuation window allowing patients to survive that would otherwise die on the battlefield if rapid evacuation capability was degraded or denied. An exploration of the surgical procedures, anaesthetic considerations and transport logistics associated with these interventions is presented in this paper. Limitations on the concept include tactical training requirement of forward deployed medical staff, definition and description of surgical intervention offered and prerequisite civilian skillset, attendant load list, and considerations of anaesthetic delivery and casualty hold elements.
08/06/2022
Trauma Prehospitalier: Aides
| Tags : traumatologie
16/02/2022
Triage en cas d'attaque terroriste: Des limites
Triage in Complex, Coordinated Terrorist Attacks
Pepper M et Al. Prehosp Disaster Med. 2019 Aug;34(4):442-448.
Introduction:
Terror attacks have increased in frequency, and tactics utilized have evolved. This creates significant challenges for first responders providing life-saving medical care in their immediate aftermath. The use of coordinated and multi-site attack modalities exacerbates these challenges. The use of triage is not well-validated in mass-casualty settings, and in the setting of intentional mass violence, new and innovative approaches are needed.
Methods:
Literature sourced from gray and peer-reviewed sources was used to perform a comparative analysis on the application of triage during the 2011 Oslo/Utoya Island (Norway), 2015 Paris (France), and 2015 San Bernardino (California USA) terrorist attacks. A thematic narrative identifies strengths and weaknesses of current triage systems in the setting of complex, coordinated terrorist attacks (CCTAs).
Discussion:
Triage systems were either not utilized, not available, or adapted and improvised to the tactical setting. The complexity of working with large numbers of patients, sensory deprived environments, high physiological stress, and dynamic threat profiles created significant barriers to the implementation of triage systems designed around flow charts, physiological variables, and the use of tags. Issues were identified around patient movement and "tactical triage."
Conclusion:
Current triage tools are inadequate for use in insecure environments, such as the response to CCTAs. Further research and validation are required for novel approaches that simplify tactical triage and support its effective application. Simple solutions exist in tactical triage, patient movement, and tag use, and should be considered as part of an overall triage system.
| Tags : triage
18/01/2022
Echo Pleurale: ??
Not so FAST-Chest ultrasound underdiagnoses traumatic pneumothorax
Santorelli JE et Al.
J Trauma Acute Care Surg. 2022 Jan 1;92(1):44-48.
-----------------------------------------------------------
Le fait de ne rien voir à l'échographie ne signifie pas qu'il n'y a rien. Cette étude prend le contre-pied de l'outil miracle que l'échographie représente pour certains.
-----------------------------------------------------------
Background: Ultrasonography for trauma is a widely used tool in the initial evaluation of trauma patients with complete ultrasonography of trauma (CUST) demonstrating equivalence to computed tomography (CT) for detecting clinically significant abdominal hemorrhage. Initial reports demonstrated high sensitivity of CUST for the bedside diagnosis of pneumothorax. We hypothesized that the sensitivity of CUST would be greater than initial supine chest radiograph (CXR) for detecting pneumothorax.
Methods: A retrospective analysis of patients diagnosed with pneumothorax from 2018 through 2020 at a Level I trauma center was performed. Patients included had routine supine CXR and CUST performed prior to intervention as well as confirmatory CT imaging. All CUST were performed during the initial evaluation in the trauma bay by a registered sonographer. All imaging was evaluated by an attending radiologist. Subgroup analysis was performed after excluding occult pneumothorax. Immediate tube thoracostomy was defined as tube placement with confirmatory CXR within 8 hours of admission.
Results: There were 568 patients screened with a diagnosis of pneumothorax, identifying 362 patients with a confirmed pneumothorax in addition to CXR, CUST, and confirmatory CT imaging. The population was 83% male, had a mean age of 45 years, with 85% presenting due to blunt trauma. Sensitivity of CXR for detecting pneumothorax was 43%, while the sensitivity of CUST was 35%. After removal of occult pneumothorax (n = 171), CXR was 78% sensitive, while CUST was 65% sensitive (p < 0.01). In this subgroup, CUST had a false-negative rate of 36% (n = 62). Of those patients with a false-negative CUST, 50% (n = 31) underwent tube thoracostomy, with 85% requiring immediate placement.
Conclusion: Complete ultrasonography of trauma performed on initial trauma evaluation had lower sensitivity than CXR for identification of pneumothorax including clinically significant pneumothorax requiring tube thoracostomy. Using CUST as the primary imaging modality in the initial evaluation of chest trauma should be considered with caution.
16/11/2021
PLP: A ne pas mettre au rebus !
Contemporary utility of diagnostic peritoneal aspiration in trauma
Morgan Schellenberg M et Al. J Trauma Acute Care Surg. 2021 Nov 1;91(5):814-819.
Background: Focused Assessment with Sonography for Trauma (FAST) has supplanted diagnostic peritoneal lavage (DPL) as the preferred bedside evaluation for traumatic hemoperitoneum. Diagnostic peritoneal aspiration (DPA) is a simpler, faster modification of DPL with an unclear role in contemporary practice. This study delineated modern roles for DPA and defined its diagnostic yield.
Methods: All trauma patients presenting to our Level I center who underwent DPA were included (May 2015 to May 2020). Demographics, comorbidities, clinical/injury data, and outcomes were collected. The diagnostic yield and accuracy of DPA were calculated against the criterion standard of hemoperitoneum at exploratory laparotomy or computed tomography scan.
