24/11/2013
Garrot abdominal: Une paire de main et des bras musclés
Temporization of Penetrating Abdominal-Pelvic Trauma With Manual External Aortic Compression: A Novel Case Report
Douma M et Al. Ann Emerg Med. 2013 Oct 23. pii: S0196-0644(13)01452-2
La prise en charge des traumatismes vasculaires de l'abdomen, du pelvis et des membres nécessite une intervention chirurgicale rapide. Il est dans ces cas nécessaire de tarir sinon de réduire le débit de saignement de telle sorte que le blessé arrive vivant dans la structure adaptée (1). Ceci est difficile quand les lésions ne sont pas ou difficilement garrotables notamment lors de traumatismes jonctionnels. Des équipements spécifiques ont été développé pour assurer une compression en amont des lésions et permettre de réduire ces débits de saignements. Ces dispositifs présenté par ailleurs (2, 3 , 4) n'ont pas encore fait leur preuve même si des rapports isolés en soulignent l'intérêt. Certains comme les pantalons antichocs sont considérés comme ayant peu d'indications du moins mal cernées (5) . Ces équipements sont rarement disponibles.
Pourtant la compression abdominale bi-manuelle est possible et en fait connue depuis longtemps notamment en obstétrique sous forme de compression utérine bi-manuelle (6, 7, 8).
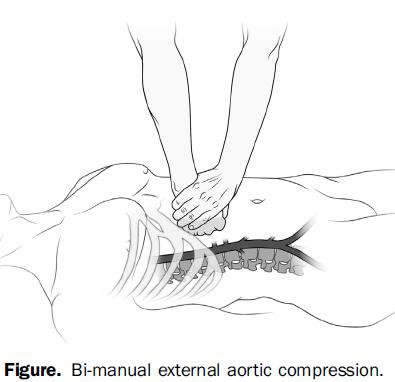
C'est ce qu'illustre le cas clinique présenté. Il existe bien sûr des facteurs limitant comme la corpulence aussi bien du blessé que du sauveteur. Il faut en effet exercer une pression abdominale de l'ordre de 40 kg pour occlure l'aorte abdominal (9).
| Tags : hémorragie, garrot
05/11/2013
Pansement hémostatique: Utile?
Comparison of ChitoFlex®, CELOX™, and QuikClot® in control of hemorrhage
Devlin JJ et all. J Emerg Med. 2011 Sep;41(3):237-45
Un article qui complète le précédent et qui doit appeler à de la mesure sur l'emploi des pansements hémostatiques. Bien qu'il existe de nombreux travaux comparatifs prônant l'intérêt de tel ou tel dispositifs, le bien fondé de leur emploi extensif ne peut toujours pas être affirmé en condition de combat. Les messages pédagogiques doivent donc avant tout porter sur l'application correcte des pansements compressifs et le packing de plaie.
------------------------------------
BACKGROUND:
Exsanguinating extremity wounds remain the primary source of battlefield mortality. Operating forces employ three agents in Iraq: HemCon® (HemCon Medical Technologies, Inc., Portland, OR), QuikClot® (Z-Medica Corporation, Wallingford, CT), and CELOX™ (SAM Medical, Tualatin, OR). Anecdotal reports suggest that these agents are less useful on small entrance, linear-tract injuries. ChitoFlex® (HemCon Medical Technologies, Inc., Portland, OR) has been introduced but is untested.
STUDY OBJECTIVES:
To compare the equivalency of the ChitoFlex® dressing, QuikClot® ACS+™ dressing, CELOX™, and standard gauze in their effectiveness to control bleeding from non-cavitary groin wounds.
METHODS:
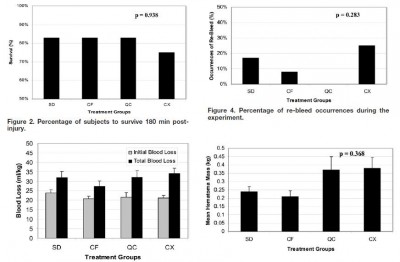
Forty-eight swine were randomly assigned to one of four treatment groups: standard gauze dressing (SD), ChitoFlex® dressing (CF), QuikClot® ACS+™ dressing (QC), and CELOX™ dressing (CX). A groin injury with limited vessel access was created in each animal. Subjects were resuscitated with 500 mL of hetastarch. The primary endpoint was 180-min survival. Secondary endpoints included total blood loss in mL/kg, incidence of re-bleeding, survival times among the animals that did not survive for 180 min, failure to achieve initial hemostasis, incidence of recurrent bleeding, time to initial re-bleeding, amount of re-bleeding, and mass of residual hematoma.
