01/02/2017
Echo: Pour le thorax surtout
Traumatic cardiac injury: Experience from a level-1 trauma centre
Mishra B. et Al. Chin J Traumatol. 2016 Dec 1;19(6):333-336.
--------------------------------------
Disposer d'un appareil d'échographie est d'un grand intérêt. Encore faut-il maîtriser cette technique (1) sous peine de se tromper dans les priorités de prise en charge. Le recours a cette technique reste débattu pour la prise en charge de traumatismes pénétrants. L'échographie thoracique est probablement à valeur ajoutée tant sur l'imagerie pleurale que péricardique. C'est ce que présente ce travail. Ce document rapporte également l'inefficacité en terme de survie de péricardocentèse pourtant prôné par l'ATLS.
--------------------------------------
Traumatic cardiac injury (TCI) is a challenge for trauma surgeons as it provides a short thera- peutic window and the management is often dictated by the underlying mechanism and hemodynamic status. The current study is to evaluate the factors influencing the outcome of TCI.
METHODS:
Prospectively maintained database of TCI cases admitted at a Level-1 trauma center from July 2008 to June 2013 was retrospectively analyzed. Hospital records were reviewed and statistical analysis was performed using the SPSS version 15.
RESULTS:
Out of 21 cases of TCI, 6 (28.6%) had isolated and 15 (71.4%) had associated injuries. Ratio be- tween blunt and penetrating injuries was 2:1 with male preponderance. Mean ISS was 31.95. Thirteen patients (62%) presented with features suggestive of shock. Cardiac tamponade was present in 12 (57%) cases and pericardiocentesis was done in only 6 cases of them. Overall 19 patients underwent surgery. Perioperatively 8 (38.1%) patients developed cardiac arrest and 7 developed cardiac arrhythmia. Overall survival rate was 71.4%. Mortality was related to cardiac arrest (p = 0.014), arrhythmia (p = 0.014), and hemorrhagic shock (p =0.04). The diagnostic accuracy of focused assessment by sonography in trauma (FAST) was 95.24%.
CONCLUSION:
High index of clinical suspicion based on the mechanism of injury, meticulous examination by FAST and early intervention could improve the overall outcome.
Trauma: Le terrorisme + grave que la violence
Violence-related Versus Terror-related Stabbings: Significant Differences in Injury Characteristics.
OBJECTIVE:
To demonstrate the gap between injury epidemiology of terror-related stabbings (TRS) and non-terror-related intentional stabbings.
BACKGROUND:
Terror attacks with sharp instruments have multiplied recently, with many victims of these incidents presented to hospitals with penetrating injuries. Because most practical experience of surgeons with intentional stabbing injuries comes from treating victims of interpersonal violence, potential gaps in knowledge may exist if injuries from TRS significantly differ from interpersonal stabbings (IPS).
METHODS:
A retrospective study of 1615 patients from intentional stabbing events recorded in the Israeli National Trauma Registry during the period of "Knife Intifada" (January 2013-March 2016). All stabbings were divided into TRS and IPS. The 2 categories were compared in terms of sustained injuries, utilization of hospital resources, and clinical outcomes.
RESULTS:
TRS patients were older, comprised more females and were ethnically homogenous. Most IPS incidents happened on weekdays and at night hours, whereas TRS events peaked midweek during morning and afternoon hours. TRS patients had more injuries of head, face, and neck, and severe head and neck injuries. IPS patients had more abdomen injuries; however, respective injuries in the TRS group were more severe. Greater injury severity of the TRS patients reflected on their higher hospital resources utilization and greater in-hospital mortality.
CONCLUSIONS:
Victims of terror stabbings are profoundly different in their characteristics, sustain injuries of a different profile and greater severity, require more hospital resources, and have worse off clinical outcomes, emphasizing the need of the healthcare systems to adjust itself appropriately to deal successfully with future terror attacks.
10/12/2016
Maintenir la pression: Hydroxocobalamine ou adré ?
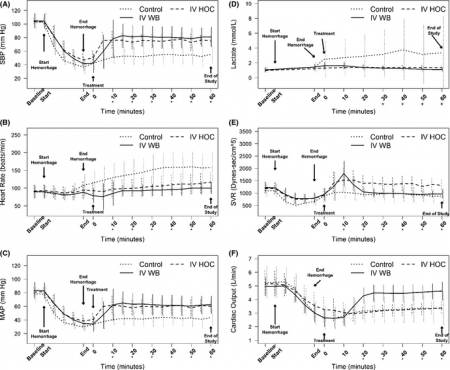
A prospective, randomized trial of intravenous hydroxocobalamin versus whole blood transfusion compared to no treatment for Class III hemorrhagic shock resuscitation in a prehospital swine model.
OBJECTIVES:
The objective was to compare systolic blood pressure (sBP) over time in swine that have had 30% of their blood volume removed (Class III shock) and treated with intravenous (IV) whole blood or IV hydroxocobalamin, compared to nontreated controlanimals.
METHODS:
Thirty swine (45 to 55 kg) were anesthetized, intubated, and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged a total of 20 mL/kg over a 20-minute period. Five minutes after hemorrhage, animals were randomly assigned to receive 150 mg/kg IV hydroxocobalamin solubilized in 180 mL of saline, 500 mL of whole blood, or no treatment. Animals were monitored for 60 minutes thereafter. A sample size of 10 animals per group was determined based on a power of 80% and an alpha of 0.05 to detect an effect size of at least a 0.25 difference (>1 standard deviation) in mean sBP between groups. sBP values were analyzed using repeated-measures analysis of variance (RANOVA). Secondary outcome data were analyzed using repeated-measures multivariate analysis of variance (RMANOVA).
