Administration of medication is a well-established part of prehospital trauma care. Guidance varies on the types of recommended medications and when they should be administered. Mnemonics have become commonplace in prehospital medicine to facilitate recall and retention. However, there is no comprehensive aid for the administration of medication in trauma patients. We propose a new mnemonic for the delivery of relevant intravenous or intraosseous medications in trauma patients. A ‘4A after Access’ approach should enhance memory recall for the efficient provision of patient care. These 4As are: antifibrinolysis, analgesia, antiemesis and antibiotics. This mnemonic is designed to be used as an optional aide memoire in conjunction with existing treatment algorithms in the military prehospital setting.
13/02/2026
Hémorragie des blessés de guerre: Quoi de disponible ?
--------------------------------
12/12/2025
TXA: 2g IV si trauma crânien
Optimal dose of tranexamic acid in traumatic brain injury: Systematic review and network meta-analysis of randomized controlled trials
Shu U et Al Journal of Trauma and Acute Care Surgery 98(5):p 816-823, May 2025.
BACKGROUND
Tranexamic acid (TXA) has been used to treat traumatic brain injury (TBI); however, no definitive conclusions have been drawn regarding its effectiveness or dosage. This study evaluated the optimal TXA dose for treating TBI using a network meta-analysis (NMA).
METHODS
Five databases were searched for peer-reviewed randomized controlled trials (RCTs) published from inception to May 2024. The inclusion criteria were as follows: (1) RCTs, (2) patients older than 1 month with TBI, (3) interventions of TXA and control, (4) primary outcomes of mortality and poor neurological outcomes and secondary outcomes of vascular occlusive events, and (5) full-text peer-reviewed articles. Two reviewers independently screened and extracted the data and assessed the risk of bias. Frequency-based NMA was performed using the Grading of Recommendations, Assessment, Development, and Evaluation working-group approach.
RESULTS
We included 10 RCTs comprising 11,237 patients with TBI. Placebo showed higher mortality compared with that of a 2-g bolus of TXA (risk ratio, 1.53; 95% confidence interval, 1.08–2.17). Higher mortality was observed with a 1-g bolus of TXA followed by 1-g maintenance TXA compared with that of a 2-g bolus of TXA (risk ratio, 1.44; 95% confidence interval, 1.02–2.03). No significant differences in poor neurological outcomes or vascular occlusive events were observed between the treatment groups.

CONCLUSION
Placebo and a 1-g bolus followed by 1-g maintenance TXA were associated with higher mortality rates than those of a 2-g bolus of TXA. No difference in vascular occlusive events was observed with either treatment, indicating that our NMA recommends 2 g of TXA. However, the data for the 2-g bolus of TXA were from a single study, and further research is needed to draw definitive conclusions.
eFAST et thorax ouvert: Manque de sensibilité +++
Accuracy, reliability, and utility of the extended focused assessment with sonography in trauma examination in the setting of thoracic gunshot wounds
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
------------------------------------------
eFAST en cas de thorax ouvert ? Et bien pas si sûr
------------------------------------------
BACKGROUND
The extended focused assessment with sonography in trauma (eFAST) examination includes additional thoracic views beyond the standard focused assessment with sonography in trauma examination. Its validation has predominantly been conducted in blunt trauma cases. Our aim was to evaluate the eFAST examination in a targeted population with penetrating thoracic trauma.
METHODS
Patients with thoracic gunshot wounds who underwent eFAST between 2017 and 2021 were included from a local trauma registry. Performance metrics for each component of eFAST in each window and pathological condition were analyzed across the entire population, as well as within two cohorts: survived and deceased patients. Chest tube placement rates were compared within true-positive and false-negative (FN) eFAST results for subgroups with pneumothorax or hemothorax.
