10/02/2014
Inhalation de fumées: Héparine en aérosol ?
Inhaled Anticoagulation Regimens for the Treatment of Smoke Inhalation–Associated Acute Lung Injury: A Systematic Review*
Miller AC et Al. Crit Care Med 2014; 42:413–419
----------------------------------------------------------------------------------------------
L'inhalation de fumées est fréquentes lors de la prise en charge de victilmes par explosion. Laprise en charge de brNébiliser 5000 à 1000U d'héparine inhalé avec 3ml de NacétylCystéine et de l'albuterol améliorerait la survie
----------------------------------------------------------------------------------------------
OBJECTIVE:
Inhaled anticoagulation regimens are increasingly being used to manage smoke inhalation-associated acute lung injury. We systematically reviewed published and unpublished preclinical and clinical trial data to elucidate the effects of these regimens on lung injury severity, airway obstruction, ventilation, oxygenation, pulmonary infections, bleeding complications, and survival.
DATA SOURCES:
PubMed, Scopus, EMBASE, and Web of Science were searched to identify relevant published studies. Relevant unpublished studies were identified by searching the Australian and New Zealand Clinical Trials Registry, World Health Organization International Clinical Trials Registry Platform, Cochrane Library, ClinicalTrials.gov, MINDCULL.com, Current Controlled Trials, and Google.
STUDY SELECTION:
Inclusion criteria were any preclinical or clinical study in which 1) animals or subjects experienced smoke inhalation exposure, 2) they were treated with nebulized or aerosolized anticoagulation regimens, including heparin, heparinoids, antithrombins, or fibrinolytics (e.g., tissue plasminogen activator), 3) a control and/or sham group was described for preclinical studies, and 4) a concurrent or historical control group described for clinical studies. Exclusion criteria were 1) the absence of a group treated with a nebulized or aerosolized anticoagulation regimen, 2) the absence of a control or sham group, and 3) case reports.
DATA EXTRACTION:
Ninety-nine potentially relevant references were identified. Twenty-seven references met inclusion criteria including 19 preclinical references reporting 18 studies and eight clinical references reporting five clinical studies.
DATA SYNTHESIS:
A systematic review of the literature is provided. Both clinical and methodological diversity precluded combining these studies in a meta-analysis.
CONCLUSIONS:
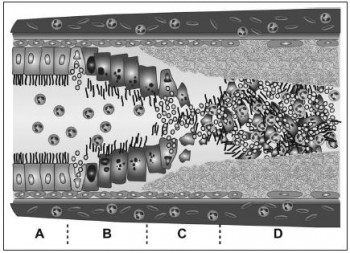
The high mortality associated with smoke inhalation-associated acute lung injury results from airway damage, mucosal dysfunction, neutrophil infiltration, airway coagulopathy with cast formation, ventilation-perfusion mismatching with shunt, and barotrauma. Inhaled anticoagulation regimens in both preclinical and clinical studies improve survival and decrease morbidity without altering systemic markers of clotting and anticoagulation. In some preclinical and clinical studies, inhaled anticoagulants were associated with a favorable effect on survival. This approach appears sufficiently promising to merit a well-designed prospective study to validate its use in patients with severe smoke inhalation-associated acute lung injury requiring mechanical ventilation.
| Tags : brûlure

Les commentaires sont fermés.