16/05/2019
PST hémostatiques: Equivalents mais bases scientifiques pauvres
Systematic review of prehospital haemostatic dressings.
INTRODUCTION:
Haemorrhage is one of the leading causes of battlefield and prehospital death. Haemostatic dressings are an effective method of limiting the extent of bleeding and are used by military forces extensively. A systematic review was conducted with the aim of collating the evidence on current haemostatic products and to assess whether one product was more effective than others.
METHODS:
A systematic search and assessment of the literature was conducted using 13 health research databases including MEDLINE and CINAHL, and a grey literature search. Two assessors independently screened the studies for eligibility and quality. English language studies using current-generation haemostatic dressings were included. Surgical studies, studies that did not include survival, initial haemostasis or rebleeding and those investigating products without prehospital potential were excluded.
RESULTS:
232 studies were initially found and, after applying exclusion criteria, 42 were included in the review. These studies included 31 animal studies and 11 clinical studies. The outcomes assessed were subject survival, initial haemostasis and rebleeding. A number of products were shown to be effective in stopping haemorrhage, with Celox, QuikClot Combat Gauze and HemCon being the most commonly used, and with no demonstrable difference in effectiveness.
CONCLUSIONS:
There was a lack of high-quality clinical evidence with the majority of studies being conducted using a swine haemorrhage model. Iterations of three haemostatic dressings, Celox, HemCon and QuikClot, dominated the studies, probably because of their use by international military forces and all were shown to be effective in the arrest of haemorrhage.
Hémorragie: Garrot, mais aussi COMPRESSION
Bleeding control in combat fields with extreme transfer time

| Tags : tourniquet
02/05/2019
Tourniquet gonflable: Un nouveau venu
Rescue Bandage TQ Inflatable Tourniquet

Un garrot développé dans le cadre de la campagne STOP THE BLEED.
Apprendre à poser un garrot: En fait, pas si simple
Can they stop the bleed? Evaluation of tourniquet application by individuals with varying levels of prior self-reported training.
McCarty et Al. Injury. 2019 Jan;50(1):10-15. doi: 10.1016/j.injury.2018.09.041.
1 garrot sur 3 posé correctement malgré une formation ad-hoc.
--------------------------------------------------------
BACKGROUND:
Application of extremity tourniquets is a central tenet of multiple national initiatives to empower laypersons to provide hemorrhage control (HC). However, the efficacy of the general population who self-report prior first-aid (FA) or HC training on individual's ability to control bleeding with a tourniquet remains unknown. Therefore, the objective of this study was to assess the effectiveness of laypeople with self-reported prior FA or HC training to control bleeding with a tourniquet.
STUDY DESIGN:
Employees of a stadium were assessed via simulation in their ability to apply a Combat Application Tourniquet. As a subgroup analysis of a larger study, participants who self-reported: 1) No prior training, 2) FA training only or 2) FA + HC training were compared. Logistic regression adjusting for age, gender, education, willingness-to-assist, and comfort level in HC was performed.
RESULTS:
317 participants were included. Compared to participants with no prior training (14.4%,n = 16/111), those with FA training only (25.2%,n = 35/139) had a 2.12-higher odds (95%CI:1.07-4.18) of correct tourniquet application while those with FA + HC (35.8%,n = 24/67) had a 3.50-higher odds (95%CI:1.59-7.72) of correct application. Participants with prior FA + HC were more willing-to-assist and comfortable performing HC than those without prior training (p < 0.05).
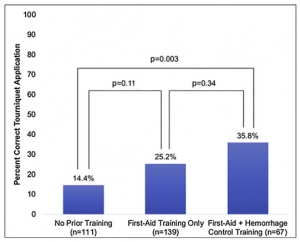
However, reporting being very willing-to-assist [OR0.83,95%CI:0.43-1.60] or very comfortable [OR1.11,95%CI:0.55-2.25] was not associated with correct tourniquet application.
