03/10/2018
Plaquettes et golden hour: Possible ?
Intravenous synthetic platelet (SynthoPlate) nanoconstructs reduce bleeding and improve 'golden hour' survival in a porcine model of traumatic arterial hemorrhage.
Traumatic non-compressible hemorrhage is a leading cause of civilian and military mortality and its treatment requires massive transfusion of blood components, especially platelets. However, in austere civilian and battlefield locations, access to platelets is highly challenging due to limited supply and portability, high risk of bacterial contamination and short shelf-life. To resolve this, we have developed an I.V.-administrable 'synthetic platelet' nanoconstruct (SynthoPlate), that can mimic and amplify body's natural hemostatic mechanisms specifically at the bleeding site while maintaining systemic safety.

Previously we have reported the detailed biochemical and hemostatic characterization of SynthoPlate in a non-trauma tail-bleeding model in mice. Building on this, here we sought to evaluate the hemostatic ability of SynthoPlate in emergency administration within the 'golden hour' following traumatic hemorrhagic injury in the femoral artery, in a pig model. We first characterized the storage stability and post-sterilization biofunctionality of SynthoPlate in vitro. The nanoconstructs were then I.V.-administered to pigs and their systemic safety and biodistribution were characterized. Subsequently we demonstrated that, following femoral artery injury, bolus administration of SynthoPlate could reduce blood loss, stabilize blood pressure and significantly improve survival. Our results indicate substantial promise of SynthoPlate as a viable platelet surrogate for emergency management of traumatic bleeding.
22/07/2018
Chitine: Prudence quand même ?
Chitin and Its Effects on Inflammatory and Immune Responses
-------------------------------------------
Les pansements hémostatiques à base de chitine sont largement utilisés et ne semblent pas actuellement poser de problème allergique (1). Néanmoins se pose la question de leur innocuité immune. Le développement des allergies croisées avec les produits dérivés de la mer et l'emploi de chitine comme complément alimentaire sont autant de facteurs de rencontre avec un allergène vrai. De telles allergies croisées s'observent également avec d'autres composants tels que la paravalbumine et le collagène des produits de la mer. Les pansements hémostatiques ne contenant pas de chitine ne semble pas exposer à ce risque potentiel.

-------------------------------------------
Chitin, a potential allergy-promoting pathogen-associated molecular pattern (PAMP), is a linear polymer composed of N-acetylglucosamine residues which are linked by β-(1,4)-glycosidic bonds. Mammalians are potential hosts for chitin-containing protozoa, fungi, arthropods, and nematodes; however, mammalians themselves do not synthetize chitin and thus it is considered as a potential target for recognition by mammalian immune system. Chitin is sensed primarily in the lungs or gut where it activates a variety of innate (eosinophils, macrophages) and adaptive immune cells (IL-4/IL-13 expressing T helper type-2 lymphocytes). Chitin induces cytokine production, leukocyte recruitment, and alternative macrophage activation. Intranasal or intraperitoneal administration of chitin (varying in size, degree of acetylation and purity) to mice has been applied as a routine approach to investigate chitin's priming effects on innate and adaptive immunity. Structural chitinpresent in microorganisms is actively degraded by host true chitinases, including acidic mammalian chitinases and chitotriosidase into smaller fragments that can be sensed by mammalian receptors such as FIBCD1, NKR-P1, and RegIIIc. Immune recognition of chitin also involves pattern recognition receptors, mainly via TLR-2 and Dectin-1, to activate immune cells to induce cytokine production and creation of an immune network that results in inflammatory and allergic responses. In this review, we will focus on various immunological aspects of the interaction between chitin and host immune system such as sensing, interactions with immune cells, chitinases as chitin degrading enzymes, and immunologic applications of chitin.
