09/01/2016
1/1/1 ou 1/1/2 ?
Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial
Holcomb JB et All. JAMA Surg. 2013 Feb;148(2):127-36
______________________________
La reconnaissance et la mise en place de la meilleure stratégie thérapeutique du choc hémorragique traumatique sont des enjeux fondamentaux qui se posent aux équipes de réanimation préhospitalières et hospitalières. L'application du concepts du damage control resuscitation (1) vise par la mise en place d'un stratégie raisonnée d'arrêt des hémorragies (2), d'un remplissage vasculaire mesuré (3) et d'une politique transfusionnelle spécifique (4). Parmi ces mesures, il apparaît important de garantir l'apport équilibré de plasma, de plaquettes et de CGR dans un ration élevé 1/1/1 ou 1/1/2. Deux études se sont attachées à ce point: L'étude PROMMTT et l'étude PROPPR ici présentée. La première confirme le bénéfice d'une telle stratégie avec une moindre mortalité chez les patients bénéficiant de rapport élevé supérieur mais uniquement dans les 6 premières heures. L'étude PROPPR semble confirmer ces données avec une moindre mortalité précoce par hémorragie mais ne réussit pas à confirmer l'intérêt d'un ratio 1/1/1 par rapport à un ratio 1/1/2 sur la mortalité à long terme.
______________________________
IMPORTANCE:
Severely injured patients experiencing hemorrhagic shock often require massive transfusion. Earlier transfusion with higher blood product ratios (plasma, platelets, and red blood cells), defined as damage control resuscitation, has been associated with improved outcomes; however, there have been no large multicenter clinical trials.
OBJECTIVE:
To determine the effectiveness and safety of transfusing patients with severe trauma and major bleeding using plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio.
DESIGN, SETTING, AND PARTICIPANTS:
Pragmatic, phase 3, multisite, randomized clinical trial of 680 severely injured patients who arrived at 1 of 12 level I trauma centers in North America directly from the scene and were predicted to require massive transfusion between August 2012 and December 2013.
INTERVENTIONS:
Blood product ratios of 1:1:1 (338 patients) vs 1:1:2 (342 patients) during active resuscitation in addition to all local standard-of-care interventions (uncontrolled).
MAIN OUTCOMES AND MEASURES:
Primary outcomes were 24-hour and 30-day all-cause mortality. Prespecified ancillary outcomes included time to hemostasis, blood product volumes transfused, complications, incidence of surgical procedures, and functional status.
RESULTS:
No significant differences were detected in mortality at 24 hours (12.7% in 1:1:1 group vs 17.0% in 1:1:2 group; difference, -4.2% [95% CI, -9.6% to 1.1%]; P = .12) or at 30 days (22.4% vs 26.1%, respectively; difference, -3.7% [95% CI, -10.2% to 2.7%]; P = .26). Exsanguination, which was the predominant cause of death within the first 24 hours, was significantly decreased in the 1:1:1 group (9.2% vs 14.6% in 1:1:2 group; difference, -5.4% [95% CI, -10.4% to -0.5%]; P = .03). More patients in the 1:1:1 group achieved hemostasis than in the 1:1:2 group (86% vs 78%, respectively; P = .006). Despite the 1:1:1 group receiving more plasma (median of 7 U vs 5 U, P < .001) and platelets (12 U vs 6 U, P < .001) and similar amounts of red blood cells (9 U) over the first 24 hours, no differences between the 2 groups were found for the 23 prespecified complications, including acute respiratory distress syndrome, multiple organ failure, venous thromboembolism, sepsis, and transfusion-related complications.
CONCLUSIONS AND RELEVANCE:
Among patients with severe trauma and major bleeding, early administration of plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio did not result in significant differences in mortality at 24 hours or at 30 days. However, more patients in the 1:1:1 group achieved hemostasis and fewer experienced death due to exsanguination by 24 hours. Even though there was an increased use of plasma and platelets transfused in the 1:1:1 group, no other safety differences were identified between the 2 groups.
| Tags : hémorragie
19/12/2015
Military medicine in the 21st
Amputé des jambes: Le bassin aussi !
