16/01/2023
Poser un drain thoracique: Le Reactor ?
Comparing a Novel Hand-Held Device for Chest Tube Insertion to the Traditional Open Tube Thoracostomy for Simple Pneumothorax in a Porcine Model
Dilday J. et Al. J Spec Oper Med. 2022 Dec 16;22(4):41-45.
------------------------------------------------------------------
Ce genre de dispositif parait être plutôt adapté à des personnels peu habitué à ce geste et surtout nécessite un équipement supplémentaire
------------------------------------------------------------------
Background: Tube thoracostomy is the most effective treatment for pneumothorax, and on the battlefield, is lifesaving. In combat, far-forward adoption of open thoracostomy has not been successful. Therefore, the ability to safely and reliably perform chest tube insertion in the far-forward combat theatre would be of significant value. The Reactor is a hand-held device for tube thoracostomy that has been validated for tension pneumothorax compared to needle decompression. Here we investigate whether the Reactor has potential for simple pneumothorax compared to open thoracostomy. Treatment of pneumothorax before tension physiology ensues is critical.
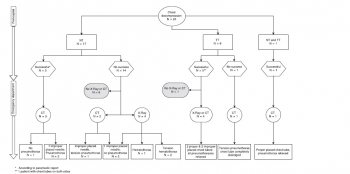
Methods: Simple pneumothoraces were created in 5 in-vivo swine models and confirmed with x-ray. Interventions were randomized to open technique (OT, n = 25) and Reactor (RT, n = 25). Post-procedure radiography was used to confirm tube placement and pneumothorax resolution. Video Assisted Thoracoscopic Surgery (VATS) was used to evaluate for iatrogenic injuries. 50 chest tubes were placed, with 25 per group.
Results: There were no statistical differences between the groups for insertion time, pneumothorax resolution, or estimated blood loss (p = .91 and .83). Injury rates between groups varied, with 28% (n = 7) in the Reactor group and 8% (n = 2) the control group (p = .06). The most common injury was violation of visceral pleura (10%, n = 5, both groups) and violation of the mediastinum (8%, n = 4, both groups).
Conclusion: The Reactor device was equal compared to open thoracostomy for insertion time, pneumothorax resolution, and injury rates. The device required smaller incisions compared to tube thoracostomy and may be useful adjunct in simple pneumothorax management.
| Tags : pneumothorax
10/06/2018
Exsufflation: 5 cm antérieur survie = 9 latéral
BACKGROUND:
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
METHODS:
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
RESULTS:
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-gauge intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-gauge IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene. The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups.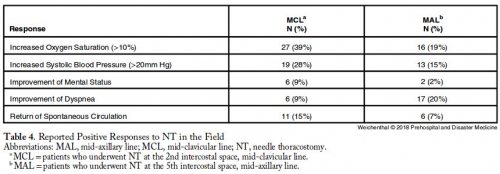
CONCLUSIONS:
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.| Tags : exsufflation, pneumothorax
01/10/2017
Exsufflation axillaire: Plus sûre
Relative device stability of anterior versus axillary needle decompression for tension pneumothorax during casualty movement: Preliminary analysis of a human cadaver model
BACKGROUND:
Tension pneumothorax (tPTX) remains a significant cause of potentially preventable death in military and civilian settings. The current prehospital standard of care for tPTX is immediate decompression with a 14-gauge 8-cm angiocatheter; however, failure rates may be as high as 17% to 60%. Alternative devices, such as 10-gauge angiocatheter, modified Veress needle, and laparoscopic trocar, have shown to be potentially more effective in animal models; however, little is known about the relative insertional safety or mechanical stability during casualty movement.
METHODS:
Seven soft-embalmed cadavers were intubated and mechanically ventilated. Chest wall thickness was measured at the second intercostal space at the midclavicular line (2MCL) and the fifth intercostal space along the anterior axillary line (5AAL). CO2 insufflation created a PTX, and needle decompression was then performed with a randomized device. Insertional depth was measured between hub and skin before and after simulated casualty transport. Thoracoscopy was used to evaluate for intrapleural placement and/or injury during insertion and after movement. Cadaver demographics, device displacement, device dislodgment, and injuries were recorded. Three decompressions were performed at each site (2MCL/5AAL), totaling 12 events per cadaver.
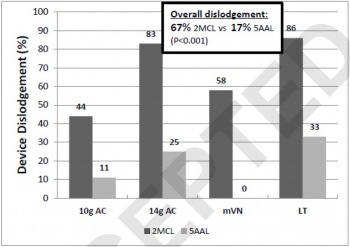
RESULTS:
Eighty-four decompressions were performed. Average cadaver age was 59 years, and body mass index was 24 kg/m. The CWT varied between cadavers because of subcutaneous emphysema, but the average was 39 mm at the 2MCL and 31 mm at the 5AAL. Following movement, the 2MCL site was more likely to become dislodged than the 5AAL (67% vs. 17%, p = 0.001). Median displacement also differed between 2MCL and 5AAL (23 vs. 2 mm, p = 0.001). No significant differences were noted in dislodgement or displacement between devices. Five minor lung injuries were noted at the 5AAL position.