21/07/2018
+ d'1 Tourniquet et 1/4 converti
Point of injury tourniquet application during Operation Protective Edge-What do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate- and short-term outcomes of point of injury (POI) tourniquet applications during "Operation Protective Edge" (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications, and short-term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps treated 704 casualties. Of these, 90 casualties were treated with 119 tourniquets of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88 of 90) of the casualties. Injuries sustained from improvised explosive devices and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p = 0.034). The success rate of the first tourniquet was reported to be 70% (84 of 119), regardless of caregiver level (p = 0.56), tourniquet type (p = 0.16), or limb characters (p = 0.48). Twenty-seven (25.7%) of 105 of the tourniquets were converted to direct pressure dressings enroute to receiving hospitals two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on eight casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5 of 85), no vascular involvement was discovered during surgery, and the fasciotomy is suspected as tourniquet related. 7%) 6 of 85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10 of 85) (one patient had both fasciotomy and neural complication without vascular injury).
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity, whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet
01/05/2018
Tourniquet: Une vieille histoire
A brief history of the tourniquet
Welling DR et Al. Vasc Surg 2012;55:286-90
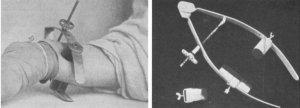
Le compresseur de Matas
| Tags : tourniquet
01/03/2018
Trauma jonctionnels: Une revue
| Tags : jonctionnel, hémorragie
15/01/2018
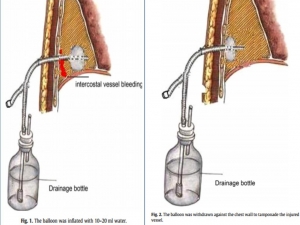
Une sonde de Foley dans le thorax
Balloon Foley catheter compression as a treatment for intercostal vessel bleeding
Chao BF et Al. Injury. 2011 Sep;42(9):958-9.
Avoir DEUX FOLEY avec soi, et ce n'est pas pour faire un sondage urinaire mais pour réaliser un tamponnement nasal, intercostale, d'une plaie cervicale ou tout simpment pour draîner un thorax
03/12/2017
Garrot: Pas si simple sans formation
The Tourniquet Gap: A Pilot Study of the Intuitive Placement of Three Tourniquet Types by Laypersons
Ross EM et Al. http://dx.doi.org/10.1016/j.jemermed.2017.09.011
--------------------------
La pose de garrot par l'intervenant le plus proche d'une victime blessé semble être une évidence. Pourtant ce travail met en évidence un taux relativement important d'échec. Ceci milite pour la conduite de campagne de formation avant toute mise à disposition de garrot industriel
--------------------------
Objectives
The objective of this pilot study was to determine which tourniquet type was the most intuitive for a layperson to apply correctly.
Methods
This project is a randomized study derived from a “Stop the Bleed” education initiative conducted between September 2016 and March 2017. Novice tourniquet users were randomized to apply one of three commercially available tourniquets (Combat Action Tourniquet [CAT; North American Rescue, LLC, Greer, SC], Ratcheting Medical Tourniquet [RMT; m2 Inc., Winooski, VT], or Stretch Wrap and Tuck Tourniquet [SWAT-T; TEMS Solutions, LLC, Salida, CO]) in a controlled setting. Individuals with formal medical certification, prior military service, or prior training with tourniquets were excluded. The primary outcome of this study was successful tourniquet placement.
Results
Of 236 possible participants, 198 met the eligibility criteria. Demographics were similar across groups. The rates of successful tourniquet application for the CAT, RMT, and SWAT-T were 16.9%, 23.4%, and 10.6%, respectively ( p = 0.149). The most common causes of application failure were: inadequate tightness (74.1%), improper placement technique (44.4%), and incorrect positioning (16.7%).
Conclusion
Our pilot study on the intuitive nature of applying commercially available tourniquets found unacceptably high rates of failure. Large-scale community education efforts and manufacturer improvements of tourniquet usability by the lay public must be made before the widespread dissemination of tourniquets will have a significant public health effect.
| Tags : tourniquet
15/11/2017
XStat versus Quikclot: Pas de différence de survie
Evaluation of XSTAT® and QuickClot® Combat Gauze® in a Swine Model of Lethal Junctional Hemorrhage in Coagulopathic Swine.