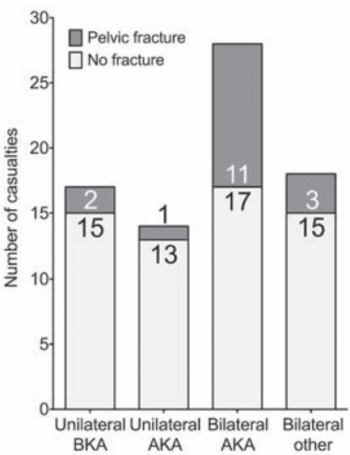
The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices
Cross AM et Al. J R Nav Med Serv 2014;100(2):152-6
---------------------------------------------
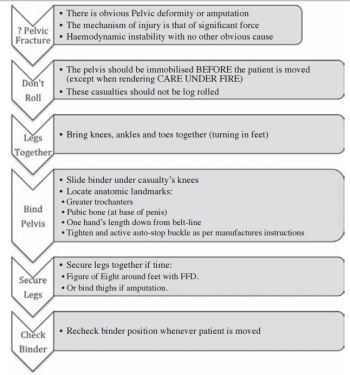
Excepté l'extraction d'urgence de blessés sous le feu, la prise en charge den cas d'amputation traumatique doit inclure la forte probabilité de traumatisme du bassin. Une utilisation large des immobilisations pelviennes doit donc être à l'esprit. On rappelle simplement la gravité et la difficulté de prise en charge des hémorragies liées aux fractures de bassin.
---------------------------------------------
AIMS:
A frequently-seen injury pattern in current military experience is traumatic lower limb amputation as a result of improvised explosive devices (IEDs). This injury can coexist with fractures involving the pelvic ring. This study aims to assess the frequency of concomitant pelvic fracture in IED-related lower limb amputation.
METHODS:
A retrospective analysis of the trauma charts, medical notes, and digital imaging was undertaken for all patients arriving at the Emergency Department at the UK military field hospital in Camp Bastion, Afghanistan, with a traumatic lower limb amputation in the six months between September 2009 and April 2010, in order to determine the incidence of associated pelvic ring fractures.
RESULTS:
Of 77 consecutive patients with traumatic lower limb amputations, 17 (22%) had an associated pelvic fracture (eleven with displaced pelvic ring fractures, five undisplaced fractures and one acetabular fracture). Unilateral amputees (n = 31) had a 10% incidence of associated pelvic fracture, whilst 30 % of bilateral amputees (n = 46) had a concurrent pelvic fracture. However, in bilateral, trans-femoral amputations (n = 28) the incidence of pelvic fracture was 39%.
CONCLUSIONS:
The study demonstrates a high incidence of pelvic fractures in patients with traumatic lower limb amputations, supporting the routine pre-hospital application of pelvic binders in this patient group
| Tags : hémorragie, immobilisation, blast
17/12/2015
Médicaliser: Pour faire quoi ?
Doctor on board ? What is the optimal skill-mix in military pre-hospital care ?
Calderbank P. et Al. Emerg Med J (2010). doi:10.1136/emj.2010.097642
--------------------------------
Le document proposé à la lecture porte sur l'intérêt de la présence d'un médecin dans la plus avancée des structures medevac qui existe actuellement: Les MERT-E des anglais. Seule 1 medevac sur 5 justifiait la présence d'un médecin. L'intervention la plus fréquemment réalisée a été l'intubation/induction en séquence rapide. Bien loin devant d'autres gestes comme la thoracostomie ou le drainage thoracique. Ceci étant dit ce constat est fait dans un contexte spécifique afghan qui ne correspond pas aux opérations actuelles où les délais de prise en charge chirurgicales peuvent être long. Cette pratique est donc essentielle à maîtriser et procède d'une véritable stratégie de formation, avec une rythmicité semestrielle, débutée dès la formation initiale, associant un parcours structuré de mises à jour technique personnelle (passage en bloc opératoire, participation à des ateliers sur simulateurs de taches) et collective. Il s'agit d'un exemple parmi d'autres où une implication personnelle forte doit être présente.
--------------------------------
Background
In a military setting, pre-hospital times may be extended due to geographical or operational issues. Helicopter casevac enables patients to be transported expediently across all terrains. The skill-mix of the prehospital team can vary. Aim To quantify the doctors’ contribution to the Medical Emergency Response TeameEnhanced (MERT-E).