CONCLUSION:
Preliminary results from this human cadaver study suggest the 5AAL position is a more stable and reliable location for thoracic decompression of tPTX during combat casualty transport.
| Tags : pneumothorax
22/04/2017
3 côtés: Non occlusif ? Pas tous égaux
Do vented chest seals differ in efficacy? An experimental evaluation using a swine hemopneumothorax model
--------------------------------
Un travail très pratique qui fait le point sur la performance des pansements 3 côtés non occlusifs. Plusieurs sont disponibles sur le marché. Mais qu'en est il des divers dispositifs proposés sur le marché. On dispose déjà de données concernant les propriétés "adhésives" de ces dispositifs (1). Avec ce travail, on a en plus une idée sur la capacité de ces pansements à permettre l'écoulement de saignement intra-thoraciques. L'historique valve d'asherman doit être considérée comme obsolète.
--------------------------------
OBJECTIVE:
Hemopneumothorax (HPTX) is the second leading cause of potentially preventable death among combat casualties. We investigated the ability of five FDA-approved non-occlusive chest seals (CSs) to seal a bleeding chest wound and prevent tension HPTX in a swine model.
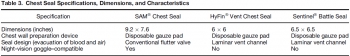
METHODS:
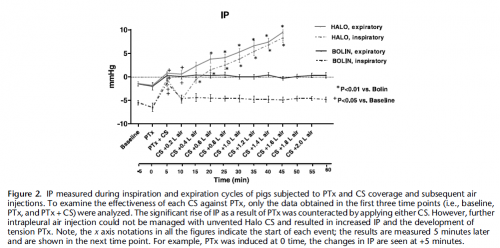
Following instrumentation, an open chest wound was created in the left thorax of spontaneously air-breathing anesthetized pigs (n=26, 43 Kg). Autologous fresh blood (226 mL) was then infused into the pleural cavity to produce HPTX. The chest wounds were then sealed with CSs. The sealant strength and venting function of CSs were challenged by infusion of 50 mL more blood directly into the chest wound and incremental air injections into the pleural cavity. Tension HPTX was defined as intrapleural (IP) pressure ≥ +1 mmHg and >20% deviation in physiological measurements.
RESULTS:
An open chest wound with HPTX raised IP pressure (~ -0.7 mmHg) and caused labored breathing and reductions in PaO2 and SvO2 (P<0.01). Sealing the wounds with the CSs restored IP pressure, and improved breathing and oxygenation. Subsequent blood infusion into the wound and IP air injections produced CS-dependent responses.
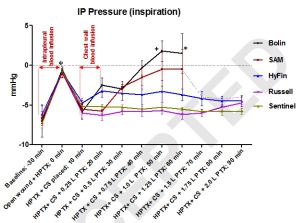
CSs with one-way valves (Bolin and SAM) did not evacuate the blood efficiently; pooled blood either detached the CSs from skin and leaked out (75%), or clotted and clogged the valve and led to tension HPTX (25%). Conversely, CSs with laminar venting channels allowed escape of blood and air from the pleural cavity and maintained IP pressure and oxygenation near normal levels. Success rates were 100% for Sentinel and Russell (6/6); 67% for HyFin (4/6); 25% for SAM (1/4); and 0% for Bolin (0/4) CSs (p=0.002).
CONCLUSION:
The sealant and valve function of vented CS differed widely in the presence of bleeding chest wounds. Medics should be equipped with more effective CSs for treating HPTX in the field.
| Tags : pneumothorax
18/01/2017
Décompression pleurale: Dur, dur...
Failure rate of prehospital chest decompression after severe thoracic trauma.
Kaserer A. et Al Am J Emerg Med. 2016 Nov 30. pii: S0735-6757(16)30892-0
-----------------------------------------------------
Une publication qui émane de nos collègues suisses et qui interpelle quelque peu. La décompression thoracique apparat être un geste dont la maîtrise est largement insuffisante y compris quand elle est réalisée au sein d'un système mature. Une raison de plus pour s'intéresser à la maîtrise effective des gestes censés participer à la mise en condition de survie des blessés. On rappelle l'intérêt de la thoracostomie au doigt (1), doigt dont la longueur est en général suffisante pour entrer dans un thorax.
-----------------------------------------------------
INTRODUCTION:
Chest decompression can be performed by different techniques, like needle thoracocentesis (NT), lateral thoracostomy (LT), or tube thoracostomy (TT). The aim of this study was to report the incidence of prehospital chest decompression and to analyse the effectiveness of these techniques.