CONCLUSION:
Self-reported prior FA + HC training, while associated with increased likelihood to correctly apply a tourniquet, results in only 1/3 of individuals correctly performing the skill. As work continues in empowering and training laypeople to act as immediate responders, these findings highlight the importance of effective layperson education techniques.
| Tags : tourniquet
26/04/2019
Bande de compression: Ne pas les vouer aux gémonies
Comparison of Two Tourniquets on a Mid-Thigh Model: The Israeli Silicone Stretch and Wrap Tourniquet vs. The Combat Application Tourniquet.
Le succès des garrots artériels tels que le SOFT-T et le CAT ne doit pas occulter l'intérêt des bandes de compression élastiques (Bande d'Esmach, SWAT-Tourniquet, IDF Silicone Tourniquet) préconisées en médecine rurale lors d'explosion de mines antipersonnelles (1). Ce travail met en avant leur efficacité.
-----------------------------------
Introduction:
Experience from recent conflicts underlines the dramatic impact of effective tourniquet use on combat casualty mortality. Although the Combat Application Tourniquet (CAT) is replacing the silicone band tourniquets (IST; "Israeli Silicone Tourniquet") in the Israeli Defense Forces, no direct comparison was made between them. The purpose of this study is to compare the performance of the two tourniquets on a mid-thigh model.
Methods:
Participants were Israeli military recruits who previously had the military first aid course. Each participant applied both the CAT and the IST. Applications were assessed by the HapMed Leg Tourniquet Trainer, which measured the applied pressure and the time required to reach it.

Results:
IST application resulted in higher rates of effective occlusion pressure compared with the CAT (91% vs. 73.1%, p < 0.01), and a higher mean occlusion pressure (41 mmHg, p < 0.01) was recorded using the IST. Among effective attempts, application time did not differ significantly between the tourniquets.
Effect of Elapsed Time Since First Aid Course on Success Rate
| Experience More Than 1 mo (n = 15) | Experience Equal to or Less Than 1 mo (n = 63) | p-Value | |
|---|---|---|---|
| Succeeded with CAT, n (%) | 7 (46.7) | 50 (79.4) | 0.01 |
| Succeeded with IST, n (%) | 14 (93.3) | 57 (90.5) | 0.5 |
Conclusion:
The IST was superior to the CAT in producing effective occlusion pressure while not prolonging application time. These results may indicate that the IST remains a valid option for controlling mid-thigh bleeding.
| Tags : tourniquet
04/04/2019
Un genou: Fait pour comprimer !
Martial arts technique for control of severe external bleeding.
Slevin JP et Al Emerg Med J. 2019 Mar;36(3):154-158. doi: 10.1136/emermed-2018-207966.
OBJECTIVES: Haemorrhage control is a critical component of preventing traumatic death. Other than the battlefield, haemostatic devices, such as tourniquets or bandages, may not be available, allowing for significant avoidable blood loss. We hypothesised that compression of vascular pressure points using a position adapted from the martial art of Brazilian Jiu-Jitsu could be adapted to decrease blood flow velocity in major extremity arteries.
METHODS: Knee mount compression was applied to the shoulder, groin and abdomen of healthy adult volunteer research subjects from Seattle, Washington, USA, from March through May 2018. Mean arterial blood flow velocity (MAV) was measured using ultrasound in the brachial and femoral arteries before and after compression. A MAV decrease greater than 20% with compression was deemed clinically relevant.
RESULTS: For 11 subjects, median (IQR) MAV combining all anatomical locations tested was 29.2 (34.1, 24.1) cm/s at baseline and decreased to 3.3 (0, 19.1) cm/s during compression (Wilcoxon p<0.001). MAV was significantly decreased during compression for each individual anatomical position tested (Wilcoxon p≤0.004). Per cent (95% CI) MAV reduction was significantly greater than 20% for shoulder compression at 97.5%(94% to 100%) and groin compression at 78%(56% to 100%), but was not statistically greater for abdominal compression at 35%(12% to 57%). Complete vessel occlusion was most common with compression at the shoulder (73%), followed by groin (55%) and abdomen (9%) (χ² LR, p=0.018).
