19/01/2023
Garrot: Moins de 2h OK mais pb après 4h
Impact of Time and Distance on Outcomes Following Tourniquet Use in Civilian and Military Settings: a Scoping Review
Joarder M et Al. https://doi.org/10.1016/j.injury.2023.01.031
Background: The last two decades have seen the reintroduction of tourniquets into guidelines for the management of acute limb trauma requiring haemorrhage control. Evidence supporting tourniquet application has demonstrated low complication rates in modern military settings involving rapid evacuation timeframes. It is unclear how these findings translate to patients who have prolonged transport times from injury in rural settings. This scoping review investigates the relationship between time and distance on metabolic complications, limb salvage and mortality following tourniquet use in civilian and military settings.
Methods: A systematic search strategy was conducted using PubMed, Embase, and SafetyLit databases. Study characteristics, setting, mechanism of injury, prehospital time, tourniquet time, distance, limb salvage, metabolic response, mortality, and tourniquet removal details were extracted from eligible studies. Descriptive statistics were recorded, and studies were grouped by ischemia time (< 2 hours, 2-4 hours, or > 4 hours).
Results: The search identified 3103 studies, from which 86 of studies were included in this scoping review. Of 86 studies, 55 studies were primarily civilian environments and 32 were based in military settings. One study included both settings. Blast injury was the most common mechanism of injury sustained by patients in military settings (72.8% [5968/8200]) followed by penetrating injury (23.5% [1926/8200]). In contrast, in civilian settings penetrating injury was the most common mechanism (47.7% [1633/3426]) followed by blunt injury (36.4% [1246/3426]).
Tourniquet time was reported in 66/86 studies. Tourniquet time over four hours was associated with reduced limb salvage rates (57.1%) and higher mortality rates (7.1%) compared with a tourniquet time of less than two hours. The overall limb salvage and mortality rates were 69.6% and 6.7% respectively. Metabolic outcomes were reported in 28/86 studies with smaller sample sizes and inconsistencies in which parameters were reported.
Conclusion: This scoping review presents literature describing comparatively safe tourniquet application when used for less than two hours duration. However, there is limited research describing prolonged tourniquet application or when used for protracted distances, such that the impact of tourniquet release time on metabolic outcomes and complications remains unclear. Prospective studies utilising the development of an international database to provide this dataset is required.
| Tags : tourniquet
25/11/2022
Point sur les matériaux hémostatiques
Emerging hemostatic materials for non-compressible hemorrhage control
Dong R. et Al. ,Natl Sci Rev. 2022 Aug 17;9(11):nwac162.
Non-compressible hemorrhage control is a big challenge in both civilian life and the battlefield, causing a majority of deaths among all traumatic injury mortalities. Unexpected non-compressible bleeding not only happens in pre-hospital situations but also leads to a high risk of death during surgical processes throughout in-hospital treatment. Hemostatic materials for pre-hospital treatment or surgical procedures for non-compressible hemorrhage control have drawn more and more attention in recent years and several commercialized products have been developed. However, these products have all shown non-negligible limitations and researchers are focusing on developing more effective hemostatic materials for non-compressible hemorrhage control. Different hemostatic strategies (physical, chemical and biological) have been proposed and different forms (sponges/foams, sealants/adhesives, microparticles/powders and platelet mimics) of hemostatic materials have been developed based on these strategies. A summary of the requirements, state-of-the-art studies and commercial products of non-compressible hemorrhage-control materials is provided in this review with particular attention on the advantages and limitations of their emerging forms, to give a clear understanding of the progress that has been made in this area and the promising directions for future generations.
04/10/2022
Pansement hémostatique et altitude: C'est OK
Hemostatic Effects of Bio-Zeolite Gauze and QuikClot Combat Gauze on Major Bleeding in Rabbits Acutely Exposed to High Altitude
Yi-jun J et Al. Prehosp Emerg Care. 2022 Sep 28;1-8
Objective:
Hemostatic gauze application is an effective way to control major bleeding, which is the most common cause of death in trauma in both civilian and military settings. Coagulation derangement after acute exposure to high altitude might alter the effects of hemostatic gauzes. The present study aimed to observe the hemostatic effects of bio-zeolite gauze (BZG) and QuikClot Combat Gauze® (QCG) on major bleeding in rabbits acutely exposed to high altitude.
