23/10/2015
Quelle place pour les facteurs de la coagulation ?
| Tags : hémorragie, coagulopathie, choc
30/09/2015
REBOA: Un savoir faire à maîtriser ?
Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage
Moor LJ et Al. J Trauma Acute Care Surg. 2015;79: 523-532
L'application du concept du garrot tactique a fait évoluer la répartition des causes évitables de décès à l'avant et met actuellement au premier plan les hémorragies du tronc (Eastridge) . SI le bon usage du garrot reste un enjeu essentiel, les efforts portent maintenant sur la prise en charge d'une part des hémorragies jonctionnelles avec le recours de dispositifs tels que le CRoC, le Sam Junctional tourniquet ou l'abdominal tourniquet et d'autre part sur la prise en charge des hémorragies du tronc. Une autre approche, connue depuis de nombreuses années mais tombée en désuétude, refait surface. L'occlusion endovasculaire de l'aorte abdominale apparaît être d'un intérêt certain. C'est ce que documente le travail présenté ci dessous. Réaliser un tel geste en préhospitalier est possible (1,2). En ce qui concerne les applications militaires dans les structures chirurgicales de role 2 voire dans certaines moyens de transport préhospitalier une réflexion apparaît nécessaire.
------------------------------------------
BACKGROUND:
Hemorrhage remains the leading cause of death in trauma patients. Proximal aortic occlusion, usually performed by direct aortic cross-clamping via thoracotomy, can provide temporary hemodynamic stability, permitting definitive injury repair. Resuscitative endovascular balloon occlusion of the aorta (REBOA) uses a minimally invasive, transfemoral balloon catheter, which is rapidly inserted retrograde and inflated for aortic occlusion, and may control inflow and allow time for hemostasis. We compared resuscitative thoracotomy with aortic cross-clamping (RT) with REBOA in trauma patients in profound hemorrhagic shock.
METHODS: Trauma registry data was used to compare all patients undergoing RTor REBOA during an 18-month period from two Level 1 trauma centers.
RESULTS: There was no difference between RT (n = 72) and REBOA groups (n = 24) in terms of demographics, mechanism of injury, or Injury Severity Scores (ISSs). There was no difference in chest and abdominal Abbreviated Injury Scale (AIS) scores between the groups. However, the RT patients had lower extremity AIS score as compared with REBOA patients (1.5 [0-3] vs. 4 [3-4],p G 0.001). Of the 72 RT patients, 45 (62.5%) died in the emergency department, 6 (8.3%) died in the operating room, and 14 (19.4%) died in the intensive care unit. Of the 24 REBOA patients, 4 (16.6%) died in the emergency department, 3 (12.5%) died in the operating room, and 8 (33.3%) died in the intensive care unit. In comparing location of death between the RT and REBOA groups, there were a significantly higher number of deaths in the emergency department among the RT patients as compared with the REBOA patients (62.5% vs. 16.7%, p G 0.001). REBOA had fewer early deaths and improved overall survival as compared with RT (37.5% vs. 9.7%, p = 0.003).
CONCLUSION: REBOA is feasible and controls noncompressible truncal hemorrhage in trauma patients in profound shock. Patients undergoing REBOA have improved overall survival and fewer early deaths as compared with patients undergoing RT.
| Tags : junctionnel
18/07/2015
Tourniquet et chaleur extrême ?
Laboratory testing of emergency tourniquets exposed to prolonged heat
Davidson JP et Al. J Spec Oper Med. 2015 Spring;15(1):34-8.
----------------------------------------------------------
Il a été démontré que la fiabilité mécanique des tourniquets pouvait être altérée si ces derniers n'étaient pas protégés (1,2,3). Le travail présenté porte sur l'effet de l'exposition prolongée à de hautes températures sur l'efficacité des garrots. Apparemment il n'y aurait pas d'effet propre.
----------------------------------------------------------
BACKGROUND:
Environmental exposure of tourniquets has been associated with component damage rates, but the specific type of environmental exposure, such as heat, is unknown. Emergency-tourniquet damage has been associated with malfunction and loss of hemorrhage control, which may risk loss of life during first aid. The purposes of the study are to determine the damage rate of tourniquets exposed to heat and to compare the rate to that of controls.
METHODS:
Three tourniquet models (Combat Application Tourniquet®; SOF® Tactical Tourniquet; Ratcheting Medical Tourniquet®) were tested using a manikin (HapMed Leg Tourniquet Trainer; www.chisystems.com) that simulates extremity hemorrhage. The study group of 15 tourniquets (five devices per model, three models) was exposed to heat (oven at 54.4° C [130° F] for 91 days), and 15 tourniquets similarly constituted the control group (unexposed to heat). Damage, hemorrhage control, distal pulse stoppage, time to effectiveness, pressure (mmHg), and blood loss volumes were measured.
RESULTS:
Three tourniquets in both groups had damage not associated with heat exposure (p = 1). Heat exposure was not associated with change in effectiveness rates (p = .32); this lack of association applied to both hemorrhage control and pulse stoppage. When adjusted for the effects of user and model, the comparisons of time to effectiveness and total blood loss were statistically significant (p < .0001), but the comparison of pressure was not (p = .0613).