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
RESULTS
A total of 288 patients were included (male, 91% male; Injury Severity Score ≥15, 48%; and died, 17%). Thirty-nine percent required chest tube, and 18% required urgent thoracic surgical intervention. Although specificity was high (91–100%) for all components, the sensitivity was less than 50% for all thoracic views, except for “no cardiac motion” (100% sensitivity). Sensitivity for pericardial fluid was 47%; for pneumothorax, 22%; for hemothorax, 36%; and for peritoneal fluid, 51% in the total population. Comparing survived versus deceased cohort, the eFAST sensitivity was higher among deaths for all components. The majority of patients (>70%) with a FN eFAST for pneumothorax or hemothorax received chest tube.

CONCLUSION
The eFAST examination showed highly variable performance metrics among patients with penetrating thoracic trauma, with all thoracic components demonstrating high specificity but low overall sensitivity. Urgent interventions were frequently received in patients with FN studies.
le x et M avant A. Transfuser avant d'intuber ?
Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know.
Paula Ferrada P et Al. J Trauma Acute Care Surg. 2025 Jul 4.
----------------------------------------------------
Hemorrhage remains a leading cause of preventable trauma-related mortality, with early resuscitation and hemorrhage control serving as crucial interventions. Emerging evidence suggests that prioritizing circulation before airway (Circulation, Airway, and Breathing [CAB]) during initial resuscitation in patients with exsanguinating injuries can improve survival by avoiding the deleterious effects of postintubation hypotension. This article reviews current evidence supporting the CAB approach and outlines best practices across prehospital, emergency department, and operative settings. Delaying advanced airway management while focusing on immediate hemorrhage control and blood product resuscitation has been associated with decreased 24-hour and 30-day mortality. This review synthesizes findings from recent multicenter trials and literature supporting the CAB paradigm, with practical recommendations for implementation in trauma care systems.
----------------------------------------------------
02/12/2025
Les drones changent la donne
20/11/2025
Chaine de survie 21ème siècle: Réflexions US
Clic sur l'image pour accéder au document
Le facteur humain reste CENTRAL
"While technology continues to transform warfare, the human element remains central to military medicine. The operational ‘kill chain’ may be accelerated by drones and artificial intelligence. However, the medical ‘survival chain’ still demands human judgement, compassion, and moral courage"
01/10/2025
Combats actuels, le mieux: Une structure chirurgicale à 1 heure
Modeling Musculoskeletal Combat Casualty Care: NATO Trauma System Performance in Large Scale Combat Operations
Cote MP et Al. JB JS Open Access. 2025 Sep 11;10(3):e25.00194. doi: 10.2106/JBJS.OA.25.00194.
Background:
It is unclear whether the current North Atlantic Treaty Organization (NATO) trauma system will be effective in the setting of Large-Scale Combat Operations (LSCO). We sought to model the efficacy of the NATO trauma system in the setting of LSCO. We also intended to model novel scenarios that could better adapt the current system to LSCO.
Methods:
We developed a discrete-event simulation model for patients with combat musculoskeletal injuries treated within the standard NATO system. The primary outcome of the model was survival. The model's health states were characterized as stable, hypovolemia, sepsis, shock, or death. The model simulated combat intensity by increasing the number of casualties up to 192 casualties per 24 hours. We explored how an augmented system (FC) and Field Hospital (FH) moved closer to the battlefront would change performance.
Results:
Mortality rates rose precipitously from a 10% baseline to 61% at 12 casualties per 24 hours in the base model. This performance was not significantly different from that of the FC model at any casualty rate. Successful evacuation of casualties was significantly more for the FH model versus the base model at 12 casualties/24 hours (47.5% vs. 39%; p = 0.046), 48 casualties/24 hours (45.5% vs. 33%; p = 0.008), and 192 casualties/24 hours (25% vs. 15.5%; p = 0.02).