Results: In total, 41 patients underwent DPA, typically after blunt trauma (n = 37, 90%). Patients were almost exclusively hypotensive (n = 20, 49%) or in arrest (n = 18, 44%). Most patients had an equivocal or negative FAST and hypotension or return of spontaneous circulation after resuscitative thoracotomy (n = 32, 78%); or had a positive FAST and known cirrhosis (n = 4, 10%). In two (5%) patients, one obese, the catheter failed to access the peritoneal cavity. Diagnostic peritoneal aspiration sensitivity, specificity, positive predictive value, and negative predictive value were 80%, 100%, 100%, and 90%, with an accuracy of 93%. One (2%) complication, a small bowel injury, occurred.
Conclusion: Despite near ubiquitous FAST availability, DPA remains important in diagnosing or excluding hemoperitoneum with exceedingly low rates of failure and complications. Diagnostic peritoneal aspiration is most conclusive when positive, without false positives in this study. Diagnostic peritoneal aspiration was most used among blunt hypotensive or postarrest patients who had an equivocal or negative FAST, in whom the preliminary diagnosis of hemoperitoneum is a critically important decision making branch point.
17/07/2021
Transfuser avant l'hôpital: Pas suffisant pour réduire la mortalité
Effect of Prehospital Red Blood Cell Transfusion on Mortality and Time of Death in Civilian Trauma Patients
Background:
Current management principles of hemorrhagic shock after trauma emphasize earlier transfusion therapy to prevent dilution of clotting factors and correct coagulopathy. London's Air Ambulance (LAA) was the first UK civilian prehospital service to routinely offer prehospital red blood cell (RBC) transfusion (phRTx). We investigated the effect of phRTx on mortality.
Methods:
Retrospective trauma database study comparing mortality before implementation with after implementation of phRTx in exsanguinating trauma patients. Univariate logistic regression was performed for the unadjusted association between phRTx and mortality was performed, and multiple logistic regression adjusting for potential confounders.
Results:
We identified 623 subjects with suspected major hemorrhage. We excluded 84 (13.5%) patients due to missing data on survival status. Overall 187 (62.3%) patients died in the before phRTx period and 143 (59.8%) died in the after phRTx group. There was no significant improvement in overall survival after the introduction of phRTx (P = 0.554). Examination of prehospital mortality demonstrated 126 deaths in the pre-phRTx group (42.2%) and 66 deaths in the RBC administered group (27.6%). There was a significant reduction in prehospital mortality in the group who received RBC (P < 0.001).
Conclusions:
phRTx was associated with increased survival to hospital, but not overall survival. The “delay death” effect of phRTx carries an impetus to further develop inhospital strategies to improve survival in severely bleeding patients.
DCR: Tout ne réduit pas la mortalité à l'hôpital ?
After 800 MTP Events, Mortality due To Hemorrhagic Shock Remains High And Unchanged Despite Several In-Hospital Hemorrhage Control Advancements
Duchesne, J et Al. SHOCK: May 27, 2021 doi: 10.1097/SHK.0000000000001817
-------------------------------------------------------
La mise en oeuvre de moyens adaptés d'hémostase comme le REBOA est proposé dans une stratégie de DCR conduite à l'hôpital. Pourtant cette publication ne milite pas pour une amélioration de la survie de patients présentants un trauma pénétrants et requérants une transfusion massive. Seules la pose de garrot et la transfusion de sang total permettent de réduire la mortalité dans un système de prise en charge adapté. La réalisation encore plus précoce pourrait être une solution.
-------------------------------------------------------
Background:
Numerous advancements in hemorrhage control and volume replacement that comprise damage control resuscitation (DCR) have been implemented in the last decade to reduce deaths from bleeding. We sought to determine the impact of DCR interventions on mortality over 12 years in a massive transfusion protocol (MTP) population. We hypothesized that mortality would be decreased in later years, which would have used more DCR interventions.
Study Design:
This was a retrospective review of all MTP patients treated at a large regional Level I trauma center from 2008–2019. Interventions by year of implementation examined included MTP 1:1 ratio (2009), liquid plasma (2010), tranexamic acid (2012), pre-hospital tourniquets (2013), REBOA/TEG (2017), satellite blood station (2018), and whole blood transfusion (2019). Relative risk and odds of mortality for DCR interventions were examined.
Results:
There were 824 MTP patients included. The cohort was primarily male (80.6%) injured by penetrating mechanism (68.1%) with median (IQR) age 31 years (23–44) and NISS 25 (16–34). Overall mortality was unchanged [(38.3% to 56.6%); P = 0.26]. Tourniquets (P = 0.02) and WB (P = 0.03) were associated with lower unadjusted mortality; only tourniquets remained significant after adjustment (OR:0.39;95%CI:0.17–0.89; P = 0.03).
Conclusions:
Despite lower mortality with use of tourniquets and WB, mortality rates due to hemorrhage have not improved at our high MTP volume institution, suggesting implementation of new in-hospital strategies is insufficient to reduce mortality. Future efforts should be directed towards moving hemorrhage control and effective resuscitation interventions to the injury scene.
04/06/2021
Extraction de blessé: L'avenir


