04/09/2016
Garrot: Mais l'occlusion dans le temps ?
Different Width and Tightening System: Emergency Tourniquets on Distal Limb Segments
BACKGROUND:
Tourniquets are used on distal limb segments. We examined calf and forearm use of four thigh-effective, commercial tourniquetswith different widths and tightening systems: 3.8 cm windlass Combat Application Tourniquet® (CAT, combattourrniquet.com) and Special Operations Forces® Tactical Tourniquet-Wide (SOFTTW, www.tacmedsolutions.com), 3.8 cm ratchet Ratcheting Medical Tourniquet - Pediatric (RMT-P, www.ratchetingbuckles. com), and 10.4 cm elastic Stretch-Wrap-And-Tuck Tourniquet® (SWATT, www.swattourniquet.com).
METHODS:
From Doppler-indicated occlusion, windlass completion was the next securing opportunity; ratchet completion was one additional tooth advance; elastic completion was end tucked under a wrap.
RESULTS:
All applications on the 16 recipients achieved occlusion. Circumferences were calf 38.1±2.5 cm and forearm 25.1±3.0 cm (p<.0001, t-test, mean±SD). Pressures at Occlusion, Completion, and 120-seconds after Completion differed within each design (p<.05, one-way ANOVA; calf: CAT 382±100, 510±108, 424±92 mmHg; SOFTT-W 381±81, 457±103, 407±88 mmHg; RMT-P 295±35, 350±38, 301±30 mmHg; SWATT 212±46, 294±59, 287±57 mmHg; forearm: CAT 301±100, 352±112, 310±98 mmHg; SOFTT-W 321±70, 397±102, 346±91 mmHg; RMT-P 237±48, 284±60, 256±51 mmHg; SWATT 181±34, 308±70, 302±70 mmHg). Comparing designs, pressures at each event differed (p<.05, one-way ANOVA), and the elastic design had the least pressure decrease over time (p<.05, one-way ANOVA). Occlusion losses differed among designs on the calf (p<.05, χ²; calf: CAT 1, SOFTT-W 5, RMT-P 1, SWATT 0; forearm: CAT 0, SOFTT-W 1, RMT-P 2, SWATT 0).
CONCLUSIONS:
All four designs can be effective on distal limb segments, the SWATT doing so with the lowest pressures and least pressure losses over time. The pressure change from Occlusion to Completion varies by tourniquet tightening system and can involve a pressure decrease with the windlass tightening systems. Pressure losses occur in as little as 120 seconds following Completion and so can loss of Occlusion. This is especially true for nonelastic strap tourniquet designs.
| Tags : tourniquet
2 garrots: Côte à côte SVP, mais attention
Pressures Under 3.8cm, 5.1cm, and Side-by-Side 3.8cm-Wide Tourniquets
-----------------------------
Plus un garrot est large et plus efficace il est. parmi les garrots en dotation le Garrot Delfi est le plus performant en terme d'occlusion. Néanmoins son emploi en première intention et hors un vecteur d'évacuation est difficilement envisageable. Aussi l'association de deux garrots apparaît elle très pertinente surtout si ces derniers sont posés côte à côte. Ce n'est pas pour autant une sécurité car en permettant l'obtention d'une pression d'occlusion plus basse, cette méthode expose à une occlusion insuffisante . Cette publication a par ailleurs comme intérêt de montrer que la pression d'occlusion baisse avec le temps et ce dès les premières minutes. Il est fondamental d'apprécier TRES régulièrement l'efficacité du garrot. Donc plutôt un garrot large d'emblée mais si l'on doit compléter poser le second à côté du premier. A noter que le garrot utilisé n'est pas en dotation dans l'armées US mais qu'il s'agit d'un des meilleurs garrots de dernière génération.
-----------------------------
BACKGROUND:
Applications of wider tourniquet are expected to occlude arterial flow at lower pressures. We examined pressures under 3.8cm-wide, 5.1cm-wide, and side-by-side-3.8cm-wide nonelastic strap-based tourniquets.
METHODS:
Ratcheting Medical Tourniquets (RMT) were applied mid-thigh and mid-arm for 120 seconds with Doppler-indicated occlusion. The RMTs were a Single Tactical RMT (3.8cm-wide), a Wide RMT (5.1cm-wide), and Paired Tactical RMTs (7.6cm-total width). Tightening completion was measured at one-tooth advance past arterial occlusion, and paired applications involved alternating tourniquet tightening.
RESULTS:
All 96 applications on the 16 recipients reached occlusion. Paired tourniquets had the lowest occlusion pressures (ρ < .05). All pressures are given as median mmHg, minimum-maximum mmHg. Thigh application occlusion pressures were Single 256, 219-299; Wide 259, 203-287; Distal of Pair 222, 183-256; and Proximal of Pair 184, 160-236. Arm application occlusion pressures were Single 230, 189-294; Wide 212, 161-258; Distal of Pair 204, 193-254, and Proximal of Pair 168, 148-227. Pressure increases with the final tooth advance were greater for the 2 teeth/cm Wide than for the 2.5 teeth/cm Tacticals (ρ < .05). Thigh final tooth advance pressure increases were Single 40, 33-49; Wide 51, 37-65; Distal of Pair 13, 1-35; and Proximal of Pair 15, 0-30. Arm final tooth advance pressure increases were Single 49, 41-71; Wide 63, 48-77; Distal of Pair 3, 0-14; and Proximal of Pair 23, 2-35. Pressure decreases occurred under all tourniquets over 120 seconds. Thigh pressure decreases were Single 41, 32-75; Wide 43, 28-62; Distal of Pair 25, 16-37; and Proximal of Pair 22, 15-37. Arm pressure decreases were Single 28, 21-43; Wide 26, 16-36; Distal of Pair 16, 12-35; and Proximal of Pair 12, 5-24. Occlusion losses before 120 seconds occurred predominantly on the thigh and with paired applications (ρ < .05). Occlusion losses occurred in six Paired thigh applications, two Single thigh applications, and one Paired arm application.