MATERIAL AND METHODS:
In this retrospective case series study, all medical records of adult trauma patients undergoing prehospital chest decompression and admitted to the resuscitation area of a level-1 trauma center between 2009 and 2015 were reviewed and analysed. Only descriptive statistics were applied.
RESULTS:
In a 6-year period 24 of 2261 (1.1%) trauma patients had prehospital chest decompression. Seventeen patients had NT, six patients TT, one patient NT as well as TT, and no patients had LT. Prehospital successful release of a tension pneumothorax was reported by the paramedics in 83% (5/6) with TT, whereas NT was effective in 18% only (3/17). In five CT scans all thoracocentesis needles were either removed or extrapleural, one patient had a tension pneumothorax, and two patients had no pneumothorax. No NT or TT related complications were reported during hospitalization.
CONCLUSION:
Prehospital NT or TT is infrequently attempted in trauma patients. Especially NT is associated with a high failure rate of more than 80%, potentially due to an inadequate ratio between chest wall thickness and catheter length as previously published as well as a possible different pathophysiological cause of respiratory distress. Therefore, TT may be considered already in the prehospital setting to retain sufficient pleural decompression upon admission.
| Tags : pneumothorax
08/05/2016
la voie axillaire +++
Chest wall thickness and decompression failure: A systematic review and meta-analysis comparing anatomic locations in needle thoracostomy
Laan DV et Al. Injury, Int. J. Care Injured 47 (2016) 797–804
------------------------------------------
Une publication, une de plus, qui met en avant l'abord axillaire pour la décompression thoracique et qui insiste sur le peu de preuve de l'inocuité des cathéters de 8 cm. On rappelle que la thoracostomie au doigt reste la référence.
------------------------------------------
Introduction:
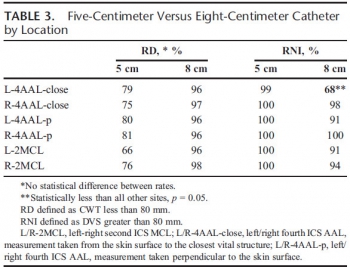
Current Advanced Trauma Life Support guidelines recommend decompression for thoracic tension physiology using a 5-cm angiocatheter at the second intercostal space (ICS) on the midclavicular line (MCL). High failure rates occur. Through systematic review and meta-analysis, we aimed to determine the chest wall thickness (CWT) of the 2nd ICS-MCL, the 4th/5th ICS at the anterior axillary line (AAL), the 4th/5th ICS mid axillary line (MAL) and needle thoracostomy failure rates using the currently recommended 5-cm angiocatheter.
Methods:
A comprehensive search of several databases from their inception to July 24, 2014 was conducted. The search was limited to the English language, and all study populations were included. Studies were appraised by two independent reviewers according to a priori defined PRISMA inclusion and exclusion criteria. Continuous outcomes (CWT) were evaluated using weighted mean difference and binary outcomes (failure with 5-cm needle) were assessed using incidence rate. Outcomes were pooled using the random-effects model.
Results:
The search resulted in 34,652 studies of which 15 were included for CWT analysis, 13 for NT effectiveness. Mean CWT was 42.79 mm (95% CI, 38.78–46.81) at 2nd ICS-MCL, 39.85 mm (95% CI, 28.70–51.00) at MAL, and 34.33 mm (95% CI, 28.20–40.47) at AAL (P = .08). Mean failure rate was 38% (95% CI, 24–54) at 2nd ICS-MCL, 31% (95% CI, 10–64) at MAL, and 13% (95% CI, 8–22) at AAL (P = .01).
Conclusion:
Evidence from observational studies suggests that the 4th/5th ICS-AAL has the lowest predicted failure rate of needle decompression in multiple populations.
| Tags : pneumothorax, exsufflation
25/02/2016
Exsufflation: Cela se complique !
Complications of needle thoracostomy: A comprehensive clinical review
Wernjck B et Al. Int J Crit Illn Inj Sci. 2015 Jul-Sep; 5(3): 160–169
---------------------------------------------
Comme toujours, après une phase d'engouement vient le temps de la réflexion. L'exsufflation à l'aiguille n'est pas d'une indication si fréquente et en plus expose à certaines complications. A lire avant de se lancer dans l'utilisation d'aiguille de tout genre.
---------------------------------------------
Needle thoracostomy (NT) is a valuable adjunct in the management of tension pneumothorax (tPTX), a life-threatening condition encountered mainly in trauma and critical care environments. Most commonly, needle thoracostomies are used in the prehospital setting and during acute trauma resuscitation to temporize the affected individuals prior to the placement of definitive tube thoracostomy (TT). Because it is both an invasive and emergent maneuver, NT can be associated with a number of potential complications, some of which may be life-threatening. Due to relatively common use of this procedure, it is important that healthcare providers are familiar, and ready to deal with, potential complications of NT.
| Tags : pneumothorax
05/08/2015
Décompression à l'aiguille: Pas fiable
Does needle thoracostomy provide adequate and effective decompression of tension pneumothorax?
