04/03/2019
Transfusion: Numéro spécial Trauma
02/11/2018
Blessés admis en role 2: Le bilan afghan
A Review of Casualties Transported to Role 2 Medical Treatment Facilities in Afghanistan.
---------------------------------------
Ce document met en évidence tout l'apport d'une chaine coordonnée de prise en charge du traumatisé par des équipes entraînées appliquant une stratégie médico-chirurgicale moderne.
---------------------------------------
Critically injured trauma patients benefit from timely transport and care. Accordingly, the provision of rapid transport and effective treatment capabilities in appropriately close proximity to the point of injury will optimize time and survival. Pre-transport tactical combat casualty care, rapid transport with en route casualty care, and advanced damage control resuscitation and surgery delivered early by small, mobile, forward-positioned Role 2 medical treatment facilities have potential to reduce morbidity and mortality from trauma. This retrospective review and descriptive analysis of trauma patients transported from Role 1 entities to Role 2 facilities in Afghanistan from 2008 to 2014 found casualties to be diverse in affiliation and delivered by various types and modes of transport. Air medical evacuation provided transport for most patients, while the shortest transport time was seen with air casualty evacuation. Although relatively little data were collected for air casualty evacuation, this rapid mode of transport remains an operationally important method of transport on the battlefield. For prehospital care provided before and during transport, continued leadership and training emphasis should be placed on the administration and documentation of tactical combat casualty care as delivered by both medical and non-medical first responders.
08/10/2018
Military Medicine: Numéro spécial 2018
15/09/2018
Aggressions collectives par arme de guerre
10/09/2018
Settings standard for CCC
08/09/2018
Le TCCC dans la vraie vie
Survey of Casualty Evacuation Missions Conducted by the 160th Special Operations Aviation Regiment During the Afghanistan Conflict.
BACKGROUND:
Historically, documentation of prehospital combat casualty care has been relatively nonexistent. Without documentation, performance improvement of prehospital care and evacuation through data collection, consolidation, and scientific analyses cannot be adequately accomplished. During recent conflicts, prehospital documentation has received increased attention for point-of-injury care as well as for care provided en route on medical evacuation platforms. However, documentation on casualty evacuation (CASEVAC) platforms is still lacking. Thus, a CASEVAC dataset was developed and maintained by the 160th Special Operations Aviation Regiment (SOAR), a nonmedical, rotary-wing aviation unit, to evaluate and review CASEVAC missions conducted by their organization.
METHODS:
A retrospective review and descriptive analysis were performed on data from all documented CASEVAC missions conducted in Afghanistan by the 160th SOAR from January 2008 to May 2015. Documentation of care was originally performed in a narrative after-action review (AAR) format. Unclassified, nonpersonally identifiable data were extracted and transferred from these AARs into a database for detailed analysis. Data points included demographics, flight time, provider number and type, injury and outcome details, and medical interventions provided by ground forces and CASEVAC personnel.
RESULTS:
There were 227 patients transported during 129 CASEVAC missions conducted by the 160th SOAR. Three patients had unavailable data, four had unknown injuries or illnesses, and eight were military working dogs. Remaining were 207 trauma casualties (96%) and five medical patients (2%). The mean and median times of flight from the injury scene to hospital arrival were less than 20 minutes. Of trauma casualties, most were male US and coalition forces (n = 178; 86%). From this population, injuries to the extremities (n = 139; 67%) were seen most commonly. The primary mechanisms of injury were gunshot wound (n = 89; 43%) and blast injury (n = 82; 40%). The survival rate was 85% (n = 176) for those who incurred trauma. Of those who did not survive, most died before reaching surgical care (26 of 31; 84%).
CONCLUSION:
Performance improvement efforts directed toward prehospital combat casualty care can ameliorate survival on the battlefield. Because documentation of care is essential for conducting performance improvement, medical and nonmedical units must dedicate time and efforts accordingly. Capturing and analyzing data from combat missions can help refine tactics, techniques, and procedures and more accurately define wartime personnel, training, and equipment requirements. This study is an example of how performance improvement can be initiated by a nonmedical unit conducting CASEVAC missions.
06/06/2018
March: Aussi chez les chinois
Expert consensus on the evaluation and diagnosis of combat injuries of the Chinese People’s Liberation Army
11/05/2018
Groupe O: Plus de mortalité ?