CONCLUSIONS:
Side-by-side tourniquets achieve occlusion at lower pressures than single tourniquets. Additionally, pressure decreases undertourniquets over time; so all tourniquet applications require reassessments for continued effectiveness.
| Tags : tourniquet
27/06/2016
Albumine 20% plutôt que fibrinogène ?
Influences of limited resuscitation with plasma or plasma protein solutions on hemostasis and survival of rabbits with noncompressible hemorrhage
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2016;81: 42–49
--------------------------------
Dans ce travail et alors que l'albumine diluée n'est pas recommandée, les auteurs évoquent la possibilité que les effets favorables d'une réanimation basée sur l'apport de plasma serait lié à l'apport de protéine et en particulier d'albumine qui aurait un effet tampon élevé, réduisant l'acidose métabolique, un des facteurs de la triade létale.
--------------------------------
BACKGROUND:
Plasma infusion with or without red blood cells is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
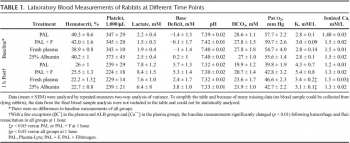
Anesthetized spontaneously breathing rabbits (3.3 ± 0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 minutes with Plasma-Lyte (PAL; 30 mL/kg), PAL + fibrinogen (PAL + F; 30 mL + 100 mg/kg), fresh rabbit plasma (15 mL/kg), or 25% albumin (ALB; 5 mL/kg) solution, all given in two bolus intravenous injections (15 minutes apart) to achieve a mean arterial pressure of 65 mm Hg, n = 8 to 9/group. Animals were monitored for 2 hours or until death, and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 minutes. At 60 minutes after injury, mean arterial pressure was higher with ALB than with crystalloids (PAL or PAL + F), but shock indices were not different despite the large differences in resuscitation volumes. Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein and increased survival rate to 100% (p < .05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSIONS:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate; however, its effects did not differ from those obtained with 25% ALB at one-third of the volume. The ALB advantage was consistent with our previous findings in which 5% ALB was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its ALB content rather than its coagulation proteins
| Tags : coagulopathie, remplissage
17/06/2016
Comprimez à distance: Avec le genou +++
Optimization of indirect pressure in order to temporize lifethreatening haemorrhage: a simulation study
Douma MJ et Al. http://dx.doi.org/10.1016/j.injury.2016.06.010
Background
Minimizing haemorrhage using direct pressure is intuitive and widely taught. In contrast, this study examines the use of indirect-pressure, specifically external aortic compression (EAC). Indirect pressure has great potential for temporizing bleeds not amenable to direct tamponade i.e. abdominal-pelvic, junctional, and multi-site trauma. However, it is currently unclear how to optimize this technique.
Methods
We designed a model of central vessel compression using the Malbrain intraabdominal pressure monitor and digital weigh scale. Forty participants performed simulated external aortic compression on the ground, on a stretcher mattress, and with and without a backboard.
Results
The greater the rescuer’s bodyweight the greater was their mean compression (Pearson’s correlation 0.93). Using one-hand, a mean of 28% participant bodyweight (95% CI, 26% - 30%) could be transmitted at sustainable effort, waist-height, and on a stretcher. A second compressing hand increased the percentage of rescuer bodyweight transmission 10-22% regardless of other factors (i.e. presence/absence or a backboard; rescuer position) (p <0.001). Adding a backboard increased transmission of rescuer bodyweight 7%-15% (p < 0.001). Lowering the patient from waist-height backboard to the floor increased transmission of rescuer bodyweight 4%-9% (p < 0.001). Kneeling on the model was the most efficient method and transmitted 11% more weight compared to two-handed maximal compression (p < 0.001).
Conclusions
Efficacy is maximized with larger-weight rescuers who use both hands, position themselves atop victims, and compress on hard surfaces/backboards. Knee compression is most effective and least fatiguing, thus assisting rescuers of lower weight and lesser strength, where no hard surfaces exist (i.e. no available backboard or trauma on soft ground), or when lengthy compression is required (i.e. remote locations). Our work quantifies methods to optimize indirect pressure as a temporizing measure following life-threatening haemorrhage not amenable to direct compression, and while expediting compression devices or definitive treatment.
04/06/2016
European guideline on management of major bleeding / Trauma
The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition
Rossaint et al. Critical Care (2016) 20:100
Background: Severe trauma continues to represent a global public health issue and mortality and morbidity in trauma patients remains substantial. A number of initiatives have aimed to provide guidance on the management of trauma patients. This document focuses on the management of major bleeding and coagulopathy following trauma and encourages adaptation of the guiding principles to each local situation and implementation within each institution.
Methods: The pan-European, multidisciplinary Task Force for Advanced Bleeding Care in Trauma was founded in 2004 and included representatives of six relevant European professional societies. The group used a structured, evidence-based consensus approach to address scientific queries that served as the basis for each recommendation and supporting rationale. Expert opinion and current clinical practice were also considered, particularly in areas in which randomised clinical trials have not or cannot be performed. Existing recommendations were reconsidered and revised based on new scientific evidence and observed shifts in clinical practice; new recommendations were formulated to reflect current clinical concerns and areas in which new research data have been generated. This guideline represents the fourth edition of a document first published in 2007 and updated in 2010 and 2013.
Results: The guideline now recommends that patients be transferred directly to an appropriate trauma treatment centre and encourages use of a restricted volume replacement strategy during initial resuscitation. Best-practice use of blood products during further resuscitation continues to evolve and should be guided by a goal-directed strategy. The identification and management of patients pre-treated with anticoagulant agents continues to pose a real challenge, despite accumulating experience and awareness. The present guideline should be viewed as an educational aid to improve and standardise the care of the bleeding trauma patients across Europe and beyond. This document may also serve as a basis for local implementation. Furthermore, local quality and safety management systems need to be established to specifically assess key measures of bleeding control and outcome.
Conclusions: A multidisciplinary approach and adherence to evidence-based guidance are key to improving patient outcomes. The implementation of locally
11/04/2016
PROPPR Study: 1-1-2 aussi bien !