RESULTS:
There were no significant differences between hemodynamic parameters of IV hydroxocobalamin versus whole blood versus control group at baseline (MANOVA; Wilks' lambda; p = 0.868) or immediately posthemorrhage (mean sBP = 47 mm Hg vs. 41 mm Hg vs. 37 mm Hg; mean arterial pressure = 39 mm Hg vs. 28 mm Hg vs. 34 mm Hg; mean serum lactate = 1.2 mmol/L vs. 1.4 mmol/L vs. 1.4 mmol/L; MANOVA; Wilks' lambda; p = 0.348). The outcome RANOVA model detected a significant difference by time between groups (p < 0.001). Specifically, 10 minutes after treatment, treated animals showed a significant increase in mean sBP compared to nontreated animals (mean sBP = 76.3 mm Hg vs. 85.7 mm Hg vs. 51.1 mm Hg; p < 0.001). RMANOVA modeling of the secondary data detected a significant difference in mean arterial pressure, heart rate, and serum lactate (p < 0.001). Similar to sBP, 10 minutes after treatment, treated animals showed a significant increase in mean arterial pressure compared to nontreated animals (mean arterial pressure = 67.7 mm Hg vs. 61.4 mm Hg vs. 40.5 mm Hg). By 10 minutes, mean heart rate was significantly slower in treated animals compared to nontreated animals (mean heart rate = 97.3 beats/min vs. 95.2 beats/min vs. 129.5 beats/min; p < 0.05). Serum lactate, an early predictor of shock, continued to rise in the control group, whereas it did not in treated animals. Thirty minutes after treatment, serum lactate values of treated animals were significantly lower compared to nontreated animals (p < 0.05). This trend continued throughout the 60-minute observation period such that 60-minute values for lactate were 1.4 mmol/L versus 1.1 mmol/L versus 3.8 mmol/L. IV hydroxocobalamin produced a statistically significant increase in systemic vascular resistance compared to control, but not whole blood, with a concomitant decrease in cardiac output.
CONCLUSIONS:
Intravenous hydroxocobalamin was more effective than no treatment and as effective as whole blood transfusion, in reversing hypotension and inhibiting rises in serum lactate in this prehospital, controlled, Class III swine hemorrhage model.
| Tags : choc
Tueries massives par armes à feu: Penser différemment !
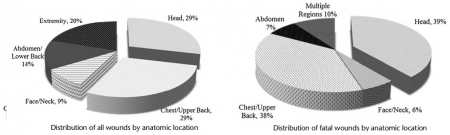
The profile of wounding in civilian public mass shooting fatalities.
BACKGROUND:
The incidence and severity of civilian public mass shootings (CPMS) continue to r.ise. Initiatives predicated on lessons learned from military woundings have placed strong emphasis on hemorrhage control, especially via use of tourniquets, as means to improve survival. We hypothesize that both the overall wounding pattern and the specific fatal wounds in CPMS events are different from those in military combat fatalities and thus may require a new management strategy.
METHODS:
A retrospective study of autopsy reports for all victims involved in 12 CPMS events was performed. Civilian public mass shootings was defined using the FBI and the Congressional Research Service definition. The site of injury, probable site of fatal injury, and presence of potentially survivable injury (defined as survival if prehospital care is provided within 10 minutes and trauma center care within 60 minutes of injury) was determined independently by each author.
RESULTS:
A total 139 fatalities consisting of 371 wounds from 12 CPMS events were reviewed. All wounds were due to gunshots. Victims had an average of 2.7 gunshots. Relative to military reports, the case fatality rate was significantly higher, and incidence of potentially survivable injuries was significantly lower. Overall, 58% of victims had gunshots to the head and chest, and only 20% had extremity wounds. The probable site of fatal wounding was the head or chest in 77% of cases.
Only 7% of victims had potentially survivable wounds. The most common site of potentially survivable injury was the chest (89%). No head injury was potentially survivable. There were no deaths due to exsanguination from an extremity.
CONCLUSION:
The overall and fatal wounding patterns following CPMS are different from those resulting from combat operations. Given that no deaths were due to extremity hemorrhage, a treatment strategy that goes beyond use of tourniquets is needed to rescue the few victims with potentially survivable injuries.
24/09/2016
Transfusion en vol: Sécurité assurée
Risk Management Analysis of Air Ambulance Blood Product Administration in Combat Operations
BACKGROUND:
Between June-October 2012, 61 flight-medic-directed transfusions took place aboard U.S. Army Medical Evacuation (medevac) helicopters in Afghanistan. This represents the initial experience for pre-hospital blood product transfusion by U.S. Army flight medics.
METHODS:
We performed a retrospective review of clinical records, operating guidelines, after-action reviews, decision and information briefs, bimonthly medical conferences, and medevac-related medical records.
RESULTS:
A successful program was administered at 10 locations across Afghanistan. Adherence to protocol transfusion indications was 97%. There were 61 casualties who were transfused without any known instance of adverse reaction or local blood product wastage. Shock index (heart rate/systolic blood pressure) improved significantly en route, with a median shock index of 1.6 (IQR 1.2-2.0) pre-transfusion and 1.1 (IQR 1.0-1.5) post-transfusion (P < 0.0001). Blood resupply, training, and clinical procedures were standardized across each of the 10 areas of medevacoperations.
DISCUSSION:
Potential risks of medical complications, reverse propaganda, adherence to protocol, and diversion and/or wastage of limited resources were important considerations in the development of the pilot program. Aviation-specific risk mitigation strategies were important to ensure mission success in terms of wastage prevention, standardized operations at multiple locations, and prevention of adverse clinical outcomes. Consideration of aviation risk mitigation strategies may help enable other helicopter emergency medical systems to develop remote pre-hospital transfusion capability. This pilot program provides preliminary evidence that blood product administration by medevac is safe.
| Tags : transfusion
22/09/2016
SmO2: Utile ?
Muscle Oxygen Saturation Improves Diagnostic Association Between Initial Vital Signs and Major Hemorrhage: A Prospective Observational Study.
