19/01/2023
Garrot: Moins de 2h OK mais pb après 4h
Impact of Time and Distance on Outcomes Following Tourniquet Use in Civilian and Military Settings: a Scoping Review
Joarder M et Al. https://doi.org/10.1016/j.injury.2023.01.031
Background: The last two decades have seen the reintroduction of tourniquets into guidelines for the management of acute limb trauma requiring haemorrhage control. Evidence supporting tourniquet application has demonstrated low complication rates in modern military settings involving rapid evacuation timeframes. It is unclear how these findings translate to patients who have prolonged transport times from injury in rural settings. This scoping review investigates the relationship between time and distance on metabolic complications, limb salvage and mortality following tourniquet use in civilian and military settings.
Methods: A systematic search strategy was conducted using PubMed, Embase, and SafetyLit databases. Study characteristics, setting, mechanism of injury, prehospital time, tourniquet time, distance, limb salvage, metabolic response, mortality, and tourniquet removal details were extracted from eligible studies. Descriptive statistics were recorded, and studies were grouped by ischemia time (< 2 hours, 2-4 hours, or > 4 hours).
Results: The search identified 3103 studies, from which 86 of studies were included in this scoping review. Of 86 studies, 55 studies were primarily civilian environments and 32 were based in military settings. One study included both settings. Blast injury was the most common mechanism of injury sustained by patients in military settings (72.8% [5968/8200]) followed by penetrating injury (23.5% [1926/8200]). In contrast, in civilian settings penetrating injury was the most common mechanism (47.7% [1633/3426]) followed by blunt injury (36.4% [1246/3426]).
Tourniquet time was reported in 66/86 studies. Tourniquet time over four hours was associated with reduced limb salvage rates (57.1%) and higher mortality rates (7.1%) compared with a tourniquet time of less than two hours. The overall limb salvage and mortality rates were 69.6% and 6.7% respectively. Metabolic outcomes were reported in 28/86 studies with smaller sample sizes and inconsistencies in which parameters were reported.
Conclusion: This scoping review presents literature describing comparatively safe tourniquet application when used for less than two hours duration. However, there is limited research describing prolonged tourniquet application or when used for protracted distances, such that the impact of tourniquet release time on metabolic outcomes and complications remains unclear. Prospective studies utilising the development of an international database to provide this dataset is required.
| Tags : tourniquet
16/08/2020
Conversion de garrot: Le concept Tourniquet +1
Tourniquet Conversion. A Recommended Approach in the Prolonged Field Care Setting
Brendon D. et Al. J Spec Oper Med . Fall 2015;15(3):81-5.
-----------------------------
Les auteurs de ce document proposent le concept du tourniquet +1 lors de la réévaluation d'un garrot posé en contexte tactique. Ceja consiste à oser un second garrot au dessous du premier avant de desserrer le premier garrot. Ils s'appuie sur la fréquence d'après eux de rupture de garrot lors de cette manoeuvre. Cette manoeuvre est à proscrire si le garrot est en place depuis plus de 6 heures. Elle est systématique si ce dernier est en place depuis moins de 2 heures. Entre les deux elle peut être réalisée. Leurs recommandations ne sont pas très claires.
-----------------------------
Life-saving interventions take precedence over diagnostic maneuvers in the Care Under Fire stage of Tactical Combat Casualty Care. The immediate threat to life with an actively hemorrhaging extremity injury is addressed with the liberal and proper use of tourniquets. The emphasis on hemorrhage control has and will continue to result in the application of tourniquets that may not be needed past the Care Under Fire stage. As soon as tactically allowable, all tourniquets must be reassessed for conversion. Reassessment of all tourniquets should occur as soon as the tactical situation permits, but no more than 2 hours after initial placement. This article describes a procedure for qualified and trained medical personnel to safely convert extremity tourniquets to local wound dressings, using a systematic process in the field setting.
| Tags : tourniquet
01/12/2019
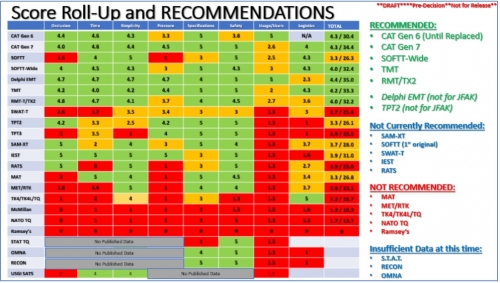
Quel tourniquet ?: Cela évolue, un peu
| Tags : tourniquet
08/10/2019
Formation au Tourniquet: Il faut mieux faire
High Tourniquet Failure Rates Among Non-Medical Personnel Do Not Improve with Tourniquet Training, Including Combat Stress Inoculation: A Randomized Controlled Trial.