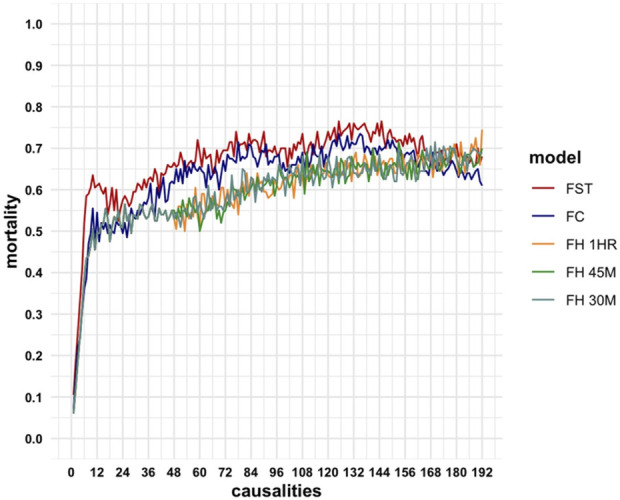
Conclusions:
The current NATO model experiences high rates of mortality in LSCO. The most effective modification entails situating Field Hospitals within one-hour of ground transport from the battlefront.
17/01/2025
Conflit ukrainien: Pour de la chirurgie encore plus proche des combats
02/01/2025
1 blessé sur 2 ne fait l'objet d'aucune mesure de sauvetage
Advancing Prehospital Combat Casualty Evacuation: Patients Amenable to Aeromedical Evacuation via Unmanned Aerial Vehicles
Maddry JK et Al. Mil Med. 2021 Feb 26;186(3-4):e366-e372.
Introduction: The U.S. military currently utilizes unmanned aerial vehicles (UAVs) for reconnaissance and attack missions; however, as combat environment technology advances, there is the increasing likelihood of UAV utilization in prehospital aeromedical evacuation. Although some combat casualties require life-saving interventions (LSIs) during medical evacuation, many do not. Our objective was to describe patients transported from the point of injury to the first level of care and characterize differences between patients who received LSIs en route and those who did not.
Materials and methods: We conducted a retrospective review of the records of traumatically injured patients evacuated between January 2011 and March 2014. We compared patient characteristics, complications, and outcomes based on whether they had an LSI performed en route (LSI vs. No LSI). We also constructed logistic regression models to determine which characteristics predict uneventful flights (no en route LSI or complications).
Results: We examined 1,267 patient records; 47% received an LSI en route. Most patients (72%) sustained a blast injury and injuries to the extremities and head. Over 78% experienced complications en route; the LSI group had higher rates of complications compared to the No LSI group. Logistic regression showed that having a blunt injury or the highest abbreviated injury scale (AIS) severity score in the head/neck region are significant predictors of having an uneventful flight.
Conclusion: Approximately half of casualties evaluated in our study did not receive an LSI during transport and may have been transported safely by UAV. Having a blunt injury or the highest AIS severity score in the head/neck region significantly predicted an uneventful flight.
09/10/2024
Combat à haute intensité: Tout repenser !
Casualty care implications of large-scale combat operations
Mason H. Remondelli MH et Al. J Trauma Acute Care Surg. 2023 Aug; 95(2 ): S180–S184.
----------------------------------------------------------------------------------
Cet article met en exergue la nécessité de repenser en profondeur l'organisation de la chaîne santé , la place prépondérante de la transfusion sanguine et l'intérêt de petites équipes chirurgicales mobiles intervenant "enterrées" au plus près des combats
----------------------------------------------------------------------------------
30/09/2024
En Ukraine ?
Lessons learned from the war in Ukraine for the anesthesiologist and intensivist: A scoping review
Jarrassier A. et Al Anaesth Crit Care Pain Med. 2024 Jul 30;43(5):101409.
--------------------------
Un point de situation particulièrement intéressant qui met en avant la nécessité de prendre en compte les spécificités de cette guerre à haute intensité: De nouvelles modalités lésionnelles notamment par les armes thermo-bariques, les difficultés de l'établissement d'une chaîne maîtrisée de prise en charge des blessés avec la réapparition du train comme vecteur d'évacuation, bien souvent la nécessité de porter la chirurgie au plus près des combats en s'appuyant sur les hôpitaux d'infrastructures, la difficulté de l'approvisionnement notamment en dérivés sanguins, la réapparition de la discussion sur le garrot, la nécessité de disposer d'équipes parfaitement formées et entraînées pour intervenir dans de telles conditions, la place tout à fait particulière et prééminente des anesthésistes-réanimateurs dans de telles situations.