L'hémorragie reste la cause principale des décès évitable et l'importance de la mise en oeuvre d'une stratégie transfusionnelle précoce est actée. Mais sur quels critères. Au delà des critères cliniques simples, on peut citer le recours au suivi des lactates. Le suivi de paramètres d'oxygénation tissulaire simple est maintenant possible. Ce qu'évoque ce document est l'emploi de la SmO2, élément déjà utilisé en médecine du sport. Le recours à un tel paramètre est donc potentiellement très intéressant si cette pertinence était confirmée et sa mesure valide avec des outils simples.
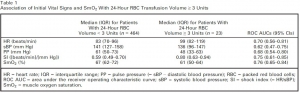
OBJECTIVES:
During initial assessment of trauma patients, vital signs do not identify all patients with life-threatening hemorrhage. We hypothesized that a novel vital sign, muscle oxygen saturation (SmO2 ), could provide independent diagnostic information beyond routine vital signs for identification of hemorrhaging patients who require packed red blood cell (RBC) transfusion.
METHODS:
This was an observational study of adult trauma patients treated at a Level I trauma center. Study staff placed the CareGuide 1100 tissue oximeter (Reflectance Medical Inc., Westborough, MA), and we analyzed average values of SmO2 , systolic blood pressure (sBP), pulse pressure (PP), and heart rate (HR) during 10 minutes of early emergency department evaluation. We excluded subjects without a full set of vital signs during the observation interval. The study outcome was hemorrhagic injury and RBC transfusion ≥ 3 units in 24 hours (24-hr RBC ≥ 3). To test the hypothesis that SmO2 added independent information beyond routine vital signs, we developed one logistic regression model with HR, sBP, and PP and one with SmO2 in addition to HR, sBP, and PP and compared their areas under receiver operating characteristic curves (ROC AUCs) using DeLong's test.
RESULTS:
We enrolled 487 subjects; 23 received 24-hr RBC ≥ 3. Compared to the model without SmO2 , the regression model with SmO2 had a significantly increased ROC AUC for the prediction of ≥ 3 units of 24-hr RBC volume, 0.85 (95% confidence interval [CI], 0.75-0.91) versus 0.77 (95% CI, 0.66-0.86; p < 0.05 per DeLong's test). Results were similar for ROC AUCs predicting patients (n = 11) receiving 24-hr RBC ≥ 9.
CONCLUSIONS:
SmO2 significantly improved the diagnostic association between initial vital signs and hemorrhagic injury with blood transfusion. This parameter may enhance the early identification of patients who require blood products for life-threatening hemorrhage.
12/09/2016
L'hôpital de proximité: Insuffisant ?
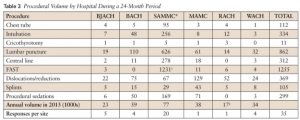
Garrison Clinical Setting Inadequate for Maintenance of Procedural Skills for Emergency Medicine Physicians: A Cross-Sectional Study
Schauer SG et Al. J Spec Oper Med. 2015 Winter;15(4):67-70
----------------------------------------
Lire également cet éditorial qui pointe l'insuffisance de l'exercice en hôpital de proximité avec le rôle important que peut jouer la simulation. Les auteurs proposent un maintien longitudinal des compétences avec des minima en termes de pratiques gestuelles avant projection.
----------------------------------------
BACKGROUND:
Emergency medicine physicians (EPs) are often placed in far-forward, isolated areas in theater. Maintenance of their emergency intervention skills is vital to okeep the medical forces deployment ready. The US Army suggests that working at a Military Treatment Facility (MTF) is sufficient t keep emergency procedural skills at a deployment-ready level. We sought to compare the volume of emergency procedures that providers reported necessary to maintain their skills with the number available in the MTF setting.
METHODS:
EPs were surveyed to quantify the number of procedures they reported they would need to perform yearly to stay deployment-ready. We obtained procedure data for their duty stations and compared the procedure volume with the survey responses to determine if working at an MTF is sufficient to keep providers' skills deployment ready.
RESULTS:
The reported necessary average numbers per year were as follows: tube thoracostomy (5.9), intubation (11.4), cricothyrotomy (4.2), lumbar puncture (5.2), central line (10.0), focused assessment with sonography for trauma (FAST) (21.3), reductions (10.6), splints (10.5), and sedations (11.7). None of the procedure volumes at MTFs met provider requirements with the exception of FAST examinations at the only trauma center.
CONCLUSIONS:
This suggests the garrison clinical environment is inadequate for maintaining procedure skills. Further research is needed to determine modalities that will provide adequate training volume.
01/09/2016
Trauma sévère: Un docteur sur scène. Et bien pas évident ?
Does the presence of an emergency physician influence pre-hospital time, pre-hospital interventions and the mortality of severely injured patients? A matched-pair analysis based on the trauma registry of the German Trauma Society (TraumaRegister DGU®)
Bieler D. et Al. http://dx.doi.org/10.1016/j.injury.2016.08.015
------------------------------------
Une remise en question un peu étonnante de la médicalisation préhospitalière par nos camarades allemands. L'augmentation globale de la qualité des intervenants et de l'organisation explique probablement les résultats de cette analyse.
------------------------------------
Purpose
The role of emergency physicians in the pre-hospital management of severely injured patients remains controversial. In Germany and Austria, an emergency physician is present at the scene of an emergency situation or is called to such a scene in order to provide pre-hospital care to severely injured patients in approximately 95% of all cases. By contrast, in the United States and the United Kingdom, paramedics, i.e. non-physician teams, usually provide care to an injured person both at the scene of an incident and en route to an appropriate hospital. We investigated whether physician or non-physician care offers more benefits and what type of on-site care improves outcome.