CONCLUSION:
Heat exposure was not associated with tourniquet damage, inability to gain hemorrhage control, or inability to stop the distal pulse.
| Tags : tourniquet
17/07/2015
Tourniquet: Une histoire de pression pas si simple
Tourniquets and Occlusion: The Pressure of Design
Wall PL et Al. Mil Med. 2013 May;178(5):578-87
-----------------------------------------------
Un travail très intéressant qui exprime bien que l'efficacité d'un garrot nécessite un ensemble de gestes parfaitement réalisés, notamment un serrage suffisant qui doit être vérifié après la pose. Il existe en effet avec les garrots de type tourniquet ou pneumatique une chute plus ou moins importante de la pression d'occlusion donc de perte d'occlusion, ce d'autant qu'un relâchement musculaire peut apparaître réduisant d'autant plus cette pression d'occlusion. Les garrots élastiques n'aurait pas cet inconvénient.
-----------------------------------------------
Abstracts: Nerve injuries result from tourniquet pressure. The objective was to determine arterial occlusion and completion pressures with the 3.8-cm-wide windlass Combat Application Tourniquet (CAT) and the 10.4-cm-wide Stretch, Wrap, and Tuck Tourniquet (SWAT-T).
Methods: Sixteen volunteers self-applied and had tourniquets applied to their thighs and arms (CAT and SWAT-T, random order, then blood pressure cuffs).
Results: Occlusion (Doppler signal elimination) pressures were higher than predicted ( p < 0.0001), highest with the CAT ( p < 0.0001), and often lower than completion pressures (completion median, range: CAT 360, 147–745 mm Hg; SWAT-T 290, 136–449 mm Hg; cuff 184, 108–281 mm Hg). Three CAT thigh and 9 CAT arm completion pressures were >500 mm Hg. Pressure decreases and occlusion losses occurred over 1 minute (pressure decrease: CAT 44 ± 33 mm Hg; SWAT-T 6 ± 8 mm Hg; cuff 14 ± 19 mm Hg; p < 0.0001; loss/initially occluded: CAT 17 of 61, SWAT-T 5 of 61, cuff 40 of 64, p < 0.01). CAT pressures before turn did not have a clear relationship with turns to occlusion.
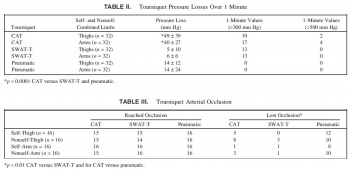 Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
| Tags : tourniquet
21/03/2015
Tourniquet: Efficace, uniquement si serré fort
Forward Assessment of 79 Prehospital Battlefield Tourniquet Use in the Current War
King DR et Al. J Spec Oper Med. 2012 Winter;12(4):33-8.
----------------------------------------------------------------------
La pose libérale d'un garrot est présentée comme étant un facteur essentiel de survie des blessés des membres. Encore faut il que ces derniers soient posés de manière correcte. Le document présenté laisse planer un gros doute. En effet il met en évidence qu'un garrot est mis en place 3 fois sur 4 alors qu'il n'y a pas de lésion vasculaire notable et que la plupart des garrots posés ne sont pas suffisamment serrés et sont en fait des garrots veineux. Pire seuls 1/3 des blessés ayant des lésions artérielles se voient appliquer un garrot artériel. C'est dire qu'une attention particulière doit être portée sur l'abolition du pouls artériel distal. Il s'agit là d'un enjeu pédagogique majeur.
----------------------------------------------------------------------
Introduction:
Battlefield tourniquet use can be lifesaving, but most reports are from hospitals with knowledge gaps remaining at the forward surgical team (FST). The quality of tourniquet applications in forward settings remain unknown. The purpose of this case series is to describe observations of tourniquet use at an FST in order to improve clinical performance.
Methods:
War casualties with tourniquet use presenting to an FST in Afghanistan in 2011 were observed. We identified appliers by training, device effectiveness, injury pattern, and clinical opportunities for improvement. Feedback was given to treating medics.
Results:
Tourniquet applications (79) were performed by special operations combat medics (47, 59%), flight medics (17, 22%), combat medics (12, 15%), and general surgeons (3, 4%). Most tourniquets were Combat Application Tourniquets (71/79, 90%). With tourniquets in place upon arrival at the FST, most limbs (83%, 54/65) had palpable distal pulses present; 17% were pulseless (11/65). Of all tourniquets, the use was venous in 83% and arterial in 17%. In total, there were 14 arterial injuries, but only 5 had effective arterial tourniquets applied.
Discussion:
Tourniquets are liberally applied to extremity injuries on the battlefield. 17% were arterial and 83% were venous tourniquets. When ongoing bleeding or distal pulses were appreciated, medics tightened tourniquets under surgeon supervision until distal pulses stopped. Medics were generally surprised at how tight a tourniquet must be to stop arterial flow–convert a venous tourniquet into an arterial tourniquet. Implications for sustainment training should be considered with regard to this life-saving skill.
| Tags : tourniquet, garrot, hémorragie
13/01/2015
Attentats: Importance du garrot
The Initial Response to the Boston Marathon Bombing. Lessons Learned to Prepare for the Next Disaster
Gates JD et AL. Ann Surg. 2014 Dec;260(6):960-6
-----------------------------------------------------------------------------------
Le concept du garrot tactique est familier aux équipes militaires. L'expérience rapportée montre que ce concept doit également le devenir dans le monde de la médecine préhospitalière. 26 soit près de 10% blessés pris en charge ont fait l'objet d'une pose de garrot. Ainsi en cas d'attentat la pose précoce d'un garrot en cas d'hémorragie des membres est elle une mesure fondamentale de mise en condition de survie.