Damage-control resuscitation and emergency laparotomy: Findings from the PROPPR study
Undurraga VJ et AL. J Trauma Acute Care Surg. 2016 Apr;80(4):568-75
BACKGROUND:
The Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) trial has demonstrated that damage-controlresuscitation, a massive transfusion strategy targeting a balanced delivery of plasma-platelet-red blood cell in a ratio of 1:1:1, results in improved survival at 3 hours and a reduction in deaths caused by exsanguination in the first 24 hours compared with a 1:1:2 ratio. In light of these findings, we hypothesized that patients receiving 1:1:1 ratio would have improved survival after emergency laparotomy.
METHODS:
Severely injured patients predicted to receive a massive transfusion admitted to 12 Level I North American trauma centers were randomized to 1:1:1 versus 1:1:2 as described in the PROPPR trial. From these patients, the subset that underwent an emergency laparotomy, defined previously in the literature as laparotomy within 90 minutes of arrival, were identified. We compared rates and timing of emergency laparotomyas well as postsurgical survival at 24 hours and 30 days.
RESULTS:
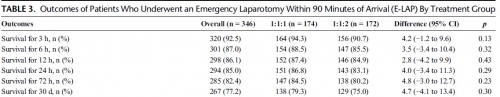
Of the 680 enrolled patients, 613 underwent a surgical procedure, 397 underwent a laparotomy, and 346 underwent an emergency laparotomy. The percentages of patients undergoing emergency laparotomy were 51.5% (174 of 338) and 50.3% (172 of 342) for 1:1:1 and 1:1:2, respectively (p = 0.20). Median time to laparotomy was 28 minutes in both treatment groups. Among patients undergoing an emergency laparotomy, the proportions of patients surviving to 24 hours and 30 days were similar between treatment arms; 24-hour survival was 86.8% (151 of 174) for 1:1:1 and 83.1% (143 of 172) for 1:1:2 (p = 0.29), and 30-day survival was 79.3% (138 of 174) for 1:1:1 and 75.0% (129 of 172) for 1:1:2 (p = 0.30).
CONCLUSION:
We found no evidence that resuscitation strategy affects whether a patient requires an emergency laparotomy, time to laparotomy, or subsequent survival.
| Tags : coagulopathie, transfusion
18/02/2016
Stabilisation pelvienne: Les genoux sont importants
Pelvic pressure changes after a fracture: A pilot cadaveric study assessing the effect of pelvic binders and limb bandaging
Morris R et Al. Injury http://dx.doi.org/10.1016/j.injury.2015.12.009
-------------------------
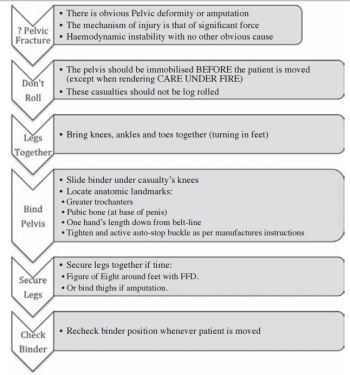
Stabiliser un bassin pour lequel il existe une suspicion de fracture est une des composantes majeures du sauvetage au combat. Ceci vise à réduire la mortalité par hémorragie non garrotable ou non comprimable. Il existe des ceintures spécifiques pour cela. Ce travail est intéressant car il illustre la complémentarité des ceintures pelviennes ET de l'immobilisation des genoux. Cette dernière permet à elle seule d'augmenter la pression intra-abdominale et partant probablement de réduire le saignement. Donc n'oublier pas d'immobiliser les genoux. Que vous disposez ou pas de ceinture pelvienne, cela sert.
-------------------------
Objectives: Pelvic binders are a life-saving intervention for hypovolaemic shock following displaced pelvic fractures, thought to act through increasing intra-pelvic pressure to reduce venous bleeding. This cadaveric study assesses changes in intra-pelvic pressure with different binders augmented by bandaging the thighs to recruit the femora as levers to close the pelvis. Access to femoral vessels via an in situ binder was also assessed.
Methods: Two embalmed cadavers were used with unstable pelvic injuries (OA/OTA 61-C1) created through disrupting the pelvic ring anteriorly and posteriorly. To measure intravesical pressure, which reflects intra-pelvic pressure, a supra-pubic catheter was inserted and connected to a water manometer whilst a spigot was placed in a urethral catheter to reduce leakage of fluid. The common and superficial femoral arteries were dissected in the left groin for each specimen prior to any intervention to allow inspection following binder application. A SAM pelvic sling II, Trauma Pelvic Orthotic Device (T-POD), Prometheus pelvic splint and an improvised pelvic binder were used on each cadaver, with each applied following lower limb bandaging with the knees slightly flexed. The groins were then inspected to assess if the femoral vessels were visible. Statistical analysis was performed in SPSS using a paired samples t test to determine if any difference existed between initial pelvic pressure in specimens compared to pressures with bandaging on and binders applied.
Results: Bandaging the lower limbs alone produced a significant increase in both peak and steady mean intra-pelvic pressure, 15.69 cmH2O and 12.38 cmH2O, respectively, compared to the baseline pressure, 8.73 cmH2O (p = 0.002 and p = 0.001, respectively). Applying the pelvic binder with the bandaging in place increased intra-pelvic pressure compared to the baseline (peak pressure of 25.38 cmH2O (p < 0.001) and steady pressure of 15.13 cmH2O (p = 0.003)). Steady mean pressures between bandaging alone and bandaging with the binder applied were not significantly different (p = 0.09), whilst the peak pressures were significantly greater when the binder was applied (p = 0.005). The improvised binder and T-POD both required cutting to access the femoral vessels which resulted in decreasing efficacy.
Conclusions: Intra-pelvic pressure was significantly increased through bandaging the lower limbs alone, and this represents a simple measure to increase intra-pelvic pressure and therefore efficacy of the binder. Access to the femoral vessels varied with binder type and represents an important consideration in polytrauma patients.
21/01/2016
Le graal plaquettaire hémostatique ?