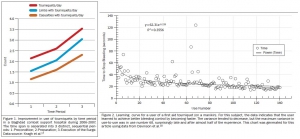
BACKGROUND:
The rate of failing to apply a tourniquet remains high.
HYPOTHESIS:
The study objective was to examine whether early advanced training under conditions that approximate combat conditions and provide stress inoculation improve competency, compared to the current educational program of non-medical personnel.
METHODS:
This was a randomized controlled trial. Male recruits of the armored corps were included in the study. During Combat Lifesaver training, recruits apply The Tourniquet 12 times. This educational program was used as the control group. The combat stress inoculation (CSI) group also included 12 tourniquet applications, albeit some of them in combat conditions such as low light and physical exertion. Three parameters defined success, and these parameters were measured by The Simulator: (1) applied pressure ≥ 200mmHg; (2) time to stop bleeding ≤ 60 seconds; and (3) placement up to 7.5cm above the amputation.
RESULTS:
Out of the participants, 138 were assigned to the control group and 167 were assigned to the CSI group. The overall failure rate was 80.33% (81.90% in the control group versus 79.00% in the CSI group; P value = .565; 95% confidence interval, 0.677 to 2.122). Differences in pressure, time to stop bleeding, or placement were not significant (95% confidence intervals, -17.283 to 23.404, -1.792 to 6.105, and 0.932 to 2.387, respectively).
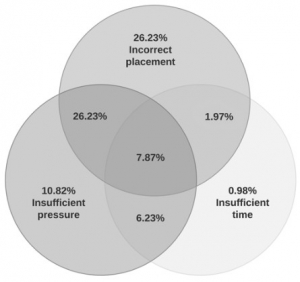
Tourniquet placement was incorrect in most of the applications (62.30%).
CONCLUSIONS:
This study found high rates of failure in tourniquet application immediately after successful completion of tourniquet training. These rates did not improve with tourniquet training, including CSI. The results may indicate that better tourniquet training methods should be pursued.
| Tags : tourniquet
06/08/2019
Garrot tactique: Oui, mais avec une réévaluation PRECOCE
Tactical tourniquet: Surgical management must be within 3 hours.
------------------------------------------
------------------------------------------
Despite longstanding controversy, tourniquets are widely used in tactical combat casualty care, with undisputed benefits for recent conflicts in Iraq and Afghanistan. Increased time delays are a particular issue in large areas, such as the Sahel-Saharan band. Complications associated with tourniquet use are predominantly related to acute ischemia with risk of amputation and ischaemia-reperfusion injury, as shown in the first clinical case. Often stated but poorly described, misuse of tourniquet and subsequent failure to interrupt arterial blood flow is also a clinical scenario that should be recognized. In the case of misuse of the tourniquet, more significant blood loss may be expected because of venous compression (« venous tourniquet », second clinical case). Early medical re-evaluation of the tourniquet is an essential component in prolonged field care. This includes reassessment of the tourniquet's ability to achieve hemostasis, abolish the downstream pulse and the relevance of the tourniquet altogether. This combat tool requires training to be successful and complications are time dependent. Tourniquet use requires appropriate application, re-evaluation and triage of wounded personnel within 3 h towards more structured surgical management.
| Tags : tourniquet
16/05/2019
Hémorragie: Garrot, mais aussi COMPRESSION
Bleeding control in combat fields with extreme transfer time

| Tags : tourniquet
02/05/2019
Apprendre à poser un garrot: En fait, pas si simple
Can they stop the bleed? Evaluation of tourniquet application by individuals with varying levels of prior self-reported training.
McCarty et Al. Injury. 2019 Jan;50(1):10-15. doi: 10.1016/j.injury.2018.09.041.