The impact of blood type O on mortality of severe trauma patients: a retrospective observational study.
BACKGROUND:
Recent studies have implicated the differences in the ABO blood system as a potential risk for various diseases, including hemostatic disorders and hemorrhage. In this study, we evaluated the impact of the difference in the ABO blood type on mortality in patients with severe trauma.
METHODS:
A retrospective observational study was conducted in two tertiary emergency critical care medical centers in Japan. Patients with trauma with an Injury Severity Score (ISS) > 15 were included. The association between the different blood types (type O versus other blood types) and the outcomes of all-cause mortality, cause-specific mortalities (exsanguination, traumatic brain injury, and others), ventilator-free days (VFD), and total transfusion volume were evaluated using univariate and multivariate competing-risk regression models. Moreover, the impact of blood type O on the outcomes was assessed using regression coefficients in the multivariate analysis adjusted for age, ISS, and the Revised Trauma Score (RTS).
RESULTS:
A total of 901 patients were included in this study. The study population was divided based on the ABO blood type: type O, 284 (32%); type A, 285 (32%); type B, 209 (23%); and type AB, 123 (13%). Blood type O was associated with high mortality (28% in patients with blood type O versus 11% in patients with other blood types; p < 0.001). Moreover, this association was observed in a multivariate model (adjusted odds ratio = 2.86, 95% confidence interval 1.84-4.46; p < 0.001). The impact of blood type O on all-cause in-hospital mortality was comparable to 12 increases in the ISS, 1.5 decreases in the RTS, and 26 increases in age.
The comparison of characteristics and outcomes between blood type O and other blood types
| Type O n = 284 |
Non-O type n = 617 |
p value | |
|---|---|---|---|
| Characteristics | |||
| Age, years (SD) | 57.3 (20.0) | 56.2 (19.4) | 0.442 |
| Female, n (%) | 64 (22.5) | 142 (23) | 0.873 |
| Charlson Comorbidity Index, median (IQR) | 0 (0–2) | 0 (0–1) | 0.829 |
| Uncrossmatched type O RBC transfusion, n (%) | 28 (9.9) | 37 (6) | 0.051 |
| RTS, (SD) | 6.85 (1.4) | 7.13 (1.2) | 0.003 |
| ISS, median (IQR) | 18 (16–25) | 19 (16–25) | 0.160 |
| AIS head, median (IQR) | 4 (3–4) | 4 (3–4) | 0.582 |
| AIS face, median (IQR) | 0 (0–0) | 0 (0–0) | 0.783 |
| AIS chest, median (IQR) | 0 (0–2) | 0 (0–3) | 0.342 |
| AIS abdomen, median (IQR) | 0 (0–0) | 0 (0–0) | 0.561 |
| AIS extremities, median (IQR) | 0 (0–2) | 0 (0–2) | 0.443 |
| AIS surface, median (IQR) | 0 (0–0) | 0 (0–0) | 0.652 |
| Outcomes | |||
| In-hospital mortality, n (%) | 80 (28.2) | 71 (11.5) | < 0.001 |
| Death due to exsanguination, n (%) | 23 (8.1) | 15 (2.4) | < 0.001 |
| Death due to TBI, n (%) | 43 (15.1) | 44 (7.1) | < 0.001 |
| Death due to other causes, n (%) | 15 (1.8) | 11 (5.3) | 0.005 |
| Ventilator-free days, mean (SD) | 18.7 (12.2) | 23.1 (9.4) | < 0.001 |
| Units of RBCs administered within 24 h, mean (SD) | 3 (9) | 2 (7) | 0.112 |
Categorical variables are expressed as numbers (%); continuous variables are presented as medians (25–75 percentiles = interquartile range (IQR))
AIS Abbreviated Injury Scale; ISS Injury Severity Score; RBC red blood cell; RTS Revised Trauma Score; SD standard deviation; TBI traumatic brain injury
Furthermore, blood type O was significantly associated with higher cause-specific mortalities and shorter VFD compared with the other blood types; however, a significant difference was not observed in the transfusion volume between the two groups.
CONCLUSIONS:
Blood type O was significantly associated with high mortality in severe trauma patients and might have a great impact on outcomes. Further studies elucidating the mechanism underlying this association are warranted to develop the appropriate intervention.
19/04/2018
Morts évitables Civil vs Militaire: Parle-t-on de la lmême chose ?