Thrombosomes: a platelet-derived hemostatic agent for control of noncompressible hemorrhage
Fitzpatrick GM et Al. Transfusion. 2013 Jan;53 Suppl 1:100S-106S
----------------
Un thrombosome est en quelque sorte une plaquette lyophilisée dans laquelle l'eau est remplacée par un sucre particulier: le trehalose. Ré exposé à une atmosphère humide, il se réhydrate pour retrouver toutes ses propriétés. Cela ne semble pas être une simple théorie car il initierait une génération de thrombine permettant la formation d'un caillot de manière satisfaisante. Des thrombosmes, du fibrinogène et du PLyo, on peut espérer !
----------------
BACKGROUND: Uncontrolled hemorrhage is responsible for ~80% of the potentially survivable deaths in combat and over 40% of early mortality in the under 65 age group in the United States. Providing an easily used infusible hemostatic agent to first responders could significantly reduce these fatalities. We report on an infusible lyophilized platelet-derived hemostatic agent stabilized with trehalose and polysucrose prior to and during lyophilization.
STUDY DESIGN AND METHODS: Characterization included determining the particle population size range, surface marker expression GPIb, GPIIbIIIa, and Annexin V binding. Function was assessed by aggregation, thromboelastography, and thrombin generation. Pharmacokinetics, biodistribution, and immunogenicity established using Indium111 labeled Thrombosomes in healthy New Zealand white rabbits (NZWRs), efficacy in thrombocytopenic NZWR, and safety in NZWRs, canines, and nonhuman primates.
RESULTS: Thrombosomes retained GPIIbIIIa expression (98.71% 0.18 of the rehydrated particles), a reduced expression of GPIb (47.77% 6.65), and Annexin V binding (86.05% 2.65). Aggregation to all agonists except thrombin in buffer (78.15% 2.5) was <50%. Thrombin generation and thromboelastography results demonstrated a concentration gradient that was consistent from lot to lot. There were no observed adverse events in any safety study and blood loss was reduced by >80% in the thrombocytopenic ear bleed model.
CONCLUSION: Our in vitro characterization studies in conjunction with preclinical animal safety and efficacy studies demonstrated lot consistency in manufacturing, maintenance of hemostatic functions of Thrombosomes, safety at high dose concentrations, and the potential to provide an effective hemostatic agent at the site of injury.
09/01/2016
1/1/1 ou 1/1/2 ?
Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial
Holcomb JB et All. JAMA Surg. 2013 Feb;148(2):127-36
______________________________
La reconnaissance et la mise en place de la meilleure stratégie thérapeutique du choc hémorragique traumatique sont des enjeux fondamentaux qui se posent aux équipes de réanimation préhospitalières et hospitalières. L'application du concepts du damage control resuscitation (1) vise par la mise en place d'un stratégie raisonnée d'arrêt des hémorragies (2), d'un remplissage vasculaire mesuré (3) et d'une politique transfusionnelle spécifique (4). Parmi ces mesures, il apparaît important de garantir l'apport équilibré de plasma, de plaquettes et de CGR dans un ration élevé 1/1/1 ou 1/1/2. Deux études se sont attachées à ce point: L'étude PROMMTT et l'étude PROPPR ici présentée. La première confirme le bénéfice d'une telle stratégie avec une moindre mortalité chez les patients bénéficiant de rapport élevé supérieur mais uniquement dans les 6 premières heures. L'étude PROPPR semble confirmer ces données avec une moindre mortalité précoce par hémorragie mais ne réussit pas à confirmer l'intérêt d'un ratio 1/1/1 par rapport à un ratio 1/1/2 sur la mortalité à long terme.
______________________________
IMPORTANCE:
Severely injured patients experiencing hemorrhagic shock often require massive transfusion. Earlier transfusion with higher blood product ratios (plasma, platelets, and red blood cells), defined as damage control resuscitation, has been associated with improved outcomes; however, there have been no large multicenter clinical trials.
OBJECTIVE:
To determine the effectiveness and safety of transfusing patients with severe trauma and major bleeding using plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio.
DESIGN, SETTING, AND PARTICIPANTS:
Pragmatic, phase 3, multisite, randomized clinical trial of 680 severely injured patients who arrived at 1 of 12 level I trauma centers in North America directly from the scene and were predicted to require massive transfusion between August 2012 and December 2013.
INTERVENTIONS:
Blood product ratios of 1:1:1 (338 patients) vs 1:1:2 (342 patients) during active resuscitation in addition to all local standard-of-care interventions (uncontrolled).
MAIN OUTCOMES AND MEASURES:
Primary outcomes were 24-hour and 30-day all-cause mortality. Prespecified ancillary outcomes included time to hemostasis, blood product volumes transfused, complications, incidence of surgical procedures, and functional status.
RESULTS:
No significant differences were detected in mortality at 24 hours (12.7% in 1:1:1 group vs 17.0% in 1:1:2 group; difference, -4.2% [95% CI, -9.6% to 1.1%]; P = .12) or at 30 days (22.4% vs 26.1%, respectively; difference, -3.7% [95% CI, -10.2% to 2.7%]; P = .26). Exsanguination, which was the predominant cause of death within the first 24 hours, was significantly decreased in the 1:1:1 group (9.2% vs 14.6% in 1:1:2 group; difference, -5.4% [95% CI, -10.4% to -0.5%]; P = .03). More patients in the 1:1:1 group achieved hemostasis than in the 1:1:2 group (86% vs 78%, respectively; P = .006). Despite the 1:1:1 group receiving more plasma (median of 7 U vs 5 U, P < .001) and platelets (12 U vs 6 U, P < .001) and similar amounts of red blood cells (9 U) over the first 24 hours, no differences between the 2 groups were found for the 23 prespecified complications, including acute respiratory distress syndrome, multiple organ failure, venous thromboembolism, sepsis, and transfusion-related complications.
