Une econférence qui fait parfaitement le point sur l'intérêt et les questions en suspens concernant l'intérêt du fibrinogène dans la réanimation hémostatique du traumasié qui saigne.
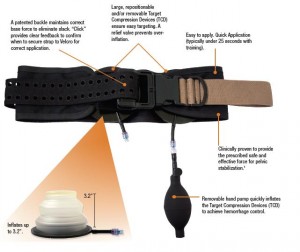
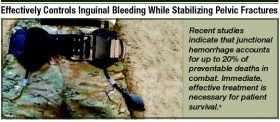
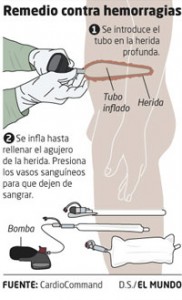
En condition de combat avant l'arivée en structure hopsitalière de campagne, l'apport de fibrinogène peut être réalisé par l'apport de plasma lyophylisé (PLYO) produit par le SSA (obtenu en moins de 6 min après reconstitution à température ambiante par adjonction d'eau PPI, chaque unité contient au moins 0,5g de fibrinogène). C'est une des composantes de la transfusion de plasma thérapeutique. qui doit désormais être envisagé au niveau du role 1 (poste de secours ou vecteur d'évacuation tactique).
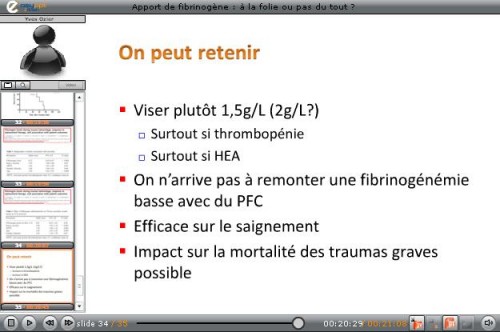
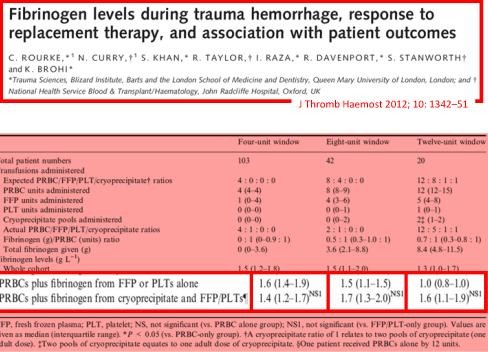
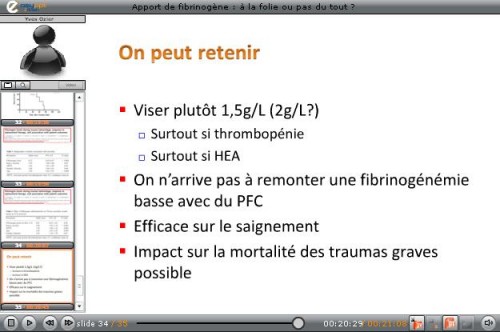
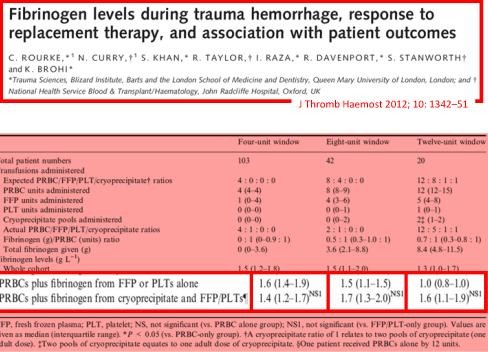
Le recours au fibrinogène (Clottafact), qui apparaît être d'un intérêt majeur compte tenu d'un apport insuffisant par la transfusion de plasma. (Abstract Rourke et all.)
Il ne peut (pour des raisons de logistique de production et de disponibilté) être apporté qu'à partir de la prise en charge hospitalière.