Methods:
Sixty rabbits were randomly and evenly divided into six groups. Animal models of simulated blast- and fragment-induced inguinal major bleeding were prepared in lower altitude and high-altitude areas, and BZG, QCG, and ordinary gauze without hemostatic material were used to control bleeding. The primary outcomes included immediate hemostasis rate, blood loss, and survival rate, while the secondary outcomes included hemodynamic parameters, laboratory examinations, and coagulation-relevant markers.
Results:
The overall effects of BZG and QCG were better than those of ordinary gauze, with a higher immediate hemostatic rate, less blood loss, and higher survival rate at 90 min after gauze application and higher red blood cell and platelet counts and lower creatinine level at 30 min after gauze application in lower altitude. The concentrations of coagulation factor XII and factor X in rabbits acutely exposed to high altitude were significantly lower than those in lower altitude. At high altitude, the hemostatic effects of BZG did not decrease significantly compared to those in the lower altitude, whereas those of ordinary gauze and QCG decreased significantly at high altitude compared to those in the lower altitude.
Conclusions:
Coagulation derangement after acute exposure to high altitude has negative effects on ordinary gauze and QCG but has no significant negative hemostatic effects on BZG.
05/12/2021
Garrot abdominal: A bien regarder !!!!
Abdominal Aortic Junctional Tourniquet - Stabilized (AAJTS) can be applied both successfully and rapidly by Combat Medical Technicians (CMTs)
Smith TM et Al. BMJ Mil Health. 2021 Nov 30;e001881.
-----------------------------------------
On parle beaucoup du REBOA, mais ce dispositif est une alternative certainement plus simple à mettre en oeuvre
-----------------------------------------
Background
‘Non-compressible’ haemorrhage is the leading cause of preventable battlefield death, often requiring surgical or radiological intervention, which is precluded in the pre-hospital environment. One-fifth of such bleeds are junctional and therefore potentially survivable. We examine the use of the Abdominal Aortic Junctional Tourniquet - Stabilized (AAJTS) among UK Combat Medical Technicians (CMTs) as a device to control junctional haemorrhage with external compression of the abdominal aorta—compression of junctional haemorrhage previously considered ‘non-compressible.’ This follows animal studies showing that the AAJTS achieves control of haemorrhage and improves physiological parameters.
Methods
CMTs were selected and applied the AAJTS to each other following a 1-hour training package. A consultant radiologist-operated hand-held ultrasound monitored flow changes in the subjects’ common femoral artery. CMTs were then surveyed for their opinions as to utility and function.
Results
21 CMTs were screened and 17 CMTs participated with 34 total applications (16 day and 18 low-light). 27/34 (79%) achieved a successful application. The median application time was 75 s in daylight and 57 s in low-light conditions. There was no significant difference in Body Mass Index (p=0.23), median systolic blood pressure (p=0.19), nor class of CMT (p=0.10) between successful and unsuccessful applications. Higher systolic blood pressure was associated with longer application times (p=0.03). Users deemed the device easy to use (median score 4.4 on a 5-point Likert scale).
Conclusion
CMTs can use AAJTS successfully after a 1-hour training session in the majority of applications. Application was successful in both daylight and low-light conditions. Self-reported usability ratings were high.
16/11/2021
PLP: A ne pas mettre au rebus !
Contemporary utility of diagnostic peritoneal aspiration in trauma
Morgan Schellenberg M et Al. J Trauma Acute Care Surg. 2021 Nov 1;91(5):814-819.
Background: Focused Assessment with Sonography for Trauma (FAST) has supplanted diagnostic peritoneal lavage (DPL) as the preferred bedside evaluation for traumatic hemoperitoneum. Diagnostic peritoneal aspiration (DPA) is a simpler, faster modification of DPL with an unclear role in contemporary practice. This study delineated modern roles for DPA and defined its diagnostic yield.
Methods: All trauma patients presenting to our Level I center who underwent DPA were included (May 2015 to May 2020). Demographics, comorbidities, clinical/injury data, and outcomes were collected. The diagnostic yield and accuracy of DPA were calculated against the criterion standard of hemoperitoneum at exploratory laparotomy or computed tomography scan.