Methods
A prospective log of missions recorded urgency category, patient nationality, mechanism of injury, medical interventions and whether, in the crew’s opinion, the presence of the doctor made a positive contribution.
Results
Between July and November 2008, MERT-E flew 324 missions for 429 patients. 56% of patients carried were local nationals, 35% were UK forces. 22% of patients were T1, 52% were T2, 21.5% were T3 and 4% were dead. 48% patients had blast injuries, 25% had gunshot wounds, 6 patients had been exposed to blast and gunshot wounds. Median time from take-off to ED arrival was 44 min. A doctor flew on 88% of missions. It was thought that a doctor’s presence was not clinically beneficial in 77% of missions. There were 62 recorded physician’s interventions: the most common intervention was rapid sequence induction (45%); other interventions included provision of analgesia, sedation or blood products (34%), chest drain or thoracostomy (5%), and pronouncing life extinct (6%).
Conclusion
MERT-E is a high value asset which makes an important contribution to patient care. A relatively small proportion of missions require interventions beyond the capability of well-trained military paramedics; the indirect benefits of a physician are more difficult to quantify.
| Tags : airway
13/11/2015
Demain: Quels enjeux ?
09/11/2015
Plaie cérébrale et coagulopathie
Quelques faits
1. Elle est fréquente voire très fréquente: Greuters et al. Critical Care 2011 15:R2 doi:10.1186/cc9399

2. Elle est + fréquente en cas d'hypoTA: Wafaisade Neurocrit Care. 2010 Apr;12(2):211-9
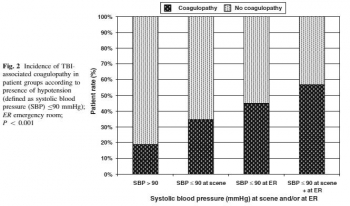
3. Elle est de mauvais pronostic: J Emerg Trauma Shock. 2013 Jul-Sep; 6(3): 180–185

4. Elle est mise en évidence plutôt par thromboélastographie (r TEG) : Sixta al., J Neurol Neurophysiol 2014, 6:5
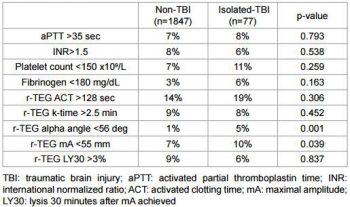
| Tags : coagulopathie
08/11/2015
Damage Control: Vraiment bénéfique
Changing Patterns of In-Hospital Deaths Following Implementation of Damage Control Resuscitation Practices in US Forward Military Treatment Facilities
Langan NR et Al. JAMA Surg. 2014;149(9):904-912
Importance
Analysis of combat deaths provides invaluable epidemiologic and quality-improvement data for trauma centers and is particularly important under rapidly evolving battlefield conditions.
Objective
To analyze the evolution of injury patterns, early care, and resuscitation among patients who subsequently died in the hospital, before and after implementation of damage control resuscitation (DCR) policies.
Design, Setting, and participants
In a review of the Joint Theater Trauma Registry (2002-2011) of US forward combat hospitals, cohorts of patients with vital signs at presentation and subsequent in-hospital death were grouped into 2 time periods: pre-DCR (before 2006) and DCR (2006-2011).
Main outcomes and measures
Injury types and Injury Severity Scores (ISSs), timing and location of death, and initial (24-hour) and total volume of blood products and fluid administered.
Results
Of 57 179 soldiers admitted to a forward combat hospital, 2565 (4.5%) subsequently died in the hospital. The majority of patients (74%) were severely injured (ISS > 15), and 80% died within 24 hours of admission. Damage control resuscitation policies were widely implemented by 2006 and resulted in a decrease in mean 24-hour crystalloid infusion volume (6.1-3.2 L) and increased fresh frozen plasma use (3.2-10.1 U) (both P < .05) in this population. The mean packed red blood cells to fresh frozen plasma ratio changed from 2.6:1 during the pre-DCR period to 1.4:1 during the DCR period (P < .01). There was a significant increase in mean ISS between cohorts (pre-DCR ISS = 23 vs DCR ISS = 27; P < .05) and a marked shift in injury patterns favoring more severe head trauma in the DCR cohort.