Comparison of Military and Civilian Methods for Determining Potentially Preventable Deaths: A Systematic Review.
Importance:
Military and civilian trauma experts initiated a collaborative effort to develop an integrated learning trauma system to reduce preventable morbidity and mortality. Because the Department of Defense does not currently have recommended guidelines and standard operating procedures to perform military preventable death reviews in a consistent manner, these performance improvement processes must be developed.
Objectives:
To compare military and civilian preventable death determination methods to understand the existing best practices for evaluating preventable death.
Evidence Review:
This systematic review followed the PRISMA reporting guidelines. English-language articles were searched from inception to February 15, 2017, using the following databases: MEDLINE (Ovid), Evidence-Based Medicine Reviews (Ovid), PubMed, CINAHL, and Google Scholar. Articles were initially screened for eligibility and excluded based on predetermined criteria. Articles reviewing only prehospital deaths, only inhospital deaths, or both were eligible for inclusion. Information on study characteristics was independently abstracted by 2 investigators. Reported are methodological factors affecting the reliability of preventable death studies and the preventable death rate, defined as the number of potentially preventable deaths divided by the total number of deaths within a specific patient population.
Findings:
Fifty studies (8 military and 42 civilian) met the inclusion criteria. In total, 1598 of 6500 military deaths reviewed and 3346 of 19 108 civilian deaths reviewed were classified as potentially preventable. Among military studies, the preventable death rate ranged from 3.1% to 51.4%. Among civilian studies, the preventable death rate ranged from 2.5% to 85.3%. The high level of methodological heterogeneity regarding factors, such as preventable death definitions, review process, and determination criteria, hinders a meaningful quantitative comparison of preventable death rates.
Conclusions and Relevance:
The reliability of military and civilian preventable death studies is hindered by inconsistent definitions, incompatible criteria, and the overall heterogeneity in study methods. The complexity, inconsistency, and unpredictability of combat require unique considerations to perform a methodologically sound combat-related preventable death review. As the Department of Defense begins the process of developing recommended guidelines and standard operating procedures for performing military preventable death reviews, consideration must be given to the factors known to increase the risk of bias and poor reliability.
20/01/2018
Queensland Clinical Practice Manual
10/11/2017
Prolonged field care: Dans la vrai vie
A survey distributed to US military medical providers solicited details of PFC encounters lasting more than 4 hours and included patient demographics, environmental descriptors, provider training, modes of transportation, injuries, mechanism of injury, vital signs, treatments, equipment and resources used, duration of PFC, and morbidity and mortality status on delivery to the next level of care. Descriptive statistics were used to analyze survey responses.
RESULTS:
Surveys from 54 patients treated during 41 missions were analyzed. The PFC provider was on scene at time of injury or illness for 40.7% (22/54) of cases. The environment was described as remote or austere for 96.3% (52/54) of cases. Enemy activity or weather also contributed to need for PFC in 37.0% (20/54) of cases. Care was provided primarily outdoors (37.0%; 20/54) and in hardened nonmedical structures (37.0%; 20/54) with 42.6% (23/54) of cases managed in two or more locations or transport platforms. Teleconsultation was obtained in 14.8% (8/54) of cases. The prehospital time of care ranged from 4 to 120 hours (median 10 hours), and five (9.3%) patients died prior to transport to next level of care.
CONCLUSION:
PFC in the prehospital setting is a vital area of military medicine about which data are sparse. This review was a novel initial analysis of recent US military PFC experiences, with descriptive findings that should prove helpful for future efforts to include defining unique skillsets and capabilities needed to effectively respond to a variety of PFC contingencies.
| Tags : prolonged field care
26/10/2017
Afflux massif: Que fait on vraiment ?
Prehospital Interventions During Mass-Casualty Events in Afghanistan: A Case Analysis.
BACKGROUND:
Mass-casualty (MASCAL) events are known to occur in the combat setting. There are very limited data at this time from the Joint Theater (Iraq and Afghanistan) wars specific to MASCAL events. The purpose of this report was to provide preliminary data for the development of prehospital planning and guidelines.