Material and methods
In a matched-pair analysis using data from the trauma registry of the German Trauma Society, we retrospectively (2002–2011) analysed the pre-hospital management of severely injured patients (ISS ≥16) by physician and non-physician teams. Matching criteria were age, overall injury severity, the presence of relevant injuries to the head, chest, abdomen or extremities, the cause of trauma, the level of consciousness, and the presence of shock.
Results
Each of the two groups, i.e. patients who were attended by an emergency physician and those who received non-physician care, consisted of 1235 subjects.
There was no significant difference between the two groups in pre-hospital time (61.1 [SD 28.9] minutes for the physician group and 61.9 [SD 30.9] minutes for non-physician group).
Significant differences were found in the number of pre-hospital procedures such as fluid administration, analgosedation and intubation. There was a highly significant difference (p < 0.001) in the number of patients who received no intervention at all applying to 348 patients (28.2%) treated by non-physician teams and to only 31 patients (2.5%) in the physician-treated group.
By contrast, there was no significant difference in mortality within the first 24 h and in mortality during hospitalisation.
Conclusion
This retrospective analysis does not allow definitive conclusions to be drawn about the optimal model of pre-hospital care. It shows, however, that there was no significant difference in mortality although patients who were attended by non-physician teams received fewer pre-hospital interventions with similar scene times
Remote damage control resuscitation: ???
THOR Position Paper on Remote Damage Control Resuscitation: Definitions, Current Practice and Knowledge Gaps
Jenkins DH et Al. Shock. 2014 May; 41(0 1): 3–12.
The concept of RDCR is in its infancy and there is a significant amount of work that needs to be done to improve outcomes for patients with life-threatening bleeding secondary to injury. The pre-hospital phase of their resuscitation is critical and if shock and coagulopathy can be rapidly identified and corrected prior to hospital admission this will likely reduce morbidity and mortality. The THOR Network is committed to improving outcomes for patients with traumatic injury through education, training and research. This position statement begins to standardize the terms used, provides an acceptable range of therapeutic options, and identifies the major knowledge gaps in the field.
27/08/2016
Interventions salvatrices: Bien sûr mais lesquelles ?
Major incident triage: A consensus based definition of the essential life-saving interventions during the definitive care phase of a major incident
Vassallo J. et Al. Injury, Int. J. Care Injured 47 (2016) 1898–190
-------------------------
Plus le contexte d'intervention est difficile soit du fait de l'environnement soit du fait du danger tactique et plus le choix des nterventions médicales doit être réflechi et restreint et mis en oeuvre par uintervenant pas forcément médecin mas formé spécifiquement à la pratique d'une action nécessaire à la survie. Ce travail identiife ainsi une trentaine de conduites essentielles à un réseau de traumatisés graves. Lire aussi cet article
-------------------------
Introduction: Triage is a key principle in the effective management of major incidents. The process currently relies on algorithms assigning patients to specific triage categories; there is, however, little guidance as to what these categories represent. Previously, these algorithms were validated against injury severity scores, but it is accepted now that the need for life-saving intervention is a more important outcome. However, the definition of a life-saving intervention is unclear. The aim of this study was to define what constitutes a life-saving intervention, in order to facilitate the definition of an adult priority one patient during the definitive care phase of a major incident.
Methods: We conducted a modified Delphi study, using a panel of subject matter experts drawn from the United Kingdom and Republic of South Africa with a background in Emergency Care or Major Incident Management. The study was conducted using an online survey tool, over three rounds between July and December 2013. A four point Likert scale was used to seek consensus for 50 possible interventions, with a consensus level set at 70%.
Results: 24 participants completed all three rounds of the Delphi, with 32 life-saving interventions reaching consensus.
Conclusions: This study provides a consensus definition of what constitutes a life-saving intervention in the context of an adult, priority one patient during the definitive care phase of a major incident. The definition will contribute to further research into major incident triage, specifically in terms of validation of an adult major incident triage tool.
| Results of the Delphi Process – Life-Saving Interventions. | |
| 1 | Intubation for actual airway obstruction |
| 2 | Intubation for impending airway obstruction |
| 3 | Surgical airway for airway obstruction |
| 4 | Surgical airway for impending airway obstruction |
| 5 | Needle thoracocentesis |
| 6 | Finger thoracostomy |
| 7 | Tube thoracostomy |
| 8 | Application of a chest seal (commercial/improvised) |
| 9 | Positive Pressure Ventilation for ventilatory inadequacy |
| 10 | Application of a tourniquet for haemorrhage control |
| 11 | Use of haemostatic agents for haemorrhage control |
| 12 | Insertion of an intra-osseous device for resuscitation purposes |
| 13 | Receiving uncross-matched blood |
| 14 | Receiving≥4 units of blood/blood products |
| 15 | Administration of tranexamic acid |
| 16 | Laparotomy for trauma |
| 17 | Thoracotomy for trauma |
| 18 | Pericardial window for trauma |
| 19 | Surgery to gain proximal vascular control |
| 20 | Interventional radiology for haemorrhage control |
| 21 | Application of a pelvic binder |
| 22 | ALS/ACLS protocols for a patient in a peri-arrest situation |
| 23 | ALS/ACLS protocols for a patient in cardiac arrest |
| 24 | Neurosurgery for the evacuation of an intra-cranial haematoma |
| 25 | Craniotomy |
| 26 | Burr Hole Insertion |
| 27 | Spinal nursing for a C1-3 fracture |