BACKGROUND:
Hemorrhage is associated with most potentially survivable deaths on the battlefield. Effective and field-tested products are lacking to treat junctional and noncompressible injuries. XSTAT® is a newly developed, U.S. Food and Drug Administration-approved product designed to treat junctional hemorrhage. The Committee on Tactical Combat Casualty Care has recently approved the product for use as part of its treatment guidelines, but data are lacking to assess its efficacy in different wounding patterns and physiologic states.
METHODS:
Dilutional coagulopathy was induced in 19 large (70-90kg), healthy, male swine by replacing 60% of each animal's estimated blood volume with room temperature Hextend ®. After dissection, isolation, and lidocaine incubation, uncontrolled hemorrhage was initiated by transection of both axillary artery and vein. Free bleeding was allowed to proceed for 30 seconds until intervention with either XSTAT or QuickClot® Combat Gauze® (CG) followed by standard backing. Primary outcomes were survival, hemostasis, and blood loss.
RESULTS:
XSTAT-treated animals achieved hemostasis in less time and remained hemostatic longer than those treated with CG. Less blood was lost during the first 10 minutes after injury in the XSTAT group than the CG group. However, no differences in survival were observed between XSTAT-treated and CG-treated groups. All animals died before the end of the observation period except one in the XSTAT-treated group.
CONCLUSION:
XSTAT performed better than CG in this model of junctional hemorrhage in coagulopathic animals. Continued testing and evaluation of XSTAT should be performed to optimize application and determine appropriate indications for use.
| Tags : hémorragie, pansement
31/08/2017
Tourniquet: Bien en contexte civil AUSSI
The trauma center is too late: Major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock
Scerbo MH et Al. Journal of Trauma and Acute Care Surgery,10.1097/TA.0000000000001666
Background: To date, no civilian studies have demonstrated that pre-hospital (PH) tourniquets improve survival. We hypothesized that late, trauma center (TC) tourniquet use would increase death from hemorrhagic shock compared to early (PH) placement.
Methods: All patients arriving to a Level-1, urban TC between 10/2008 and 01/2016 with a tourniquet placed prior to (T-PH) or after arrival to the TC (T-TC) were evaluated. Cases were assigned the following designations: indicated [absolute indication (vascular injury requiring repair/ligation, operation within 2 hours for extremity injury, or traumatic amputation), or relative indication (major musculoskeletal/soft-tissue injury requiring operation 2-8 hours after arrival, documented large blood loss)], or non-indicated. Outcomes were death from hemorrhagic shock, physiology upon arrival to the TC and massive transfusion requirements. Following univariate analysis, logistic regression was carried out to assess independent predictors of death from hemorrhagic shock.
Results: 306 patients received 326 tourniquets for injuries to 157 upper and 147 lower extremities. 281 (92%) had an indication for placement. 70% of patients had a blunt mechanism of injury. T-TC patients arrived with a lower systolic blood pressure [101 (86, 123) versus 125 (100, 145)mmHg, p<0.001], received more transfusions in the first hour of arrival (55% versus 34%, p=0.02) and had a greater mortality from hemorrhagic shock (14% vs. 3.0%, p=0.01). When controlling for year of admission, mechanism of injury and shock upon arrival (SBP ≤90mmHg or HR ≥120 bpm or base deficit ≤ 4), indicated T-TC had a 4.5-fold increased odds of death compared to T-PH [OR 4.5, 95% CI 1.23-16.4, p=0.02)].
Conclusions: Waiting until TC arrival to control hemorrhage with a tourniquet was associated with worsened blood pressure and increased transfusion within the first hour of arrival. In routine civilian trauma patients, delaying to T-TC was associated with 4.5-fold increased odds of mortality from hemorrhagic shock
| Tags : tourniquet
05/05/2017
Fractions coagulantes: Mieux que PFC ?
Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial.
-------------------------------------------------
Un travail dont les conclusions sont très claires. La prise en charge de la coagulopathie traumatique bénéficie bien plus d'une stratégie d'apports ciblés de fractions coagulantes concentrées, notamment de fibrinogène ici 50 mg/kg, qu'une stratégie classique basée sur l'apport de PFC.