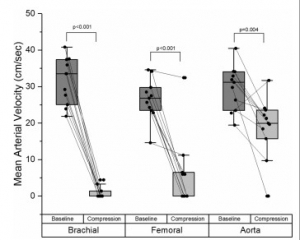
CONCLUSION: The Brazilian Jiu-Jitsu knee mount position can significantly decrease blood flow in major arteries of the extremities. This technique may be useful for bleeding control after injury.
10/03/2019
Garrot jonctionnel: Pas si performant que cela !
Comparison of Three Junctional Tourniquets Using a Randomized Trial Design.
BACKGROUND:
Hemorrhage remains a leading cause of death in both civilian and military settings. Of preventable deaths from hemorrhage, a significant portion occurs from junctional wounds that are not amenable to traditional extremity tourniquets. Junctional tourniquets (JTQs) can potentially provide hemorrhage control by compressing the arteries at the junction of the trunk and extremities. The FDA has cleared 3 JTQ products: The Combat Ready Clamp (CRoC®), the Junctional Emergency Treatment Tool (JETT™), and the SAM® JunctionalTourniquet (SJT). However, little is known regarding which of these JTQs is superior in application time, effectiveness in pulse elimination, effectiveness during transport, and user preference.
METHODS:
Active duty corpsmen (N = 49) were given standardized instruction and hands-on training with the CRoC®, JETT™, and SJT, then sequentially applied each JTQ unilaterally to a fellow study participant in a randomized order. Pulse elimination was determined by Doppler ultrasound at the dorsalis pedis immediately then reevaluated after a short transport. User preference data were collected following testing. Data were analyzed using repeated measures ANOVA and non-parametric statistics at p < 0.05.
RESULTS:
The CRoC® was significantly slower in application time than the JETT™ and SJT. Effectiveness was similar for CRoC®, JETT™, and SJT. Effectiveness during transport was significantly higher for SJT than for the JETT™, but no JTQ performed well during transport (24-48% effectiveness).
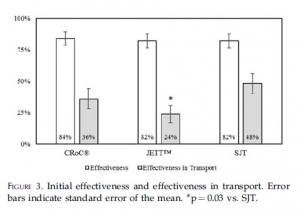
SJT ranked first in perceived ease of use, stability, and reliability, and in user trust and overall preference. Participants provided cogent suggestions for product improvement.
CONCLUSIONS:
All JTQ devices performed poorly during transport. Combined, present findings highlight the potential of JTQ products for saving lives threatened by junctional wounds, but also highlight the need for specific product improvements towards fostering JTQ performance in patient transport.
| Tags : jonctionnel
23/01/2019
Et pourquoi pas un ballonet pré-pelvien ?
Minimally invasive preperitoneal balloon tamponade and abdominal aortic junctional tourniquet versus open packing for pelvic fracture-associated hemorrhage: Not all extrinsic compression is equal.
--------------------------------------------------------
On propose souvent la réalisation d'une hémostase temporaire par a pose de sondes à ballonet. Ce travail (partiellement déjà présenté en 2016) rapporte une expérience de ce type avec un produit initialement dédié à la chirurgie pariétale herniaire. La simplicité de sa pose et son efficacité semblent prometteurs du moins chez le cochon.
--------------------------------------------------------
BACKGROUND:
Minimally invasive preperitoneal balloon tamponade (PPB) and abdominal aortic junctional tourniquets (AAJT) have been proposed as alternatives to open preperitoneal packing (OP) for the management of pelvic fracture-associated hemorrhage. We hypothesized that the PPB (SpaceMaker Pro) and AAJT would result in similar rates of survival and blood loss versus OP METHODS: 32 swine underwent creation of a combined open-book pelvic fracture and major iliac vascular injuries. Animals were randomized to no intervention (n=7), OP (n=10), PPB (n=9), or AAJT (n=6) at a mean arterial pressure <40 mmHg following initiation of uncontrolled hemorrhage. Survival (up to 60 min + 10 min after intervention reversal), hemodynamics, extraperitoneal pressures, blood loss, and associated complications were compared between groups.