RESULTS:
Survival occurred in 10 of 12 SD animals, 10 of 12 CF animals, 10 of 12 QC animals, and 9 of 12 CX animals. No statistically significant difference was found.
CONCLUSION:
In our study of limited-access extremity bleeding, ChitoFlex® performed equally well in mitigating blood loss and promoting survival. The ChitoFlex® dressing is an equally effective alternative to currently available hemostatic agents. However, no agents were superior to standard gauze in our model of limited access.
| Tags : pansement
22/09/2013
Pansement hémostatique:Vraiment utile ?
Watters J et all. J Trauma. 2011;70:1413–1419
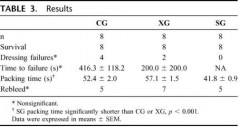
Un travail intéressant qui s'interroge sur le vrai intérêt des pansements hémostatiques. Sans remettre en question ce dernier cet article remet en question le positionnement de ce type de matériel. Dans un travail expérimental sur un modèle animal, un packing de plaie avec de la gaze simple serait plus rapide et tout aussi efficace qu'un packing effectué avec le Combat gauze ou le celox gauze.
-----------------------------------------------------------------
Results: All animals survived to study end. There were no differences in baseline physiologic or coagulation parameters or in dressing success rate (SG: 8/8, CG: 4/8, XG: 6/8) or blood loss between groups (SG: 260 mL, CG: 374 mL, XG: 204 mL; p > 0.3). SG (40 seconds ± 0.9 seconds) packed significantly faster than either the CG (52 ± 2.0) or XG (59 ± 1.9). At 120 minutes, all groups had a significantly shorter time to clot formation compared with baseline (p < 0.01). At 30 minutes, the XG animals had shorter time to clot compared with SG and CG animals (p < 0.05). All histology sections had mild intimal and medial edema. No inflammation, necrosis, or deposition of dressing particles in vessel walls was observed. No histologic or ultrastructural differences were found between the study dressings.
-----------------------------------------------------------------
"There are reasons that standard woven gauze bandages have existed for millennia. They are lightweight, absorbent, highly conformable, stable in a variety of environmental conditions, and inexpensive. Multiple advanced hemostatic agents have resulted in superior homeostasis, improved outcomes, and likely saved lives compared with SG when applied according to manufacturers’ recommendations for compression time. However, in a care under fire scenario or in a situation of mass casualties, compression times of 2 minutes to 5 minutes are not feasible. During ongoing battle, only lifethreatening injuries should be addressed and often the wounded must self-apply a tourniquet or dressing. An individual rendering self or buddy aid will need to continue to engage in battle as the first priority. Major vascular injuries, which cannot be controlled through application of a tourniquet, must be addressed as quickly as possible before profound bleeding incapacitates the casualty. Similarly, when there are persons with multiple injuries or wounds to treat, dressings must be rapidly placed and effective without prolonged hold times"
Conclusion: Ce qui compte c'est la compression et le packing de plaie
| Tags : pansement
08/09/2013
Stabilisation pelvienne: Vraiment utile !
Emergency stabilization of the pelvic ring: Clinical comparison between three different techniques
Pizanis A. et All. Injury. 2013 Aug 2. pii: S0020-1383(13)00316-1.
Background: Emergency devices for pelvic ring stabilization include circumferential sheets, pelvic binders, and c-clamps. Our knowledge ofthe outcome ofthese techniques is currently based on limited information.
Methods: Using the dataset of the German Pelvic Trauma Registry, demographic and injury-associated characteristics as well as the outcome of pelvic fracture patients after sheet, binder, and c-clamp treatment was compared. Outcome parameters included transfusion requirement of packed red blood cells, length of hospital stay, mortality, and incidence of lethal pelvic bleeding.
Results: Two hundred seven of 6137 (3.4%) patients documented in the German Pelvic Trauma Registry between April 30th 2004 and January 19th 2012 were treated by sheets, binders, or c-clamps. In most cases, c-clamps (69%) were used, followed by sheets (16%), and binders (15%). The median age was significantly lower in patients treated with binders than in patients treated with sheets or c-clamps (26 vs. 47 vs. 42 years, p = 0.01). Sheet wrapping was associated with a significantly higher incidence of lethal pelvic bleeding compared to binder or c-clamp stabilization (23% vs. 4% vs. 8%). No significant differences between the study groups were found in sex, fracture type, blood haemoglobin concentration, arterial blood pressure, Injury Severity Score, the incidence of additional pelvic packing and arterial embolization, need of red blood cell transfusion, length of hospitalisation, and mortality.