-----------------------------------------------------------------------------------
OBJECTIVE:
We discuss the strengths of the medical response to the Boston Marathon bombings that led to the excellent outcomes. Potential shortcomings were recognized, and lessons learned will provide a foundation for further improvements applicable to all institutions.
BACKGROUND:
Multiple casualty incidents from natural or man-made incidents remain a constant global threat. Adequate preparation and the appropriate alignment of resources with immediate needs remain the key to optimal outcomes.
METHODS:
A collaborative effort among Boston's trauma centers (2 level I adult, 3 combined level I adult/pediatric, 1 freestanding level I pediatric) examined the details and outcomes of the initial response. Each center entered its respective data into a central database (REDCap), and the data were analyzed to determine various prehospital and early in-hospital clinical and logistical parameters that collectively define the citywide medical response to the terrorist attack.
RESULTS:
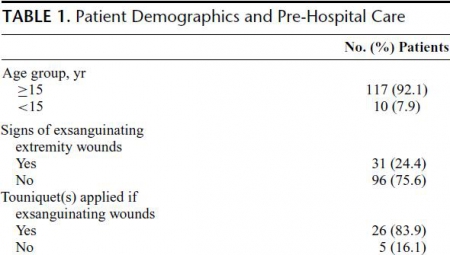
A total of 281 people were injured, and 127 patients received care at the participating trauma centers on that day. There were 3 (1%) immediate fatalities at the scene and no in-hospital mortality. A majority of the patients admitted (66.6%) suffered lower extremity soft tissue and bony injuries, and 31 had evidence for exsanguinating hemorrhage, with field tourniquets in place in 26 patients. Of the 75 patients admitted, 54 underwent urgent surgical intervention and 12 (22%) underwent amputation of a lower extremity.
CONCLUSIONS:
Adequate preparation, rapid logistical response, short transport times, immediate access to operating rooms, methodical multidisciplinary care delivery, and good fortune contributed to excellent outcomes.
| Tags : tourniquet, garrot, hémorragie
13/12/2014
Quikclot: Un bon choix, mais les autres aussi
Comparison of novel hemostatic dressings with QuikClot combat gauze in a standardized swine model of uncontrolled hemorrhage.
Rall JM et AL. J Trauma Acute Care Surg. 2013 Aug;75(2 Suppl 2):S150-6
L'emploi des pansements hémostatiques en médecine de l'avant est devenue une pratique courante, même si cette dernière s'appuie sur relativement peu d'arguments avérés. Leur efficacité repose sur leur application au contact de la lésion qui saigne et une compression initiale. Hors ces deux critères de performance sont pas toujours remplis en condition de combat. C'est ce qui explique que certains soient relativement critiques par rapport à leur intérêt réel en condition de combat et on insiste beaucoup actuellement sur la notion de pansement compressif et de packing de plaie. Il n'en demeure pas moins indispensable de connaître ce que propose l'industrie en la matière. Le document proposé fait le point sur le différents produits utilisables. Il utilise pour cela un modèle expérimental de plaie artérielle. Sont comparés trois produits le Quikclot, le Celox et le Chitogauze. 5 versions au total sont analysées car le Quikclot et le Celox sont proposés en deux versions qui diffèrent par leur masse.
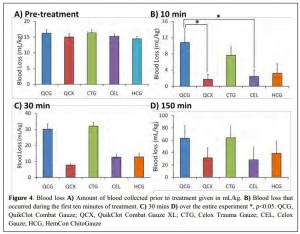

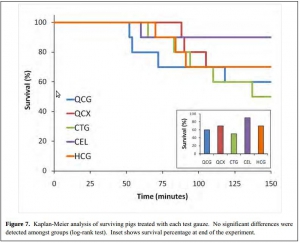
Très globalement plus la masse de produit est grande et plus l'efficacité est au rendez vous (Le Quikclot XL et le Celox, masse de 50 g de pansement) . Parmi les présentations qui proposent une masse de pansement de l'ordre de 20g l'Hemcon Chitogauze apparaît être immédiatement le plus efficace malheureusement est observé un pourcentage de resaignement élevé. Finalement de ce document on peut retenir que l'Hemcon Chitogauze, le CeloxTrauma gauze et le Quikclot Gauze ont des performances similaires. On remarque que pour le Quikclot Gauze la survie à 150 min est la plus élevée pour les pansements de 20 g, même si ceci n'est pas significatif au plan statistique. Ce dernier reste donc un très bon choix. Il est en dotation dans l'armée française .
On rappelle que ce dernier existe en deux version la version rolled et la version Z folded qui est plus particulièrement mise en avant par le fabricant pour les applications militaires.
07/12/2014
Tourniquet: Que disent les utilisateurs ?