Results: In total, 41 patients underwent DPA, typically after blunt trauma (n = 37, 90%). Patients were almost exclusively hypotensive (n = 20, 49%) or in arrest (n = 18, 44%). Most patients had an equivocal or negative FAST and hypotension or return of spontaneous circulation after resuscitative thoracotomy (n = 32, 78%); or had a positive FAST and known cirrhosis (n = 4, 10%). In two (5%) patients, one obese, the catheter failed to access the peritoneal cavity. Diagnostic peritoneal aspiration sensitivity, specificity, positive predictive value, and negative predictive value were 80%, 100%, 100%, and 90%, with an accuracy of 93%. One (2%) complication, a small bowel injury, occurred.
Conclusion: Despite near ubiquitous FAST availability, DPA remains important in diagnosing or excluding hemoperitoneum with exceedingly low rates of failure and complications. Diagnostic peritoneal aspiration is most conclusive when positive, without false positives in this study. Diagnostic peritoneal aspiration was most used among blunt hypotensive or postarrest patients who had an equivocal or negative FAST, in whom the preliminary diagnosis of hemoperitoneum is a critically important decision making branch point.
25/09/2021
Olaes Bandage: En mieux
06/02/2021
Sonde Foley: CH 14 et 15 ml
Foley catheter action in the nasopharynx: a cadaveric study
Objectives:
To determine the action of the Foley catheter in the posterior nasal cavity in relation to balloon volume, and to deduce its implications in the treatment of posterior epistaxis.
Design:
Human cadaveric study.
Materials:
Twenty nasal fossae of 10 adult cadavers.
Interventions:
A Foley catheter (size 14) was inserted into the nasopharynx via each nostril. The catheter balloon was inflated to its recommended maximum volume with 15 mL of water. Firm traction was applied to the catheter. Colored liquid was instilled into the ipsilateral aspect of the nasal cavity, and liquid leakage into the contralateral side was monitored using a nasoendoscope. The balloon was reduced in volume by 1-mL steps, and the same fluid infusion and documentation procedures were performed for each reduced volume until the balloon slipped out of the nose. The procedure was repeated in the opposite nostril.

Main outcome measures:
Successful choanal sealing and anterior balloon shift into the nasal fossa in relation to the balloon size.
Results:
The Foley catheter balloon sealed the choana without any leakage of infused liquid into the contralateral side at appropriate inflation volumes in 17 (85%) of 20 nasal fossae. Complete sealing between volumes of 12 and 15 mL was achieved in 13 fossae (65%), between 11 and 15 mL in 10 nasal fossae (50%), and between 5 and 15 mL in 3 nasal fossae (15%). Failure to seal at any volume occurred in 3 nasal fossae (15%). Bimodal seal (ie, complete seal at high [15 mL] and low volumes [4-7 mL], but leakage in intermediate volumes) occurred in 3 nasal fossae (15%). The balloon remained in the nasopharynx under traction and did not slip past the choanal rim to encroach on the middle and inferior turbinates until the balloon volume was reduced to between 4 and 7 mL. The balloon slid out of the nose at a volume of 5 mL or less. The inflation volumes ranging from 8 to 12 mL were statistically more effective in sealing the choana than lower volumes (4-7 mL) (P<.002, chi(2) test).
Conclusions:
At different inflation volumes, the Foley catheter balloon acts primarily (1) as a platform for an anterior gauze pack (at 4-15 mL); (2) as an effective seal of the choana (at 8-15 mL usually and at 4-7 mL occasionally); and (3) as a compressor of the region behind the middle and inferior turbinates (at 4-7 mL), provided that the balloon under traction does not slip out of the nose.
02/02/2021
TXA: Oui, mais parfois pas nécessaire
Unjustified Administration in Liberal Use of Tranexamic Acid in Trauma Resuscitation
Tareq Kheirbek T et Al. J Surg Res . 2021 Feb;258:125-131. doi: 10.1016/j.jss.2020.08.045.
Background:
Early administration of tranexamic acid (TXA) has been widely implemented for the treatment of presumed hyperfibrinolysis in hemorrhagic shock. We aimed to characterize the liberal use of TXA and whether unjustified administration was associated with increased venous thrombotic events (VTEs).
Methods:
We identified injured patients who received TXA between January 2016 and January 2018 by querying our Level 1 trauma center's registry. We retrospectively reviewed medical records and radiologic images to classify whether patients had a hemorrhagic injury that would have benefited from TXA (justified) or not (unjustified).