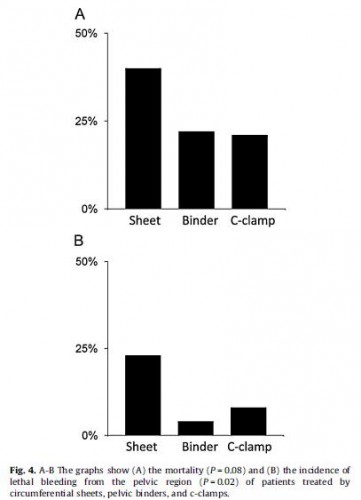
Conclusions: The data suggest that emergency stabilization ofthe pelvic ring by binders and c-clamps is associated with a lower incidence of lethal pelvic bleeding compared to sheet wrapping.
| Tags : pelvis
06/09/2013
Tourniquet abdominal: Compression axillaire ?
| Tags : tourniquet, hémorragie, jonctionnel
07/08/2013
Plasma: En préhospitalier AUSSI +++
Point-of-injury use of reconstituted freeze dried plasma as a resuscitative fluid: A special report for prehospital trauma care
Glassberg E. et All. J J Trauma Acute Care Surg. 2013;75(Suppl 2):S111YS111.
La prise en charge d'hémorrragie catastrophique en phase préhospitalière est particulièrement complexe. Ces dernières années la mise en place d'un réseau structuré de prise en charge, 'application de procédures spécifiques visant à arrêter les hémorragies au plus tôt, le recours à l'acide tranexaminique, la prévention des hypothermies et l'application d'une politique raisonnée de rénaimation/chirurgie ont constitué une grande avancée. Certaines nations ont équipé leurs vecteurs d'évacuations de concentrés érythrocytaires. Le maintien d'une coagulation optimale est un enjeu majeur. Pour cela existe, entre autres, le plasma lyophilisé. Les forces armées israéliennes militent pour l'emploi de ce type de solutions en phase préhospitalière
| Tags : coagulopathie, hémorragie
22/07/2013
Tourniquet: Serrer fort et surtout vérifier l'efficacité
Forward Assessment of 79 Prehospital Battlefield Tourniquets Used in the Current War
King DR et All. J Spec Oper Med. 2012 Winter;12(4):33-8.
Un article important qui doit faire réfléchir à la manière dont l'instruction sur le garrot est conduite aussi bien au niveau du SC1 que du SC 2.
Dans ce document il est expliqué que 79 garrots sont posés sur 65 jambes garrotées de 54 combattants. Seules 17 jambes avaient des lésions artérielles. 14 d'entre elles étaient majueres mais seules 4 avait un garrot sérré correctement c'est à dire avec abolition du pouls distal. mais qu'aucune lésion artérielle n'a été prise en charge sans garrot sur la même période. Un rappel simple est fait sen outre sur l'importance de la largeur du garrot.
________________________________________________
Introduction: Battlefield tourniquet use can be lifesaving, but most reports are from hospitals with knowledge gaps remaining at the forward surgical team (FST). The quality of tourniquet applications in forward settings remain unknown. The purpose of this case series is to describe observations oftourniquet use at an FST in order to improve clinical performance.
Methods: War casualties with tourniquet use presenting to an FST in Afghanistan in 2011 were observed. We identified appliers by training, device effectiveness, injury pattern, and clinical opportunities for improvement. Feedback was given to treating medics. Results: Tourniquet applications (79) were performed by special operations combat medics (47, 59%), flight medics (17, 22%), combat medics (12, 15%), and general surgeons (3, 4%). Most tourniquets were Combat Application Tourniquets (71/79, 90%). With tourniquets in place upon arrival at the FST, most limbs (83%, 54/65) had palpable distal pulses present; 17% were pulseless (11/65). Of all tourniquets, the use was venous in 83% and arterial in 17%. In total, there were 14 arterial injuries, but only 5 had effective arterial tourniquetsapplied.
Discussion: Tourniquets are liberally applied to extremity injuries on the battlefield. 17% were arterial and 83% were venous tourniquets. When ongoing bleeding or distal pulses were appreciated, medics tightened tourniquets under surgeon supervision until distal pulses stopped. Medics were generally surprised at how tight a tourniquet must be to stop arterial flow ? convert a venous tourniquet into an arterial tourniquet. Implications for sustainment training should be considered with regard to this life-saving skill.