1 garrot sur 3 posé correctement malgré une formation ad-hoc.
--------------------------------------------------------
BACKGROUND:
Application of extremity tourniquets is a central tenet of multiple national initiatives to empower laypersons to provide hemorrhage control (HC). However, the efficacy of the general population who self-report prior first-aid (FA) or HC training on individual's ability to control bleeding with a tourniquet remains unknown. Therefore, the objective of this study was to assess the effectiveness of laypeople with self-reported prior FA or HC training to control bleeding with a tourniquet.
STUDY DESIGN:
Employees of a stadium were assessed via simulation in their ability to apply a Combat Application Tourniquet. As a subgroup analysis of a larger study, participants who self-reported: 1) No prior training, 2) FA training only or 2) FA + HC training were compared. Logistic regression adjusting for age, gender, education, willingness-to-assist, and comfort level in HC was performed.
RESULTS:
317 participants were included. Compared to participants with no prior training (14.4%,n = 16/111), those with FA training only (25.2%,n = 35/139) had a 2.12-higher odds (95%CI:1.07-4.18) of correct tourniquet application while those with FA + HC (35.8%,n = 24/67) had a 3.50-higher odds (95%CI:1.59-7.72) of correct application. Participants with prior FA + HC were more willing-to-assist and comfortable performing HC than those without prior training (p < 0.05).
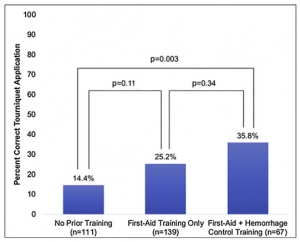
However, reporting being very willing-to-assist [OR0.83,95%CI:0.43-1.60] or very comfortable [OR1.11,95%CI:0.55-2.25] was not associated with correct tourniquet application.
CONCLUSION:
Self-reported prior FA + HC training, while associated with increased likelihood to correctly apply a tourniquet, results in only 1/3 of individuals correctly performing the skill. As work continues in empowering and training laypeople to act as immediate responders, these findings highlight the importance of effective layperson education techniques.
| Tags : tourniquet
26/04/2019
Bande de compression: Ne pas les vouer aux gémonies
Comparison of Two Tourniquets on a Mid-Thigh Model: The Israeli Silicone Stretch and Wrap Tourniquet vs. The Combat Application Tourniquet.
Le succès des garrots artériels tels que le SOFT-T et le CAT ne doit pas occulter l'intérêt des bandes de compression élastiques (Bande d'Esmach, SWAT-Tourniquet, IDF Silicone Tourniquet) préconisées en médecine rurale lors d'explosion de mines antipersonnelles (1). Ce travail met en avant leur efficacité.
-----------------------------------
Introduction:
Experience from recent conflicts underlines the dramatic impact of effective tourniquet use on combat casualty mortality. Although the Combat Application Tourniquet (CAT) is replacing the silicone band tourniquets (IST; "Israeli Silicone Tourniquet") in the Israeli Defense Forces, no direct comparison was made between them. The purpose of this study is to compare the performance of the two tourniquets on a mid-thigh model.
Methods:
Participants were Israeli military recruits who previously had the military first aid course. Each participant applied both the CAT and the IST. Applications were assessed by the HapMed Leg Tourniquet Trainer, which measured the applied pressure and the time required to reach it.

Results:
IST application resulted in higher rates of effective occlusion pressure compared with the CAT (91% vs. 73.1%, p < 0.01), and a higher mean occlusion pressure (41 mmHg, p < 0.01) was recorded using the IST. Among effective attempts, application time did not differ significantly between the tourniquets.