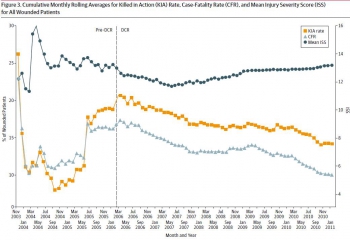
Conclusions and relevance
There has been a significant shift in resuscitation practices in forward combat hospitals indicating widespread military adoption of DCR. Patients who died in a hospital during the DCR period were more likely to be severely injured and have a severe brain injury, consistent with a decrease in deaths among potentially salvageable patients
| Tags : remplissage
06/11/2015
Prolonged field Care: Novateur ? Pas vraiment
Prolonged Field Care Working Group Position Paper Prolonged Field Care Capabilities
Bal JA et All. J Spec Oper Med. 2015 Fall;15(3):78-80
Le concept du TCCC, issu de l'analyse des décès au combat lors de la guerre de Somalie, a vu toute sa pertinence prouvée en afghanistan. Des gestes simples réalisés par des soldats et des combat medic ont permis d'éviter le décès de nombre de soldats. Ces derniers étaient alors évacués rapidement vers des structures chirurgicales. Le concept afghan permettait cela.
Ce n'est pas le cas des conflits actuels, conflits pendant lesquels le combattant blessé doit se voir appliquer pendant plusieurs heures une démarche de prise en charge (remplissage, analgésie, nursing,..) très proche de la réanimation préhospitalière. C'est bien compte tenu de l'absence de médecins et donc de connaissances en la matière que cette pratique de prise en charge est considérée par nos collègues US comme nouvelle. Ce concept ne doit donc pas probablement être considéré comme novateur pour nous car il s'agit d'une démarche de convergence d'une pratique anglo-saxonne vers notre médicalisation de l'avant.
02/11/2015
Mg++: Médicament de la coagulopathie ?
Both acute delivery of and storage with magnesium sulfate promote cold-stored platelet aggregation and coagulation function
Meledeo MA et Al. J Trauma Acute Care Surg. 2015 Oct;79(4 Suppl 2):S139-45
----------------------------------------
Il y a quelque mois était publié un travail de recherche portant sur l'intérêt de l'administration de Adénosine/Lidocaïne/Mg2+ ALM (1, 2, 3). Une hypothèse faite par les auteurs serait que L'ALM agirait comme un antifibrinolytique en activant la voie du thrombin-activatable fibrinolysis inhibitor (TAFI) plutôt que celle de la protéine C. Cette action passerait par un mécanisme antiinflammatoire, une modification de la polarité endothéliale et une action sur la fonction plaquettaire. Le travail expérimental dont l'abstract est présenté met en avant l'intérêt de l'adminsitration de magnésium pour la restauration de la fonction plaquettaire après conservation de palquettes d'aphérèse au delà de 5 jours.
----------------------------------------
BACKGROUND:
The platelet storage lesion causes loss of function and viability over time. A new paradigm for platelet storage is desired to enable safer, more effective transfusions while reducing waste. We hypothesized that repletion of Mg, which is chelated by citrate anticoagulant, could reduce platelet storage lesion severity when given in conjunction with storage at a refrigerated temperature.
METHODS:
Apheresis platelet units were collected from healthy donors and stored at 22°C or 4°C. On Days 0, 2, 4, and 8, samples were collected for analyses of receptor-mediated aggregation, coagulation, adhesion to collagen under flow, and viability. In the first series, samples were given anacute dose of MgSO4 before testing; in the second series, storage bags were supplemented with 0-, 3-, or 6-mM MgSO4.
RESULTS:
Acutely delivered MgSO4 induced a more rapid coagulation time in apheresis platelets, further enhanced by storage at 4°C. Plateletadhesion to a collagen surface while exposed to arterial shear rates (920 s) was enhanced by MgSO4 supplementation-acute MgSO4 had a large effect on adhesion of fresh platelets, which diminished more rapidly in 22°C samples, while storage with MgSO4 showed significant benefits even out to Day 4 at both temperatures. Although 4°C storage improves the longevity of platelet aggregation responses to agonists, MgSO4 supplementation did not change those responses.