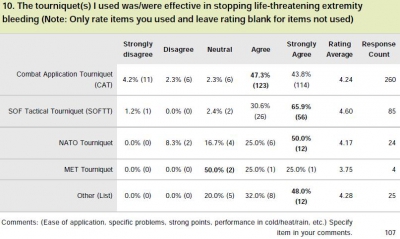
Le garrot en dotation dans l'armée française est le Special Operation Tactical Tourniquet (SOFT-T) , concurrent du Combat Application Tourniquet (CAT). Il existe de nombreux travaux qui cherchent à comparer entre eux les divers produits proposés par l'industrie. Tel garrot semble plus efficace sur des modèles expériemetaux, un autre voit sa barre de torsion se briser, un autre est plus fragile que son concurrent lorsque les conditions de stockage ne sont pas optimales.

Une autre démarche consiste à demander à ceux qui les ont employé en conditions réelles. Une idée est donnée par le tableau qui suit et qui est tiré d'un questionnaire de suivi de mise en oeuvre des équipements du TCCC. Le modèle actuellement en dotation apparaît parfaitement adapté.
Clic sur l'image pour accéder au suivi des équipemens du TCCC
| Tags : tourniquet
01/11/2014
Garrot: A partir de quand est on fiable ?
Single versus Double Routing of the Band in the Combat Application Tourniquet.
J Spec Oper Med. 2013 Spring;13(1):34-41.
Le sauvetage au combat met en avant l'importance d'arrêter toute hémorragie le plus tôt possible. Le garrot tient là une place essentielle. Mais à partir de quand l'apprentissage de cette technique peut il être considéré comme optimal. Une réponse est apporté par ce travail: La maîtrise de ce geste semble être obtenue à partir de 30 poses.
Background: Common first aid tourniquets, like the Combat Application Tourniquet (CAT) of a windlass and band design, can have the band routed through the buckle in three different ways, and recent evidence indicates users may be confused with complex doctrine.
Objective: The purpose of the present study is to measure the differential performance of the three possible routings in order to better understand good tourniquet practice.
Methods: A training manikin was used by two investigators to measure tourniquet effectiveness, time to stop bleeding, and blood loss.
Results: The effectiveness rate was 99.6% (239/240) overall. Results were similar for both single-slit routings (inside vs. outside, p > 0.05). Effectiveness rates (yes-no results for hemorrhage control expressed as a proportion of iterations) were not statistically different between single and double routing. However, the time to stop bleeding and blood loss were statistically different (p < 0.05).
Conclusions: CAT band routing, through the buckle either singly or doubly, affects two key performance criteria: time to stop bleeding and volume of blood lost. Single routing proved to be faster, thereby saving more blood. Learning curves required to optimize user performance varied over 30-fold depending on which variable was selected (e.g., effectiveness vs. blood loss).
| Tags : tourniquet
N'oublions pas: Comprimer est essentiel
Laboratory assessment of out-of-hospital interventions to control junctional bleeding from the groin in a manikin model l.
Kragh JF et Al Am J Emerg Med. 2013 Aug;31(8):1276-8
Junctional body regions between the trunk and its appendages, such as the groin, are too proximal for a regular limb tourniquet to fit [1,2]. Not since 1993’s Black Hawk Down has junctional hemorrhage control become such a hot topic in military casualty care [1–7]. In February 2013, the US military’s Task Force Medical Afghanistan requested a fill of a gap in junctional hemorrhage control as an urgent operational need, meaning that junctional hemorrhage control devices should be considered urgently to fill a gap in medical care in war. A small but growing body of evidence indicates that hemorrhage control can be attained out-of-hospital with mechanical compression, using such interventions as medical devices, on a pressure point proximal to a bleeding wound [3–9]. To evaluate laboratory use of junctional hemorrhage control interventions, we gathered data on stopping groin bleeding in a manikin model to understand the plausibility of such interventions for future human subject research.
Under an approved protocol, we tested efficacy of interventions in a manikin designed to train medics in out-of-hospital hemorrhage control (Combat Ready Clamp [CRoC] Trainer Manikin, Operative Experience, Inc, North East, MD). We filled the blood reservoir with 4 liters of water; we refilled the reservoir after 5 iterations or 1.5 liters of lost fluid, whichever came first. The manikin had a right-groin gunshot wound through the proximal thigh where the common femoral artery flow was controllable by skin compression over it at the level of the inguinal fold. There was 3 cm between the pressure point where compression was applied and the proximal extent of the wound. Interventions were timed, blood loss was measured, and efficacy was noted. Efficacy was operationally defined as visually stopped flow into the wound from the vessel lumen. Pearls and pitfalls of intervention use were recorded.