-------------------------------------------------
Background
Effective treatment of trauma-induced coagulopathy is important; however, the optimal therapy is still not known. We aimed to compare the efficacy of first-line therapy using fresh frozen plasma (FFP) or coagulation factor concentrates (CFC) for the reversal of trauma-induced coagulopathy, the arising transfusion requirements, and consequently the development of multiple organ failure.
Methods
This single-centre, parallel-group, open-label, randomised trial was done at the Level 1 Trauma Center in Innsbruck Medical University Hospital (Innsbruck, Austria). Patients with trauma aged 18–80 years, with an Injury Severity Score (ISS) greater than 15, bleeding signs, and plasmatic coagulopathy identified by abnormal fibrin polymerisation or prolonged coagulation time using rotational thromboelastometry (ROTEM) were eligible. Patients with injuries that were judged incompatible with survival, cardiopulmonary resuscitation on the scene, isolated brain injury, burn injury, avalanche injury, or prehospital coagulation therapy other than tranexamic acid were excluded. We used a computer-generated randomisation list, stratification for brain injury and ISS, and closed opaque envelopes to randomly allocate patients to treatment with FFP (15 mL/kg of bodyweight) or CFC (primarily fibrinogen concentrate [50 mg/kg of bodyweight]). Bleeding management began immediately after randomisation and continued until 24 h after admission to the intensive care unit. The primary clinical endpoint was multiple organ failure in the modified intention-to-treat population (excluding patients who discontinued treatment). Reversal of coagulopathy and need for massive transfusions were important secondary efficacy endpoints that were the reason for deciding the continuation or termination of the trial. This trial is registered with ClinicalTrials.gov, number NCT01545635.
Findings
Between March 3, 2012, and Feb 20, 2016, 100 out of 292 screened patients were included and randomly allocated to FFP (n=48) and CFC (n=52). Six patients (four in the FFP group and two in the CFC group) discontinued treatment because of overlooked exclusion criteria or a major protocol deviation with loss of follow-up. 44 patients in the FFP group and 50 patients in the CFC group were included in the final interim analysis. The study was terminated early for futility and safety reasons because of the high proportion of patients in the FFP group who required rescue therapy compared with those in the CFC group (23 [52%] in the FFP group vs two [4%] in the CFC group; odds ratio [OR] 25·34 [95% CI 5·47–240·03], p<0·0001) and increased needed for massive transfusion (13 [30%] in the FFP group vs six [12%] in the CFC group; OR 3·04 [0·95–10·87], p=0·042) in the FFP group. Multiple organ failure occurred in 29 (66%) patients in the FFP group and in 25 (50%) patients in the CFC group (OR 1·92 [95% CI 0·78–4·86], p=0·15).
Interpretation
Our results underline the importance of early and effective fibrinogen supplementation for severe clotting failure in multiple trauma. The available sample size in our study appears sufficient to make some conclusions that first-line CFC is superior to FFP.
| Tags : coagulopathie
29/04/2017
Une ceinture pour tourniquet ? Plutôt l'inverse.
Belts Evaluated as Limb Tourniquets: BELT Study Comparing Trouser Supporters Used as Medical Devices in a Manikin Model of Wound Bleeding.
Bequette BW et Al Wilderness Environ Med. 2017 Apr 19. pii: S1080-6032(17)30060-1.
--------------------------------
Une idée, qui n'est pas nouvelle de même que celui de pantalon intégrant un garrot (1), mais on devrait plutôt dire un tourniquet pour ceinture. Ce travail est par ailleurs intéressant car il aborde la problématique des garrots insuffisamment serrés.
--------------------------------
OBJECTIVE:
The purpose of the present study is to compare several models of commercially designed belts as used as a tourniquet.
METHODS:
In the Belts Evaluated as Limb Tourniquets (BELT) study, an experiment was designed to test the effectiveness of pants belts as non improvised medical devices to control hemorrhage in a manikin. Models of belts included Tourni-belt, Tourniquet Belt, ParaBelt, and Battle Buddy. Data collected included effectiveness, time to stop bleeding, total time of application, pressure, blood loss, and composite results (score count of good results; composite outcome good if every component was good).