________________________________________________
1. Les garrots doivent être serrés de manière conforme; arrêt du saignement et dès que possible contrôle de l'absence de pouls.
2. Les garrots doivent être surveillés tout au long de la chaine de prise en charge
3. La fiche mémento sur le concept de garrot tactique est à lire et relire
| Tags : tourniquet, garrot
16/07/2013
Management of bleeding and coagulopathy following major trauma: an updated European guideline
| Tags : hémorragie, traumatologie
06/07/2013
Sonde de foley: Au moins 2 et pas pour un sondage
Improved mortality from penetrating neck and maxillofacial trauma using Foley catheter balloon tamponade in combat
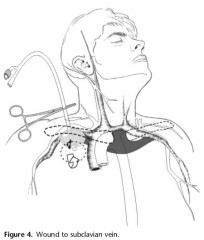
Weppner J. J Trauma Acute Care Surg. 2013;75: 00Y00
BACKGROUND:
The military medical community has promoted use of Foley catheter balloon tamponade in the initial management of vascular injury owing to neck or maxillofacial trauma. The aim of the study was to compare outcomes with Foley catheter tamponade with those obtained with traditional use of external pressure.
METHODS:
This retrospective cohort study evaluated all cases of persistent bleeding caused by penetrating neck or maxillofacial trauma received at one forward aid station between December 2009 and October 2011. Cohorts included those who were treated with Foley catheter tamponade and those managed with external pressure. Which treatment option was applied depended solely on the availability of Foley catheters at the time. The effectiveness of each technique in controlling initial and delayed hemorrhage is described, and the impact on mortality is analyzed using the Student’s t test and Fisher’s exact test.
RESULTS:
Seventy-seven subjects met the inclusion criteria with 42 subjects in the Foley group and 35 subjects in the external pressure group. A statistically significant difference was found between the groups regarding delayed failure, experienced by three patients (7%) in the Foley group and nine patients (26%) in the external pressure group ( p G 0.05). The difference in mortality, 5% (two patients) in the Foley tamponade group and 23% (eight patients) in the external pressure group, was statistically significant ( p G 0.05).
CONCLUSION:
For penetrating neck and maxillofacial injuries in a combat environment, Foley catheter balloon tamponade significantly reduced mortality when compared with direct pressure techniques through its effect on preventing delayed bleeding.
--------------------------------------------------------------------
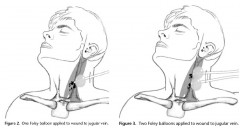 The Foley catheter tamponade is relatively simple and very easy to perform rapidly. Before its insertion in the cases examined in this study, a hemorrhaging wound was identified in the neck ormaxillofacial area, and a hemostat was applied to the distal endof an 18 Fr Foley catheter (30 cm3). The catheter was then introduced with a finger into the wound and directed along the wound track to the estimated or palpated source of bleeding, after which the Foley balloon was inflated with sterile water until the bleeding stopped or moderate resistance felt. If this technique did not stop the hemorrhage and either a deep wound or large defect was present in the bleeding vessel, it was considered that the balloon may have only been able to provide distal control. In such cases, a second catheter was introduced into the wound and inflated to provide more proximal control.
The Foley catheter tamponade is relatively simple and very easy to perform rapidly. Before its insertion in the cases examined in this study, a hemorrhaging wound was identified in the neck ormaxillofacial area, and a hemostat was applied to the distal endof an 18 Fr Foley catheter (30 cm3). The catheter was then introduced with a finger into the wound and directed along the wound track to the estimated or palpated source of bleeding, after which the Foley balloon was inflated with sterile water until the bleeding stopped or moderate resistance felt. If this technique did not stop the hemorrhage and either a deep wound or large defect was present in the bleeding vessel, it was considered that the balloon may have only been able to provide distal control. In such cases, a second catheter was introduced into the wound and inflated to provide more proximal control.
When treating Zone I injuries of the supraclavicular fossa, the catheter was introduced as far as possible past the defect in the vessel, allowing the balloon to be inflated before being pulled back firmly and then held in place with a hemostat. Doing so compressed the injured vessel onto the first rib and clavicle, which was intended to tamponade bleeding into the chest. If external hemorrhage continued following insertion of the Foley catheter, a second catheter may have been inserted to control bleeding
05/07/2013
Garrot: Une nouvelle ère ?