CONCLUSIONS AND RELEVANCE:
Among patients with severe trauma and major bleeding, early administration of plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio did not result in significant differences in mortality at 24 hours or at 30 days. However, more patients in the 1:1:1 group achieved hemostasis and fewer experienced death due to exsanguination by 24 hours. Even though there was an increased use of plasma and platelets transfused in the 1:1:1 group, no other safety differences were identified between the 2 groups.
| Tags : hémorragie
25/12/2015
Transfusion de CGR: Les + graves seulement
Red Blood Cell Transfusion and Mortality in Trauma Patients: Risk-Stratified Analysis of an Observational Study
Perel P et Al. PLoS Med. 2014 Jun 17;11(6):e1001664
-------------------------------------
Les données qui suivent sont extraites de la cohorte des patients inclus dans l'étude CRASH2. Cette réinterprétation des données a pour objectif d'analyser le lien entre la mortalité à 28 jours et la transfusion de CGR. Les auteurs retrouvent un effet délétère de la transfusion de CGR pour les patients les moins à risque de mortalité. Ceci est en faveur des démarches de stratégies transfusionnelles sinon restrictives du moins raisonnées en fonction du contexte notamment préhospitalier où cette pratique associée à l'apport de fractions coagulantes semble être d'un grand intérêt(1).
-------------------------------------
Background:
Haemorrhage is a common cause of death in trauma patients. Although transfusions are extensively used in the care of bleeding trauma patients, there is uncertainty about the balance of risks and benefits and how this balance depends on the baseline risk of death. Our objective was to evaluate the association of red blood cell (RBC) transfusion with mortality according to the predicted risk of death.
Methods and Findings:
A secondary analysis of the CRASH-2 trial (which originally evaluated the effect of tranexamic acid on mortality in trauma patients) was conducted. The trial included 20,127 trauma patients with significant bleeding from 274 hospitals in 40 countries. We evaluated the association of RBC transfusion with mortality in four strata of predicted risk of death: ,6%, 6%–20%, 21%–50%, and .50%. For this analysis the exposure considered was RBC transfusion, and the main outcome was death from all causes at 28 days. A total of 10,227 patients (50.8%) received at least one transfusion. We found strong evidence that the association of transfusion with all-cause mortality varied according to the predicted risk of death (p-value for interaction ,0.0001). Transfusion was associated with an increase in all-cause mortality among patients with , 6% and 6%–20% predicted risk of death (odds ratio [OR] 5.40, 95% CI 4.08–7.13, p,0.0001, and OR 2.31, 95% CI 1.96–2.73, p,0.0001, respectively), but with a decrease in all-cause mortality in patients with .50% predicted risk of death (OR 0.59, 95% CI 0.47–0.74, p,0.0001). Transfusion was associated with an increase in fatal and non-fatal vascular events (OR 2.58, 95% CI 2.05–3.24, p,0.0001). The risk associated with RBC transfusion was significantly increased for all the predicted risk of death categories, but the relative increase was higher for those with the lowest (,6%) predicted risk of death (p-value for interaction ,0.0001). As this was an observational study, the results could have been affected by different types of confounding. In addition, we could not consider haemoglobin in our analysis. In sensitivity analyses, excluding patients who died early; conducting propensity score analysis adjusting by use of platelets, fresh frozen plasma, and cryoprecipitate; and adjusting for country produced results that were similar.
Conclusions:
The association of transfusion with all-cause mortality appears to vary according to the predicted risk of death. Transfusion may reduce mortality in patients at high risk of death but increase mortality in those at low risk. The effect of transfusion in low-risk patients should be further tested in a randomised trial.
| Tags : hémorragie
22/12/2015
Tourniquet: Contrefaçons=Danger
Le regain d'intérêt pour la mise en place de garrot en cas d'hémorragie massive des membres ne doit pas faire oublier deux choses: Avoir appris correctement et utiliser un matériel adhoc.
Concernant ce dernier point apparaissent sur le marché nombre de garrots qui soit n'ont pas été validés soit sont des contrefaçons de ce dernier, soit des garrots proposés dans le cadre d'activité de type Softball.
Plutôt que d'utiliser un garrot de piêtre qualité, il vaut probablement mieux avoir recours à un garrot artisanal dont l'efficacité n'est pas remise en cause sous réserve d'une technique de pose maîtrisée.
On rappelle que les 3 seuls garrots validés par l'armée américaine sont le CAT, le SOFTT et le Delfi EMT. Les SEULS garrots en service dans l'armée française sont le SOFTT et le Delfi EMT. Ces garrots sont produits par des industriels au terme de travaux de recherche et de démarche d'évolution et de politique qualité aboutis, toutes démarches absentes chez les copieurs et les contrefacteurs.
Tous les autres garrots n'ont pas suivis les mêmes process de développement, ce qui ne permet pas de garantir ni leur efficacité dans le temps, ni leur fiabilité.
Un exemple de copie du SOFTT est ici présenté
Un point d'alerte majeur aux USA
| Tags : tourniquet
20/12/2015
Coagulopathie: Du fibrinogène avant tout
Trauma-induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs
Nardi G et al. Critical Care (2015) 19:83
------------------------------------
Le damage control resuscitation fait largement appel à l'apport de plasma, concentrés de globules rouges et de plaquettes dans un rapport de 1/1/1 (1). Malgré la relative correction de la coagulopathie la survie à long terme ne semble pas être améliorée (2). Aussi certains proposent d'avoir plutôt recours à l'administration précoce de fibrinogène plutôt que l'administration de plasma. Le travail suivant qui propose l'apport précoce de 2g de fibrinogène est en faveur d'une telle démarche.
------------------------------------
INTRODUCTION:
Hemorrhage is the principal cause of death in the first few hours following severe injury. Coagulopathy is a frequent complication of critical bleeding. A network of Italian trauma centers recently developed a protocol to prevent and treat trauma-induced coagulopathy. A pre-post cohort multicenter study was conducted to assess the impact of the early coagulation support (ECS) protocol on blood products consumption,mortality and treatment costs.
METHODS:
We prospectively collected data from all severely injured patients (Injury Severity Score (ISS) >15) admitted to two trauma centers in 2013 and compared these findings with the data for 2011. Patients transfused with at least 3 units of packed red blood cells (PRBCs) within 24 hours of an accident were included in the study. In 2011, patients with significant hemorrhaging were treated with early administration of plasma with the aim of achieving a high (≥1:2) plasma-to-PRBC ratio. In 2013, the ECS protocol was the treatment strategy. Outcome data, blood product consumption and treatment costs were compared between the two periods.