RESULTS:
Differences in effectiveness percentages among models were not statistically significant. The difference in mean between users was statistically significant for stop time, total time, pressure, blood loss, composite score, and composite outcome. Mean time to stop bleeding differed for only 1 pair of models after the Tukey-Kramer adjustment; ParaBelt was faster than Tourniquet Belt. Mean total time of application differed between ParaBelt-Tourniquet Belt and Tourni-belt-Tourniquet Belt; the former model in both pairs was faster. No significant difference in mean blood loss measured by model was found. For composite outcome score, no pairwise difference between models was significant. For composite outcome (good-bad), ParaBelt had good results in 75% of tests; the other 3 models had significantly worse results.
CONCLUSIONS:
In a preliminary laboratory analysis of belt tourniquet models using a manikin, performance differed by model. ParaBelt performed better than other models for the composite outcome.our tourniquet ?
| Tags : tourniquet
11/04/2017
Tourniquet: Les israéliens, pour +++
Point of injury tourniquet application during Operation Protective Edge - what do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate and short term outcomes of point of injury (POI) tourniquet applications during 'Operation Protective Edge' (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications and short term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps (IDF-MC) treated 704 casualties. Out of these, 90 casualties were treated with 119 tourniquets out of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88/90) of the casualties. Injuries sustained from Improvised explosive devices (IED) and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p=0.034). The success rate of the first tourniquet was reported to be 70% (84/119), regardless of caregiver level (P=0.56), tourniquet type (P=0.16) or limb characters (p=0.48). two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on 8 casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5/85) no vascular involvement was discovered during surgery and the fasciotomy is suspected as tourniquet related. 7%) 6/85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10/85) (one patient had both fasciotomy and neural complication without vascular injury)
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet
25/03/2017
Packing de plaie = Pansement hémostatique
Uncontrolled hemorrhage remains one of the leading causes of trauma deaths and one of the most challenging problems facing emergency medical professionals. Several hemostatic agents have emerged as effective adjuncts in controlling extremity hemorrhage. However, a review of the current literature indicates that none of these agents have proven superior under all conditions and in all wound types. This study compared several hemostatic agents in a lethal penetrating groin wound model where the bleeding site could not be visualized.
METHODS:
A complex groin injury with a small penetrating wound, followed by transection of the femoral vessels and 45 seconds of uncontrolled hemorrhage, was created in 80 swine. The animals were then randomized to five treatment groups (16 animals each). Group 1 was Celox-A (CA), group 2 was combat gauze (CG), group 3 was Chitoflex (CF), group 4 was WoundStat (WS), and group 5 was standard gauze (SG) dressing. Each agent was applied with 5 minutes of manual pressure. Hetastarch (500 mL) was infused over 30 minutes. Hemodynamic parameters were recorded over 180 minutes. Primary endpoints were attainment of initial hemostasis and incidence of rebleeding.
RESULTS:
Overall, no difference was found among the agents with respect to initial hemostasis, rebleeding, and survival. Localizing effects among the granular agents, with and without delivery mechanisms, revealed that WS performed more poorly in initial hemostasis and survival when compared to CA.
CONCLUSIONS:
In this swine model of uncontrolled penetrating hemorrhage, SG dressing performed similarly to the hemostatic agents tested. This supports the concept that proper wound packing and pressure may be more important than the use of a hemostatic agent in small penetrating wounds with severe vascular trauma.
23/03/2017
REBOA: Une technique qui trouve sa place
Resuscitative endovascular balloon occlusion of the aorta for uncontrolled haemorrhagic shock as an adjunct to haemostatic procedures in the acute care setting
-------------------------------
Le principe d'occlusion artérielle n'est pas nouveau. L'occlusion endovasculaire de l'aorte trouve sa place dans la gestion des hémorragies abdominales incontrôlable. Son intérêt en traumatologie ballistique de guerre est probable (1). Cette technique a été récemment décrite en phase préhospitalière (2). Nos conditions d'exercice méritent que l'on s'intéresse à cette technique (3).