Results:
Ninety-five patients received TXA for traumatic injuries, 42.1% were given by emergency medical services. TXA was considered unjustified in 35.8% of the patients retrospectively and in 52% of the patients when given by emergency medical services. Compared with unjustified administration, patients in the justified group were younger (47.6 versus 58.4; P = 0.02), more hypotensive in the field (systolic blood pressure: 107 ± 31 versus 137 ± 32 mm Hg; P < 0.001) and in the emergency department (systolic blood pressure: 97 ± 27 versus 128 ± 27; P < 0.001), and more tachycardic in emergency department (heart rate: 99 ± 29 versus 88 ± 19; P = 0.04). The justified group also had higher injury severity score (median 24 versus 11; P < 0.001), was transfused more often (81.7% versus 20.6%; P < 0.001), and had higher in-hospital mortality (39.3% versus 2.9%; P < 0.001), but there was no difference in the rate of VTE (8.2% versus 5.9%).
Conclusions:
Our results highlight a high rate of unjustified administration, especially in the prehospital setting. Hypotension and tachycardia were indications of correct use. Although we did not observe a difference in VTE rates between the groups, though, our study was underpowered to detect a difference. Cautious implementation of TXA in resuscitation protocols is encouraged in the meantime. Nonetheless, adverse events associated with unjustified TXA administration should be further evaluated
22/10/2020
Albumine: Le retour ?
Should Albumin be Considered for Prehospital Resuscitation in Austere Environments? A Prospective Randomized Survival Study in Rabbits
Kheirabadi BS et Al. Shock . 2020 Sep;54(3):358-367.
--------------------------------
Le remplissage vasculaire par albumine diluée n'est pas spécialement recommandé. Pourtant il semblerait que cela soit à tort dans certains environnements. C'est du moins ce que laisse penser ce travail expérimental chez le lapin.
--------------------------------
Background:
The new guidelines for prehospital care of combat casualties in shock recommend administration of whole blood or blood components to increase blood pressure to a permissible hypotensive level (i.e., hypotensive resuscitation [HR]). We investigated if 2 h of HR using limited volumes of whole blood, plasma, or albumin would lead to full recovery and long-term survival of rabbits subjected to severe hemorrhagic shock (HS).
Methods:
Following instrumentation, laparotomy was performed on IV-anesthetized spontaneously breathing New Zealand white rabbits (3.0 kg -3.5 kg). Next, ∼40% of rabbits' blood volume was removed producing HS (mean arterial pressure [MAP]∼20 mm Hg). Fifteen minutes later, rabbits were resuscitated with a limited volume (12.5 mL/kg) of rabbit whole blood (fresh whole blood [FWB]), rabbit fresh frozen plasma (FFP), or 5% human albumin (ALB) to a target pressure (MAP) of 60 mm Hg (n=8/grp) and monitored for 2 h. Liver bleeding time was measured at baseline and 10 min after HR. Subsequently, animals were fully resuscitated (blood + lactated Ringer [LR]), surgically repaired, and recovered for 8 days. An untreated group (n = 6) was also included.
Results:
Following HS, lactate and base deficit levels were increased to 8.2 ± 1.6 and 12.9 ± 3.1 mM respectively with no difference among groups. A lower volume of FWB volume was required to reach the target MAP (P < 0.05 vs. ALB) but MAP declined during the HR period (P < 0.01 vs. ALB).
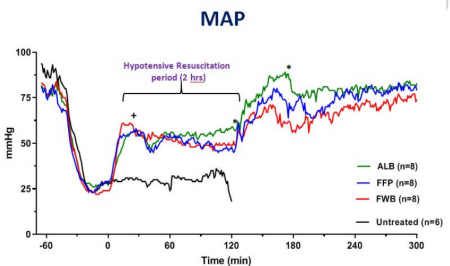
FWB provided higher hematocrit and platelets but it did not reduce lactate level faster than other fluids. Beside higher fibrinogen, no differences were found in hemostatic or resuscitative effects of FFP versus ALB. Bleeding time was prolonged with ALB and FFP fluids but unchanged with FWB. Untreated rabbits died during shock or shortly after. All treated rabbits except one recovered and lived for 8 days with normal blood tests and similar tissue histology.