RESULTS:
The two groups were well matched for demographics, injury severity (ISS: 32.9 in 2011 versus 33.6 in 2013) and clinical and laboratory data on admission. In 2013, a 40% overall reduction in PRBCs was observed, together with a 65% reduction in plasma and a 52% reduction in platelets. Patients in the ECS group received fewer blood products: 6.51 units of PRBCs versus 8.14 units. Plasma transfusions decreased from 8.98 units to 4.21 units (P <0.05), and platelets fell from 4.14 units to 2.53 units (P <0.05). Mortality in 2013 was 13.5% versus 20% in 2011 (13 versus 26 hospital deaths, respectively) (nonsignificant). When costs for blood components, factors and point-of-care tests were compared, a €76,340 saving in 2013 versus 2011 (23%) was recorded.
CONCLUSIONS:
The introduction of the ECS protocol in two Italian trauma centers was associated with a marked reduction in blood product consumption, reaching statistical significance for plasma and platelets, and with a non-significant trend toward a reduction in early and 28-daymortality. The overall costs for transfusion and coagulation support (including point-of-care tests) decreased by 23% between 2011 and 2013.
| Tags : coagulopathie
19/12/2015
Amputé des jambes: Le bassin aussi !
The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices
Cross AM et Al. J R Nav Med Serv 2014;100(2):152-6
---------------------------------------------
Excepté l'extraction d'urgence de blessés sous le feu, la prise en charge den cas d'amputation traumatique doit inclure la forte probabilité de traumatisme du bassin. Une utilisation large des immobilisations pelviennes doit donc être à l'esprit. On rappelle simplement la gravité et la difficulté de prise en charge des hémorragies liées aux fractures de bassin.
---------------------------------------------
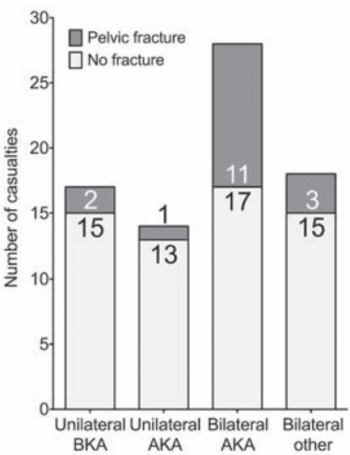
AIMS:
A frequently-seen injury pattern in current military experience is traumatic lower limb amputation as a result of improvised explosive devices (IEDs). This injury can coexist with fractures involving the pelvic ring. This study aims to assess the frequency of concomitant pelvic fracture in IED-related lower limb amputation.
METHODS:
A retrospective analysis of the trauma charts, medical notes, and digital imaging was undertaken for all patients arriving at the Emergency Department at the UK military field hospital in Camp Bastion, Afghanistan, with a traumatic lower limb amputation in the six months between September 2009 and April 2010, in order to determine the incidence of associated pelvic ring fractures.
RESULTS:
Of 77 consecutive patients with traumatic lower limb amputations, 17 (22%) had an associated pelvic fracture (eleven with displaced pelvic ring fractures, five undisplaced fractures and one acetabular fracture). Unilateral amputees (n = 31) had a 10% incidence of associated pelvic fracture, whilst 30 % of bilateral amputees (n = 46) had a concurrent pelvic fracture. However, in bilateral, trans-femoral amputations (n = 28) the incidence of pelvic fracture was 39%.
CONCLUSIONS:
The study demonstrates a high incidence of pelvic fractures in patients with traumatic lower limb amputations, supporting the routine pre-hospital application of pelvic binders in this patient group
| Tags : hémorragie, immobilisation, blast
17/12/2015
Tourniquet:Oui, mais bien posé= Serrer FORT
Evaluation of rapid training in ultrasound guided tourniquet application skills
Jaffer U. et Al. International Journal of Surgery 10 (2012) 563-567
-------------------------------------------------
Il existe actuellement un engouement justifié pour l'emploi du tourniquet comme moyen d'hémostase. Néanmoins il est important de rappeler que la pose d'un garrot a pour objectif l'arrêt d'un saignement important le plus souvent d'origine artérielle. Ils se doivent donc d'être serrés fort. Le travail proposé rappelle que la formation à la pose d'un garrôt n'est pas simplement sa manipulation mais qu'elle doit porter de manière spécifique sur les critères d'arrêt du saignement. En effet dans un modèle classique d'instruction de pose sur patient sain, les critères d'arrêt du serrage ne correspondent pas à ceux nécessaires en réel. Dans le travail proposé la pose à l'aveugle d'un garrot ne permet d'obtenir l'arrêt du saignement que dans moins d'1/4 à 1/5 des cas. Un enseignement donc à conduire par ceux qui en ont une pratique avancée. L'apport de simulateurs de saignement objectif comme celui du TOMMAN est certainement très intéressant.
Pour info: Fiche memento Garrot tactique
-------------------------------------------------
Tourniquet application has been widely accepted to improve survival for major limb trauma. Colour duplex ultrasound (US) can be used as a non-invasive method of confirming cessation of arterial flow. Participants with no or limited experience of ultrasound were taught to apply the Tourniquet with ultrasound guidance. Following this, participants were tested in effective tourniquet application: Blind and with ultrasound guidance. US guidance improved abolition of limb perfusion from 22 to 93 per cent in upper limb; from 25 to 100 per cent in lower limb (p ¼ 0.0027 and <0.0001).


Membre Sup Membre inf
No significant difference was found in application time for the lower limb; less time was taken for application with US guidance in the upper limb 8.1 (7.1, 8.6) vs 4.5 s (4.0, 5.3; median (IQR)), p ¼ 0.002. Tourniquet ultrasound skills are rapidly acquired by novice operators. Accuracy improves with ultrasound guidance, this may have a role in improving survival.
03/11/2015
Vers la machine à coaguler: Horizon 2040 ?
Deep Bleeder Acoustic Coagulation (DBAC)—part II: in vivo testing of a research prototype system
Sekins KM et Al. Sekins et al. Journal of Therapeutic Ultrasound (2015) 3:17
Background:
Deep Bleeder Acoustic Coagulation (DBAC) is an ultrasound image-guided high-intensity focused ultrasound (HIFU) method proposed to automatically detect and localize (D&L) and treat deep, bleeding, combat wounds in the limbs of soldiers. A prototype DBAC system consisting of an applicator and control unit was developed for testing on animals. To enhance control, and thus safety, of the ultimate human DBAC autonomous product system, a thermal coagulation strategy that minimized cavitation, boiling, and non-linear behaviors was used.