Martin M et Al. J Trauma Acute Care Surg. 2012;73: 1412-1417
-----------------------
La décompression thoracique est une des mesures qui vise à réduire le nombre de morts évitables. Il s'agit d'une procédure mise en oeuvre peu fréquemment. L'exsufflation à l'aiguille est la méthode enseignée. Il existe beaucoup de débats concernant le lieu de ponction (plutôt par voie axillaire et non par voie antérieure), la longueur du cathéter (certains proposent 8 cm au risque de ponction parenchymateuse et des gros vaisseaux), le diamètre. Le travail proposé est très intéressant car il exprime toute les réserves qui doivent encadrer ce geste qui ne semble pas aussi efficace que cela car outre les problèmes mécanique il apparaît bien qu'un cathéter de 14G risque d'être insuffisant. On rappelle quand même que la thoracostomie au doigt est toujours possible et que votre doigt a de fortes chances de mesurer 8 cm donc de pouvoir pénétrer dans un thorax après création d'un stomie intercostale à la pince de monro-kelly.
-----------------------
BACKGROUND:
Tension pneumothorax (tPTX) is a common and potentially fatal event after thoracic trauma. Needle decompression is the currently accepted first-line intervention but has not been well validated. The purpose of this study was to evaluate the effectiveness of a properly placed and patent needle thoracostomy (NT) compared with standard tube thoracostomy (TT) in a swine model of tPTX.
METHODS:
Six adult swine underwent instrumentation and creation of tPTX using thoracic CO2 insufflation via a balloon trocar. A continued 1 L/min insufflation was maintained to simulate an ongoing air leak. The efficacy and failure rate of NT (14 gauge) compared with TT (34F) was assessed in two separate arms: (1) tPTX with hemodynamic compromise and (2) tPTX until pulseless electrical activity (PEA) obtained. Hemodynamics was assessed at 1 and 5 minutes after each intervention.
RESULTS:
A reliable and highly reproducible tPTX was created in all animals with a mean insufflation volume of 2441 mL. tPTX resulted in the systolic blood pressure declining 54% from baseline (128Y58 mm Hg), cardiac output declining by 77% (7Y1.6 L/min), and equalization of central venous pressure and wedge pressures. In the first arm, there were 19 tPTX events treated with NT placement. All NTs were patent on initial placement, but 5 (26%) demonstrated mechanical failure (due to kinking, obstruction, or dislodgment) within 5 minutes of placement, all associated with hemodynamic decline. Among the 14 NTs that remained patent at 5 minutes, 6 (43%) failed to relieve tension physiology for an overall failure rate of 58%. Decompression with TTwas successful in relieving tPTX in 100%. In the second arm, there were 21 tPTX with PEA events treated initially with either NT (n = 14) or TT (n = 7). The NT failed to restore perfusion in nine events (64%), whereas TT was successful in 100% of events as a primary intervention and restored perfusion as a rescue intervention in eight of the nine NT failures (88%).
CONCLUSION: Thoracic insufflation produced a reliable and easily controlled model of tPTX. NT was associated with high failure rates for relief of tension physiology and for treatment of tPTX-induced PEA and was due to both mechanical failure and inadequate tPTX evacuation. This performance data should be considered in future NT guideline development and equipment design
| Tags : exsufflation, pneumothorax
21/06/2015
Pneumothorax en vol: Merci l'écho
In-flight thoracic ultrasound detection of pneumothorax in combat
Madill JJ J Emerg Med. 2010 Aug;39(2):194-7
-----------------------------------------------
Ce cas clinique est intéressant car il démontre que le recours à l'échographie est dans ce cas non seulement possible mais indispensable compte tenu des difficultés d'auscultation en vol. Ceci étant dit il faut cependant être bien conscient du caractère opérateur dépendant de l'échographie qui peut être peu parlante et nécessiter donc une pratique réelle au delà d'une simple formation à la FAST échographie
-----------------------------------------------
Background: Ultrasonography is the only portable imaging modality available in the helicopter medical evacuation environment where physical examination is limited, auscultation is impossible, long transport times may occur, and altitude variations are frequent. Although the use of ultrasonography by aviation medical personnel has been documented, minimal literature exists on the contribution of in-flight ultrasonography to patient management. Objectives: This case demonstrates an indication for the use of in-flight ultrasonography. It shows how it can affect in-flight management and direct lifesaving intervention.