Conclusions:
Two hours of HR using a limited volume of FWB, FFP, or ALB led to full recovery and long-term survival of rabbits subjected to HS. Apart from bleeding time, no clinically significant differences were found among the three fluids. Five percent human albumin solutions are isotonic, iso-oncotic, ready-to-use, stable, and compatible with all blood types and should be considered for prehospital resuscitation where blood products are not available or not accepted.
| Tags : remplissage
16/08/2020
Conversion de garrot: Le concept Tourniquet +1
Tourniquet Conversion. A Recommended Approach in the Prolonged Field Care Setting
Brendon D. et Al. J Spec Oper Med . Fall 2015;15(3):81-5.
-----------------------------
Les auteurs de ce document proposent le concept du tourniquet +1 lors de la réévaluation d'un garrot posé en contexte tactique. Ceja consiste à oser un second garrot au dessous du premier avant de desserrer le premier garrot. Ils s'appuie sur la fréquence d'après eux de rupture de garrot lors de cette manoeuvre. Cette manoeuvre est à proscrire si le garrot est en place depuis plus de 6 heures. Elle est systématique si ce dernier est en place depuis moins de 2 heures. Entre les deux elle peut être réalisée. Leurs recommandations ne sont pas très claires.
-----------------------------
Life-saving interventions take precedence over diagnostic maneuvers in the Care Under Fire stage of Tactical Combat Casualty Care. The immediate threat to life with an actively hemorrhaging extremity injury is addressed with the liberal and proper use of tourniquets. The emphasis on hemorrhage control has and will continue to result in the application of tourniquets that may not be needed past the Care Under Fire stage. As soon as tactically allowable, all tourniquets must be reassessed for conversion. Reassessment of all tourniquets should occur as soon as the tactical situation permits, but no more than 2 hours after initial placement. This article describes a procedure for qualified and trained medical personnel to safely convert extremity tourniquets to local wound dressings, using a systematic process in the field setting.
| Tags : tourniquet
18/07/2020
Arrêter un saignement de langue
Use of an improvised clamp to manage bleeding tongue injuries,
Chen M.W.J. et Al. Am J Emergency Medicine (2020), https://doi.org/10.1016/j.ajem.2020.06.051
Compresses éventuellement hémostatiques, deux abaisses langues, du sparadrap. Et voilà la langue est comprimée.
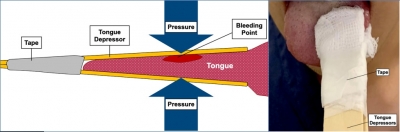
| Tags : hémorragie
03/01/2020
Hydroxocobalamine pour l'hémorragie aussi ?
Intravenous Hydroxocobalamin Versus Hextend Versus Control for Class III Hemorrhage Resuscitation in a Prehospital Swine Model.
Background:
Hydroxyethyl starch (Hextend) has been used for hemorrhagic shock resuscitation, however, hydroxyethyl starch may be associated with adverse outcomes.
Objective:
To compare systolic blood pressure (sBP) in animals that had 30% of their blood volume removed and treated with intravenous hydroxocobalamin, hydroxyethyl starch, or no fluid.
Methods:
Twenty-eight swine (45-55 kg) were anesthetized and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged 20 mL/kg over 20 minutes and then administered 150 mg/kg IV hydroxocobalamin in 180 mL saline, 500 mL hydroxyethyl starch, or no fluid and monitored for 60 minutes. Data were modeled using repeated measures multivariate analysis of variance.
Results:
There were no significant differences before treatment. At 20 minutes after hemorrhage, there was no significant difference in mean sBP between treated groups, however, control animals displayed significantly lower mean sBP (p < 0.001). Mean arterial pressure and heart rate improved in the treated groups but not in the control group (p < 0.02). Prothrombin time was longer and platelet counts were lower in the Hextend group (p < 0.05). Moreover, thromboelastography analysis showed longer clotting (K) times (p < 0.05) for the hydroxyethyl starch-treated group.
Conclusion:
Hydroxocobalamin restored blood pressure more effectively than no treatment and as effectively as hydroxyethyl starch but did not adversely affect coagulation.
IT Clamp: Pas si bien que cela ?
External Soft-Tissue Hemostatic Clamp Compared to a Compression Tourniquet as Primary Hemorrhage Control Device in Pilot Flow Model Study.
