05/04/2016
Immobiliser le rachis: Comme il faut !
Safety of the lateral trauma position in cervical spine injuries: a cadaver model study
Hyldmo PK et Al. Acta Anaesthesiol Scand. 2016 Mar 7. doi: 10.1111/aas.12714.
__________________________
Bien immobiliser un rachis avec la bonne position. Lire aussi 1, 2, 3
__________________________

| Tags : rachis
04/08/2015
Collier cervical: Pas utile ?
Cervical spine injury in dismounted improvised explosive device trauma
Taddeo j et Al. Can J Surg. 2015 Jun; 58(3 Suppl 3): S104–S107
-------------------------------
La mise en place d'un collier cervical est une mesure classique en traumaotlogie routière. Elle n'est cependant pas recommandée en cas de traumatisme d'origine ballistique. La probabilité de lésions instables du rachis semble faible surtout si il s'agit de blessures survenues lors de combat à pied et sans atteinte crânienne associée. L'étude présentée conforte cette position.
-------------------------------
Background
The injury pattern from improvised explosive device (IED) trauma is different if the target is in a vehicle (mounted) or on foot (dismounted). Combat and civilian first response protocols require the placement of a cervical collar on all victims of a blast injury.
Methods
We searched the Joint Theatre Trauma Registry (JTTR) and the Role 3 Hospital, Kandahar Airfield (KAF) database from Mar. 1, 2008, to May 31, 2011. We collected data on cervical fracture; head injury; traumatic amputation; initial blood pressure, pulse, injury severity score (ISS), Glasgow Coma Scale (GCS) score and base excess; and patient demographic information.
Results
The concordance rate between JTTR and KAF databases was 98%. Of the 15 693 admissions in JTTR, 326 patients with dismounted IED injuries were located. The rate of cervical collar prehospital placement was 7.6%. Cervical fractures were found in 19 (5.8%) dismounted IED victims, but only 4 (1.2%) were considered radiographically unstable. None of these 19 patients had prehospital placement of a collar. Patients with cervical spine fractures were more severely injured than those without (ISS 18.2 v. 13.4; GCS 10.1 v. 12.5). Patients with head injuries had significantly higher risk of cervical spine injury than those with no head injury recorded (13.6% v. 3.9%). No differences in frequency of cervical spine injury were found between patients who had associated traumatic amputations and those who did not (5.4% v. 6.0%).
Conclusion
Dismounted IED is a mechanism of injury associated with a low risk for cervical spine trauma. A selective protocol for cervical collar placement on victims of dismounted IED blasts is possible and may be more amenable to combat situations.
| Tags : rachis
03/03/2015
Stabilisation du rachis: C'est particulier en milieu hostile
Recommandation 1 (grade:1C) :
Neutral alignment should be restored and maintained with light or moderate manual cervical traction during extrication, unless such a maneuver is met with resistance, increased pain, or new or worsening neurologic deficit.
Recommandation 2 (grade:1C):
Patients requiring extrication, when the cervical spine cannot be cleared before extrication, should be placed in a cervical collar and allowed to exit the situation under their own volition if alert and reliable. Otherwise extrication should be performed with a KED (or similar device) plusc ervical collar,and the immobilized patient moved in a sitting position onto a long spine board, vacuum mattress, orsimilar device.
Recommandation 3 (grade:1C):
The lift and slide transfer with trap squeeze is preferred to the log roll when transferring patients to and from a backboard
Recommandation 4 (grade:2C):
Spinal immobilization should be considered in patients with evidence of spinal injury, including those with neurologic injury, and those patients who have experienced severe trauma and are unconscious or exhibit altered mental status.
Recommandation 5 (grade:2B):
The cervical collar (or improvised equivalent) should beconsidered one ofs everal tools available to aid in immobilization of the cervical spine. It should not be considered adequate immobilization in and of itself, nor should it beconsidered necessary if adequate immobilization can be accomplished by other means, or if the presence of the collar in itself compromises emergent patient care.