CONCLUSION:
Acute MgSO4 reduces clot time likely through the transient increase of free Ca. Limited differences between platelet function inacute delivery of and storage with MgSO4 diminish the possibility that Mg-induced metabolic inhibition of platelets synergizes with 4°C storage. Regardless, magnesium supplementation to platelets is an exciting possibility in transfusion because the adhesion response of 22°C-stored platelets on Day 4 is significantly enhanced when stored with 6-mM MgSO4
| Tags : coagulopathie
01/11/2015
IED à pied: Amputations 2aires fréquentes
Outcomes after Long-Term Follow-Up of Combat-Related Extremity Injuries in a Multidisciplinary Limb Salvage Clinic
Casey K et Al. Ann Vasc Surg. 2015 Apr;29(3):496-501
Background: Although the incidence of casualties from the Global War on Terror is decreasing, there remains a focus on the long-term sequelae from injuries sustained in the combat. Patients with prior significant limb injuries remain at risk of future complications. This study examines our institution’s experience with a multidisciplinary team approach toward this challenging patient population.
Methods: A retrospective review was performed on all patients treated in a single institution Limb Preservation Clinic over a 2-year period. Those patients who sustained a combatrelated injury in theater were examined. Patient demographics, mechanism of injury, amputation rates, time to amputation, and reasons for failure were examined.
Results: Ninety-four patients were evaluated in our multidisciplinary Limb Preservation Clinic over a 2-year period. Twenty patients (21%) were seen for combat-related injuries. Sixteen patients were evaluated and treated for chronic complications at a median of 13 months from their injury. All 16 patients were male with a median age of 24 years (range, 20e35). Ten patients sustained injuries secondary to a dismounted improvised explosive device (IED). All 16 patients had extensive soft tissue injuries and associated fractures. Only 2 patients sustained a vascular injury. The median number of prior surgeries to the affected limb was 8 (range, 3e19). The limb salvage rate of 37% was lower than our noncombat cohort (47%). The most common reasons for delayed amputation included chronic pain, osteomyelitis, and soft tissue infections.
Conclusions: The high secondary amputation rates seen in this cohort underscores the need for long-term follow-up. Despite successful initial outcomes, many patients eventually progress to limb loss. Patients who sustain a dismounted IED are at greatest risk for a delayed amputation. Identifying and addressing those factors which lead to delayed amputation should be a priority for returning war veterans and focus of future studies.
23/10/2015
Quelle place pour les facteurs de la coagulation ?
| Tags : hémorragie, coagulopathie, choc
11/10/2015
Les blessés français en afghanistan
09/10/2015
Pas bon si TA < 100
Hypotension is 100 mm Hg on the battlefield
Eastridge DJ et All. Am J Surg. 2011 Oct;202(4):404-8
BACKGROUND:
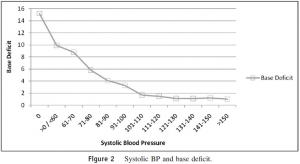
Historically, emergency physicians and trauma surgeons have referred to a systolic blood pressure (SBP) of 90 mm Hg as hypotension. Recent evidence from the civilian trauma literature suggests that 110 mm Hg may be more appropriate based on associated acidosis and outcome measures. In this analysis, we sought to determine the relationship between SBP, hypoperfusion, and mortality in the combat casualty.
METHODS:
A total of 7,180 US military combat casualties from the Joint Theater Trauma Registry from 2002 to 2009 were analyzed with respect to admission SBP, base deficit, and mortality. Base deficit, as a measure of hypoperfusion, and mortality were plotted against 10-mm Hg increments in admission SBP.
RESULTS:
By plotting SBP, baseline mortality was less than 2% down to a level of 101 to 110 mm Hg, at which point the slope of the curve increased dramatically to a mortality rate of 45.1% in casualties with an SBP of 60 mm Hg or less but more than 0 mm Hg. A presenting SBP of 0 mm Hg was associated with 100% mortality. The data also established a similar effect for base deficit with a sharp increase in the rate of acidosis, which became manifest at an SBP in the range of 90 to 100 mm Hg.
CONCLUSIONS:
This analysis shows that an SBP of 100 mm Hg or less may be a better and more clinically relevant definition of hypotension and impending hypoperfusion in the combat casualty. One utility of this analysis may be the more expeditious identification of battlefield casualties in need of life-saving interventions such as the need for blood or surgical intervention.