Acute blood loss represents a leading cause of death in both civilian and battlefield trauma, despite the prioritization of massive hemorrhage control by well-adopted trauma guidelines. Current Tactical Combat Casualty Care (TCCC) and Tactical Emergency Casualty Care (TECC) guidelines recommend the application of a tourniquet to treat life-threatening extremity hemorrhages. While extremely effective at controlling blood loss, the proper application of a tourniquet is associated with severe pain and could lead to transient loss of limb function impeding the ability to self-extricate or effectively employ weapons systems. As a potential alternative, Innovative Trauma Care (San Antonio, Texas USA) has developed an external soft-tissue hemostatic clamp that could potentially provide effective hemorrhage control without the aforementioned complications and loss of limb function. Thus, this study sought to investigate the effectiveness of blood loss control by an external soft-tissue hemostatic clamp versus a compression tourniquet.
HYPOTHESIS:
The external soft-tissue hemostatic clamp would be non-inferior at controlling intravascular fluid loss after damage to the femoral and popliteal arteries in a normotensive, coagulopathic, cadaveric lower-extremity flow model using an inert blood analogue, as compared to a compression tourniquet.
METHODS:
Using a fresh cadaveric model with simulated vascular flow, this study sought to compare the effectiveness of the external soft-tissue hemostatic clamp versus the compression tourniquet to control fluid loss in simulated trauma resulting in femoral and posterior tibial artery lacerations using a coagulopathic, normotensive, cadaveric-extremity flow model. A sample of 16 fresh, un-embalmed, human cadaver lower extremities was used in this randomized, balanced two-treatment, two-period, two-sequence, crossover design. Statistical significance of the treatment comparisons was assessed with paired t-tests. Results were expressed as the mean and standard deviation (SD).
RESULTS:
Mean intravascular fluid loss was increased from simulated arterial wounds with the external soft-tissue hemostatic clamp as compared to the compression tourniquet at the lower leg (119.8mL versus 15.9mL; P <.001) and in the thigh (103.1mL versus 5.2mL; P <.001).
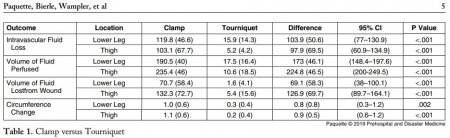
CONCLUSION:
In this hemorrhagic, coagulopathic, cadaveric-extremity experimental flow model, the use of the external soft-tissue hemostatic clamp as a hasty hemostatic adjunct was associated with statistically significant greater fluid loss than with the use of the compression tourniquet.
21/12/2019
En attendant le REBOA: Une paire de main ou un genou !
Proximal External Aortic Compression for Life-Threatening Abdominal-Pelvic and Junctional Hemorrhage: An Ultrasonographic Study in Adult Volunteers.
INTRODUCTION:
Following life-threatening junctional trauma, the goal is to limit blood loss while expediting transfer to operative rescue. Unfortunately, life-threatening abdominal-pelvic or junctional hemorrhage is often not amenable to direct compression and few temporizing strategies are available beyond hemostatic dressings, hypotensive resuscitation, and balanced transfusion.
OBJECTIVES:
In this study, we evaluated proximal external aortic compression to arrest blood flow in healthy adult men.
METHODS:
This was a simulation trial of proximal external aortic compression, for life-threatening abdominal-pelvic and junctional hemorrhage, in a convenience sample of healthy adult male volunteers. The primary end points were cessation of femoral blood flow as assessed by pulse wave Doppler ultrasound at the right femoral artery, caudal to the inguinal ligament. Secondary end points were discomfort and negative sequelae.
RESULTS:
Aortic blood flow was arrested in 12 volunteers. Median time to blood flow cessation was 12.5 seconds. Median reported discomfort was 5 out of 10. No complications or negative sequelae were reported.

CONCLUSION:
This trial suggests that it may be reasonable to attempt temporization of major abdominal-pelvic and junctional hemorrhage using bimanual proximal external aortic compression. In the absence of immediate alternatives for this dangerous and vexing injury pattern, there appear to be few downsides to prehospital proximal external aortic compression while concomitantly expediting definite care.
01/12/2019
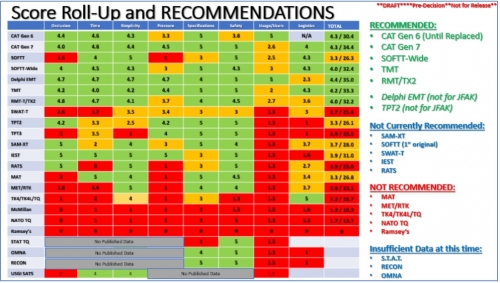
Quel tourniquet ?: Cela évolue, un peu
| Tags : tourniquet
14/10/2019
Pansements compressifs: Le test de la NAMRU
Pas nouveau mais instructif dans le contexte de bataille commerciale entre les industriels
08/10/2019
IT Clamp: Pas convaincant !