RESULTS:
Prior to injury, no difference was measured between groups for weight, hemodynamics, lactate, and hematocrit (all p>0.05). The injury was uniformly lethal without intervention, with survival time (mean) of 5 min, peak preperitoneal pressure (PP) of 14 mmHg, blood loss of 960 g, and peak lactate of 2.6 mmol/L. Survival time was 44 min with OP vs. 60 min with PPB and AAJT (p<0.01). Peak PP (mmHg) was 19 with OP, 23 with PPB, and 23 with AAJT (p>0.05). Blood loss (g) was 850 with OP, 930 with PPB, and 600 with AAJT (p>0.05). Peak lactate (mmol/L) was 3.3 with OP, 4.3 with PPB, and 6.3 with AAJT (p<0.01). Only 33% of AAJT animals survived intervention reversal vs. 60% for OP and 67% for PPB (p<0.01). Necropsy revealed bowel/bladder injury in 50% of AAJT subjects vs. 0% in all other arms (p<0.01).
CONCLUSIONS:
PPB is a safe and potentially effective alternative to OP for the management of lethal pelvic fracture-associated hemorrhage. AAJT offers a similar survival benefit to PPB but has concerning rates of ischemia-reperfusion and compressive abdominal organ injury.
| Tags : pelvis
09/01/2019
Tourniquet: Comment sont ils testés ?
La qualité des garrots mis à disposition des combattants est très importante. On peut penser que c'est le cas avec les fabricants ayant pignon sur rue. C'est le cas notamment de TAC MED Solutions (SOFT Tourniquet) et de CAT Ressources ( le CAT). Il existe des machines spécifiquement conçues pour ces tests.
Clic sur l'image pour accéder au site
08/01/2019
TXA à l'avant: Peut être pas si simple !
Prehospital Tranexamic Acid Administration During Aeromedical Transport After Injury.
Tranexamic acid (TXA) has been shown to reduce mortality in the treatment of traumatic hemorrhage. This effect seems most profound when given early after injury. We hypothesized that extending a protocol for TXA administration into the prehospital aeromedical setting would improve outcomes while maintaining a similar safety profile to TXA dosed in the emergency department (ED).
MATERIALS AND METHODS:
We identified all trauma patients who received TXA during prehospital aeromedical transport or in the ED at our urban level I trauma center over an 18-mo period. These patients had been selected prospectively for TXA administration using a protocol that selected adult trauma patients with high-risk mechanism and concern for severe hemorrhage to receive TXA. Patient demographics, vital signs, lab values including thromboelastography, blood administration, mortality, and complications were reviewed retrospectively and analyzed.
RESULTS:
One hundred sixteen patients were identified (62 prehospital versus 54 ED). Prehospital TXA patients were more likely to have sustained blunt injury (76% prehospital versus 46% ED, P = 0.002). There were no differences between groups in injury severity score or initial vital signs.
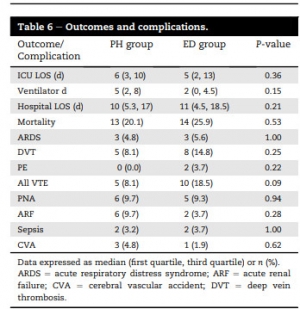
There were no differences in complication rates or mortality. Patients receiving TXA had higher rates of venous thromboembolic events (8.1% in prehospital and 18.5% in ED) than the overall trauma population (2.1%, P < 0.001).
CONCLUSIONS:
Prehospital administration of TXA during aeromedical transport did not improve survival compared with ED administration. Treatment with TXA was associated with increased risk of venous thromboembolic events. Prehospital TXA protocols should be refined to identify patients with severe hemorrhagic shock or traumatic brain injury.