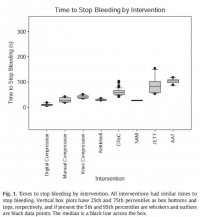
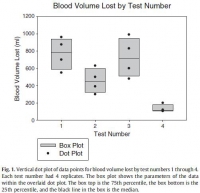
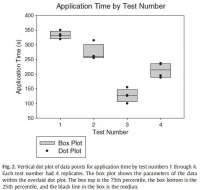
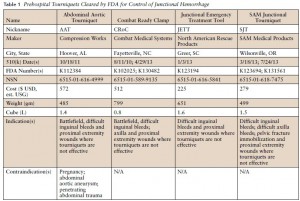
Interventions to control hemorrhage included medical device use, manual or digital compression, and improvised use of a rock-like kettlebell (to simulate a rock used in care on the battlefield in a case recorded in the Department of Defense Trauma Registry in 2012). Interventions included digital (finger) compression, manual compression (heel of the hand), knee compression, compression by a 50lb kettlebell (Hampton Fitness Products, Ventura, CA), and medical device use (Combat Ready Clamp, CRoC, Combat Medical Systems, Fayetteville, NC; SAM Junctional Tourniquet, SAM, SAM Medical Products, Portland, OR; Junctional Emergency Treatment Tool, JETT, North American Rescue Products, Greer, SC; Abdominal Aortic Tourniquet, AAT, Compression Works, Hoover, AL). The first device assessed was the CRoC which, of the devices studied, was cleared first by the US Food and Drug Administration on August 11, 2010. The first setting of the evaluation (which was for the CRoC) was in a simulation center as previously reported with three to five people, and the other setting of the evaluation was on a table with one to three people [5]. The data from that initial setting is included here for comparison of time to stop bleeding, blood loss volume, and device efficacy [5]. Since the blood loss rate was non-linear (as it is in real situations for casualties because bleeding is brisker initially rather than later), we did not refill the bladder after each iteration. The manikin was not designed to differentiate between performance of devices, so we only compared results to acceptable benchmarks. The benchmark for time to stop bleeding was 300 seconds (s), and the benchmark for blood loss was a normal adult male blood volume, 5 L. Hemorrhage was controlled with 100% efficacy in the manikin model for each intervention. The times to stop bleeding and volumes of blood lost were acceptable for all devices and iterations (Figs. 1 and 2; Tables 1 and 2). Advantages and disadvantages were learned with experience in the use of each intervention (Table 3). Traits of interventions varied through wide ranges (Table 4).

N'oublions pas le packing de plaie
A manikin model for study of wound-packing interventions to control out-of-hospital hemorrhage
Kragh JF et Al. Am J Emerg Med. 2014 Sep;32(9):1130-1
To the Editor,
With hemorrhage being the primary cause of mortality on the battlefield [1-3], wound-packing practice by US military medics in the wars since September 11, 2001, has changed from a conservative to an assertive approach. The foremost emphasis changed from preventing contamination to controlling hemorrhage. As no specific hemostatic dressings were available at the start of the wars, after such dressings were fielded, medics changed their approach by packing wounds with more gauze earlier in casualty care and deeper into subfascial cavitary wounds as a way to control hemorrhage. Although experienced medics and trainers favor an assertive approach, there is limited empirical evidence of improvements. In addition, with the development of various dressings with hemostatic properties [4-6], no systematic approach to trial wound-packing techniques easily has been developed. When a war ends and military medical care shifts toward peacetime duties and garrison work, skill sets in trauma care degrade as skill performance is less often. Furthermore, peacetime training reverts back toward everyday work such as sick call and away from future combat casualty care. The reversion tendency allows less training of new medics in combat casualty care than those who were trained during busy years of sustained combat; like nothing in peacetime, the present danger of combat during wartime focuses attention on hemorrhage control. A challenge for medics to be as well trained in peacetime in combat casualty care as during wartime is a recurring theme of military medicine.
Of the medical advances in prehospital combat casualty care during the current wars, we feel that the most important are regular tourniquets, junctional tourniquets, and wound packing because of their potential capacity to save numerous casualties from the most common cause of death on the battlefield—wound exsanguination. To not backslide on these 3 skills, we continue scholarly work to refine them. We call these skills the “Big 3,” and we have published mostly on tourniquets. To stimulate development of best practices in wound packing, we now focus the present report on an introductory test method to increase awareness of knowledge gaps within the science of wound packing.
The purpose of the present study is to introduce a laboratory model of hemorrhage with data comparing gauze wound packing and medical device use to better understand out-of-hospital hemorrhage control. In an approved protocol, we used a manikin model designed for the capacity to train medics in techniques of gauze wound packing for hemorrhage control in trauma care. The manikin trainer (Combat Ready Clamp [CRoC] Trainer Manikin; Operative Experience, Inc, North East, MD) had a gunshot wound of the right groin that bled water from the common femoral artery; the wound track went through the thigh posterior to anterior. We measured blood volume lost from bleeding, the application time, and hemorrhage control (yes-no). We had only 1 user who had never packed a wound prehospital and had never been trained in this task. We made 4 tests. The first test was that we used a type of gauze (QuikClot Combat Gauze; Z-Medica, Wallingford, CT) alone in accordance with its instructions for use (IFU) except we used no overwrap for pressure; the overwrap is the fourth and final step of the gauze IFU. The second test was like the first, but we used the full IFU that included use of an overwrap (AirWrap, RevMedx, Wilsonville, OR). The third test was only the A manikin model for study of wound-packing interventions to control out-of-hospital hemorrhage
use of the overwrap and no gauze; this test included no inflation of the pneumatic bladder within the overwrap. The fourth test included the gauze, the overwrap, and the inflation of the overwrap. Each test had 4 replicates.
The results showed an apparent differential performance of the methods of hemorrhage control, but the test order indicated possible learning that may be a confounder. The fourth test performed better than the first 3 with respect to reduced blood loss (Fig. 1), which may mean that the fourth method is best or that the user learned with experience. Perhaps both are true. Application time also improved (Fig. 2), and the evaluation was sensitive enough to detect longer application times with additional steps in the wound-wrapping process.