New Tourniquet Device Concepts for Battlefield Hemorrhage Control
Kragh JF et all.US Army Med Dep J. 2011 Apr-Jun:38-48.
Ground:
Given the recent success of emergency tourniquets, limb exsanguination is no longer the most common cause of preventable death on the battlefield; hemorrhage amenable to truncal tourniquets now is. The purpose of the present study is to discuss the gaps today in battlefield hemorrhage control and candidate solutions in order to stimulate the advancement of prehospital combat casualty care.
Methods:
A literature review, a market survey of candidate devices, a request for devices, and an analysis of the current situation regarding battlefield hemorrhage control were performed.
Results:
Hemorrhage control for wounds in the junction between the trunk and the limbs and neck is a care gap in the current war, and, of these, the pelvic (including buttock and groin proximal to the inguinal ligament) area is the most common. Historical and recent reports give background information indicating that truncal tourniquets are plausible devices for controlling junctional hemorrhage on the battlefield. A request for candidate devices yielded few prototypes, only one of which was approved by the US Food and Drug Administration.
Conclusions:
In order to solve the now most common cause of preventable death on the battlefield, junctional hemorrhage from the pelvic area, the planned approach is a systematic review of research, device and model development, and the fielding of a good device with appropriate training and doctrine.
| Tags : jonctionnel, tourniquet
04/07/2013
Hémostase: L'émergence des nanoparticules ?
Nano hemostat solution: immediate hemostasis at the nanoscale
Ellis-Behnke RG et all. Nanomedicine: Nanotechnology, Biology, and Medicine 2 (2006) 207 – 215
--------------------------------------------------------------------------------------
Hemostasis is a major problem in surgical procedures and after major trauma. There are few effective methods to stop bleeding without causing secondary damage. We used a self-assembling peptide that establishes a nanofiber barrier to achieve complete hemostasis immediately when applied directly to a wound in the brain, spinal cord, femoral artery, liver, or skin of mammals. This novel therapy stops bleeding without the use of pressure, cauterization, vasoconstriction, coagulation, or cross-linked adhesives. The self-assembling solution is nontoxic and nonimmunogenic, and the breakdown products are amino acids, which are tissue building blocks that can be used to repair the site of injury. Here we report the first use of nanotechnology to achieve complete hemostasis in less than 15 seconds, hich could fundamentally change how much blood is needed during surgery of the future.
--------------------------------------------------------------------------------------
Dans ce modèle une hémostase obtenue en moins de 15 secondes par un mécanisme peu évident:
1. ["First, we know that the hemostasis is not explainable by clotting. Blood clots are produced after injury, but do not begin to form until 1 to 2 minutes have elapsed, depending upon the status and coagulation history of the patient"]
2. ["the electron micrographs show no evidence of platelet aggregation at the interface of the material and wound site"]
3. ["We believe this tight contact is crucial to the hemostatic action because of the size of the self-assembling peptide units."]
| Tags : hémorragie
02/07/2013
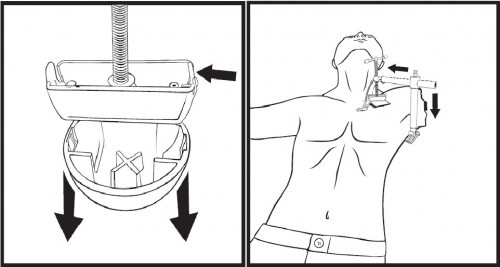
Croc axillaire:En théorie, c'est possible
Technique of axillary use of a Combat Ready Clamp to stop junctional bleeding
Kragh JF et All. http://dx.doi.org/10.1016/j.ajem.2013.02.027
Bien que le Croc ne soit validé que les plaies de l'aine, son emploi au membre supérieur est possible.
Enlever la cupule et appliquer la barre de compression parallèle à la clavicule. Le serrage compotre en moyenne 5 tours.
| Tags : hémorragie
29/06/2013
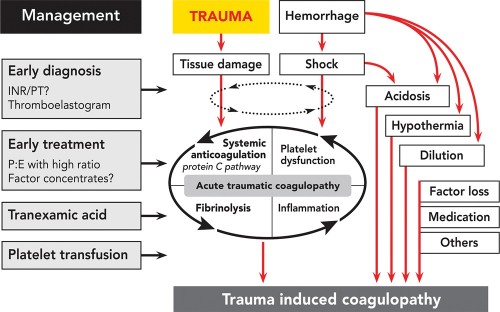
Coagulopathie du trauma: Que faire ?