20/09/2015
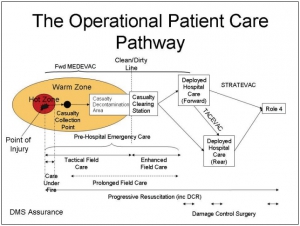
The Operational Patient Care Pathway
The Operational Patient Care Pathway
Une évolution importante de nos amis anglais qui précise le concept du "Prolonged Field Care" et révisent le concept de la golden Hour et des minutes de platine pour le 10-1-2 + 2
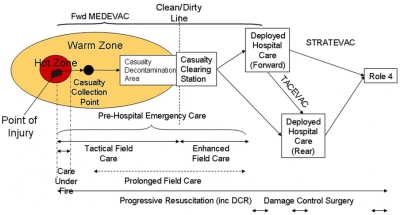
For debate: the Operational Patient Care Pathway
Bricknell M. J R Army Med Corps. 2014 Mar;160(1):64-9
| Tags : tactique
18/09/2015
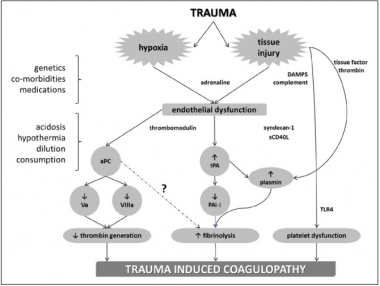
Coagulopathie traumatique: Mécanismes
Trauma-Induced Coagulopathy: An Institution's 35 Year Perspective on Practice and Research
Gonzales E. et Al. Scandinavian Journal of Surgery 103: 89–103, 2014
| Tags : coagulopathie
01/08/2015
Milieu isolé: Mieux vaut avoir été préparé(e)
Preparing for Operations in a Resource-Depleted and/or Extended Evacuation Environment
Corey G et Al. J Spec Oper Med. 2013 Fall;13(3):74-80
The wars in Afghanistan and Iraq are the only conflicts to which many medics have ever been exposed. These mature theaters have robust medical systems that ensure rapid access to full-spectrum medical care for all combat-wounded and medically injured personnel. As current conflicts draw to a close, U.S. medics may be deployed to environments that will require the ability to stabilize casualties for longer than 1 hour. Historical mission analysis reveals the need to review skills that have not been emphasized during upgrade and predeployment training. This unit’s preparation for the extended care environment can be accomplished using a 4-point approach: (1) review of specific long-term skills training, (2) an extended care lab that reviews extended care skills and then lets the medic practice in a real-time scenario, (3) introduction to the HITMAN mnemonic tool, which helps identify and address patient needs, and (4) teleconsultation.
30/07/2015
ATLS: Référence en ballistique ? Bof !
Myths and Misinformation About Gunshot Wounds may Adversely Affect Proper Treatment.
Hafertepen SC et Al. World J Surg. 2015 Jul;39(7):1840-7
-----------------------------------
La pertinence de l'ATLS est régulièrement battue en brèche pour les systèmes de prise en charge des traumatisés organisés en réseau. Historiquement il s'agissait d'apporter des connaissances de base à des équipes novices en la matière. Une revue cochrane n'est pas du tout en faveur. Un éditorial récent, mais il n'est pas isolé, exprime bien le caractère non adapté de ce concept à la réalité des trauma center actuels. Certains vont très loin dans la critique mettant en évidence dans le contenu même des dernières révisions la retranscription de données non validées. C'est le cas du document proposé. Au delà du caractère structurant réel d'un acronyme, c'est bien d'un contenu basique (trop) et souvent erroné dont nous devons être conscient.
-----------------------------------
BACKGROUND:
Poorly designed experiments and popular media have led to multiple myths about wound ballistics. Some of these myths have been incorporated into the trauma literature as fact and are included in Advanced Trauma Life Support (ATLS). We hypothesized that these erroneous beliefs would be prevalent, even among those providing care for patients with gunshot wounds (GSWs), but could be addressed through education.
METHODS:
ATLS course content was reviewed. Several myths involving wound ballistics were identified. Clinically relevant myths were chosen including wounding mechanism, lead poisoning, debridement, and antibiotic use. Subsequently, surgery and emergency medicine services at three different trauma centers were studied. All three sites were busy, urban trauma centers with a significant amount of penetrating trauma. A pre-test was administered prior to a lecture on wound ballistics followed by a post-test. Pre- and post-test scores were compared and correlated with demographic data including ATLS course completion, firearm/ballistics experience, and years of post-graduate medical experience (PGME).