Material and methods:

The in vivo DBAC applicator design had four therapy tiles (Tx) and two 3D (volume) imaging probes (Ix) and was configured to be compatible with a porcine limb bleeder model developed in this research. The DBAC applicator was evaluated under quantitative test conditions (e.g., bleeder depths, flow rates, treatment time limits, and dose exposure time limits) in an in vivo study (final exam) comprising 12 bleeder treatments in three swine. To quantify blood flow rates, the “bleeder” targets were intact arterial branches, i.e., the superficial femoral artery (SFA) and a deep femoral artery (DFA). D&L identified, characterized, and targeted bleeders. The therapy sequence selected Tx arrays and determined the acoustic power and Tx beam steering, focus, and scan patterns. The user interface commands consisted of two buttons: “Start D&L” and “Start Therapy.” Targeting accuracy was assessed by necropsy and histologic exams and efficacy (vessel coagulative occlusion) by angiography and histology.
Results:
The D&L process (Part I article, J Ther Ultrasound, 2015 (this issue)) executed fully in all cases in under 5 min and targeting evaluation showed 11 of 12 thermal lesions centered on the correct vessel subsection, with minimal damage to adjacent structures. The automated therapy sequence also executed properly, with select manual steps. Because the dose exposure time limit (tdose ≤ 30 s) was associated with nonefficacious treatment, 60-s dosing and dual-dosing was also pursued. Thrombogenic evidence (blood clotting) and collagen denaturation (vessel shrinkage) were found in necropsy and histologically in all targeted SFAs. Acute SFA reductions in blood flow (20–30 %) were achieved in one subject, and one partial and one complete vessel occlusion were confirmed angiographically. The complete occlusion case was achieved with a dual dose (90 s total exposure) with focal intensity ≈500 W/cm2 (spatial average, temporal average).
23/10/2015
Quelle place pour les facteurs de la coagulation ?
| Tags : hémorragie, coagulopathie, choc
30/09/2015
REBOA: Un savoir faire à maîtriser ?
Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage
Moor LJ et Al. J Trauma Acute Care Surg. 2015;79: 523-532
L'application du concept du garrot tactique a fait évoluer la répartition des causes évitables de décès à l'avant et met actuellement au premier plan les hémorragies du tronc (Eastridge) . SI le bon usage du garrot reste un enjeu essentiel, les efforts portent maintenant sur la prise en charge d'une part des hémorragies jonctionnelles avec le recours de dispositifs tels que le CRoC, le Sam Junctional tourniquet ou l'abdominal tourniquet et d'autre part sur la prise en charge des hémorragies du tronc. Une autre approche, connue depuis de nombreuses années mais tombée en désuétude, refait surface. L'occlusion endovasculaire de l'aorte abdominale apparaît être d'un intérêt certain. C'est ce que documente le travail présenté ci dessous. Réaliser un tel geste en préhospitalier est possible (1,2). En ce qui concerne les applications militaires dans les structures chirurgicales de role 2 voire dans certaines moyens de transport préhospitalier une réflexion apparaît nécessaire.
------------------------------------------
BACKGROUND:
Hemorrhage remains the leading cause of death in trauma patients. Proximal aortic occlusion, usually performed by direct aortic cross-clamping via thoracotomy, can provide temporary hemodynamic stability, permitting definitive injury repair. Resuscitative endovascular balloon occlusion of the aorta (REBOA) uses a minimally invasive, transfemoral balloon catheter, which is rapidly inserted retrograde and inflated for aortic occlusion, and may control inflow and allow time for hemostasis. We compared resuscitative thoracotomy with aortic cross-clamping (RT) with REBOA in trauma patients in profound hemorrhagic shock.
METHODS: Trauma registry data was used to compare all patients undergoing RTor REBOA during an 18-month period from two Level 1 trauma centers.
RESULTS: There was no difference between RT (n = 72) and REBOA groups (n = 24) in terms of demographics, mechanism of injury, or Injury Severity Scores (ISSs). There was no difference in chest and abdominal Abbreviated Injury Scale (AIS) scores between the groups. However, the RT patients had lower extremity AIS score as compared with REBOA patients (1.5 [0-3] vs. 4 [3-4],p G 0.001). Of the 72 RT patients, 45 (62.5%) died in the emergency department, 6 (8.3%) died in the operating room, and 14 (19.4%) died in the intensive care unit. Of the 24 REBOA patients, 4 (16.6%) died in the emergency department, 3 (12.5%) died in the operating room, and 8 (33.3%) died in the intensive care unit. In comparing location of death between the RT and REBOA groups, there were a significantly higher number of deaths in the emergency department among the RT patients as compared with the REBOA patients (62.5% vs. 16.7%, p G 0.001). REBOA had fewer early deaths and improved overall survival as compared with RT (37.5% vs. 9.7%, p = 0.003).
CONCLUSION: REBOA is feasible and controls noncompressible truncal hemorrhage in trauma patients in profound shock. Patients undergoing REBOA have improved overall survival and fewer early deaths as compared with patients undergoing RT.
| Tags : junctionnel
18/07/2015
Tourniquet et chaleur extrême ?
Laboratory testing of emergency tourniquets exposed to prolonged heat
Davidson JP et Al. J Spec Oper Med. 2015 Spring;15(1):34-8.
----------------------------------------------------------
Il a été démontré que la fiabilité mécanique des tourniquets pouvait être altérée si ces derniers n'étaient pas protégés (1,2,3). Le travail présenté porte sur l'effet de l'exposition prolongée à de hautes températures sur l'efficacité des garrots. Apparemment il n'y aurait pas d'effet propre.
----------------------------------------------------------
BACKGROUND:
Environmental exposure of tourniquets has been associated with component damage rates, but the specific type of environmental exposure, such as heat, is unknown. Emergency-tourniquet damage has been associated with malfunction and loss of hemorrhage control, which may risk loss of life during first aid. The purposes of the study are to determine the damage rate of tourniquets exposed to heat and to compare the rate to that of controls.