| 28 | Administration of a seizure-terminating medication |
| 29 | Active rewarming for initial core temp<32° celcius |
| 30 | Passive rewarming for initial core temp<32° celcius |
| 31 | Correction of low blood glucose |
| 32 | Administration of chemical antidotes |
| Tags : triage
11/08/2016
Transfusion, Thrombosis and Bleeding Management
Special Issue: Transfusion, Thrombosis and Bleeding Management
January 2015 - Volume 70, Issue Supplement s1 - Pages 1–e41
Clic sur l'image pour accéder au numéro en ligne
Blood – the most important humour? (pages 1–e1)
C. R. Bailey, A. A. Klein and B. J. Hunt
Version of Record online: 1 DEC 2014 | DOI: 10.1111/anae.12930
Review Articles
L. Green, S. Allard and R. Cardigan
☛ CPD available at http://www.learnataagbi.org
Corrected by:
Corrigendum: Modern banking, collection, compatibility testing and storage of blood and blood components
Vol. 70, Issue 3, 373, Version of Record online: 11 FEB 2015
Evidence and triggers for the transfusion of blood and blood products (pages 10–e3)
A. Shah, S. J. Stanworth and S. McKechnie
Pre-operative anaemia (pages 20–e8)
B. Clevenger and T. Richards
The pathophysiology and consequences of red blood cell storage (pages 29–e12)
D. Orlov and K. Karkouti
Red cell transfusion and the immune system (pages 38–e16)
S. Hart, C. M. Cserti-Gazdewich and S. A. McCluskey
The current place of aprotinin in the management of bleeding (pages 46–e17)
D. Royston
The current place of tranexamic acid in the management of bleeding (pages 50–e18)
B. J. Hunt
Practical management of major blood loss (pages 54–e20)
R. Gill
Management of peri-operative anti-thrombotic therapy (pages 58–e23)
J. J. van Veen and M. Makris
Laboratory monitoring of haemostasis (pages 68–e24)
A. Fowler and D. J. Perry
Point-of-care monitoring of haemostasis (pages 73–e26)
S. V. Mallett and M. Armstrong
Haemostatic management of obstetric haemorrhage (pages 78–e28)
R. E. Collis and P. W. Collins
Haemostatic management of cardiac surgical haemorrhage (pages 87–e31)
M. W. Besser, E. Ortmann and A. A. Klein
The pathogenesis of traumatic coagulopathy (pages 96–e34)
A. Cap and B. J. Hunt
Management of traumatic haemorrhage – the European perspective (pages 102–e37)
H. Schöchl, W. Voelckel and C. J. Schlimp
Management of traumatic haemorrhage – the US perspective (pages 108–e38)
R. P. Dutton
Surgery in patients with inherited bleeding disorders (pages 112–e40)
P. K. Mensah and R. Gooding
The management of abnormal haemostasis in the ICU (pages 121–e41)
A. Retter and N. A. Barrett
13/06/2016
Trauma Center: Formateur pour la guerre ?
Skill sets and competencies for the modern military surgeon: Lessons from UK military operations in Southern Afghanistan
Ramassamy A. et Al. Injury. 2010 May;41(5):453-9.
Introduction:
British military forces remain heavily committed on combat operations overseas.UK military operations in Afghanistan (Operation HERRICK) are currently supported by a surgical facility at Camp Bastion, in Helmand Province,in the south of the country. There have been no large published series of surgical workload on Operation HERRICK. The aim of this study is to evaluate this information in order to determine the appropriate skill set for the modern military surgical team.
Method:
A retrospective analysis of operating theatre records between 1st May 2006 and 1st May 2008 was performed. Data was collated on a monthly basis and included patient demographics, operation type and time of operation.
Results:
During the study period 1668 cases required 2210 procedures. Thirty-two per cent were coalition forces (ISAF),27% were Afghan security forces (ANSF)and 39% were civilians. Paediatric casualties accounted for 14.7% of all cases. Ninety-three per cent of cases were secondary to battle injury and of these 51.3% were emergencies. The breakdown of procedures,by specialty, was 66% (1463) orthopaedic, 21% (465) general surgery, 6% (139) head and neck, 5% (104) burns surgery and a further (50) non-battle, non-emergency procedures. There was an almost twofold increase in surgical workload in the second year (1103 cases) compared to the first year of the deployment (565 caps e<s ,0.05).
Discussion:
Surgical workload over the study period has clearly increased markedly since the initial deployment of ISAF forces to Helmand Province. A 6-week deployment to Helmand Province currently provides an equivalent exposure to penetrating trauma as 3 years trauma experience in the UK NHS. The spectrum of injuries seen and the requisite skill set that the military surgeon must possess is outside that usually employed within the NHS. A number of different strategies; including the deployment of trainee specialist registrars to combat hospitals, more focused pre-deploymentmilitary surgery training courses, and wet-laboratory work are proposed to prepare for future generations of surgeons operating in conflict environments
12/04/2016
Plaies crâniennes: Un avenir est possible !
Long-term outcomes of combat casualties sustaining penetrating traumatic brain injury
Weisbrod AB et Al. J Trauma Acute Care Surg. 2012;73: 1525-1530
----------------------
Une prise en charge agressive globale des traumatismes cranio-cérébraux permet le retour à une indépendance fonctionnelle. Leur prise en charge doit donc être parfaite dès la prise en charge et la prévention des acsos un leitmotiv.
----------------------
BACKGROUND:
Previous studies have documented short-term functional outcomes for patients sustaining penetrating brain injuries (PBIs). However, little is known regarding the long-term functional outcome in this patient population. Therefore, we sought to describe the long-term functional outcomes of combat casualties sustaining PBI.
METHODS:
Prospective data were collected from 2,443 patients admitted to a single military institution during an 8-year period from 2003 to 2011. PBI was identified in 137 patients and constitute the study cohort. Patients were stratified by age, Injury Severity Score (ISS) and admission Glasgow Coma Scale (aGCS) score. Glasgow Outcome Scale (GOS) scores were calculated at discharge, 6 months, 1 year and 2 years. Patients with a GOS score of 4 or greater were considered to have attained functional independence (FI).