RESULTS:
One-hundred and fifteen clinicians participated in the study. A mean pre-test score of 34 % improved to 78 % on the post-test with associated improvements in all areas of knowledge (p < 0.001). Years of PGME correlated with higher pre-test score (p = 0.021); however, ATLSstatus did not (p = 0.774).
CONCLUSIONS:
Erroneous beliefs involving wound ballistics are prevalent even among clinicians who frequently treat victims of GSWs and could lead to inappropriate treatment. Focused education markedly improved knowledge. The ATLS course and manual promulgate some of these myths and should be revised.
20/07/2015
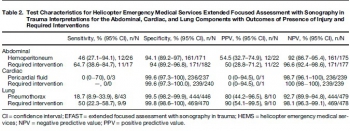
Echo en hélico: Avec formation solide !
Prospective evaluation of prehospital trauma ultrasound during aeromedical transport.
Press GM et Al. J Emerg Med. 2014 Dec;47(6):638-45
------------------------------------------------
L'apport de l'échographie est incontournable pour la prise en charge des traumatisés. Son emploi en prehospitalier est proposé. Pour autant la mise en oeuvre de ce moyen d'exploration n'est pas si simple et demande une grande expertise. Le travail présenté porte sur la mise en oeuvre de ce type d'exploration par technicinens paramédicaux expérimentés et ayant suivi une formation sur une période de deux mois. malgré cela leur performance reste modeste. Un examen négatif de permet pas de conclure. Ceci plaide pour un peu de modération concernant l'engouement actuel. Comme pour tout il faut investir sur la formation pour être performant.
------------------------------------------------
BACKGROUND:
Ultrasound is widely considered the initial diagnostic imaging modality for trauma. Preliminary studies have explored the use of trauma ultrasound in the prehospital setting, but the accuracy and potential utility is not well understood.
OBJECTIVE:
We sought to determine the accuracy of trauma ultrasound performed by helicopter emergency medical service (HEMS) providers.
METHODS:
Trauma ultrasound was performed in flight on adult patients during a 7-month period. Accuracy of the abdominal, cardiac, and lung components was determined by comparison to the presence of injury, primarily determined by computed tomography, and to required interventions.
RESULTS:
HEMS providers performed ultrasound on 293 patients during a 7-month period, completing 211 full extended Focused Assessment with Sonography for Trauma (EFAST) studies. HEMS providers interpreted 11% of studies as indeterminate. Sensitivity and specificity for hemoperitoneum was 46% (95% confidence interval [CI] 27.1%-94.1%) and 94.1% (95% CI 89.2%-97%), and for laparotomy 64.7% (95% CI 38.6%-84.7%) and 94% (95% CI 89.2%-96.8%), respectively. Sensitivity and specificity for pneumothorax were 18.7% (95% CI 8.9%-33.9%) and 99.5% (95% CI 98.2%-99.9%), and for thoracostomy were 50% (95% CI 22.3%-58.7%) and 99.8% (98.6%-100%), respectively. The positive likelihood ratio for laparotomy was 10.7 (95% CI 5.5-21) and for thoracostomy 235 (95% CI 31-1758), and the negative likelihood ratios were 0.4 (95% CI 0.2-0.7) and 0.5 (95% CI 0.3-0.8), respectively. Of 240 cardiac studies, there was one false-positive and three false-negative interpretations (none requiring intervention).
CONCLUSIONS:
HEMS providers performed EFAST with moderate accuracy. Specificity was high and positive interpretations raised the probability of injury requiring intervention. Negative interpretations were predictive, but sensitivity was not sufficient for ruling out injury.
| Tags : échographie
Dossier sauvetage au combat
Dossier "Sauvetage au combat"

01 Pierret C. Les traumatismes jonctionnels en situation de guerre.Medecine et Armees 2014-4.291-9.(format pdf, 175 kB).
02 Precloux P. Operation Pamir bilan et analyse activite des postes medicaux role 1 RSA 2011. Medecine et Armees 2014-4. 299-309.(format pdf, 315 kB).