There was no surprise that the gauze performed better as indicated by reduced blood loss (Fig. 1) when it was used fully in accordance with its IFU in that the second test performed better than the first. In addition, there was no surprise that the overwrap performed better when it was used fully in accordance with its intent in that the fourth test performed better than the third since the overwrap was designed to wrap over gauze.
The strength of this report is that it introduces a method of analyzing wound-packing techniques that generated hypotheses for testing. Hypothesis-driven experiments will follow this hypothesis generating report to check differential performance of techniques such as preliminarily studied here. The method permits learning curve analysis to see how fast users can be in hemorrhage control; we have previously found that tourniquet use, for example, appears to take more than 30 tests before users flatten their learning curve [7].
Determining optimal care techniques and training regimens may help to improve clinical performance. The limitation of the present report is its introductory design; the preliminary finding is only able to generate hypotheses. Future directions include analyses of techniques and learning curves.
John F. Kragh Jr., MD
US Army Institute of Surgical Research
Joint Base San Antonio
Fort Sam Houston, TX
Uniformed Services University of the Health Sciences
F. Edward Hébert School of Medicine Bethesda, MD
Corresponding author at: US Army Institute of Surgical Research
Damage Control Resuscitation, 3698 Chambers Pass
Ste B, Joint Base San Antonio
Fort Sam Houston, TX
E-mail address: john.f.kragh.civ@mail.mil
John Steinbaugh
RevMedx, Inc, Wilsonville, OR
Donald L. Parsons, PA-C
Combat Medic Training
US Army Medical Department Center and School
Joint Base San Antonio, Fort Sam Houston, TX
Robert L. Mabry, MD
Emergency Medical Services Fellowship
San Antonio Military Medical Center
Joint Base San Antonio
Fort Sam Houston, TX
Bijan S. Kheirabadi, PhD
Michael A. Dubick, PhD
Damage Control Resuscitation
US Army Institute of Surgical Research
Joint Base San Antonio
Fort Sam Houston, TX
| Tags : packing
31/10/2014
Garrot: Pas de jeu avant de serrer
No slackers in tourniquet use to stop bleeding
Polston RW et Al. J Spec Oper Med. 2013 Summer;13(2):12-9.
La performance d'un garrot tient pour beaucoup à la manière dont il va être posé. Le garrot en dotation comporte un dispositif de serrage de type tourniquet. L'efficacité de ce dispositif est en grande partie liée à l'absence de jeu au niveau de la sangle du garrot avant le serrage. Il est fondamental de positionner le garrot à la racine du membre, de le mettre en tension manuellement en tirant sur la sangle de façon à effectuer un premier serrage du garrot et ensuite de renforcer ce serrage par la barre du tourniquet. On rappelle qu'en principe l'efficacité est obtenue à partir de 3 tours. (la fiche technique). Le travail présenté ci après est éloquent sur l'intérêt de prohiber tout jeu avec de tourner la barre de torsion.
----------------------------------------------------------------------------------
Background: Tourniquets on casualties in war have been loose in 4%?9% of uses, and such slack risks death from uncontrolled bleeding. A tourniquet evidence gap persists if there is a mechanical slack?performance association.
Objective: The purpose of the present study was to determine the results of tourniquet use with slack in the strap versus no slack before windlass turning, in order to develop best practices. Methods: The authors used a tourniquet manikin 254 times to measure tourniquet effectiveness, windlass turns, time to stop bleeding, and blood volume lost at 5 degrees of strap slack (0mm, 25mm, 50mm, 100mm, and 200mm maximum).
Results: When comparing no slack (0mm) to slack (any positive amount), there were increases with slack in windlass turns (p < .0001, 3-fold), time to stop bleeding (p < .0001, 2-fold), and blood volume lost (p < .0001, 2-fold). When comparing no slack to 200mm slack, the median results showed an increase in slack for windlass turns (p < .0001), time to stop bleeding (p < .0001), and blood volume lost (p < .0001).
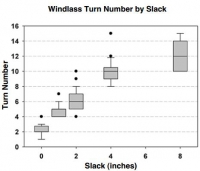
Conclusions: Any slack presence in the strap impaired tourniquet performance. More slack had worse results. Trainers can now instruct tourniquet users with concrete guidance.
| Tags : garrot, tourniquet
Garrot: Comment positionner la boucle ?
Emergency tourniquet effectiveness in four positions on the proximal thigh.
Kragh JF et Al. J Spec Oper Med. 2014 Spring;14(1):26-9.
La procédure du sauvetage au combat précise que le garrot doit être posé à la racine du membre. Elle ne précise cependant pas comment le dispositif de serrage doit être placé: en avant sur le côté en arrière du membre. Ce travail tente de répondre à cette question.
----------------------------------------------------------------------------------
Objective: The purpose of the present study is to determine the performance of tourniquet use by the placement of the tourniquet's windlass on the extremity in four positions: medial, lateral, anterior, and posterior? to inform tourniquet instructors and develop best tourniquet practices.
Methods: A HapMed™ Leg Tourniquet Trainer was used as a manikin to test the effectiveness of an emergency tourniquet, the Special Operations Forces Tactical Tourniquet. Two users made 10 tests, each in four positions.