METHODS:
Three tourniquet models (Combat Application Tourniquet®; SOF® Tactical Tourniquet; Ratcheting Medical Tourniquet®) were tested using a manikin (HapMed Leg Tourniquet Trainer; www.chisystems.com) that simulates extremity hemorrhage. The study group of 15 tourniquets (five devices per model, three models) was exposed to heat (oven at 54.4° C [130° F] for 91 days), and 15 tourniquets similarly constituted the control group (unexposed to heat). Damage, hemorrhage control, distal pulse stoppage, time to effectiveness, pressure (mmHg), and blood loss volumes were measured.
RESULTS:
Three tourniquets in both groups had damage not associated with heat exposure (p = 1). Heat exposure was not associated with change in effectiveness rates (p = .32); this lack of association applied to both hemorrhage control and pulse stoppage. When adjusted for the effects of user and model, the comparisons of time to effectiveness and total blood loss were statistically significant (p < .0001), but the comparison of pressure was not (p = .0613).
CONCLUSION:
Heat exposure was not associated with tourniquet damage, inability to gain hemorrhage control, or inability to stop the distal pulse.
| Tags : tourniquet
17/07/2015
Tourniquet: Une histoire de pression pas si simple
Tourniquets and Occlusion: The Pressure of Design
Wall PL et Al. Mil Med. 2013 May;178(5):578-87
-----------------------------------------------
Un travail très intéressant qui exprime bien que l'efficacité d'un garrot nécessite un ensemble de gestes parfaitement réalisés, notamment un serrage suffisant qui doit être vérifié après la pose. Il existe en effet avec les garrots de type tourniquet ou pneumatique une chute plus ou moins importante de la pression d'occlusion donc de perte d'occlusion, ce d'autant qu'un relâchement musculaire peut apparaître réduisant d'autant plus cette pression d'occlusion. Les garrots élastiques n'aurait pas cet inconvénient.
-----------------------------------------------
Abstracts: Nerve injuries result from tourniquet pressure. The objective was to determine arterial occlusion and completion pressures with the 3.8-cm-wide windlass Combat Application Tourniquet (CAT) and the 10.4-cm-wide Stretch, Wrap, and Tuck Tourniquet (SWAT-T).
Methods: Sixteen volunteers self-applied and had tourniquets applied to their thighs and arms (CAT and SWAT-T, random order, then blood pressure cuffs).
Results: Occlusion (Doppler signal elimination) pressures were higher than predicted ( p < 0.0001), highest with the CAT ( p < 0.0001), and often lower than completion pressures (completion median, range: CAT 360, 147–745 mm Hg; SWAT-T 290, 136–449 mm Hg; cuff 184, 108–281 mm Hg). Three CAT thigh and 9 CAT arm completion pressures were >500 mm Hg. Pressure decreases and occlusion losses occurred over 1 minute (pressure decrease: CAT 44 ± 33 mm Hg; SWAT-T 6 ± 8 mm Hg; cuff 14 ± 19 mm Hg; p < 0.0001; loss/initially occluded: CAT 17 of 61, SWAT-T 5 of 61, cuff 40 of 64, p < 0.01). CAT pressures before turn did not have a clear relationship with turns to occlusion.
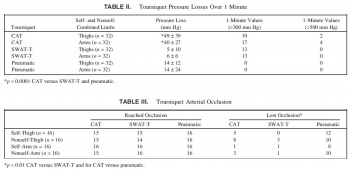 Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
| Tags : tourniquet
21/03/2015
Tourniquet: Efficace, uniquement si serré fort
Forward Assessment of 79 Prehospital Battlefield Tourniquet Use in the Current War
King DR et Al. J Spec Oper Med. 2012 Winter;12(4):33-8.
----------------------------------------------------------------------
La pose libérale d'un garrot est présentée comme étant un facteur essentiel de survie des blessés des membres. Encore faut il que ces derniers soient posés de manière correcte. Le document présenté laisse planer un gros doute. En effet il met en évidence qu'un garrot est mis en place 3 fois sur 4 alors qu'il n'y a pas de lésion vasculaire notable et que la plupart des garrots posés ne sont pas suffisamment serrés et sont en fait des garrots veineux. Pire seuls 1/3 des blessés ayant des lésions artérielles se voient appliquer un garrot artériel. C'est dire qu'une attention particulière doit être portée sur l'abolition du pouls artériel distal. Il s'agit là d'un enjeu pédagogique majeur.
----------------------------------------------------------------------
Introduction:
Battlefield tourniquet use can be lifesaving, but most reports are from hospitals with knowledge gaps remaining at the forward surgical team (FST). The quality of tourniquet applications in forward settings remain unknown. The purpose of this case series is to describe observations of tourniquet use at an FST in order to improve clinical performance.
Methods:
War casualties with tourniquet use presenting to an FST in Afghanistan in 2011 were observed. We identified appliers by training, device effectiveness, injury pattern, and clinical opportunities for improvement. Feedback was given to treating medics.
Results:
Tourniquet applications (79) were performed by special operations combat medics (47, 59%), flight medics (17, 22%), combat medics (12, 15%), and general surgeons (3, 4%). Most tourniquets were Combat Application Tourniquets (71/79, 90%). With tourniquets in place upon arrival at the FST, most limbs (83%, 54/65) had palpable distal pulses present; 17% were pulseless (11/65). Of all tourniquets, the use was venous in 83% and arterial in 17%. In total, there were 14 arterial injuries, but only 5 had effective arterial tourniquets applied.
Discussion:
Tourniquets are liberally applied to extremity injuries on the battlefield. 17% were arterial and 83% were venous tourniquets. When ongoing bleeding or distal pulses were appreciated, medics tightened tourniquets under surgeon supervision until distal pulses stopped. Medics were generally surprised at how tight a tourniquet must be to stop arterial flow–convert a venous tourniquet into an arterial tourniquet. Implications for sustainment training should be considered with regard to this life-saving skill.
| Tags : tourniquet, garrot, hémorragie