03 Leyral J. Echographie de l avant au Role 1 quelle formation pour medecin unite.Medecine et Armees 2014-4.309-14.(format pdf, 98 kB).
04 Favier LC.Quelles devraient etre les indications de l echographie en Role 1. Medecine et Armees 2014-4.315-20.(format pdf, 140 kB).
05. Danguy M. Actualisation des garrots de type tourniquet. Medecine et Armees 2014-4. 321-8.(format pdf, 149 kB).
06. Mathieu L. Délabrements etendus par blast a haute intensite.nouvelle entite lesionnelle EEI. Medecine et Armees 2014-4. 329-5.(format pdf, 198 kB).
07 Mathieu L. Traumatismes par blast de arriere pied lies aux attaques de vehicules par EEI. Medecine et Armees 2014-4.337-44.(format pdf, 273 kB).
08 Gunepin M. Evacuations medicales intra-theatres pour raisons dentaires au cours operation Serval. Medecine et Armees 2014-4.345-51.(format pdf, 126 kB).
09 Crehange G. Etude de la qualite de l air a Kaboul. Medecine et Armees 2014-4.353-61.(format pdf, 113 kB).
| Tags : sauvetage
11/07/2015
ATLS: Une vision archaïque ?
ATLS: Archaic Trauma Life Support?
Wiles MD Anaesthesia 2015, 70, 893–906
--------------------------------------------------
Un éditorial décoifffant mais pas tant que cela. Une revue cochrane récente ne trouvait pas d'argument en faveur de l'intérêt de l'ATLS (1). Le bien fondé de ce type de fromation est très débattue dans les pays disposant d'une structure spécialisée de prise en charge de traumatisé( 2). Peu étonnant quand on connait l'histoire de l'ATLS censé apporter des connaissances et une méthode à des personnels et des structures hospitalières non spécialisées en traumatologie. Les conclusions de cet éditorial repositionne très bien ce type de formations courtes
--------------------------------------------------
No one could have imagined that when a light aircraft crashed in rural Nebraska in 1976, the nature of global trauma management would be forever altered. James Styner, an orthopaedic surgeon, was piloting the plane in question and the accident resulted in the death of his wife and serious injuries to himself and his four children. The standard of care that he and his family received in the local hospital in the aftermath of the crash so horrified Styner that he decided to establish a new system for the management of major trauma...........................
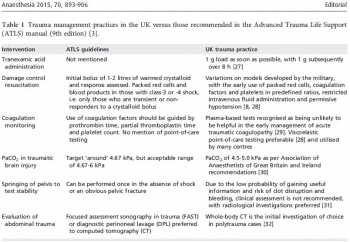
......So what direction should trauma training take in the future?
I would suggest the following:
1 Treat ATLS as a ‘basic’ trauma course, with attendance limited to junior medical staff with no trauma experience. Candidates will learn the common language and vocabulary of trauma management, which will be of benefit when they subsequently attend trauma calls in clinical practice. In the developing world, where resources and personnel are limited, ATLS will continue to have a role.
2 Stop routine recertification of ATLS for individuals experienced in trauma management. Given the high cost of these courses (~£600 (€825; $918) for certification and £350 (€482; $535) for recertification) this practice will account for a significant proportion of an individual’s annual study leave budget. This time and money would be better invested in developing enhanced leadership, communication and teamworking skills.
3 In line with the Royal College of Anaesthetists, remove ATLS certification as a prerequisite for the completion of training in surgery and emergency medicine. Instead, focus on ensuring adequate experience in the management of major trauma.
4 Similarly, for consultant posts that include trauma management, remove ATLS certification as an appointment criterion.
Evidence of experience in trauma management, alongside formal training in leadership and/or human factors, would be of greater relevance.
5 Require regular team-training sessions for MTC staff, either by video review or utilising simulation, ideally within the team’s usual working environment. This would allow training to be institution-specific, with the potential to refine protocols and undertake focused debriefs of recent cases.
When introduced almost 40 years ago, ATLS represented the cutting edge of trauma management; unfortunately, the course has failed to evolve at a pace that allows it to be relevant to the care delivered in modern MTCs. This course without doubt revolutionised trauma care, but it should now be reserved for use in isolated rural centres or environments where trauma is managed infrequently and with limited resources. The King is dead, long live the King.