Case Scenario: Management of Trauma-induced Coagulopathy in a Severe Blunt Trauma Patient
David JS et All. Anesthesiology 2013; 119:191–200
Un point très clair du problème
| Tags : coagulopathie
03/06/2013
Garrots: Sur soi mais pas n'importe comment !
Efficacy of tourniquets exposed to the afghanistan combat environment stored in individual first aid kits versus on the exterior of plate carriers
Weppner J et all. Mil Med. 2013 Mar;178(3):334-7
Between February and May 2010, 1st Battalion, 6th Marines reported a 10% (10/92) breakage rate for tourniquets. One theory suggested was that tourniquets were weakened by exposure to the Afghan environment. Our study was designed to compare three groups of Afghanistan-exposed tourniquets to unexposed tourniquets. The three experimental arms were: (1) Afghan-exposed tourniquets worn on the plate carrier, (2) Afghan-exposed tourniquets carried in the Individual First Aid Kit (IFAK) and wrapped in manufacturer plastic wrapping, and (3) Afghan-exposed tourniquets carried in the IFAK with the manufacturer plastic wrapping removed. The outcome measures of this study were efficacy, breakage, and number of turns required to successfully stop the distal pulse. Tourniquets worn on the plate carrier had an efficacy of 57%, which was significantly lower than the control efficacy rate of 95.2%. When compared to the control arm, there were no significant differences in efficacy between the tourniquets stored in the IFAK with or without manufacturing packaging. No control tourniquets or tourniquets stored in IFAKs broke; however, 46 (12%) of the plate carrier-exposed tourniquets did break. No statistically significant differences were found between the four groups with regard to the median number of turns required to stop the distal pulse.
| Tags : tourniquet
02/06/2013
Hémorragies jonctionnelles: Comprimer le pelvis
UK Combat-Related Pelvic Junctional Vascular Injuries 2008-2011: Implications for Future Intervention.
Walker NM et All. - Bone Joint Journal (2013) vol. 95-B no. SUPP 8 13
---------------------------------------------------------------------------------------
L'arrêt d'une hémorragie jonctionnelle est un enjeu majeur. Plusieurs dispositifs ont été récemment proposés. Il semble que la grande majorité des lésions observées se situent au dessus du ligament inguinal rendant ainsi l'efficacité de dispositif comme le CRoC limité. Le tourniquet abdominal ou le sam junctionnal tourniquet paraissent ainsi au moins théoriquement un meilleur choix si toutefois ils permettent une compression suffisante.
---------------------------------------------------------------------------------------
In a recent publication, 4.6% of 6450 Coalition deaths over ten years were reported to be due to junctional bleeding. The authors suggested that some of these deaths could have been avoided with a junctional hemorrhage control device.
Prospectively collected data on all injuries sustained in Afghanistan by UK military personnel over a 2 year period were reviewed. All fatalities with significant pelvic injuries were identified and analysed, and the cause of death established.
Significant upper thigh, groin or pelvic injuries were recorded in 124 casualties, of which 92 died. Pelvic injury was the cause of death in 42; only 1 casualty was identified where death was at least in part due to a vascular injury below the inguinal ligament, not controlled by a tourniquet, representing <1% of all deaths. Twenty one deaths were due to vascular injury between the aortic bifurcation and the inguinal ligament, of which 4 survived to a medical facility.
Some potentially survivable deaths due to exsanguination may be amenable to more proximal vascular control. We cannot substantiate previous conclusions that this can be achieved through use of a groin junctional tourniquet. There may be a role for more proximal vascular control of pelvic bleeding.
| Tags : tourniquet, hémorragie, jonctionnel
26/05/2013
Plasma lyophilisé: Une réalité
Le Service de Santé des Armées a recours depuis de nombreuses années (1, 2) à une présentation originale de plasma thérapeutique le PLYO.
Initialement réservé à un emploi en opérations extérieures, il vient d'être validé sous contraintes pour un usage sur le territoire national: Le plasma lyophilisé (PLYO) est principalement distribué aux unités médico-chirurgicales militaires déployées en Opérations Extérieures (OPEX) pour répondre aux contraintes logistiques du contexte opérationnel et à la nécessité de disposer, sans délai, de plasma pour le traitement des blessés hémorragiques. En milieu civil, le PLYO pourrait être utilisé par les établissements de santé présentant des difficultés logistiques majeures ne permettant pas d’assurer une chaîne du froid négative ou au cours de situations d’extrême urgence avec nécessité d’un apport de plasma thérapeutique sans délai. Dans cette deuxième indication, le PLYO devrait être utilisé en attendant que le plasma frais congelé soit décongelé et disponible. Le plasma lyophilisé français (PLyo®) préparé préférentiellement à partir de plasma frais congelé traité par l’amotosalen. Il est obtenu par lyophilisation à partir d’un mélange de PFC-IA issus d’aphérèse, provenant de dix donneurs différents au maximum, de groupes sanguins A, B, et AB, exempts d’anticorps immuns anti-A ou anti-B, conservés à une température inférieure ou égale à −25 °C.