Effect of Elapsed Time Since First Aid Course on Success Rate
| Experience More Than 1 mo (n = 15) | Experience Equal to or Less Than 1 mo (n = 63) | p-Value | |
|---|---|---|---|
| Succeeded with CAT, n (%) | 7 (46.7) | 50 (79.4) | 0.01 |
| Succeeded with IST, n (%) | 14 (93.3) | 57 (90.5) | 0.5 |
Conclusion:
The IST was superior to the CAT in producing effective occlusion pressure while not prolonging application time. These results may indicate that the IST remains a valid option for controlling mid-thigh bleeding.
| Tags : tourniquet
21/07/2018
+ d'1 Tourniquet et 1/4 converti
Point of injury tourniquet application during Operation Protective Edge-What do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate- and short-term outcomes of point of injury (POI) tourniquet applications during "Operation Protective Edge" (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications, and short-term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps treated 704 casualties. Of these, 90 casualties were treated with 119 tourniquets of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88 of 90) of the casualties. Injuries sustained from improvised explosive devices and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p = 0.034). The success rate of the first tourniquet was reported to be 70% (84 of 119), regardless of caregiver level (p = 0.56), tourniquet type (p = 0.16), or limb characters (p = 0.48). Twenty-seven (25.7%) of 105 of the tourniquets were converted to direct pressure dressings enroute to receiving hospitals two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on eight casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5 of 85), no vascular involvement was discovered during surgery, and the fasciotomy is suspected as tourniquet related. 7%) 6 of 85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10 of 85) (one patient had both fasciotomy and neural complication without vascular injury).
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity, whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet
01/05/2018
Tourniquet: Une vieille histoire
A brief history of the tourniquet
Welling DR et Al. Vasc Surg 2012;55:286-90
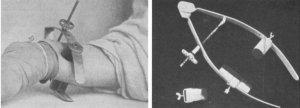
Le compresseur de Matas
| Tags : tourniquet
03/12/2017
Garrot: Pas si simple sans formation
The Tourniquet Gap: A Pilot Study of the Intuitive Placement of Three Tourniquet Types by Laypersons
Ross EM et Al. http://dx.doi.org/10.1016/j.jemermed.2017.09.011
--------------------------
La pose de garrot par l'intervenant le plus proche d'une victime blessé semble être une évidence. Pourtant ce travail met en évidence un taux relativement important d'échec. Ceci milite pour la conduite de campagne de formation avant toute mise à disposition de garrot industriel
--------------------------
Objectives
The objective of this pilot study was to determine which tourniquet type was the most intuitive for a layperson to apply correctly.
Methods
This project is a randomized study derived from a “Stop the Bleed” education initiative conducted between September 2016 and March 2017. Novice tourniquet users were randomized to apply one of three commercially available tourniquets (Combat Action Tourniquet [CAT; North American Rescue, LLC, Greer, SC], Ratcheting Medical Tourniquet [RMT; m2 Inc., Winooski, VT], or Stretch Wrap and Tuck Tourniquet [SWAT-T; TEMS Solutions, LLC, Salida, CO]) in a controlled setting. Individuals with formal medical certification, prior military service, or prior training with tourniquets were excluded. The primary outcome of this study was successful tourniquet placement.
Results
Of 236 possible participants, 198 met the eligibility criteria. Demographics were similar across groups. The rates of successful tourniquet application for the CAT, RMT, and SWAT-T were 16.9%, 23.4%, and 10.6%, respectively ( p = 0.149). The most common causes of application failure were: inadequate tightness (74.1%), improper placement technique (44.4%), and incorrect positioning (16.7%).
Conclusion
Our pilot study on the intuitive nature of applying commercially available tourniquets found unacceptably high rates of failure. Large-scale community education efforts and manufacturer improvements of tourniquet usability by the lay public must be made before the widespread dissemination of tourniquets will have a significant public health effect.
| Tags : tourniquet
31/08/2017
Tourniquet: Bien en contexte civil AUSSI
The trauma center is too late: Major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock
Scerbo MH et Al. Journal of Trauma and Acute Care Surgery,10.1097/TA.0000000000001666
Background: To date, no civilian studies have demonstrated that pre-hospital (PH) tourniquets improve survival. We hypothesized that late, trauma center (TC) tourniquet use would increase death from hemorrhagic shock compared to early (PH) placement.
Methods: All patients arriving to a Level-1, urban TC between 10/2008 and 01/2016 with a tourniquet placed prior to (T-PH) or after arrival to the TC (T-TC) were evaluated. Cases were assigned the following designations: indicated [absolute indication (vascular injury requiring repair/ligation, operation within 2 hours for extremity injury, or traumatic amputation), or relative indication (major musculoskeletal/soft-tissue injury requiring operation 2-8 hours after arrival, documented large blood loss)], or non-indicated. Outcomes were death from hemorrhagic shock, physiology upon arrival to the TC and massive transfusion requirements. Following univariate analysis, logistic regression was carried out to assess independent predictors of death from hemorrhagic shock.