RESULTS:
The mean (SD) age of the cohort was 25 (7) years, mean (SD) ISS was 28 (9), and mean (SD) aGCS score was 8.8 (4.0). PBI mechanisms included gunshot wounds (31%) and blast injuries (69%). Invasive intracranial monitoring was used in 80% of patients, and 86.9% of the study cohort underwent neurosurgical intervention. Complications included cerebrospinal fluid leak (8.3%), venous thromboembolic events (15.3%), meningitis (24.8%), systemic infection (27.0%), and mortality (5.8%). The cohort was stratified by aGCS score and showed significant improvement in functional status when mean discharge GOS score was compared with mean GOS score at 2 years. For those with aGCS score of 3 to 5 (2.3 [0.9] vs. 2.9 [1.4], p G 0.01), 32% progressed to FI. For those with aGCS score of 6 to 8 (3.1 [0.7] vs. 4.0 [1.2], p G 0.0001), 63% progressed to FI. For those with aGCS score of 9 to 11 (3.3 [0.5] vs. 4.3 [0.8], p G 0.0001), 74% progressed to FI. For those with aGCS score of 12 to 15 (3.9 [0.7] vs. 4.8 [0.4], p G 0.00001), 100% progressed to FI.
CONCLUSION: Combat casualties with PBI demonstrated significant improvement in functional status up to 2 years from discharge, and a large proportion of patients sustaining severe PBI attained FI.
| Tags : crâne
Sauvetage au combat: Connaître et appliquer la procédure
Preventable deaths in trauma patients associated with non adherence to management guidelines
Marson CA et Al. Rev Bras Ter Intensiva. 2010; 22(3):220-228
------------------------------------------------------
Connaître, maîtriser chacune des composantes d'une procédure et les mettre en oeuvre est un facteur de survie des blessés. Le respect de la procédure du sauvetage au combat apparait fondamental. Il est nécessaire de le rappeler.
------------------------------------------------------
Objectives: To evaluate patients treated for traumatic injuries and to identify adherence to guidelines recommendations of treatment and association with death. The recommendations adopted were defined by the committee on trauma of the American College of Surgeons in advanced trauma life support.
Methods: Retrospective cohort study conducted at a teaching hospital. The study population was victims of trauma ≥ 12 years of age with injury severity scores ≥ 16 who were treated between January 1997 and December 2001. Data collection was divided into three phases: pre-hospital, in-hospital, and post-mortem. The data collected were analyzed using EPI INFO.
Results: We analyzed 207 patients, 147 blunt trauma victims (71%) and 60 (29%) penetrating trauma victims. Trauma victims had a 40.1% mortality rate. We identified 221 non adherence events that occurred in 137 patients. We found a mean of 1.61 non adherence per patient, and it occurred less frequently in survivors (1.4) than in non-survivors (1.9; p=0.033). According to the trauma score and injury severity score methodology, 54.2% of deaths were considered potentially preventable. Non adherence occurred 1.77 times more frequently in those considered potentially preventable deaths compared to other non-survivors (95% CI: 1.12–2.77; p=0.012), and 92.9% of the multiple non adherence occurred in the first group (p=0.029).
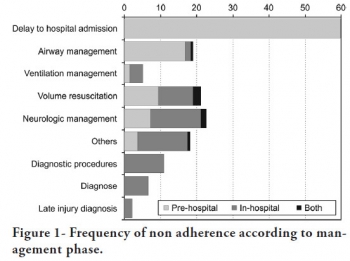
Conclusions: Non adherence occurred more frequently in patients with potentially preventable deaths. Non adherence to guidelines recommendations can be considered a contributing factor to death in trauma victims and can lead to an increase in the number of potentially preventable deaths.
| Tags : procedure evdg
30/01/2016
Retex 13/11/2015
28/01/2016
TXA: Interrogations
Les études CRASH2 et MATTERS ont mis en évidence l'intérêt de l'emploi du TXA en traumatologie grave.
Il s'agit d'un dérivé de la lysine qui agit en se liant au plasminogène bloquant ainsi l'interaction plasminogène-fibrine, donc la fibrinolyse du caillot. Le TXA franchit la barrière sang-cerveau, diffuse dans le LCR et le globe oculaire
Persistent malgré tout quelques interrogations en matière d'innocuité persistent. Si l'étude crash2 n' pas montré de risque thromboembolique majeurs, ce n'est pas le cas d' l'étude MATTERS avec environ 10 fois plus d'épisodes thrombo-emboliques en cas d'usage de TXA. Par ailleurs il est rapporté un risque d'hypotension lors de l'administration rapide de TXA et de convulsions lors de l'emploi de posologies élevées. Ceci ne remet pas en cause le recours précoce au TXA dont l'emploi ne doit pas être banalisé et respecter un certain nombre de règles: probabilité forte de coagulopathie traumatique notamment attesté par une hypotension sévère , 1ère dose le plus tôt possible (au mieux dans la première heure) et pas après 3h, deuxième dose dans les 08h00, administration lente pour éviter hypotension, pas de surdosage facteur de crises convulsives, ne pas administrer en même temps/même ligne que du PLYO.
Un certain nombre d'études complémentaires sont en cours:
1. L'étude "Pre-hospital Antifibrinolytics for Traumatic Coagulopathy and Haemorrhage" a pour objectif d'affiner notre connaissance de l'emploi du TXA.
2.L'étude "Design of the Study of Tranexamic Acid during Air Medical Prehospital Transport (STAAMP) Trial: Addressing the Knowledge Gaps" a pour objet d'étuider la mortalité à 30 jours de traumatisés sévères pris en charge par medevac héliportées.
3. L'étude "Tranexamic Acid Mechanisms and Pharmacokinetics In Traumatic Injury (TAMPITI Trial)" vise quand à elle à confirmer un certain nombre d'hypothèses sur le mécanisme d'action.