Recommandation 6 (grade:1B):
Use of the cervical collar is contraindicated in ankylosing spondylitis. Patients with suspected injury should hav etheir neck supported in a position of comfort
Recommandation 6 (grade:1C):
Vacuum mattress provides superior immobilization, with or without a standard cervical collar, and improved patient comfort (with corresponding decreased risk of pressure sores) and is preferred over a backboard for immobilization of either the entire spine or specific segments of concern.
Recommandation 6 (grade:1A):
Appropriately trained personnel, using either the NEXUS criteria or the Canadian C- spine rule, can safely and effectively make decisions in the prehospital setting about whether or not ac ervical spine should be immobilized.
Recommandation 7(grade:1B):
Spinal immobilization should not be performed in the presence of penetrating trauma
Clic sur l'image pour accéder au document
| Tags : rachis, immobilisation
13/05/2014
Lésions rachidiennes: Plus fréquentes qu'envisagé
Spinal Injuries in United States Military Personnel Deployed to Iraq and Afghanistan
An Epidemiological Investigation Involving 7877 Combat Casualties From 2005 to 2009
Schoenfeld AJ et All. Spine 2013;38:1770–1778
Les lésions du rachis sont plus fréquentes que ce qui était supposé. Ce travail rapporte qu'une atteinte du rachis est présente dans 11% des cas. Une des explications est que l'amélioration des conditions de prise en charge permet la survie de blessés plus graves qu'auparavant, qui autrefois ne survivait pas à leurs blessures.
-----------------------------------------------------------
In the years 2005 to 2009, 872 (11.1%) casualties with spine injuries were identified among a total of 7877 combat wounded. The mean age of spine casualties was 26.6 years. Spine fractures were the most common injury morphology, comprising 83% of all spinal wounds. The incidence of combat-related spinal trauma was 4.4 per 10,000, whereas that of spine fractures was 4.0 per 10,000. Spinal cord injuries occurred at a rate of 4.0 per 100,000.
Spinal cord injuries were most likely to occur in Afghanistan (incident rate ratio: 1.96; 95% confi dence interval: 1.68–2.28), among Army personnel (incident rate ratio: 16.85; 95% confidence interval: 8.39–33.84), and in the year 2007 (incident rate ratio: 1.90; 95% confi dence interval: 1.55–2.32). Spinal injuries from gunshot were significantly more likely to occur in Iraq (17%) than in Afghanistan (10%, P = 0.02).
-----------------------------------------------------------
| Tags : rachis
21/03/2013
Immobilisation du rachis: Dès que possible ! Surtout si VBIED
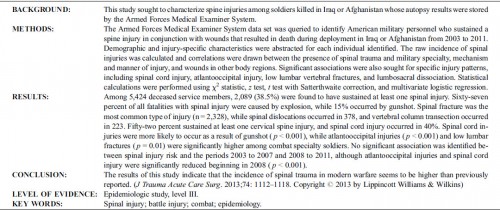
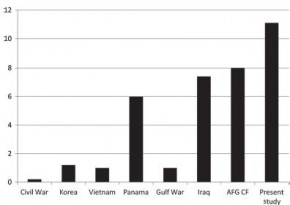
J Trauma Acute Care Surg. 2013;74: 1112-1118
Si l'atteinte du rachis cervical était dans les derniers conflits est de l'ordre de 1 à 2%, ce taux est monté à 5-8% dans le conflit irakien. Ceci s'explique par l'émergence d'un nouveau mécanisme d'aggression par IED. La procédure du sauvetage au combat stipule que l'imobilisation du rachis cervical ne doit pas être réalisée sous le feu direct de l'ennemi. La frequence des lésions du rachis dans les combats actuels l'impose cependant dès que blessé et sauveteurs sont à l'abri surtout si il s'agit d'un VBIED. C'est que suggère cette publication édifiante qui porte sur l'analyse des lésions du rachis cervical chez les soldats décédés.
| Tags : rachis, balistique