METHODS:
Cases were identified using the Department of Defense (DoD; Virginia USA) Trauma Registry (DoDTR) and the Prehospital Trauma Registry (PHTR). These cases were identified as part of a research study evaluating Tactical Combat Casualty Care (TCCC) guidelines. Cases that were designated as or associated with denoted MASCAL events were included. Data Fifty subjects were identified during the course of this project. Explosives were the most common cause of injuries. There was a wide range of vital signs. Tourniquet placement and pressure dressings were the most common interventions, followed by analgesia administration.
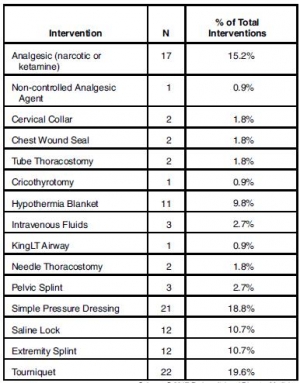
Oral transmucosal fentanyl citrate (OTFC) was the most common parenteral analgesic drug administered. Most were evacuated as "routine." Follow-up data were available for 36 of the subjects and 97% were discharged alive.
CONCLUSIONS:
The most common prehospital interventions were tourniquet and pressure dressing hemorrhage control, along with pain medication administration. Larger data sets are needed to guide development of MASCAL in-theater clinical practice guidelines.
| Tags : mascal
08/05/2017
Hémorragie: De la glace sur le visage ?
Face Cooling Increases Blood Pressure during Simulated Blood Loss
B. Johnson et Al. Proceedings of Experimental Biology 2017 Chicago
-------------------------------------
Une constatation qui ne devrait pas surprendre ceux qui s'intéressent à la médecine de plongée et au réflexe d'immersion (1, 2, 3, 4), dont le facteur principal de déclenchement est l'exposition de la face à de l'eau froide.
-------------------------------------
Introduction
Blood loss causes central hypovolemia and in severe instances, it can decrease blood pressure and lead to cardiovascular decompensation. Simple and quick interventions that can be used to prevent cardiovascular decompensation in pre-hospital settings could be a valuable tool for first responsders. Cooling the forehead and cheeks using an ice/water slurry mixture has been shown to increase blood pressure for over 15 minutes. Therefore, face cooling could be used to mitigate decreases in blood pressure during blood loss.
Purpose
We tested the hypothesis that face cooling during simulated blood loss will increase blood pressure. Methods Ten healthy participants (22 ± 2 years, 3 women) completed two randomized trials on separate days. Both trials began with 30 mmHg of lower body negative pressure (LBNP) to simulate blood loss for 6 minutes. Then, either a 2.5 L plastic bag of an ice/water slurry mixture (0 ± 0°C) (LBNP+FC) or a 2.5 L plastic bag of thermoneutral water (34 ± 1°C) (LBNP+SHAM) was placed on the forehead and eyes and 30 mmHg of LBNP was maintained for an additional 15 minutes.

We continuously measured blood pressure (Penaz method), heart rate (ECG), stroke volume (Modelflow), cardiac output, total peripheral resistance, and forehead temperature throughout the protocol.
Results
Forehead temperature did not change from LBNP (34.2 ± 0.6°C) to LBNP+SHAM (33.9 ± 1.4°C, P > 0.999) and decreased from LBNP (34.4 ± 0.5°C) to LBNP+FC (11.0 ± 1.6°C, P < 0.001). Mean arterial pressure did not change from LBNP (82 ± 10 mmHg) to LBNP+SHAM (80 ± 8 mmHg, P = 0.978), but markedly increased during LBNP+FC. The peak increase from LBNP (77 ± 9 mmHg) was observed after 3 minutes of LBNP+FC (98 ± 15 mmHg, P < 0.001). Heart rate during LBNP (76 ± 14 bpm, P = 0.978) was not different from LBNP+SHAM (75 ± 13 bpm). Heart rate was lower throughout LBNP+FC beginning at 2 minutes of FC (60 ± 16 bpm) versus LBNP (80 ± 19 bpm, P < 0.001). Stroke volume did not change from LBNP (72 ± 15 mL) to LBNP+SHAM (67 ± 18 mL, P = 0.857). However, stroke volume increased from LBNP (78 ± 16 mL) to LBNP+FC, and peaked after 5 minutes of FC (97 ± 32 mL, P < 0.001). Cardiac output did not change from LBNP (5.4 ± 1.0 L/min) to LBNP+SHAM (4.9 ± 1.0 L/min, P > 0.415). Cardiac output slightly decreased from LBNP (6.2 ± 1.5 L/min) to 2 minutes of LBNP+FC (5.3 ± 1.6 L/min, P = 0.038). Total peripheral resistance did not change from LBNP (15.6 ± 3.7 mmHg/L/min) to LBNP+SHAM (17.3 ± 3.2 mmHg/L/min, P = 0.613). Total peripheral resistance throughout LBNP+FC was greater than LBNP. The peak increase in total peripheral resistance was observed after 2 minutes of LBNP+FC (20.0 ± 6.2 mmHg/L/min) versus LBNP (13.2 ± 3.9 mmHg/L/min, P < 0.001).