Pour approfondir avec en perspective le blessé de guerre hémorragique:
(1) Un revue générale sur la coagulopathie de l'hémorragie massive: "Hemodilution caused by trauma and major surgery induces complex hemostatic changes involving procoagulant factors as well as anticoagulant, fibrinolytic, and antifibrinolytic factors. The endothelial responses to shear stress, active proteases, and various inflammatory cells and cytokines add further complexity to the pathophysiology of massive hemodilution. In addition to the conventional transfusion products, which are often difficult to administer in a timely manner, purified factor concentrates of plasma origin and from recombinant synthesis are highly concentrated (i.e., small volume) for a rapid restoration of targeted factor(s). The use of point-of-care testing is desirable to optimize the dose and timing of such intervention. Additional clinical trials of different factor concentrate therapies are required to validate their efficacy and safety in patients after trauma or major surgery.152 Further understanding of the time course of pathophysiological changes in massive hemodilution is necessary to optimally balance hemostatic and anticoagulant therapies."
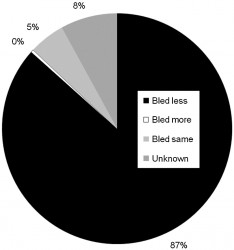
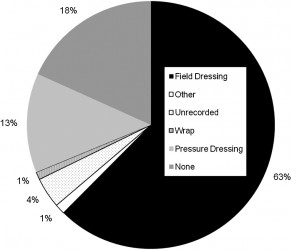
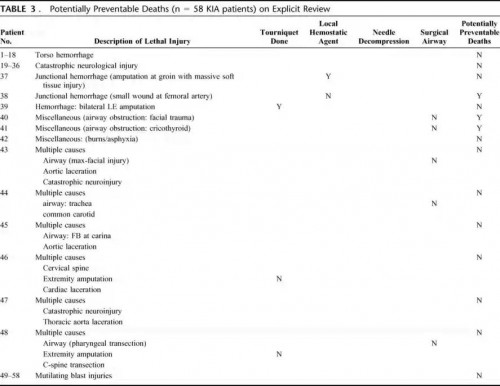
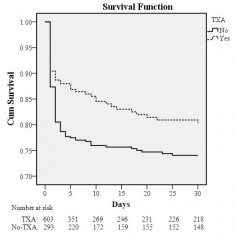
(2) Un focus sur le blessé de guerre: "In patients with combatrelated trauma requiring massive transfusion, the transfusion of an increased fibrinogen: RBC ratio was independently associated with improved survival to hospital discharge, primarily by decreasing death from hemorrhage. Prospective studies are needed to evaluate the best source of fibrinogen and the optimal empiric ratio of fibrinogen to RBCs in patients requiring massive transfusion."
(3) La stratégie transfusionnelle du blessé de guerre SFAR 2012: " En traumatologie, l’administration de fibrinogène est recommandée : dose initiale de 3 à 4 g suivie d’une administration régulière en cas d’hypofibrinogènémie biologique (<1,5 à 2 g/l) ou de signes thromboelastométriques de déficit fonctionnel en fibrinogène [8]. Une analyse nord-américaine rétrospective de 252 dossiers de BdG ayant nécessité une TM a permis de mettre en évidence qu’un apport faible de fibrinogène (< 0,2 g/CGR) au cours de la transfusion était associé à une majoration significative de la mortalité de ces blessés [39]. Le SSA américain utilise l’apport de cryoprécipités contenant surtout du fibrinogène et d’autres facteurs de coagulation pour compenser ces déficits [37]. Les recommandations du SSA français sont l’administration de fibrinogène de façon répétée afin de maintenir un fibrinogène plasmatique supérieur à 1,5 g/l ou en l’absence de laboratoire (situation des structures chirurgicales « légères »), d’administrer au moins 0,2 g de fibrinogène par CGR transfusé."