Une bonne partie de ces constatations avaient été faites notamment lors de la crise COVID (histoire de l'EMR SSA de Mulhouse puis dans les DOM). Oui mais elles ont été oubliées noyées dans le quotidien.
Background
The war in Ukraine provides purposefully anesthesiologists and intensivists with important data for improving the management of trauma patients. This scoping review aims to investigate the specific management of war-related trauma patients, during the war in Ukraine, through an objective and comprehensive analysis.
Methods
A comprehensive search of the Embase, Medline, and Open Grey databases from 2014 to February 2024 yielded studies focusing on anesthesia and surgery. These studies were assessed by PRISMA and STROBE criteria and needed to discuss anesthesiology and surgical procedures.
Results
Of the 519 studies identified, 21 were included, with a low overall level of evidence. The studies covered 11,622 patients and 2470 surgical procedures. Most patients were Ukrainian men, 25–63 years old, who had sustained severe injuries from high-energy weapons, such as multiple rocket systems and combat drones. These injuries included major abdominal, facial, and extremity traumas. The surgical procedures varied from initial debridement to complex reconstructions. Anesthesia management faced significant challenges, including resource scarcity and the need for quick adaptability. Evacuations of casualties were lengthy, complex, and often involved rail transportation. Hemorrhage control with tourniquets was critical but associated with many complications. The very frequent presence of multi-resistant organisms required dedicated preventive measures and appropriated treatments. The need for qualified human resources underscored the importance of civilian-military cooperation.
Conclusion
This scoping review provides original and relevant insights on the lessons learned from the ongoing war in Ukraine, which could be useful for anesthesiologists and intensivists.
06/05/2024
La "chaine de survie" du combat moderne: A révolutionner, et cela presse
The “Survival Chain” Medical Support to Military Operations on the Future Battlefield
Gurney MJ et Al. JFQ 112, 1st Quarter 2024
Un plaidoyer pour plus de technicité, de savoir faire , d'agilité bref une professionnalisation encore plus grande des équipes santé vers le trauma et la réanimation.
Clic sur l'image
02/04/2024
Les gestes US du Role 1 chez les américains
An Analysis of 13 Years of Prehospital Combat Casualty Care: Implications for Maintaining a Ready Medical Force
Schauer SG et Al. Prehosp Emerg Care. 2022 May-Jun;26(3):370-379.
----------------------------------
Des choses simples dans un contexte où les medevac étaient très rapides, ce qui n'est plus le cas. Poser des garrots est toujours nécessaires MAIS ne suffit plus. Les gestes sophistiqués de réanimation doivent absolument être maîtrisées. Cela passe par une autre vision, que celle actuelle, de la médicalisation de l'avant.
----------------------------------
Background:
Most potentially preventable deaths occur in the prehospital setting before reaching a military treatment facility with surgical capabilities. Thus, optimizing the care we deliver in the prehospital combat setting represents a ripe target for reducing mortality. We sought to analyze prehospital data within the Department of Defense Trauma Registry (DODTR).
Materials and methods:
We requested all encounters with any prehospital activity (e.g., interventions, transportation, vital signs) documented within the DODTR from January 2007 to March 2020 along with all hospital-based data that was available. We excluded from our search casualties that had no prehospital activity documented.
Results:
There were 28,950 encounters that met inclusion criteria. Of these, 25,897 (89.5%) were adults and 3053 were children (10.5%). There was a steady decline in the number of casualties encountered with the most notable decline occurring in 2014. U.S. military casualties comprised the largest proportion (n = 10,182) of subjects followed by host nation civilians (n = 9637). The median age was 24 years (interquartile range/IQR 21-29).
Most were battle injuries (78.6%) and part of Operation ENDURING FREEDOM (61.8%) and Operation IRAQI FREEDOM (24.4%). Most sustained injuries from explosives (52.1%) followed by firearms (28.1%), with serious injury to the extremities (24.9%) occurring most frequently. The median injury severity score was 9 (IQR 4-16) with most surviving to discharge (95.0%). A minority had a documented medic or combat lifesaver (27.9%) in their chain of care, nor did they pass through an aid station (3.0%). Air evacuation predominated (77.9%).