Results: 306 patients received 326 tourniquets for injuries to 157 upper and 147 lower extremities. 281 (92%) had an indication for placement. 70% of patients had a blunt mechanism of injury. T-TC patients arrived with a lower systolic blood pressure [101 (86, 123) versus 125 (100, 145)mmHg, p<0.001], received more transfusions in the first hour of arrival (55% versus 34%, p=0.02) and had a greater mortality from hemorrhagic shock (14% vs. 3.0%, p=0.01). When controlling for year of admission, mechanism of injury and shock upon arrival (SBP ≤90mmHg or HR ≥120 bpm or base deficit ≤ 4), indicated T-TC had a 4.5-fold increased odds of death compared to T-PH [OR 4.5, 95% CI 1.23-16.4, p=0.02)].
Conclusions: Waiting until TC arrival to control hemorrhage with a tourniquet was associated with worsened blood pressure and increased transfusion within the first hour of arrival. In routine civilian trauma patients, delaying to T-TC was associated with 4.5-fold increased odds of mortality from hemorrhagic shock
| Tags : tourniquet
21/07/2017
SOFT-Tourniquet: Du nouveau
Tactical Médical Solutions qui est le fabricant du SOFT-Tourniquet, garrot en dotation dans l'armée française, propose une nouvelle version de son garrot Wide. Sa nouvelle boucle est d'emploi bien plus aisé que la précédente et positionne ce garrot parmi les tous meilleurs(CAT, SOFT-T, TK4,...)

Clic sur l'image pour accéder au site. Le distributeur en France.
| Tags : tourniquet
29/04/2017
Une ceinture pour tourniquet ? Plutôt l'inverse.
Belts Evaluated as Limb Tourniquets: BELT Study Comparing Trouser Supporters Used as Medical Devices in a Manikin Model of Wound Bleeding.
Bequette BW et Al Wilderness Environ Med. 2017 Apr 19. pii: S1080-6032(17)30060-1.
--------------------------------
Une idée, qui n'est pas nouvelle de même que celui de pantalon intégrant un garrot (1), mais on devrait plutôt dire un tourniquet pour ceinture. Ce travail est par ailleurs intéressant car il aborde la problématique des garrots insuffisamment serrés.
--------------------------------
OBJECTIVE:
The purpose of the present study is to compare several models of commercially designed belts as used as a tourniquet.
METHODS:
In the Belts Evaluated as Limb Tourniquets (BELT) study, an experiment was designed to test the effectiveness of pants belts as non improvised medical devices to control hemorrhage in a manikin. Models of belts included Tourni-belt, Tourniquet Belt, ParaBelt, and Battle Buddy. Data collected included effectiveness, time to stop bleeding, total time of application, pressure, blood loss, and composite results (score count of good results; composite outcome good if every component was good).
RESULTS:
Differences in effectiveness percentages among models were not statistically significant. The difference in mean between users was statistically significant for stop time, total time, pressure, blood loss, composite score, and composite outcome. Mean time to stop bleeding differed for only 1 pair of models after the Tukey-Kramer adjustment; ParaBelt was faster than Tourniquet Belt. Mean total time of application differed between ParaBelt-Tourniquet Belt and Tourni-belt-Tourniquet Belt; the former model in both pairs was faster. No significant difference in mean blood loss measured by model was found. For composite outcome score, no pairwise difference between models was significant. For composite outcome (good-bad), ParaBelt had good results in 75% of tests; the other 3 models had significantly worse results.