Conclusions
Face cooling during simulated moderate blood loss increases blood pressure through an increase in total peripheral resistance. Although more research is warranted, face cooling during blood loss is a potential simple and quick intervention that could delay cardiovascular decompensation. Support or Funding InformationUniversity at Buffalo IMPACT Award
| Tags : choc, hémorragie
System to achieve ZERO preventable deaths
10/03/2017
Sauvetage au combat à la mer: Quid ?
Multi-Injury Casualty Stream Simulation in a Shipboard Combat Environment
-------------------------
L'attention portée à la prise en charge des blessés de guerre se porte essentiellement aux blessés lors de combat se déroulant au sol. Il ne faut pas oublier aussi ce qui se passe sur (voire sous) la surface de la mer. Ce qui est vrai à terre ne l'est probablement pas à la mer. Le trauma des membres est certainement moins prééminent. Les mécanismes ballistiques, l'environnement de prise en charge sont totalement différents aussi les réponses, c'est à dire la manière de conduire le sauvetage au combat, le sont également. Cependant la rareté des engagements sur mer rend difficile la mise sur pied d'une conduite basée sur les faits, d'où l'intérêt des outils de simulation statistique. C'est ce que propose cet article.
-------------------------
| Trauma Category | AIREX(%) | UNDEX(%) |
| Amputations (a) | 3.00 | 3.00 |
| Asphyxiations | 1.34 | 3.50 |
| Burns | 25.30 | 15.09 |
| Concussions/Internal Organs | 2.85 | 9.29 |
| Contusions/Abrasions | 7.06 | 16.28 |
| Fractures | 6.70 | 11.52 |
| Miscellaneous | 4.96 | 12.08 |
| Nonfatal Immersions | 2.00 | 2.00 |
| Penetrating Wounds | 44.88 | 20.49 |
| Sprains/Strains/Dislocations | 1.91 | 6.75 |
| Total | 100.00 | 100.00 |
| Tags : naval
06/03/2017
PTSD: Les soignants aussi
PTSD in those who care for the injured
Luftman K. et Al. Injury, Int. J. Care Injured 48 (2017) 293–296
-------------------------------------
PTSD, les soignants aussi. Cela peut paraître évident mais ce qui interpelle, c'est l'importance du phénomène.
---------------------------------------
Background: Post Traumatic Stress Disorder (PTSD) has become a focus for the care of trauma victims, but the incidence of PTSD in those who care for injured patients has not been well studied. Our hypothesis was that a significant proportion of health care providers involved with trauma care are at risk of developing PTSD.
Methods: A system-wide survey was applied using a modified version of the Primary Care PTSD Screen [PC-PTSD], a validated PTSD screening tool currently being used by the VA to screen veterans for PTSD. Pre-hospital and in-hospital care providers including paramedics, nurses, trauma surgeons, emergency medicine physicians, and residents were invited to participate in the survey. The survey questionnaire was anonymously and voluntarily performed online using the Qualtrix system. Providers screened positive if they affirmatively answered any three or more of the four screening questions and negative if they answered less than three questions with a positive answer. Respondents were grouped by age, gender, region, and profession.
Results: 546 providers answered all of the survey questions. The screening was positive in 180 (33%) and negative in 366 (67%) of the responders. There were no differences observed in screen positivity for gender, region, or age. Pre-hospital providers were significantly more likely to screen positive for PTSD compared to the in-hospital providers (42% vs. 21%, P < 0.001). Only 55% of respondents had ever received any information or education about PTSD and only 13% of respondents ever sought treatment for PTSD.
Conclusion: The results of this survey are alarming, with high proportions of healthcare workers at risk for PTSD across all professional groups. PTSD is a vastly underreported entity in those who care for the injured and could potentially represent a major problem for both pre-hospital and in-hospital providers. A larger, national study is warranted to verify these regional results
| Tags : ptsd
Réduire une épaule luxée: Le choix !