Conclusions:
Within our dataset, the deployed U.S. military medical system provided prehospital medical care to at least 28,950 combat casualties consisting mostly of U.S. military personnel and host nation civilian care. There was a rapid decline in combat casualty volumes since 2014, however, on a per-encounter basis there was no apparent drop in procedural volume.
15/03/2024
Plus d'infirmiers spécialisés dans le trauma
Une évidence. Et dans le système français le modèle de cet infirmier est un IADE
ACNPs in the U.S. Army-Medical Force Multipliers for Large-Scale Combat Operations
18/02/2024
Les 4 As: le A de RYAN
27/01/2024
Traumatisé par armes à feu: Trauma Center mais aussi un meilleur préhospitalier ?
A Decade of Firearm Injuries: Have We Improved ?
Sarah A Hatfield SA et Al. J Trauma Acute Care Surg. 2024 Jan 16.doi: 10.1097/TA.0000000000004249.
Background:
Firearm injuries are a growing public health issue, with marked increases coinciding with the coronavirus disease 2019 (COVID-19) pandemic. This study evaluates temporal trends over the past decade, hypothesizing that despite a growing number of injuries, mortality would be unaffected. In addition, the study characterizes the types of centers affected disproportionately by the reported firearm injury surge in 2020.
Methods:
Patients aged 18 years and older with firearm injuries from 2011-2020 were identified retrospectively using the National Trauma Data Bank (NTDB®). Trauma centers not operating for the entirety of the study period were excluded to allow for temporal comparisons. Joinpoint regression and risk-standardized mortality ratios (SMR) were used to evaluate injury counts and adjusted mortality over time. Subgroup analysis was performed to describe centers with the largest increases in firearm injuries in 2020.
Results:
A total of 238,674 patients, treated at 420 unique trauma centers, met inclusion criteria. Firearm injuries increased by 31.1% in 2020, compared to an annual percent change of 2.4% from 2011-2019 (p = 0.01). Subset analysis of centers with the largest changes in firearm injuries in 2020 found that they were more often level I centers, with higher historic trauma volumes and percentages of firearm injuries (p < 0.001). Unadjusted mortality decreased by 0.9% from 2011-2020, but after controlling for demographics, injury characteristics and physiology, there was no difference in adjusted mortality over the same time period. However, among patients with injury severity scores ≥25, adjusted mortality improved compared to 2011 (SMR of 0.950 in 2020, 95% CI 0.916 - 0.986).
Conclusions:
Firearm injuries pose an increasing burden to trauma systems, with level I and high-volume centers seeing the largest growth in 2020. Despite increasing numbers of firearm injuries, mortality has remained unchanged over the past decade.
01/12/2023
Military Medicine
28/11/2023
Conflit en Ukraine: Enseignements, vision UK
Transferable military medical lessons from the Russo-Ukraine war
Hodgetts TJ, et al. BMJ Mil Health 2023;0:1–4
The first year of the war in Ukraine has presented critical lessons for the UK’s Defence Medical Services (DMS) regarding its preparedness to support the nation for warfighting at scale. There are tactical, clinical, and strategic challenges that must be addressed. The war has exposed the limitations of international humanitarian law and the laws of armed conflict in protecting forward field hospitals from deliberate targeting. The DMS may need to employ measures such as disguise, deception, and dispersal to provide care in a contested environment. The historical trend of disinvestment in military medical capability between major conflicts, known as the "Walker Dip," represents a clinical risk that must be mitigated. Even if this is achieved, clinical outcomes during large-scale warfighting are likely to be worse that those the nation has come to expect during more low-intensity conflicts. Effective civilian-military collaboration will be paramount to manage casualties at scale. Both novel and reversionary modes of transportation may be required, such as the mass movement of casualties by train. The need for a sufficient and capable medical workforce, amid global shortages and post-COVID burnout, calls for further investment. The DMS requires innovation and adaptability to harness the ability to adopt external ideas, translate successful innovations and address complex challenges. By addressing tactical vulnerabilities, enhancing clinical preparedness, fostering civilian-military collaboration, and embracing innovation, the DMS will be better equipped to support the UK and allied armed forces in future warfighting at scale.