Il en existe d'autres. Le plasma lyophilisé sud-africain (Bioplasma®) est le seul équivalent au monde du plasma lyophilisé français du fait de son universalité. Il s’agit d’un produit sud-africain bénéficiant d’une autorisation nationale depuis 1994 et commercialisé depuis 1996. Ce plasma est lyophilisé, universel et traité par solvant-détergent. Il existe en deux formats de flacon : 50 ou 200 mL. Le plasma lyophilisé allemand (LyoPlas N-W®), produit par le service de transfusion sanguine de la croix rouge allemande, provient d’un seul donneur de sang total ou d’aphérèse. Il n’est donc pas universel au regard de la compatibilité ABO. Le produit est sécurisé par quarantaine de quatre mois. Il peut être stocké 15 mois entre +2 et +25 °C.
Une révue récente fait le point sur les divers plasma thérapeutiques disponibles.
| Tags : coagulopathie
20/04/2013
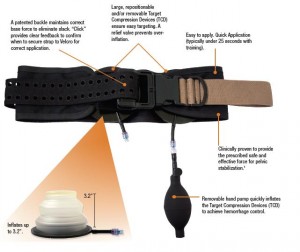
Hémorragie jonctionnelle: Un nouveau dispositif de compression
La prise en charge des hémorragies jonctionnelles est un des enjeux actuels de la chirurgie de guerre. Réaliser une compression artérielle fémorale peut être obtenu manuellement ou bien à l'aide de dispositifs mécaniques. L'utilisation du Combat Ready Clamp (CRoC) fait partie de la doctrine actuelle du TCCC américain. Un produit similaire est proposé: Le Junctionnal Emergency Treatment Tool (JETT). L'intérêt de ce type de dispositifs ne parait pas devoir être limité au préhospitalier. Ils sont en effet utilisés de manière courante à l'hôpital notamment pour comprimer les régions fémorales lors du retrait des dispositifs artériels fémoraux (femostop). Un troisième dispositif compressif vient compléter l'offre: Le SAM junctionnal tourniquet dont l'usage semble plus simple et qui offre surtout l'avantage de réaliser une stabilisation pelvienne. (voir ici sa validation sur cadavre)
Cependant malgré tout leur intérêt potentiel aucun de ces produits n'a été vraiment validé
| Tags : hémorragie, jonctionnel, garrot
23/03/2013
Tourniquet: Quel efficacité et avec quoi ?
Performance improvement in emergency tourniquet use during the Baghdad surge
Kragh JF et all. Am J Emerg Med 2013 Mar 4. pii: S0735-6757(12)00611-0.
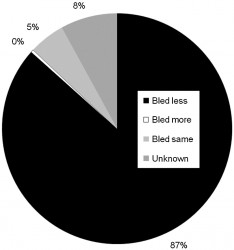
Cette lettre à l"éditeur rapporte l'étude comparée sur 3 périodes des conditions d'emploi et l'efficacité des garrrots pendant les combats s'étant déroulés pour le contrôle de la ville de Baghdad. 1252 garrots ont été posés chez 727 blessés sur 952 membres. L'emploi avant la structure chirurgicale est bien plus fréquente dans la dernière période avec un taux qui passe de 84% à 97% et un taux de survie de 86.6% à 90.8%.
La réponse initiale à la pose de ce garrot est dans 87% une réduction du saignement. Dans 5% des cas le saignement n'est pas modifié. Il est augmenté dans 0.3%. La réponse au garrot n'est pas documentée dans 8% des cas. Ce document confirme les précautions à prendre lors du déserrement de garrot rapportant une baisse de la pression artérielle d'au moins 30 mmHg chez 2% des blessés.