Par ailleurs, le TXA n'est pas le seul antifibrinolyique utilisable.
| Tags : coagulopathie
23/01/2016
Maîtriser l'airway +++, entre autres
Augmentation of point of injury care: Reducing battlefield
mortality—The IDF experience
Benov A. et Al. Injury. 2015 Nov 18. pii: S0020-1383(15)00697-X. doi: 10.1016/j.injury.2015.10.078.
------------------------------
Une publication particulièrement intéressante car elle émane de collègues militaires qui interviennent dans un contexte très particulier de prise en charge de blessés tels qu'on peut les rencontrer en opérations extérieures mai dans un contexte de réseau de traumatologie civile puisque que les hôpitaux de recueil de ces blessés sont les hôpitaux civils. Les données présentées ne portent que sur la prise en charge de combattants.
Un des points analysé est la performance des équipes dans certains gestes considérés comme essentiel, notamment la gestion des voies aériennes. Comme dans l'armée française l'intubation orotrachéale et la criciothyrotomie représentent les deux procédures mises en oeuvre par des médecins. Manifestement, il existe une grande maîtrise de la coniotomie alors que celle de l'Intubation est moins évidente: 41% de succès et une moyenne de 2 tentatives. Ceci reste problématique lorsque la prise en charge des blessés se fait loin d'un trauma center et qu'il faut envisager la gestion de ces voies aériennes et l'initiation d'une ventilation pendant plusieurs heures (jours ?). Pour ces raisons et même si la probabilité d'être confronté à une telle situation est faible, ce travail rapporte les 2/3 des blessés ne sont pas urgent et que 5% seulement des nécessitent un geste sur les voies aériennes, il s'agit d'un point fondamental en matière de réduction de morts indues.
------------------------------
STUDY OBJECTIVE:
In 2012, the Israel Defense Forces Medical Corps (IDF-MC) set a goal of reducing mortality and eliminating preventable death on the battlefield. A force buildup plan entitled "My Brother's Keeper" was launched addressing: trauma medicine, training, change of Clinical Practice Guidelines (CPGs), injury prevention, data collection, global collaboration and more. The aim of this article is to examine how military medical carehas evolved due "My Brother's Keeper" between Second Lebanon War (SLW, 2006) to Operation Protective Edge (OPE, 2014).
METHODS:
Records of all casualties during OPE and SLW were extracted and analyzed from the I.D.F Trauma Registry. Noncombat injuries and civilian injuries from missile attacks were excluded from this analysis.
RESULTS:
The plans main impacts were; incorporation of a physician or paramedic as an integral part of each fighting company, implementation of new CPGs, introduction of new approaches for extremity haemorrhage control and Remote Damage Control Resuscitation at point of injury (POI) using single donor reconstituted freeze dried plasma (25 casualties) and transexamic acid (98 casualties). During OPE, 704 soldiers sustained injuries compared with 833 casualties during SLW. Fatalities were 65 and 119, respectively, cumulating to Case Fatality Rate of 9.2% and 14.3%, respectively.
CONCLUSIONS:
Significant changes in the way the IDF-MC provides combat casualty care have been made in recent years. It is the transformation from concept to doctrine and integration into a structured and Goal-Oriented Casualty Care System, especially POI care that led to the unprecedented survival rates in IDF as shown in this conflict.
| Tags : airway
ATLS: pas de plue value pour la catastrophe
Triage performance of Swedish physicians using the ATLS algorithm in a simulated mass casualty incident: a prospective cross-sectional survey
Lampi et al.Scand J Trauma Resusc Emerg Med. 2013; 21: 90.
----------------------------------------------------
On revient une fois de plus sur l'intérêt relativement limité de l'apport de l'ATLS dans un système de santé avancé. L'émergence de nouvelles modalités d'enseignement en ligne, l'introduction de la simulation médicale, le contenu relativement basique souvent non en phase avec les pratiques médicales du moment et un modèle économique qui interpelle font que l'on doit se poser la question de sa pertinence. Cet article exprime que cet apport n'est pas prouvé en médecine de catastrophe, du moins sur un aspect important qu'est l'emploi de la mnémonique ABCDE.
----------------------------------------------------
Background: In a mass casualty situation, medical personnel must rapidly assess and prioritize patients for treatment and transport. Triage is an important tool for medical management in disaster situations. Lack of common international and Swedish triage guidelines could lead to confusion. Attending the Advanced Trauma Life Support (ATLS) provider course is becoming compulsory in the northern part of Europe. The aim of the ATLS guidelines is provision of effective management of single critically injured patients, not mass casualties incidents. However, the use of the ABCDE algorithms from ATLS, has been proposed to be valuable, even in a disaster environment. The objective for this study was to determine whether the mnemonic ABCDE as instructed in the ATLS provider course, affects the ability of Swedish physician’s to correctly triage patients in a simulated mass casualty incident.
Methods: The study group included 169 ATLS provider students from 10 courses and course sites in Sweden; 153 students filled in an anonymous test just before the course and just after the course. The tests contained 3 questions based on overall priority. The assignment was to triage 15 hypothetical patients who had been involved in a bus crash. Triage was performed according to the ABCDE algorithm. In the triage, the ATLS students used a colour-coded algorithm with red for priority 1, yellow for priority 2, green for priority 3 and black for dead. The students were instructed to identify and prioritize 3 of the most critically injured patients, who should be the first to leave the scene. The same test was used before and after the course.
Results: The triage section of the test was completed by 142 of the 169 participants both before and after the course. The results indicate that there was no significant difference in triage knowledge among Swedish physicians who attended the ATLS provider course. The results also showed that Swedish physicians have little experience of real mass casualty incidents and exercises.
Conclusion: The mnemonic ABCDE doesn’t significantly affect the ability of triage among Swedish physicians. Actions to increase Swedish physicians’ knowledge of triage, within the ATLS context or separately, are warranted
12/01/2016
Dexamethasone: Hémostatique cérébral ?