External Soft-Tissue Hemostatic Clamp Compared to a Compression Tourniquet as Primary Hemorrhage Control Device in Pilot Flow Model Study.
INTRODUCTION:
Acute blood loss represents a leading cause of death in both civilian and battlefield trauma, despite the prioritization of massive hemorrhage control by well-adopted trauma guidelines. Current Tactical Combat Casualty Care (TCCC) and Tactical Emergency Casualty Care (TECC) guidelines recommend the application of a tourniquet to treat life-threatening extremity hemorrhages. While extremely effective at controlling blood loss, the proper application of a tourniquet is associated with severe pain and could lead to transient loss of limb function impeding the ability to self-extricate or effectively employ weapons systems. As a potential alternative, Innovative Trauma Care (San Antonio, Texas USA) has developed an external soft-tissue hemostatic clamp that could potentially provide effective hemorrhage control without the aforementioned complications and loss of limb function. Thus, this study sought to investigate the effectiveness of blood loss control by an external soft-tissue hemostatic clamp versus a compression tourniquet.
HYPOTHESIS:
The external soft-tissue hemostatic clamp would be non-inferior at controlling intravascular fluid loss after damage to the femoral and popliteal arteries in a normotensive, coagulopathic, cadaveric lower-extremity flow model using an inert blood analogue, as compared to a compression tourniquet.
METHODS:
Using a fresh cadaveric model with simulated vascular flow, this study sought to compare the effectiveness of the external soft-tissue hemostatic clamp versus the compression tourniquet to control fluid loss in simulated trauma resulting in femoral and posterior tibial artery lacerations using a coagulopathic, normotensive, cadaveric-extremity flow model. A sample of 16 fresh, un-embalmed, human cadaver lower extremities was used in this randomized, balanced two-treatment, two-period, two-sequence, crossover design. Statistical significance of the treatment comparisons was assessed with paired t-tests. Results were expressed as the mean and standard deviation (SD).
RESULTS:
Mean intravascular fluid loss was increased from simulated arterial wounds with the external soft-tissue hemostatic clamp as compared to the compression tourniquet at the lower leg (119.8mL versus 15.9mL; P <.001) and in the thigh (103.1mL versus 5.2mL; P <.001).
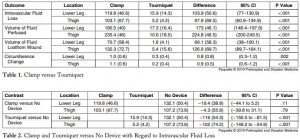
CONCLUSION:
In this hemorrhagic, coagulopathic, cadaveric-extremity experimental flow model, the use of the external soft-tissue hemostatic clamp as a hasty hemostatic adjunct was associated with statistically significant greater fluid loss than with the use of the compression tourniquet.
Formation au Tourniquet: Il faut mieux faire
High Tourniquet Failure Rates Among Non-Medical Personnel Do Not Improve with Tourniquet Training, Including Combat Stress Inoculation: A Randomized Controlled Trial.
BACKGROUND:
The rate of failing to apply a tourniquet remains high.
HYPOTHESIS:
The study objective was to examine whether early advanced training under conditions that approximate combat conditions and provide stress inoculation improve competency, compared to the current educational program of non-medical personnel.
METHODS:
This was a randomized controlled trial. Male recruits of the armored corps were included in the study. During Combat Lifesaver training, recruits apply The Tourniquet 12 times. This educational program was used as the control group. The combat stress inoculation (CSI) group also included 12 tourniquet applications, albeit some of them in combat conditions such as low light and physical exertion. Three parameters defined success, and these parameters were measured by The Simulator: (1) applied pressure ≥ 200mmHg; (2) time to stop bleeding ≤ 60 seconds; and (3) placement up to 7.5cm above the amputation.
RESULTS:
Out of the participants, 138 were assigned to the control group and 167 were assigned to the CSI group. The overall failure rate was 80.33% (81.90% in the control group versus 79.00% in the CSI group; P value = .565; 95% confidence interval, 0.677 to 2.122). Differences in pressure, time to stop bleeding, or placement were not significant (95% confidence intervals, -17.283 to 23.404, -1.792 to 6.105, and 0.932 to 2.387, respectively).