09/11/2018
Tourniquet abdominal: OK pour 60 min mais max 240 min
Abdominal Aortic and Junctional Tourniquet release after 240 minutes is survivable and associated with small intestine and liver ischemia after porcine class II hemorrhage.
Uncontrolled hemorrhage is a leading cause of tactical trauma-related deaths. Hemorrhage from the pelvis and junctional regions are particularly difficult to control due to the inability of focal compression. The Abdominal Aortic and Junctional Tourniquet (AAJT) occludes aortic blood flow by compression of the abdomen. The survivability of tourniquet release beyond 120 minutes is unknown and fluid requirements to maintain sufficient blood pressure during prolonged application are undetermined. We therefore compared 60-minute and 240-minute applications and release of the AAJT for 30 minutes, with crystalloid fluid therapy, after a Class II hemorrhage.
METHODS:
Sixty-kilogram anesthetized pigs were subjected to 900-mL hemorrhage and AAJT application for 60 minutes (n = 5), 240 minutes (n = 5), and fluid therapy only for 240 minutes (n = 5) and reperfusion for 30 minutes.
RESULTS:
The AAJT application was hemodynamically and respiratory tolerable for 60 minutes and 240 minutes. Cumulative fluid requirements decreased by 64%, comparable to 3000 mL of crystalloids. Mechanical ventilation was impaired. AAJT increased the core temperature by 0.9°C compared with fluid therapy. Reperfusion consequences were reversible after 60 minutes but not after 240 minutes. A 240-minute application resulted in small intestine and liver ischemia, persisting hyperkalemia, metabolic acidosis, and myoglobinemia, suggesting rhabdomyolysis.
CONCLUSION:
The AAJT application for 240 minutes with reperfusion was survivable in an intensive care setting and associated with abdominal organ damage. Long time consequences and spinal cord effects was not assessed. We propose an application time limit within 60 minutes to 240 minutes, though further studies are needed to increase the temporal resolution. The AAJT application may be considered as a rescue option to maintain central blood pressure and core temperature in cases of hemorrhagic shock from extremity bleedings, if fluid therapy is unavailable or if the supply is limited.
08/11/2018
Tourniquet abdominal: Le - longtemps possible
Long-term consequences of abdominal aortic and junctional tourniquet for hemorrhage control
Kheirabadi BS et Al. J Surg Res. 2018 Nov;231:99-108.
BACKGROUND:
Specialized tourniquets have been deployed to the battlefield for the control of junctional/pelvic hemorrhage despite limited knowledge concerning their safety and duration of use. This study investigated long-term effects of abdominal application of the abdominal aortic and junctionaltourniquet (AAJT) in a swine survival model.
METHODS:
Anesthetized spontaneously air-breathing swine were subjected to bilateral femoral artery injuries and subsequent 40% hemorrhage. Further hemorrhage was controlled by applying the AAJT on the lower abdomen for 0 h (n = 2, controls), 1 h (n = 6), 1.5 h (n = 6), or 2 h (n = 3). Before tourniquet release, arterial injuries were repaired, and mechanical ventilation and rapid crystalloid fluid were provided for at least 5 min. Additional fluid and 500 mL autologous blood were transfused after restoring blood flow. Animals were recovered and their mobility and health monitored up to 2 wk.
RESULTS:
AAJT application occluded the infrarenal abdominal aorta and stopped bilateral groin hemorrhage with rapid reversal of hemorrhagic shock and improved cranial blood pressure. All animals including controls recovered overnight but regaining hind leg function varied among AAJT-treated groups.
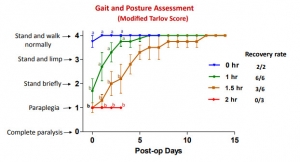
In contrast to 1 h AAJT-treated swine that recovered full mobility in 1 wk, 2 h animals developed persistent hind leg paraplegia concurrent with urinary retention and ischemic necrosis of lumber muscles and had to be euthanized 3 d after surgery. Half of the 1.5-h group also had to be euthanized early due to paraplegia, whereas the other half recovered motor function within 2 wk.