Case Report: A patient with blast injury developed hemodynamic instability of unclear etiology during transport in the combat aviation environment. To our knowledge, this is the first reported case where in-flight thoracic ultrasonography augmented physical examination and diagnosed an untreated pneumothorax when auscultation was impossible. It directed the decision to perform in-flight procedural intervention with tube thoracostomy. This rapidly improved the patient’s hemodynamic stability in a remote and hostile setting.
Conclusion: In-flight thoracic ultrasonography is a portable imaging tool that can be used by aviation medical personnel to detect pneumothorax in environments where physical examination is limited and auscultation is impossible
| Tags : pneumothorax, échographie
09/06/2015
Faut il drainer avant de décoller: Non ?
Air Transport of Patients with Pneumothorax: Is Tube Thoracostomy Required Before Flight ?
Braude D et Al. Air Med J. 2014 Jul-Aug;33(4):152-6
Objective: It is conventionally thought that patients with pneumothorax (PTX) require tube thoracostomy (TT) before air medical transport (AMT), especially in unpressurized rotor-wing (RW) aircraft, to prevent deterioration from expansion of the PTX or development of tension PTX. We hypothesize that patients with PTX transported without TT tolerate RW AMT without serious deterioration, as defined by hypotension, hypoxemia, respiratory distress, intubation, bag valve mask ventilation, needle thoracostomy (NT), or cardiac arrest during transport.
Methods: We conducted a retrospective review of a case-series of trauma patients transported to a single Level 1 trauma center via RW with confirmed PTX and no TT. Using standardized abstraction forms, we reviewed charts for signs of deterioration. Those patients identified as having clinical deterioration were independently reviewed for the likelihood that the clinical deterioration was a direct consequence of PTX.
Results: During the study period, 66 patients with confirmed PTX underwent RW AMT with an average altitude gain of 1890 feet, an average barometric pressure 586-600 mmHg, and average flight duration of 28 minutes. All patients received oxygen therapy; 14/66 patients (21%) were supported with positive pressure ventilation. Eleven of 66 patients (17%) had NT placed before flight and 4/66 (6%) had NT placed during flight. Four of 66 patients (6% CI0.3-11.7) may have deteriorated during AMT as a result of PTX; all were successfully managed with NT.
Conclusions: In this series, 6% of patients with PTX deteriorated as result of AMT without TT, yet all patients were managed successfully with NT. Routine placement of TT in patients with PTX before RW AMT may not be necessary. Further prospective evaluation is warranted.
| Tags : pneumothorax, drainage thorax
03/06/2015
Par le côté et avec du long ?
Evaluation of 8.0-cm needle at the fourth anterior axillary line for needle chest decompression of tension pneumothorax
Chang SJ et Al. J Trauma Acute Care Surg. 2014;76: 1029-1034
----------------------------------------------------------------------------
La décompression d'un thorax sous pression doit maintenant se faire par voie latérale, la voie antérieure étant associée à un taux d'échec important notamment avec l'emploi de cathéters veineux classiques dont la longueur est rarement supérieure à 5 cm. Le recours à des cathéters de 8 cm est ainsi prôné dans la littérature anglo-saxone sur des seuls arguments anatomiques. Le risque de ponction de structures intrathoraciques est réel et doit rendre mesuré quand au recours à de tels dispositifs. On rappelle que la thoracostomie au doigt doit être considérée comme la référence.
| Tags : exsufflation, pneumothorax
24/04/2015
Pneumothorax: Passez par le côté
Failed needle decompression of bilateral spontaneous tension pneumothorax
Bac PT et Al. Acta Anaesthesiol Scand. 2015 Apr 21. doi: 10.1111/aas.12538. [Epub ahead of print]
-------------------------------------------------
Cet article a le mérite de rappeler que la détresse respiratoire est ua prmeier plan enc as de pneumothorax suffocant chez le patient non ventilé, que la voie latérale doit être privilégié et surtout que la thoracostomie simple est parfaitement efficace.
-------------------------------------------------
This case report presents a young male admitted with primary bilateral spontaneous tension pneumothorax and severe respiratory distress. This is an extremely rare condition. The patient was on the verge of hypoxic cardiac arrest and the attempted needle thoracocentesis was unsuccessful. Needle thoracocentesis in the midclavicular line of the second intercostal space is widely used and recommended as first-line treatment of tension pneumothorax. Reviewing the literature, the procedure is not based on solid evidence. It has high failure rates and potentially serious complications. Alternatives to this approach are perhaps more appropriate. Correctly done, needle thoracocentesis has its place in the presence of a diagnosed or suspected tension pneumothorax when no other options are available. If needle thoracocentesis is chosen, then insertion in the mid-anterior axillary line of the 3rd–5th intercostal space is an appropriate alternative site. Otherwise, lateral thoracostomy, with or without chest tube insertion, is a safe procedure with a high success rate. It should be considered as the first-line treatment of tension pneumothorax, particularly in the unstable patient
| Tags : pneumothorax, exsufflation
10/03/2015
Pansements 3 côtés: C'est efficace
Vented Chest Seals for Prevention of Tension Pneumothorax in a Communicating Pneumothorax
Kotora JG et Al. J Emerg Med. 2013 Nov;45(5):686-94.