25/11/2023
Intubation des traumas sévères pénétrants
Prehospital and emergency department airway management of severe penetrating trauma in Sweden during the past decade
Renberg M et Al. Scand J Trauma Resusc Emerg Med. 2023 Nov 24;31(1):85
------------------------------------
On sait cet exercice difficile même entre des mains expérimentées. Cet article le confirme. N'oublions pas; ce qui compte en premier c'est d'oxygéner. Avant de procéder à une intubation, bien évaluer l'état hémodynamique car une induction et une mise sous respirateur peuvent l'altérer, voire être responsable d'un arrêt cardiaque.
------------------------------------
Background:
Prehospital tracheal intubation (TI) is associated with increased mortality in patients with penetrating trauma, and the utility of prehospital advanced airway management is debated. The increased incidence of deadly violence in Sweden warrants a comprehensive evaluation of current airway management for patients with penetrating trauma in the Swedish prehospital environment and on arrival in the emergency department (ED).
Methods:
This was an observational, multicenter study of all patients with penetrating trauma and injury severity scores (ISSs) ≥ 15 included in the Swedish national trauma register (SweTrau) between 2011 and 2019. We investigated the frequency and characteristics of prehospital and ED TI, including 30-day mortality and patient characteristics associated with TI.
Result:
Of 816 included patients, 118 (14.5%) were intubated prehospitally, and 248 (30.4%) were intubated in the ED. Patients who were intubated prehospitally had a higher ISS, 33 (interquartile range [IQR] 25, 75), than those intubated in the ED, 25 (IQR 18, 34). Prehospital TI was associated with a higher associated mortality, OR 4.26 (CI 2.57, 7.27, p < 0.001) than TI in the ED, even when adjusted for ISS (OR 2.88 [CI 1.64, 5.14, p < 0.001]). Hemodynamic collapse (≤ 40 mmHg) and low GCS score (≤ 8) were the characteristics most associated with prehospital TI. Traumatic cardiac arrests (TCAs) occurred in 154 (18.9%) patients, of whom 77 (50%) were intubated prehospitally and 56 (36.4%) were intubated in the ED. A subgroup analysis excluding TCA showed that patients with prehospital TI did not have a higher mortality rate than those with ED TI, OR 2.07 (CI 0.93, 4.51, p = 0.068), with OR 1.39 (0.56, 3.26, p = 0.5) when adjusted for ISS.
Conclusion:
Prehospital TI was associated with a higher mortality rate than those with ED TI, which was specifically related to TCA; intubation did not affect mortality in patients without cardiac arrest. Mortality was high when airway management was needed, regardless of cardiac arrest, thereby emphasizing the challenges posed when anesthesia is needed. Several interventions, including whole blood transfusions, the implementation of second-tier EMS units and measures to shorten scene times, have been initiated in Sweden to counteract these challenges. Sweden.
| Tags : intubation, airway
20/11/2023
Les anesthésistes: Pièce importante dans les guerres hybrides
A Gray Future: The Role of the Anesthesiologist in Hybrid Warfare
Granholm F et Al. Anesthesiology. 2023 Nov 1;139(5):563-567.
During the last few decades, the increasing use of asymmetric and multimodal tactics by terrorists has led anesthesiologists worldwide to analyze and discuss their role in mass casualty scenarios in more depth. Now anesthesiologists must address the new situation of hybrid threats and hybrid warfare. This will have a direct impact on anesthesiology and intensive care, and in the end, the health and well-being of critical patients of all ages. To be able to respond to a hybrid threat efficiently and effectively, it is imperative that anesthesiologists play an early and integral role in mitigation and response planning.