Results: Effectiveness rates of tourniquet use were 100% in all four positions. The two tourniquet users were both right-hand dominant and used their right hand to turn the windlass. One user turned the windlass clockwise, and the other turned it counterclockwise. The association between time to stop bleeding and tourniquet position was statistically significant but associations between time to stop bleeding and the user, user-by-position, and windlass turn number were not statistically significant. The association between tourniquet position and pressure under the tourniquet was statistically significant, and the association between user and pressure under thetourniquet was statistically significant, but the user-by-position and windlass turn number were not statistically significant. The associations betweentourniquet position and blood loss volume, user and blood loss volume, and user-by-position and blood loss volume were statistically significant. Conclusions: The present study found that tourniquet effectiveness rates were uniformly 100% irrespective of whether the windlass position was medial, lateral, anterior, or posterior. These excellent clinical and statistical results indicate that users may continue to place the tourniquets as they prefer upon the proximal thigh
| Tags : tourniquet, garrot
Garrot jonctionnel: CROC et SAM ?
Testing of junctional tourniquets by military medics to control simulated groin hemorrhage.
Kragh JF et Al. J Spec Oper Med. 2014 Fall;14(3):58-63.
Ce qui est certain, c'est ce qui est écrit sur cette image
Difficile d'avoir une idée précise sur les performances relatives des matériels proposés par les industriels. Ce qui suit éclaire un peu.
BACKGROUND:
Junctional hemorrhage is a common cause of death on the battlefield, but there is no documented direct comparison for the use of junctional tourniquet models by US medics. The purpose of this testing is to assess military medic experience with the use of junctional tourniquets in simulated out-of-hospital trauma care.
METHODS:
Nine medics (seven men and two women) used four different junctional tourniquets: Combat Ready Clamp™ (CRoC™; http://www.combatmedicalsystems.com), Abdominal Aortic and Junctional Tourniquet™ (AAJT™; http://www.compressionworks.net), Junctional Emergency Treatment Tool (JETT™; http://www.narescue .com), and SAM Junctional Tourniquet® (SJT®; http:// www.sammedical.com/products). These medics also acted as simulated casualties. Effectiveness percentages, as measured by stopped distal pulse by Doppler auscultation, and time to effectiveness were recorded in two tests per tourniquet (72 total tests). Tourniquet users ranked their preference of model by answering the question: "If you had to go to war today and you could only choose one, which tourniquet would you choose to bring?"
RESULTS:
All tourniquets used were safe under the conditions of this study. Both the SJT and the CRoC had high effectiveness percentages; their rate difference was not statistically significant. The SJT and the CRoC had fast times to effectiveness; their time difference was not statistically significant. Users preferred the SJT and the CRoC; their ranked difference was not statistically significant.
CONCLUSION:
The SJT and the CRoC were equally effective and fast and were preferred by the participants
| Tags : jonctionnel
30/10/2014
Plaquettes synthétiques: Possible ? Mais oui
Tuning Ligand Density on Intravenous Hemostatic Nanoparticles Dramatically Increases Survival Following Blunt Trauma
Proc Natl Acad Sci U S A. 2014 Jul 15;111 (28) 10293-10298
Des plaquettes synthétiques pour arrêter le saignement ? Certains l'ont fait grâce à la technologie des nanoparticules (1, 2). Un espoir qui reste à confirmer.
-----------------------------------------------------------------------------------
Explosions account for 79% of combat-related injuries, leading to multiorgan hemorrhage and uncontrolled bleeding. Uncontrolled bleeding is the leading cause of death in battlefield traumas as well as in civilian life. We need to stop the bleeding quickly to save lives, but, shockingly, there are no treatments to stop internal bleeding. A therapy that halts bleeding in a site-specific manner and is safe, stable at room temperature, and easily administered is critical for the advancement of trauma care. To address this need, we have developed hemostatic nanoparticles that are administered intravenously. When tested in a model of blast trauma with multiorgan hemorrhaging, i.v. administration of the hemostatic nanoparticles led to a significant improvement in survival over the short term (1 h postblast). No complications from this treatment were apparent out to 3 wk. This work demonstrates that these particles have the potential to save lives and fundamentally change trauma care.
-----------------------------------------------------------------------------------
| Tags : hémorragie
23/10/2014
Pansements hémostatiques: Actualisation 2014
Review of New Topical Hemostatic Dressings for Combat Casualty Care
Benett BL et Al Mil Med. 2014 May;179(5):497-514
This review analyzes the new (2008-2013) hemostatic agents and dressings for enhanced efficacy in preclinical studies, and investigates supportive findings among case reports of effectiveness and safety in hospital and prehospital literature. A literature search was conducted using PubMed, National Library of Medicine using key words and phrases. The search revealed a total of 16 articles that fit the criteria established for third-generation hemostatic dressings. There were a total of 9 preclinical, 5 clinical, and 2 prehospital studies evaluated. Evaluation of these third- generation studies reveals that mucoadhesive (chitosan) dressings, particularly Celox Gauze and ChitoGauze, clearly show equal efficacy to Combat Gauze across many dependent variables. Chitosan-based products are ideal prehospital dressings because they are shown to work independently from the physiological clotting mechanisms. Many first-, second-, and third-generation chitosan-based dressings have been in use for years by the United States and other NATO militaries at the point of injury, and during tactical evacuation, in Operation Enduring Freedom and Operation Iraqi Freedom without reported complications or side effects. Based on the reported efficacy and long-term safety of chitosan-based products, increased use of Celox Gauze and ChitoGauze within the Department of Defense and civilian venues merits further consideration and open debate.
| Tags : hémorragie, pansement
14/09/2014
Plaie de l'abdomen: Comprimez avec le genou !