--------------------------------------------------------------------------------------------------------------------
La prise en charge d'une plaie thoracique soufflante (1) est une éventualité peu fréquente qui expose d'une part au risque de détresse respiratoire aiguë et d'autre part au risque d'instabilité hémodynamique en rapport avec le caractère compressif d'un épanchement intra-thoracique gazeux ou liquidien (2) L'exsufflation et/ou la pose d'un pansement 3 côtés sont alors requis. Ce dernier peut être réalisé simplement ou par l'emploi de dispositifs commerciaux prêts à l'emploi. Le travail présenté exprime l'efficacité des pansements "3 côtés" de dernières générations aussi bien en matière d'adhérence cutanée que d'efficacité d'évacuation de l'air et secrétions intra-thoraciques. Ils jouent donc ainsi parfaitement le rôle pour lesquels ils ont été conçus (3).
--------------------------------------------------------------------------------------------------------------------
BACKGROUND:
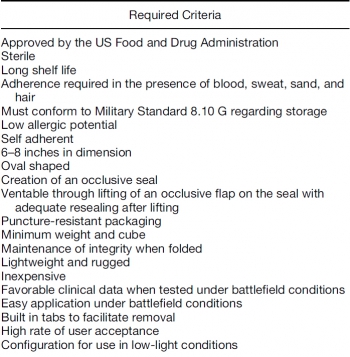
Tension pneumothorax accounts for 3%–4% of combat casualties and 10% of civilian chest trauma. Air entering a wound via a communicating pneumothorax rather than by the trachea can result in respiratory arrest and death. In such cases, the Committee on Tactical Combat Casualty Care advocates the use of unvented chest seals to prevent respiratory compromise.
OBJECTIVE: A comparison of three commercially available vented chest seals was undertaken to evaluate the efficacy of tension pneumothorax prevention after seal application.
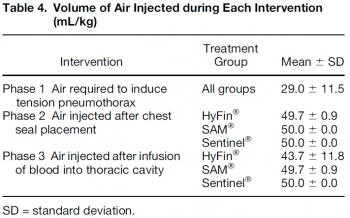
METHODS:
A surgical thoracostomy was created and sealed by placing a shortened 10-mL syringe barrel (with plunger in place) into the wound. Tension pneumothorax was achieved via air introduction through a Cordis to a maximum volume of 50 mL/kg. A 20% drop in mean arterial pressure or a 20% increase in heart rate confirmed hemodynamic compromise. After evacuation, one of three vented chest seals (HyFin ®, n = 8; Sentinel ®, n = 8, SAM ®, n = 8) was applied. Air was injected to a maximum of 50 mL/kg twice, followed by a 10% autologous blood infusion, and finally, a third 50 mL/kg air bolus. Survivors completed all three interventions, and a 15-min recovery period.
RESULTS:
The introduction of 29.0 (±11.5) mL/kg of air resulted in tension physiology. All three seals effectively evacuated air and blood. Hemodynamic compromise failed to develop with a chest seal in place.
CONCLUSIONS:
HyFin ®, SAM ®, and Sentinel ® vented chest seals are equally effective in evacuating blood and air in a communicating pneumothorax model. All three prevented tension pneumothorax formation after penetrating thoracic trauma
| Tags : pneumothorax, exsufflation
23/02/2015
Pneumo suffocant: Oui
Clic sur l'image pour accéder au document
Pneumothorax compressif, sous tension, tamponnade gazeuse. Autant de termes utilisés pour cette situation clinique à laquelle est souvent associé l'existence d'une hypotension artérielle, en fait surtout présente chez les patients ventilés. La détresse respiratoire est souvent au premier plan che le blessé non ventilé et le terme de pneumothorax suffocant adapté. Le document proposé est un peu ancien mais apporte une vision relativement didactique de la problématique séméiologique et physiopathologique.
| Tags : pneumothorax
08/01/2015
Pneumo suffocant: HypoTA, pas toujours!