A systematic and technical guide on how to reduce a shoulder dislocation
Alkaduhimi, et Al. Turk J Emerg Med. 2016 Dec; 16(4): 155–168.
Objectives
Our objective is to provide a systematic and technical guide on how to reduce a shoulder dislocation, based on techniques that have been described in literature for patients with anterior and posterior shoulder instability.
Materials and methods
A PubMed and EMBASE query was performed, screening all relevant literature on the closed reduction techniques. Studies regarding open reduction techniques and studies with fracture dislocations were excluded.
Results
In this study we give an overview of 23 different techniques for closed reduction and 17 modifications of these techniques.
Discussion
In this review article we present a complete overview of the techniques, that have been described in the literature for closed reduction for shoulder dislocations. This manuscript can be regarded as a clinical guide how to perform a closed reduction maneuver, including several technical tips and tricks to optimize the success rate and to avoid complications.
Conclusion
There are 23 different reduction techniques with 17 modifications of these techniques. Knowledge of the different techniques is highly important for a good reduction.
Trauma center: Niveau 1 ou 2 ?
Patient Outcomes at Urban and Suburban Level I Versus Level II Trauma Centers.
Il est admis que la prise en charge des traumatisés dans des structures optimisées comme les trauma center de niveau 1 améliore la survie. Il semblerait que ceci mérite encore d'être encore discuté tout particulièrement en zone urbaine ou sub-urbaine et quand les équipes chirurgicales des TC de niveau 2 ont reçu une formation adaptée. Bien équipé ne signifie pas performance, les auteurs mettent en avant la qualité des équipes opérant dans le centre avant la disponibilité d'équipement spécialisé ne correspondant pas forcément aux besoins quotidiens.
-------------------------
STUDY OBJECTIVE:
Regionalized systems of trauma care and level verification are promulgated by the American College of Surgeons. Whether patient outcomes differ between the 2 highest verifications, Levels I and II, is unknown. In contrast to Level IIcenters, Level I centers are required to care for a minimum number of severely injured patients, have immediate availability of subspecialty services and equipment, and demonstrate research, substance abuse screening, and injury prevention. We compare risk-adjusted mortality outcomes at Levels I and II centers.
METHODS:
This was an analysis of data from the 2012 to 2014 Los Angeles County Trauma and Emergency Medical Information System. The system includes 14 trauma centers: 5 Level I and 9 Level II centers. Patients meeting criteria for transport to a trauma center are routed to the closest center, regardless of verification level. All adult patients (≥15 years) treated at any of the traumacenters were included. Outcomes of patients treated at Level I versus Level II centers were compared with 2 validated risk-adjusted models: Trauma Score-Injury Severity Score (TRISS) and the Haider model.
RESULTS:
Adult subjects (33,890) were treated at a Level I center; 29,724, at a Level II center. We found lower overall mortality at Level II centers compared with Level I, using TRISS (odds ratio 0.68; 95% confidence interval 0.59 to 0.78) and Haider (odds ratio 0.84; 95% confidence interval 0.73 to 0.97).
CONCLUSION:
In this cohort of patients treated at urban and suburban trauma centers, treatment at a Level II trauma center was associated with overall risk-adjusted reduced mortality relative to that at a Level I center. In the subset of penetrating trauma, no differences in mortality were found. Further study is warranted to determine optimal trauma system configuration and allocation of resources.
17/02/2017
Visualisation mentale: Mieux que l'ATLS
Lorello GR et Al CJEM. 2016 Mar;18(2):136-42. doi: 10.1017/cem.2015.4. Epub 2015 Apr 10.
--------------------------------
l'ATLS (Advanced trauma life support) est souvent présenté comme la panacée en matière de prise en charge du traumatisé. Il n'est pas inintéressant d'avoir une analyse très critique de ce type de formation dont le but originel était d'apporter, en 2 jours et demi, des connaissances de base à des équipes peu formées à la pris en charge de traumatisés sévères. Aussi doit on considérer qu'elle a été d'un apport fondamental dans les pays ne disposant pas de réseaux avancés. Si le contenu structuré et le recours à des ateliers pratiques apparaît attrayant , le contenu médical est régulièrement non conforme aux bonnes pratiques et les enseignants souvent non experts du sujet (1, 2). Il a pu être proposé de traduire l'acronyme ATLS par "Archaic Trauma Life Support"(3). Le travail proposé confirme bien les limites de cette formation qui ne parait plus adapté au contexte actuel pour des professionnels de l'affaire (4). Quand on s'adresse à des étudiants avancés dans leur cursus de formation, la préparation d'un exercice de simulation en équipe par l'imagerie mentale est plus efficace.