-------------------------------
Background:
Haemorrhagic shock is a major cause of death in the acute care setting. Since 2009, our emergency department has used intra-aortic balloon occlusion (IABO) catheters for resuscitative endovascular balloon occlusion of the aorta (REBOA).
Methods: REBOA procedures were performed by one or two trained acute care physicians in the emergency room (ER) and intensive care unit (ICU). IABO catheters were positioned using ultrasonography. Collected data included clinical characteristics, haemorrhagic severity, blood cultures, metabolic values, blood transfusions, REBOA-related complications and mortality.
Results: Subjects comprised 25 patients (trauma, n = 16; non-trauma, n = 9) with a median age of 69 years and a median shock index of 1.4. REBOA was achieved in 22 patients, but failed in three elderly trauma patients. Systolic blood pressure significantly increased after REBOA (107 vs. 71 mmHg, p < 0.01). Five trauma patients (20 %) died in ER, and mortality rates within 24 h and 60 days were 20 % and 12 %, respectively. No REBOA-related complications were encountered. The total occlusion time of REBOA was significantly lesser in survivors than that in non-survivors (52 vs. 97 min, p < 0.01). Significantly positive correlations were found between total occlusion time of REBOA and shock index (Spearman’s r = 0.6) and lactate concentration (Spearman’s r = 0.7) in survivors.
Conclusion: REBOA can be performed in ER and ICU with a high degree of technical success. Furthermore, correlations between occlusion time and initial high lactate levels and shock index may be important because prolonged occlusion is associated with a poorer outcome.
| Tags : choc, hémorragie
17/03/2017
Tourniquet: La nouveauté de SamMedical
SAM Tourniquet XT
Un garrot, dont l'intérêt apparaît être d'une part sur sa largeur et d'autre part sur sa boucle de serrage innovante.
Clic sur l'image pour accéder à une vidéo
| Tags : tourniquet
14/03/2017
Tourniquet: Attention
-------------------
La pose d'un garrot est essentiel à la survie d'un blessé présentant une hémorragie sévère des membres. Encore faut-il qu'il soit de bonne qualité. Les autorités sanitaires américaines insistent sur l'importance de ne se fournir qu'auprès de distributeurs connues distribuant des garrots éprouvés plutôt que de céder aux sirènes de la copie chinoise de basse qualité. En effet même ces garrots voient leur efficacité réduite après exposition aux conditions de combat. C'est ce que met une fois de plus en évidence ce travail.
-------------------
BACKGROUND:
The purpose of the present study was to mechanically assess models of emergency tourniquet after 18 months of environmental exposure to weather to better understand risk of component damage.
MATERIALS AND METHODS:
An experiment was designed to test tourniquet performance on a manikin thigh. Three tourniquet models were assessed: Special Operations Forces Tactical Tourniquet Wide, Ratcheting Medical Tourniquet, and Combat Application Tourniquet. Unexposed tourniquets formed a control group stored in a laboratory; exposed tourniquets were placed outdoors on a metal roof for 18 months in San Antonio, Texas. Two users, a military cadet and a scientist, made 300 assessments in total. Assessment included major damage (yes-no), effectiveness (hemorrhage control, yes-no), casualty survival (alive-dead), time to stop bleeding, pressure, and blood loss. Time, pressure, and blood loss were reported in tests with effectiveness.
RESULTS:
Exposed devices had worse results than unexposed devices for major damage (3% [4/150] versus 0% [0/150]; ρ = .018), effectiveness (89% versus 99%; ρ = .002), and survival of casualties (89% versus 100%; ρ < .001). In tests for effectiveness, exposed devices had worse results than unexposed devices for time to stop bleeding (29 seconds versus 26 seconds; ρ = .01) and pressure (200mmHg versus 204mmHg; ρ = .03, respectively), but blood loss volume did not differ significantly.