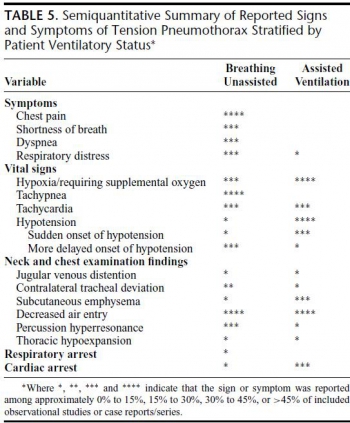
Clinical Presentation of Patients With Tension Pneumothorax A Systematic Review
Roberts DJ et Al. Ann Surg 2015;00:1–11
--------------------------------------------------------------
Il est souvent estimé que l'hypotension artérielle est un des symptômes clé du pneumothorax suffocant. Pourtant ceci semble surtout vrai pour le pneumothorax sous machine et beaucoup moins pour le pneumothorax du patient en ventilation spontanée.
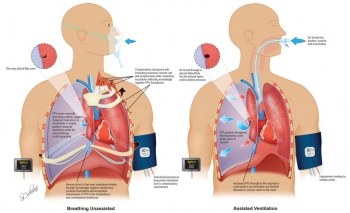
Chez le sujet en ventilation spontanée, l'hypotension est tardive. tachypnée et détresse respiratoire sont au premier plan.
| Tags : pneumothorax
28/12/2014
Un trocard de coelio ?
Standard laparoscopic trocars for the treatment of tension pneumothorax: A superior alternative to needle decompression
Quinton H. et Al. J Trauma Acute Care Surg. 2014;77: 170-175.
-------------------------------------------------------
Le recours à un cathéter d'au moins 8 cm est prôné par certains du fait de l'épaisseur de la paroi thoracique. L'inconvénient de cette longueur est le risque non négligeable de ponction parenchymateuse surtout lors de l'emploi de la voie antérieure.
La voie latérale exposerait maoins à ce risque. Une alternative bien moins dangereuse et toute aussi efficace est la thoracostomie au doigt. Et pourquoi pas un trocard de coelio ?
-------------------------------------------------------
BACKGROUND: Needle thoracostomy (NT) is a commonly taught intervention for tension pneumothorax (tPTX) but has a high failure rate. We hypothesize that standard 5-mm laparoscopic trocars may be a safe and more effective alternative.
METHODS: Thirty episodes of tPTX and 27 episodes of tension-induced pulseless electrical activity (PEA) were induced in five adult swine using thoracic CO2 insufflation via balloon trocar. Tension was defined as a 50% decrease in cardiac output. Chest decompression was performed with 5-mm laparoscopic trocars for the treatment of both tPTX with hemodynamic compromise and tension-induced PEA. The lungs and heart were inspected and graded at necropsy for trocar-related injury. Results were also compared with success rates with NT in the same model.
RESULTS: The placement of a 5-mm trocar rapidly and immediately relieved tension physiology in 100% of the cases. Mean arterial pressure, cardiac output, central venous pressure, and pulmonary capillary wedge pressure all returned to baseline within 1 minute of trocar placement. Adequate perfusion was restored in 100% of tension-induced PEA cases within 30 seconds of trocar placement. There was no evidence of trocar-related heart or lung damage in any of the experimental animals at necropsy (mean injury scores, 0 for both). Fivemillimeter trocars significantly outperformed standard NT for both tPTX and tension-induced PEA arrest.
CONCLUSION: tPTX and tension-induced PEA can be safely and effectively treated with chest decompression using 5-mm laparoscopic trocars. This technique may serve as a more rapid and reliable alternative to needle decompression.
| Tags : pneumothorax
17/11/2014
Pneumothorax et vol en altitude : Possible ?
Cleared for takeoff: The effects of hypobaric conditions on traumatic pneumothoraces
Majercik S. et All. J Trauma Acute Care Surg. 2014;77: 729-733
| Tags : pneumothorax
10/12/2013
Thoracostomie au doigt: Le mieux !
Simple thoracostomy in prehospital trauma management is safe and effective: a 2-year experience by helicopter emergency medical crews
Massaruttia D et Al. Eur J Emerg Med. 2006 Oct;13(5):276-80
-----------------------------------------------------------------------
La réalisation d'une exsufflation à l'aiguille bien que classique reste discutable du fait de nombreux problèmes techniques et du caractère très relatif de son efficacité. La thoracostomie au doigt doit être considérée comme la technique de référence.
-----------------------------------------------------------------------
OBJECTIVE:
To evaluate the effectiveness and potential complications of simple thoracostomy, as first described by Deakin, as a method for prehospital treatment of traumatic pneumothorax.
METHODS:
Prospective observational study of all severe trauma patients rescued by our Regional Helicopter Emergency Medical Service and treated with on-scene simple thoracostomy, over a period of 25 months, from June 1, 2002 to June 30, 2004.