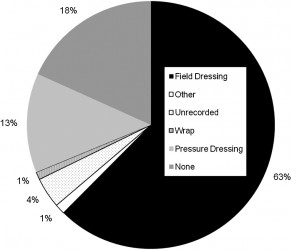
Par ailleurs l'emploi isolé d'un garrot ne s'observe que dans 18% des cas. Le plus souvent il est utilisé avec un pansement simple et dans 13% des cas avec un pansementcompressif et 1% un bandage compressif du membre.
En résumé le garrot doit être posé plus tôt et plus souvent permettant d'obtenir une meilleure survie.
| Tags : tourniquet
04/02/2013
Le CROC: Une validation expérimentale
Assessment of users to control simulated junctional hemorrhage with the combat ready clamp (CRoC™).
Mann-Salinas EA et all. Int J Burn Trauma 2013;3(1):49-54
The Combat Ready Clamp (CRoC™) was designed to control hemorrhage from the groin region, on the battlefield. The purpose of this experiment was to determine whether CRoC™ user performance varied by the surface the casualty laid on (flat-hard, flat-soft, and curved-soft) and how quickly the device could be applied. The commercial manikin selected to assess user performance was designed to train soldiers in CRoC™ use. The manikin simulated severe hemorrhage from an inguinal wound, controllable by correct use of the CRoC™. Each individual (n = 6) performed 3 iterations on each of the 3 surfaces (54 iterations total). The CRoC™ achieved hemorrhage control 100% of the time (54/54). Patient surface affected time to stop bleeding. The flat-soft surface (padded, 55 ± 9.7 seconds) was significantly different from the curved-soft surface (litter, 65 ± 16.5 seconds) and had the lowest overall total time (p = 0.007); time for the hard-flat surface was 58 ± 9.5 seconds. Users were trained to use the Combat Ready Clamp effectively, and the surface the casualty was lying on made some difference to user performance. All six persons trained had success in all nine of their iterations of CRoC™ use– a 100% rate. These findings indicate that training was effective and that training of other users is plausible, feasible, and practical within the scope of the present evidence.
19/01/2013
Hémorragies jonctionnelles: De quoi dispose-t-on en préhospitalier ?
La prise en charge d'hémorragies jonctionnelles est une véritable gageure en préhospitalier. Si ces hémorragies ne sont pas garrotables encore peut-on espérer d'en réduire le débit par la compression directe en ayant recours à l'association de packing de plaies, pansement hémostatiques et pansements compressifs. Depuis peu certains dispositifs mécaniques sont proposés bien que n'ayant pas fait l'objet de validation réelle. Une simple image vaut plus que de long commentaires, alors imprégnez vous de celles-ci.
1. Réaliser un pansement compressif:
Souvenez vous que vous devez disposer de pansement et que vous devez être en capacités de réaliser un pansement de ce type sur une racine de membres. Il doit être associer rembourage de toute cavité avec ce que vous avez sous la main, idéalement pansement hémostatique au contact de ce qui saigne et COMPRESSION forte.
2. Comprimer l'aorte abdominale:
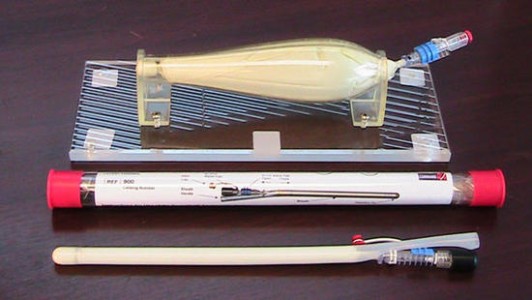
Le garrot abdominal (The Abdominal Aortic Tourniquet)
Ce dispositif existe depuis plusieurs années. Il a une assisse expérimentale mais n'est pas diffusé. On pourrait l'assimiler grossièrement au compartiment abdominal du pantalon antichoc
3. Comprimer l'artère fémorale au pli inguinal
Le CROC: (Combat Ready Clamp)
Ce dispsositif a été validé par l'armée US qui vient de l'intégrer au TCCC.
Le JETT (Junctional Emergency Treatment Tool)
Ce dispositif vient d'être présenté et semble être efficace
Lire aussi ce document
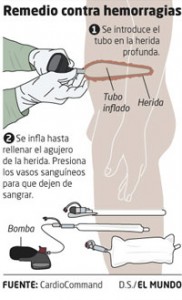
4. Réaliser l'équivalent d'un packing de plaie
Le principe est d'insérer un ballon que l'on gonfle dans la cavité. Ceci est faisable avec une sonde de foley, mais dans ce cas le ballon est de bien plus grand volume.
5. Comprimer directement la zone hémorragique par un clamp