L'ATLS demeure néanmoins un bon moyen d'appréhender pour les novices les bases fondamentales de la prise en charge des traumatisés. Ce n'est pas le seul et il existe d'autres approches notamment le DIU de traumatisés sévères (5) ou l'European Trauma Course (6), dernier donnant un grande place à la simulation.
INTRODUCTION:
Effective trauma resuscitation requires the coordinated efforts of an interdisciplinary team. Mental practice (MP) is defined as the mental rehearsal of activity in the absence of gross muscular movements and has been demonstrated to enhance acquiring technical and procedural skills. The role of MP to promote nontechnical, team-based skills for trauma has yet to be investigated.
METHODS:
We randomized anaesthesiology, emergency medicine, and surgery residents to two-member teams randomly assigned to either an MP or control group. The MP group engaged in 20 minutes of MP, and the control group received 20 minutes of Advanced Trauma Life Support (ATLS) training. All teams then participated in a high-fidelity simulated adult trauma resuscitation and received debriefing on communication, leadership, and teamwork. Two blinded raters independently scored video recordings of the simulated resuscitations using the Mayo High Performance Teamwork Scale (MHPTS), a validated team-based behavioural rating scale. The Mann-Whitney U-test was used to assess for between-group differences.
RESULTS:
Seventy-eight residents provided informed written consent and were recruited. The MP group outperformed the control group with significant effect on teamwork behaviour as assessed using the MHPTS: r=0.67, p<0.01.
CONCLUSIONS:
MP leads to improvement in team-based skills compared to traditional simulation-based trauma instruction. We feel that MP may be a useful and inexpensive tool for improving nontechnical skills instruction effectiveness for team-based trauma care.
| Tags : top
01/02/2017
Echo: Pour le thorax surtout
Traumatic cardiac injury: Experience from a level-1 trauma centre
Mishra B. et Al. Chin J Traumatol. 2016 Dec 1;19(6):333-336.
--------------------------------------
Disposer d'un appareil d'échographie est d'un grand intérêt. Encore faut-il maîtriser cette technique (1) sous peine de se tromper dans les priorités de prise en charge. Le recours a cette technique reste débattu pour la prise en charge de traumatismes pénétrants. L'échographie thoracique est probablement à valeur ajoutée tant sur l'imagerie pleurale que péricardique. C'est ce que présente ce travail. Ce document rapporte également l'inefficacité en terme de survie de péricardocentèse pourtant prôné par l'ATLS.
--------------------------------------
Traumatic cardiac injury (TCI) is a challenge for trauma surgeons as it provides a short thera- peutic window and the management is often dictated by the underlying mechanism and hemodynamic status. The current study is to evaluate the factors influencing the outcome of TCI.
METHODS:
Prospectively maintained database of TCI cases admitted at a Level-1 trauma center from July 2008 to June 2013 was retrospectively analyzed. Hospital records were reviewed and statistical analysis was performed using the SPSS version 15.
RESULTS:
Out of 21 cases of TCI, 6 (28.6%) had isolated and 15 (71.4%) had associated injuries. Ratio be- tween blunt and penetrating injuries was 2:1 with male preponderance. Mean ISS was 31.95. Thirteen patients (62%) presented with features suggestive of shock. Cardiac tamponade was present in 12 (57%) cases and pericardiocentesis was done in only 6 cases of them. Overall 19 patients underwent surgery. Perioperatively 8 (38.1%) patients developed cardiac arrest and 7 developed cardiac arrhythmia. Overall survival rate was 71.4%. Mortality was related to cardiac arrest (p = 0.014), arrhythmia (p = 0.014), and hemorrhagic shock (p =0.04). The diagnostic accuracy of focused assessment by sonography in trauma (FAST) was 95.24%.
CONCLUSION:
High index of clinical suspicion based on the mechanism of injury, meticulous examination by FAST and early intervention could improve the overall outcome.