CONCLUSIONS:
In a preliminary laboratory analysis of belt tourniquet models using a manikin, performance differed by model. ParaBelt performed better than other models for the composite outcome.our tourniquet ?
| Tags : tourniquet
11/04/2017
Tourniquet: Les israéliens, pour +++
Point of injury tourniquet application during Operation Protective Edge - what do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate and short term outcomes of point of injury (POI) tourniquet applications during 'Operation Protective Edge' (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications and short term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps (IDF-MC) treated 704 casualties. Out of these, 90 casualties were treated with 119 tourniquets out of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88/90) of the casualties. Injuries sustained from Improvised explosive devices (IED) and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p=0.034). The success rate of the first tourniquet was reported to be 70% (84/119), regardless of caregiver level (P=0.56), tourniquet type (P=0.16) or limb characters (p=0.48). two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on 8 casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5/85) no vascular involvement was discovered during surgery and the fasciotomy is suspected as tourniquet related. 7%) 6/85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10/85) (one patient had both fasciotomy and neural complication without vascular injury)
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet
17/03/2017
Tourniquet: La nouveauté de SamMedical
SAM Tourniquet XT
Un garrot, dont l'intérêt apparaît être d'une part sur sa largeur et d'autre part sur sa boucle de serrage innovante.
Clic sur l'image pour accéder à une vidéo
| Tags : tourniquet
14/03/2017
Tourniquet: Attention
-------------------
La pose d'un garrot est essentiel à la survie d'un blessé présentant une hémorragie sévère des membres. Encore faut-il qu'il soit de bonne qualité. Les autorités sanitaires américaines insistent sur l'importance de ne se fournir qu'auprès de distributeurs connues distribuant des garrots éprouvés plutôt que de céder aux sirènes de la copie chinoise de basse qualité. En effet même ces garrots voient leur efficacité réduite après exposition aux conditions de combat. C'est ce que met une fois de plus en évidence ce travail.
-------------------
BACKGROUND:
The purpose of the present study was to mechanically assess models of emergency tourniquet after 18 months of environmental exposure to weather to better understand risk of component damage.
MATERIALS AND METHODS:
An experiment was designed to test tourniquet performance on a manikin thigh. Three tourniquet models were assessed: Special Operations Forces Tactical Tourniquet Wide, Ratcheting Medical Tourniquet, and Combat Application Tourniquet. Unexposed tourniquets formed a control group stored in a laboratory; exposed tourniquets were placed outdoors on a metal roof for 18 months in San Antonio, Texas. Two users, a military cadet and a scientist, made 300 assessments in total. Assessment included major damage (yes-no), effectiveness (hemorrhage control, yes-no), casualty survival (alive-dead), time to stop bleeding, pressure, and blood loss. Time, pressure, and blood loss were reported in tests with effectiveness.
RESULTS:
Exposed devices had worse results than unexposed devices for major damage (3% [4/150] versus 0% [0/150]; ρ = .018), effectiveness (89% versus 99%; ρ = .002), and survival of casualties (89% versus 100%; ρ < .001). In tests for effectiveness, exposed devices had worse results than unexposed devices for time to stop bleeding (29 seconds versus 26 seconds; ρ = .01) and pressure (200mmHg versus 204mmHg; ρ = .03, respectively), but blood loss volume did not differ significantly.
CONCLUSION:
Compared with unexposed control devices, environmentally exposed tourniquets had worse results in tests of component damage, effectiveness, and casualty survival.
| Tags : tourniquet
16/02/2017
TMT tourniquet: Un nouveau venu
Un nouveau venu qui fait aussi bien que la référence US, à savoir le CAT, sans apporter plus (1). Ne pas confondre ce garrot dont le distributeur est connu et dont la fabrication parfaitement tracée. Sans aucune comparaison avec nombre de copies qui ne bénéficient pas des mêmes contrôle de qualité distribués à moins de 10 Euros et qui peuvent faire illusion.