CONCLUSIONS:
The results of this animal study indicated that ischemic reperfusion injuries associated with abdominal application of the AAJT were time-dependent. To avoid permanent injuries, AAJT application on the abdomen to control a groin hemorrhage could not be longer than 1 h. This was consistent with recent instructions for application of this tourniquet on the abdomen in patients
Tourniquet abdominal = REBOA Zone 3
Comparison of zone 3 Resuscitative Endovascular Balloon Occlusion of the Aorta and the Abdominal Aortic and Junctional Tourniquet in a model of junctional hemorrhage in swine
BACKGROUND:
Traumatic injuries to the pelvis and high junctional injuries are difficult to treat in the field; however, Resuscitative EndovascularBalloon Occlusion of the Aorta (REBOA) and the Abdominal Aortic and Junctional Tourniquet (AAJT) constitute two promising treatment modalities. The aim of this study is to use a large animal model of pelvic hemorrhage to compare the survival, hemostatic, hemodynamic, and metabolic profile of both techniques.
METHODS:
Yorkshire swine (n = 10, 70-90 kg) underwent general anesthesia, instrumentation, and surgical isolation of the femoral artery. Uncontrolled hemorrhage was initiated by an arteriotomy. Animals were randomly allocated to either REBOA or AAJT. Following completion of device application, both groups received a 500 mL Hextend bolus. After 1 hour, the injured femoral artery was ligated to simulate definitive hemostasis followed by a second Hextend bolus and device removal. Animals were observed for two more hours. Physiological data were collected throughout the experiments and compared between groups.
RESULTS:
Both techniques achieved 100% hemostasis, and all animals survived the entire experiment except one in the REBOA group. During the hour treatment phase, the AAJT group had a higher mean arterial pressure than the REBOA group (59.9 ± 16.1 versus 44.6 ± 9.8 mm Hg, respectively; P < 0.05). The AAJT-treated group had higher lactate levels than the REBOA-treated group (4.5 ± 2.0 versus 3.2 ± 1.3 mg/dL, respectively; P < 0.05).
CONCLUSIONS:
Despite their mechanistic differences, both techniques achieved a similar hemostatic, hemodynamic, and metabolic profile. Some differences do exist including lactate levels and blood pressure.
09/10/2018
Voies aériennes et choc hémorragique, que faire ?
Airway and ventilation management strategies for hemorrhagic shock. To tube, or not to tube, that is the question!
Hudson AJ et Al. J Trauma Acute Care Surg. 2018 Jun;84(6S Suppl 1):S77-S82
------------------------------
Primum non nocere. Souvent ne pas faire parce que c'est le plus prudent ET NON PAS PARCE QU'ON N'A PAS APPRIS ET QU'ON NE SAIT DONC PAS FAIRE.
------------------------------
Many standard trauma management guidelines advocate the early use of endotracheal intubation (ETI) and positive pressure ventilation as key treatment interventions in hemorrhagic shock. The evidence for using these airway and ventilation strategies to manage a circulation problem is unclear. The potentially harmful effects of drug-assisted intubation and positive pressure ventilation include reduced cardiac output, apnea, hypoxia, hypocapnea (due to inadvertent hyperventilation), and unnecessarily prolonged on-scene times. Conversely, the beneficial effects of spontaneous negative pressure ventilation on cardiac output are well described. Few studies, however, have attempted to explore the potential advantages of a strategy of delayed intubation and ventilation (together with a policy of aggressive volume replacement) in shocked trauma patients. Given the lack of evidence, the decision making around how, when, and where to subject shocked trauma patients to intubation and positive pressure ventilation remains complex. If providers choose to delay intubation, they must have the appropriate skills to safely manage the airway and recognize the need for subsequent intervention. If they decide to perform intubation and positive pressure ventilation, they must understand the potential risks and how best to minimize them. We suggest that for patients with hemorrhagic shock who do not have a compromised airway and who are able to maintain adequate oxygen saturation (or mentation if monitoring is unreliable), a strategy of delayed intubation should be strongly encouraged.
| Tags : choc
Pansement hémostatique: Emploi ciblé pour les + graves ?