RESULTS:
Fifty-five consecutive severely injured patients with suspected pneumothorax and an average Revised Trauma Score of 9.6+/-2.7 underwent field simple thoracostomy. Oxygen saturation significantly improved after the procedure (from 86.4+/-10.2% to 98.5%+/-4.7%, P<0.05). No difference exists in the severity of thoracic lesions between patients with systolic arterial pressure and oxygen saturation below and above or equal to 90. A pneumothorax or a haemopneumothorax was found in 91.5% of the cases and a haemothorax in 5.1%. No cases of major bleeding, lung laceration or pleural infection were recorded. No cases of recurrent tension pneumothorax were observed. Forty (72.7%) patients survived to hospital discharge.
CONCLUSIONS:
Prehospital treatment of traumatic pneumothorax by simple thoracostomy without chest tube insertion is a safe and effective technique.
| Tags : pneumothorax
01/09/2013
Pneumothorax: Pansement NON OCCLUSIF
Vented versus unvented chest seals for treatment of pneumothorax and prevention of tension pneumothorax in a swine model
Kheirabadi BS et all. J Trauma Acute Care Surg. 2013;75: 150-156
La procédure du sauvetage au combat indique qu'un thorax ouvert ne doit JAMAIS être fermé et qu'un pansement 3 côtés doit être mis en place pour éviter toute surpression intrathoracique. Ceci diffère du TCCC américain qui recommande l'occlusion de la plaie et la surveillance du blessé à la recherche d'un pneumothorax suffocant. Mais les choses évoluent à la lumière de la remise en question de pratiques pas toujours bien documentées. Le TCCC va proposer le recours non pas à l'emploi d'un pansement 3 côtés consommateur de temps mais à l'utilisation de pansements adhésifs prêts à l'emploi.
L'article présenté montre très clairement l'intérêt de la mise en place de pansement permettant l'évacuation de l'air intrathoracique.
Au delà de l'intérêt des dispositifs prêts à l'emploi avec valve de surpression, il y a le problème du choix du modèle. La procédure du sauvetage au combat propose la valve d'asherman, qui doit être considérée comme obsolète car bien qu'efficace, sa capacité d'adhésion à la peau est perfectible. Il semble que les modèles concurrents (Hyfin Vent Chest Seal, SAM chest seal et Sentinel chest seal) proposés par l'industrie aient la même efficacité
| Tags : exsufflation, pneumothorax, matériel
02/07/2013
Pneumothorax: Dès 10 mmHg
Physiology and cardiovascular effect of severe tension pneumothorax in a porcine model
Nelson D et all. J Surg Res. 2013 Jun 5. pii: S0022-4804(13)00505-2
BACKGROUND:
Pneumothoraces are relatively common among trauma patients and can rapidly progress to tension physiology and death if not identified and treated. We sought to develop a reliable and reproducible large animal model of tension pneumothorax and to examine the cardiovascular effects during progression from simple pneumothorax to tension pneumothorax.
MATERIALS AND METHODS:
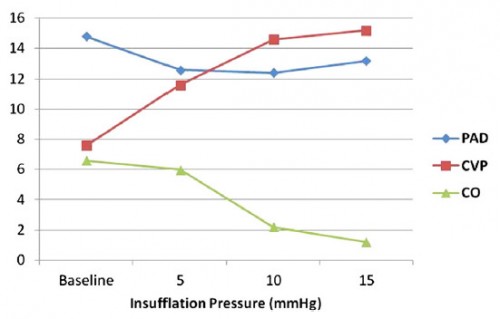
Ten swine were intubated, sedated, and placed on mechanical ventilation. After a midline celiotomy, a 10-mm balloon-tipped laparoscopic trocar was placed through the diaphragm, and a 28F chest tube was placed in the standard position and clamped. Thoracic insufflation was performed in 5-mm increments, and continuous cardiovascular measurements were obtained.
RESULTS:
Mean insufflation pressures of 10 mm Hg were associated with a 67% decrease in cardiac output (6.6 L/min versus 2.2 l/min; P = 0.04). An additional increase in the insufflation pressure (mean 15 mm Hg) was associated with an 82% decrease in cardiac output from baseline (6.8 versus 1.2 L/min; P < 0.01). Increasing insufflation pressures were associated with a corresponding increase in central venous pressure (from 7.6 mm Hg to 15.2 mm Hg; P < 0.01) and a simultaneous decrease in the pulmonary artery diastolic pressure (from 15 mm Hg to 12 mm Hg; P = 0.06), with the central venous pressure and pulmonary artery diastolic pressure approaching equalization immediately before the development of major hemodynamic decline. Pulseless electrical activity arrest was induced at an average of 20 mm Hg. Tension physiology was immediately reversible with adequate decompression, allowing for multiple repeated trials.
CONCLUSIONS:
A reliable and highly reproducible model was created for severe tension pneumothorax in a large animal. Major cardiovascular instability proceeding to pulseless electrical activity arrest with stepwise insufflation was noted. This model could be highly useful for studying new diagnostic and treatment modalities for tension pneumothorax.
| Tags : pneumothorax