| Tags : tourniquet
08/02/2017
Tourniquets contrefaits = DANGER
DANGER
Les événements récents ont mis en avant l'importance de l'application précoce de garrot. L'approvisionnement en garrot est un véritable challenge et un marché où la guerre commerciale fait maintenant rage. Si le nombre de fabricants historiques de garrot était relativement restreint (CAT, SOFT-T, TK4, RATS, MAT, SWAT), on voit fleurir nombre de copies essentiellement chinoises dont il est relativement aisé de se procurer des exemplaires, notamment sur le marché de l'AIRSOFT. Deux fabricants sont particulièrement la cible de ces contrefacteurs CAT ressources et TACMED solutions, car ce sont les deux garrots validés par les US dans le cadre du TCCC. Ces deux fabricants diffusent leurs produits pour une 20aines d'euros. Le garrot en service dans l'armée française depuis une dizaine d'année est le SOFT-T de la société TACMED, garrot dont il existe une version adaptée pour l'enfant. Les contrefacteurs chinois affichent des tarifs parfois 10 fois moindres. Les produits proposés par ces sociétés ne peuvent pas disposer des qualités techniques de même niveau que ceux détenus par les originaux. Un aspect important des garrots est leur résistance au vieillissement, aux intempéries, au froid, aux UV. Il a été démontré que ces caractéristiques sont très importantes en terme d'efficacité après quelques mois de port du garrot en ambiance opérationnelle vraie. Il serait étonnant que ces copies de garrot, dont les matières premières et les circuits de fabrication sont pour le moins opaques offrent les mêmes garanties de sécurité que ceux de fabricants historiques maîtrisant tous les process de fabrication de leur production.
Par ailleurs il semblerait que les conditions des certifications CE et ISO 134 (1,2,3)85 soit sujettes à caution car en partie relevant d'une autocertification.
Les autorités américaines ne sont saisies de ce problème et rappellent l'importance de ne s'approvisionner que chez les forunisseurs des garrots validés dans le T3C, à savoir les garrots produits apr CAT ressources et TacMed Solutions en excluant toute autre production au prétexte de tarifs à première vue (tro) alléchants. Lire le rapport de la FDA
Je vous propose dans le lien suivant quelques exemples concernant le garrot SOFT-T
Matériel Tourniquet Contrefaçons.pdf
Certains modèles de tourniquet s'inspirent très fortement de ces produits et en particulier du SOF-T (notamment le wide) mais avec une démarche d' innovation réelle. Aussi ces tourniquets sont ils différents de simples copies et très probablement de bonne qualité. Ils ne sont pas produits en chine mais dans des pays de l'Est européen, voire en Russie (a,b). On manque néanmoins de recul d'expertise technique de ces derniers.
Dans l'état actuel des choses, à moins de s'équiper pour de l'airsoft, la prudence est de rester à l'écart des ces garrots et de continuer à utiliser les produits distribués par les fournisseurs reconnus des fabricants historiques (4, 5,6)
| Tags : tourniquet
11/11/2016
15 ans d'emploi du tourniquet: Que dire ?
Battlefield Tourniquets: Lessons Learned in Moving Current Care Toward Best Care in an Army Medical Department at War
Kragh JF Jr et Al. US Army Med Dep J. 2016 Apr-Sep;(2-16):29-36.
------------------------------
Un point d'étape qui insiste sans surprise sur l'apport d'une pose précoce d'un garrot. Précoce mais aussi rapide: 25 secondes sont nécessaires aux plus entraînés mais c'est 20 secondes de trop. Plus on s'entraîne et plus vite ET mieux on pose ce garrot.
------------------------------
Bleeding prevention and control by tourniquet use by out-of-hospital caregivers is a major breakthrough in military medicine of current wars. The present review documents developments in tourniquet practices since 2001 among the US military services for aid in improving doctrine, policy, and especially care in wars to come. Tourniquets are an adjunct for resuscitation in self-care and buddy aid and today are issued to all military service persons who deploy into a combat zone. In the US Army, virtually every Soldier is trained in first aid tourniquet use; since 2009 they are instructed early and often to use them early and often. Despite substantial knowledge gains among the services in tourniquet use and resulting improvements in casualty survival, current evidence shows persistent diffi culties in achieving best care with tourniquet use for individual trauma patients. Nevertheless, contemporary tourniquet use incorporates key lessons learned over the last 14 years of war that include: (1) tourniquet use reliably stops bleeding from limb wounds and prevents mortality in prehospital settings; and (2) brief tourniquet use appears to be safe. These 2 lessons have become so evident that civilian emergency medical systems have begun using them, albeit unevenly. Collection and interpretation of data of casualties with tourniquet use have showed that such intervention has lifesaving benefit through 2 mechanisms: control of both ongoing hemorrhage and shock severity. The next generation of interventions in bleeding control involves developing the skill sets, education, and standards of tourniquet users which may improve hemorrhage control in wars to come
| Tags : tourniquet