Catastrophic haemorrhage in military major trauma patients: a retrospective database analysis of haemostatic agents used on the battlefield.
Winstanley M Winstanley et Al. J R Army Med Corps. 2018 Oct 3. pii: jramc-2018-001031
-----------------------------------------
Une publication qui mettrait en évidence l'intérêt des pansements hémostatiques avec une amélioration de la survie des blessés les plus graves. A prendre quand même avec de beaucoup de recul car les derniers blessés inclus le sont sur une période de plus de 10 ans et qu'entre temps beaucoup d'évolution ont eu lieu tant sur la stratégie de prise en charge que les pansements hémostatiques notamment pour le QUIKCLOT concurrent américain du CELOX qui lui est britannique. Par ailleurs les groupes sont stratifiés par index global de sévérité sans que l'on ait une idée sur la nature des lésions ayant motivé leur emploi? Comme pour les tourniquets où les contrefaçons foisonnent, les enjeux financiers liés à la promotion de tel pansement ou d'un autre sont colossaux dès lors que le marché civil s'ouvre à eux. Une publication dont l'impartialité est à remettre en cause. On rappelle quand même qu'un bon packing de plaie avec un bon pansement compressif représentent la base.
-----------------------------------------
OBJECTIVES:
Catastrophic haemorrhage is a leading cause of morbidity and mortality in trauma, in both military and civilian settings. There are numerous studies looking at the effectiveness of different haemostatic agents in the laboratory but few in a clinical setting. This study analyses the use of haemostatic dressings used in patients injured on the battlefield and their association with survival.
METHOD:
A retrospective database review was undertaken using the UK Joint Theatre Trauma Registry from 2003 to 2014, during combat operations in Iraq and Afghanistan. Data included patient demographics, the use of haemostatic dressings, New Injury Severity Score (NISS) and patient outcome.
RESULTS:
Of 3792 cases, a haemostatic dressing was applied in 317 (either Celox, Hemcon or Quickclot). When comparing patients who had a haemostatic dressing applied versus no haemostatic agent, there was a 7% improvement in survival. Celox was the only individual haemostatic dressing that was associated with a statistically significant improvement in survival, which was most apparent in the more severely injured (NISS 36-75).
CONCLUSION:
We have shown an association between use of haemostatic agents and improved survival, mostly in those with more severe injuries, which is particularly evident in those administered Celox. This supports the continued use of haemostatic agents as part of initial haemorrhage control for patients injured in conflict and suggests that civilian organisations that may need to deal with patients with similar injury patterns should consider their use and implementation.
| Tags : packing
03/10/2018
Plaquettes et golden hour: Possible ?
Intravenous synthetic platelet (SynthoPlate) nanoconstructs reduce bleeding and improve 'golden hour' survival in a porcine model of traumatic arterial hemorrhage.
Traumatic non-compressible hemorrhage is a leading cause of civilian and military mortality and its treatment requires massive transfusion of blood components, especially platelets. However, in austere civilian and battlefield locations, access to platelets is highly challenging due to limited supply and portability, high risk of bacterial contamination and short shelf-life. To resolve this, we have developed an I.V.-administrable 'synthetic platelet' nanoconstruct (SynthoPlate), that can mimic and amplify body's natural hemostatic mechanisms specifically at the bleeding site while maintaining systemic safety.