Abdominal aortic and iIiac artery compression following penetrating trauma: A study of feasibility
Douma et Al. Prehosp Disaster Med. 2014 Jun;29(3):299-302
Introduction
Penetrating junctional trauma is a leading cause of preventable death on the battlefield. Similarly challenging in civilian settings, exsanguination from the vessels of the abdomen, pelvis, and groin can occur in moments. Therefore, iliac artery or abdominal aortic compression has been recommended. Based on prior research, 120 lbs (54 kg) or 140 lbs (63 kg) of compression may be required to occlude these vessels, respectively. Whether most rescuers can generate this amount of compression is unknown.
Objective
To determine how many people in a convenience sample of 44 health care professionals can compress 120 lbs and 140 lbs.
Methods
This study simulated aortic and iliac artery compression. Consent was obtained from 44 clinicians (27 female; 17 male) from two large urban hospitals in Edmonton, Alberta, Canada. Participants compressed the abdominal model, which consisted of a medical scale and a 250 ml bag of saline, covered by a folded hospital blanket and placed on the ground. In random order, participants compressed a force they believed maintainable for 20 minutes (“maintainable effort”) and then a maximum force they could maintain for two minutes (“maximum effort”). Compression was also performed with a knee. Descriptive statistics were used to evaluate the data.
Results
Compression was directly proportional to the clinician's body weight. Participants compressed a mean of 55% of their body weight with two hands at a maintainable effort, and 69% at a maximum effort. At maintainable manual effort, participants compressed a mean of 86 lbs (39 kg). Sixteen percent could compress over 120 lbs, but none over 140 lbs. At maximum effort, participants compressed a mean of 108 lbs (48 kg). Thirty-four percent could compress greater than 120 lbs and 11% could compress greater than 140 lbs. Using a single knee, participants compressed a mean weight of 80% of their body weight with no difference between maintainable and maximum effort.
Conclusion
This work suggests that bimanual compression following penetrating junctional trauma is feasible. However, it is difficult, and is not likely achievable or sustainable by a majority of rescuers. Manual compression (used to temporize until device application and operative rescue) requires a large body mass. To maintain 140 lbs of compression (for example during a lengthy transport), participants needed to weigh 255 lbs (115 kg). Alternatively, they needed to weigh 203 lbs (92 kg) to be successful during brief periods. Knee compression may be preferable, especially for lower-weight rescuers.
| Tags : hémorragie
31/05/2014
Pansements hémostatiques: Utilité non démontrée
Haemostatic dressings in prehospital care
Hewitt Smith A. et Al. Emerg Med J 2013; 30:784–789
--------------------------------------------------------------
Une revue de littérature qui confirme que le bien fondé de l'emploi des pansements hémostatiques n'est pas si solide que cela. Pansement compressif et packing de plaie sont des valeurs sûres.
--------------------------------------------------------------
| Tags : pansement, hémorragie, massive bleeding control
14/04/2014
Tourniquet jonctionnel: Réflexions US
Management of Junctional Hemorrhage in Tactical Combat Casualty Care: TCCC Guidelines–Proposed Change 13-03
Kotwal RS et Al. J Spec Oper Med. 2013 Winter;13(4):85-93.
Clic sur l'image pour accéder au document
L'industrie nous propose des "garrots jonctionnels". Difficile de se faire une idée précise. Les US ont intégré le CRoC au TCCC. Cependant ce dispositif n'est pas si simple à monter. Cet article offre une lecture intéressante sur le sujet. Le tourniquet abdominal ne doit pas être appliqué plus d'une heure. Les autres le peuvent pour une durée maximum de 4 heures. Enfin le Sam Junctional Tourniquet est homologué par la FDA en tant que ceinture pelvienne.
| Tags : jonctionnel
07/04/2014
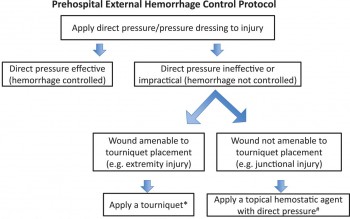
Le point sur le contrôle des hémorragies externes
An Evidence-based Prehospital Guideline for External Hemorrhage Control: American College of Surgeons Committee on Trauma
Bulger EM et Al. Prehosp Emerg Care. 2014 Apr-Jun;18(2):163-73.
Cet article fait le point à partir de données publiées sur les grands principes d'arrêt des hémorragies externes: Compression directe, garrot artériel en cas d'inefficacité, relatif faible niveau de preuves pour les pansements hémostatiques à utiliser néanmoins comme agent de packing de plaies, nécessité de poursuivre la recherche sur les dispositifs de compression jonctionnelle.
ATTENTION Il s'agit de préhospitalier CIVIL
Clic sur l'image pour accéder au document
| Tags : hémorragie, garrot