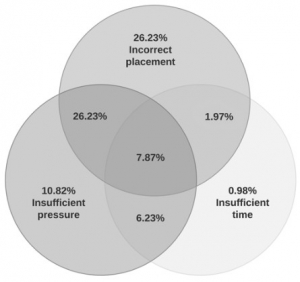
Tourniquet placement was incorrect in most of the applications (62.30%).
CONCLUSIONS:
This study found high rates of failure in tourniquet application immediately after successful completion of tourniquet training. These rates did not improve with tourniquet training, including CSI. The results may indicate that better tourniquet training methods should be pursued.
| Tags : tourniquet
21/09/2019
Garrot: Précoce, mais à réévaluer
Duration of extremity tourniquet application profoundly impacts soft-tissue antibiotic exposure in a rat model of ischemia-reperfusion injury
Mangum LC et al. Injury 10.1016/j.injury.2019.09.025
Introduction
Extremity tourniquet (TNK) application is an effective means of achieving compressible hemorrhage control in the emergency prehospital and clinical trauma setting. Modern United States military medical doctrine recommends TNK use to prevent lethal hemorrhage from extremity injury, followed by systemic prophylactic antibiotics to prevent wound infection. Because tissue pharmacokinetics of prophylactic antimicrobials during and after TNK-induced limb ischemia are largely unknown, this study was conducted to empirically determine the relationship between TNK application time and soft tissue antibiotic exposure in order to guide medical personnel in the management of extremity trauma.
Materials and Methods
Hind limbs of anesthetized male Sprague Dawley rats were exsanguinated, and ischemia maintained by a pneumatic cuff placed at the level of the mid femur on one limb; the non-ischemic contralateral limb served as comparison tissue. Systemic prophylactic antibiotics (cefazolin, moxifloxacin, or ertapenem) were administered intravenously before or after TNK release following 2 or 4 hours of ischemia with subsequent re-dosing every 12 hours for 3 days. Free antibiotic in the interstitial fluid (ISF) of the tibialis anterior muscle of both hind limbs was recovered via microdialysis during ischemia and over three periods during reperfusion: immediately following TNK release, at 24 hours post TNK release, and at 72 hours post TNK release. Plasma and ISF free drug concentrations were determined by high-performance liquid chromatography.
Results
Tourniquet application prevented delivery of prophylactic antibiotics into distal soft tissue for the duration of ischemia, and caused a profound reduction in skeletal muscle drug exposure for up to 72 hours following TNK release. A progressive decline in tissue antibiotic exposure during reperfusion was observed as TNK times increased from 2 hours to 4 hours.

The timing and severity of reduced drug distribution in post-ischemic skeletal muscle varied substantially among the three antibiotic classes evaluated.
Conclusions
Prolonged tourniquet application can significantly reduce distribution of prophylactic antibiotics into soft tissue during and after ischemia, potentially impairing prophylaxis of extremity wound infection. Our findings support the examination of alternative approaches to wound infection prophylaxis under conditions of delayed casualty evacuation when occlusive hemorrhage control measures are utilized.
06/08/2019
Garrot tactique: Oui, mais avec une réévaluation PRECOCE
Tactical tourniquet: Surgical management must be within 3 hours.
------------------------------------------
------------------------------------------
Despite longstanding controversy, tourniquets are widely used in tactical combat casualty care, with undisputed benefits for recent conflicts in Iraq and Afghanistan. Increased time delays are a particular issue in large areas, such as the Sahel-Saharan band. Complications associated with tourniquet use are predominantly related to acute ischemia with risk of amputation and ischaemia-reperfusion injury, as shown in the first clinical case. Often stated but poorly described, misuse of tourniquet and subsequent failure to interrupt arterial blood flow is also a clinical scenario that should be recognized. In the case of misuse of the tourniquet, more significant blood loss may be expected because of venous compression (« venous tourniquet », second clinical case). Early medical re-evaluation of the tourniquet is an essential component in prolonged field care. This includes reassessment of the tourniquet's ability to achieve hemostasis, abolish the downstream pulse and the relevance of the tourniquet altogether. This combat tool requires training to be successful and complications are time dependent. Tourniquet use requires appropriate application, re-evaluation and triage of wounded personnel within 3 h towards more structured surgical management.
| Tags : tourniquet