Previously we have reported the detailed biochemical and hemostatic characterization of SynthoPlate in a non-trauma tail-bleeding model in mice. Building on this, here we sought to evaluate the hemostatic ability of SynthoPlate in emergency administration within the 'golden hour' following traumatic hemorrhagic injury in the femoral artery, in a pig model. We first characterized the storage stability and post-sterilization biofunctionality of SynthoPlate in vitro. The nanoconstructs were then I.V.-administered to pigs and their systemic safety and biodistribution were characterized. Subsequently we demonstrated that, following femoral artery injury, bolus administration of SynthoPlate could reduce blood loss, stabilize blood pressure and significantly improve survival. Our results indicate substantial promise of SynthoPlate as a viable platelet surrogate for emergency management of traumatic bleeding.
22/07/2018
Chitine: Prudence quand même ?
Chitin and Its Effects on Inflammatory and Immune Responses
-------------------------------------------
Les pansements hémostatiques à base de chitine sont largement utilisés et ne semblent pas actuellement poser de problème allergique (1). Néanmoins se pose la question de leur innocuité immune. Le développement des allergies croisées avec les produits dérivés de la mer et l'emploi de chitine comme complément alimentaire sont autant de facteurs de rencontre avec un allergène vrai. De telles allergies croisées s'observent également avec d'autres composants tels que la paravalbumine et le collagène des produits de la mer. Les pansements hémostatiques ne contenant pas de chitine ne semble pas exposer à ce risque potentiel.

-------------------------------------------
Chitin, a potential allergy-promoting pathogen-associated molecular pattern (PAMP), is a linear polymer composed of N-acetylglucosamine residues which are linked by β-(1,4)-glycosidic bonds. Mammalians are potential hosts for chitin-containing protozoa, fungi, arthropods, and nematodes; however, mammalians themselves do not synthetize chitin and thus it is considered as a potential target for recognition by mammalian immune system. Chitin is sensed primarily in the lungs or gut where it activates a variety of innate (eosinophils, macrophages) and adaptive immune cells (IL-4/IL-13 expressing T helper type-2 lymphocytes). Chitin induces cytokine production, leukocyte recruitment, and alternative macrophage activation. Intranasal or intraperitoneal administration of chitin (varying in size, degree of acetylation and purity) to mice has been applied as a routine approach to investigate chitin's priming effects on innate and adaptive immunity. Structural chitinpresent in microorganisms is actively degraded by host true chitinases, including acidic mammalian chitinases and chitotriosidase into smaller fragments that can be sensed by mammalian receptors such as FIBCD1, NKR-P1, and RegIIIc. Immune recognition of chitin also involves pattern recognition receptors, mainly via TLR-2 and Dectin-1, to activate immune cells to induce cytokine production and creation of an immune network that results in inflammatory and allergic responses. In this review, we will focus on various immunological aspects of the interaction between chitin and host immune system such as sensing, interactions with immune cells, chitinases as chitin degrading enzymes, and immunologic applications of chitin.
21/07/2018
+ d'1 Tourniquet et 1/4 converti
Point of injury tourniquet application during Operation Protective Edge-What do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate- and short-term outcomes of point of injury (POI) tourniquet applications during "Operation Protective Edge" (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications, and short-term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps treated 704 casualties. Of these, 90 casualties were treated with 119 tourniquets of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88 of 90) of the casualties. Injuries sustained from improvised explosive devices and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p = 0.034). The success rate of the first tourniquet was reported to be 70% (84 of 119), regardless of caregiver level (p = 0.56), tourniquet type (p = 0.16), or limb characters (p = 0.48). Twenty-seven (25.7%) of 105 of the tourniquets were converted to direct pressure dressings enroute to receiving hospitals two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on eight casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5 of 85), no vascular involvement was discovered during surgery, and the fasciotomy is suspected as tourniquet related. 7%) 6 of 85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10 of 85) (one patient had both fasciotomy and neural complication without vascular injury).
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity, whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet
01/05/2018
Tourniquet: Une vieille histoire
A brief history of the tourniquet
Welling DR et Al. Vasc Surg 2012;55:286-90
Le compresseur de Matas
| Tags : tourniquet
01/03/2018
Trauma jonctionnels: Une revue
| Tags : jonctionnel, hémorragie