CONCLUSION:
Compared with unexposed control devices, environmentally exposed tourniquets had worse results in tests of component damage, effectiveness, and casualty survival.
| Tags : tourniquet
16/02/2017
TMT tourniquet: Un nouveau venu
Un nouveau venu qui fait aussi bien que la référence US, à savoir le CAT, sans apporter plus (1). Ne pas confondre ce garrot dont le distributeur est connu et dont la fabrication parfaitement tracée. Sans aucune comparaison avec nombre de copies qui ne bénéficient pas des mêmes contrôle de qualité distribués à moins de 10 Euros et qui peuvent faire illusion.

| Tags : tourniquet
08/02/2017
Tourniquets contrefaits = DANGER
DANGER
Les événements récents ont mis en avant l'importance de l'application précoce de garrot. L'approvisionnement en garrot est un véritable challenge et un marché où la guerre commerciale fait maintenant rage. Si le nombre de fabricants historiques de garrot était relativement restreint (CAT, SOFT-T, TK4, RATS, MAT, SWAT), on voit fleurir nombre de copies essentiellement chinoises dont il est relativement aisé de se procurer des exemplaires, notamment sur le marché de l'AIRSOFT. Deux fabricants sont particulièrement la cible de ces contrefacteurs CAT ressources et TACMED solutions, car ce sont les deux garrots validés par les US dans le cadre du TCCC. Ces deux fabricants diffusent leurs produits pour une 20aines d'euros. Le garrot en service dans l'armée française depuis une dizaine d'année est le SOFT-T de la société TACMED, garrot dont il existe une version adaptée pour l'enfant. Les contrefacteurs chinois affichent des tarifs parfois 10 fois moindres. Les produits proposés par ces sociétés ne peuvent pas disposer des qualités techniques de même niveau que ceux détenus par les originaux. Un aspect important des garrots est leur résistance au vieillissement, aux intempéries, au froid, aux UV. Il a été démontré que ces caractéristiques sont très importantes en terme d'efficacité après quelques mois de port du garrot en ambiance opérationnelle vraie. Il serait étonnant que ces copies de garrot, dont les matières premières et les circuits de fabrication sont pour le moins opaques offrent les mêmes garanties de sécurité que ceux de fabricants historiques maîtrisant tous les process de fabrication de leur production.
Par ailleurs il semblerait que les conditions des certifications CE et ISO 134 (1,2,3)85 soit sujettes à caution car en partie relevant d'une autocertification.
Les autorités américaines ne sont saisies de ce problème et rappellent l'importance de ne s'approvisionner que chez les forunisseurs des garrots validés dans le T3C, à savoir les garrots produits apr CAT ressources et TacMed Solutions en excluant toute autre production au prétexte de tarifs à première vue (tro) alléchants. Lire le rapport de la FDA
Je vous propose dans le lien suivant quelques exemples concernant le garrot SOFT-T
Matériel Tourniquet Contrefaçons.pdf
Certains modèles de tourniquet s'inspirent très fortement de ces produits et en particulier du SOF-T (notamment le wide) mais avec une démarche d' innovation réelle. Aussi ces tourniquets sont ils différents de simples copies et très probablement de bonne qualité. Ils ne sont pas produits en chine mais dans des pays de l'Est européen, voire en Russie (a,b). On manque néanmoins de recul d'expertise technique de ces derniers.
Dans l'état actuel des choses, à moins de s'équiper pour de l'airsoft, la prudence est de rester à l'écart des ces garrots et de continuer à utiliser les produits distribués par les fournisseurs reconnus des fabricants historiques (4, 5,6)
| Tags : tourniquet
04/02/2017
QuikClot: Du nouveau, pour l'hôpital
La gamme quikclot s'agrandit avec toute une proposition de pansement adapté à l'usage hospitalier, que ce soit peropératoire ou en soins critiques.


| Tags : hémorragie
22/01/2017
Du sang qui descend du ciel
Nous ne sommes pas les seuls à avoir à faire face au contexte d'isolement. Il est particulièrement intéressant de regarder comment ces problèmes sont abordés par les pays en voie de construction. L'exemple rwandais devrait nous interpeller. Le recours à des drones de livraison en contexte militaire n'est pas une utopie car ce mode de ravitaillement a été utilisé en afghanistan.
| Tags : transfusion