Steroid-loaded Hemostatic Nanoparticles Alleviate Injury Progression after Blast Trauma
Hubbard WD et Al.. ACS Macro Lett., 2015, 4 (4), pp 387–391
The purpose of this study was to investigate whether hemostatic dexamethasone-loaded nanoparticles (hDNP) functionalized with a peptide that binds with activated platelets could reduce cellular injury and improve functional outcomes in a model of blast trauma. Functionalized nanoparticles, or synthetic platelets, offer a wide variety of benefits and advantages compared to alternatives, such as increased biocompatibility and targeting of the injury site (DePalma, 2005). Blood loss is the primary cause of death at acute time points post injury in both civilian and battlefield traumas. Currently, there is a shortage in treatments for internal bleeding, especially for rapid administration in open field combat. In a recent U.K. study, less than fifty percent of soldiers diagnosed with primary blast lung injury (PBLI), the most common fatal blast injury, survived to reach a medical facility (Smith, 2011). This study examines potential therapeutic effects of hDNP on subacute recovery in brain pathology and behavior after blast polytrauma. An established polytrauma model that simulates severe injury, including PBLI and blast-induced neurotrauma (BINT), can be used to evaluate life-saving therapeutics (Hubbard, 2014). Poly(lactic-co-glycolic acid)-based nanoparticles with poly(ethylene glycol) arms and the arginine-glycine-aspartic acid (RGD) peptide to target activated platelets were fabricated. A blast-induced polytrauma rodent model was used to evaluate the functionalized nanoparticles at an acute stage. After anesthesia, Male Sprague Dawley rats were exposed to a single, representative “free field” blast wave from an Advanced Blast Simulator at Virginia Tech at a peak overpressure of 28 psi for 2.5 ms duration, operating above 50% lethality risk, in a sidethorax orientation (Hubbard, 2014). After injury, animals were immediately injected intravenously with hDNP, control dexamethasone-loaded nanoparticles (cDNP), or lactated ringers (LR) and physiological parameters were monitored. Sham animals were not injected or exposed to the blast wave. Open field assays were performed on surviving animals to measure levels of anxiety. At one week post-blast, brains were extracted and sections from the amygdala were obtained for immunofluorescent staining using glial fibrillary acidic protein (GFAP; activated astrocytes), cleaved caspase-3 (apoptosis), and SMI-71 (blood-brain barrier). According to physiological monitoring immediately after blast, oxygen saturation was significantly decreased in the control and LR groups compared to the active and sham groups. Using the open field test, elevated anxiety parameters were found in the control and LR groups compared to the hDNP group. GFAP was significantly elevated in the control group compared to the hDNP and sham groups in the amygdala. Caspase-3 was also significantly elevated in the control group compared to the hDNP group. SMI-71 was significantly reduced in the LR group compared to the sham group. hDNP treatment has the potential to assist recovery after internal hemorrhage. Immediate intervention to assuage hemorrhage, one source for injury pathology, is crucial to mitigate debilitating injury mechanisms that lead to cognitive and emotional deficits (Shetty, 2014).
It is possible that through prevention of microhemorrhaging of the blood-brain barrier (BBB), hDNP was able to mitigate cellular injury and improve cognitive outcomes. Future studies will evaluate the effect on inflammatory and hypoxia-related proteins after hDNP administration post-trauma.
| Tags : blast, hémorragie
Prédire le besoin transfusionnel tôt ?
Automated analysis of vital signs to identify patients with substantial bleeding before hospital arrival: a feasibility study
Liu J et Al. Shock. 2015 May;43(5):429-36.
---------------------------------------------------------
Dépister un saignement significatif à partir des éléments standards de monitorage préhospitalier serait possible à en croire cet article. Il existe actuellement un grand nombre de recherche dans ce domaine. A suivre.
---------------------------------------------------------
Trauma outcomes are improved by protocols for substantial bleeding, typically activated after physician evaluation at a hospital. Previous analysis suggested that prehospital vital signs contained patterns indicating the presence or absence of substantial bleeding. In an observational study of adults (aged Q18 years) transported to level I trauma centers by helicopter, we investigated the diagnostic performance of the Automated Processing of the Physiological Registry for Assessment of Injury Severity (APPRAISE) system, a computational platform for real-time analysis of vital signs, for identification of substantial bleeding in trauma patients with explicitly hemorrhagic injuries. We studied 209 subjects prospectively and 646 retrospectively. In our multivariate analysis, prospective performance was not significantly different from retrospective.

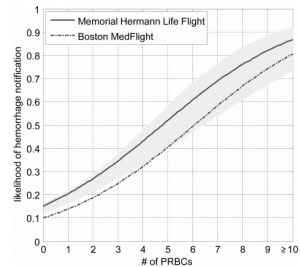
The APPRAISE system was 76% sensitive for 24-h packed red blood cells of 9 or more units (95% confidence interval, 59% Y 89%) and significantly more sensitive (P G 0.05) than any prehospital Shock Index of 1.4 or higher; sensitivity, 59%; initial systolic blood pressure (SBP) less than 110 mmHg, 50%; and any prehospital SBP less than 90 mmHg, 50%. The APPRAISE specificity for 24-h packed red blood cells of 0 units was 87% (88% for any Shock Index Q1.4, 88% for initial SBP G110 mmHg, and 90% for any prehospital SBP G90 mmHg). Median APPRAISE hemorrhage notification time was 20 min before arrival at the trauma center. In conclusion, APPRAISE identified bleeding before trauma center arrival. En route, this capability could allow medics to focus on direct patient care rather than the monitor and, via advance radio notification, could expedite hospital interventions for patients with substantial blood loss.

1365-2044/asset/olbannerleft.gif?v=1&s=bd83df57543a1d11ffc15f630bb1301f0be80859)

