01/11/2015
Plaie du cou et packing de plaie
| Tags : cou
06/07/2013
Sonde de foley: Au moins 2 et pas pour un sondage
Improved mortality from penetrating neck and maxillofacial trauma using Foley catheter balloon tamponade in combat
Weppner J. J Trauma Acute Care Surg. 2013;75: 00Y00
BACKGROUND:
The military medical community has promoted use of Foley catheter balloon tamponade in the initial management of vascular injury owing to neck or maxillofacial trauma. The aim of the study was to compare outcomes with Foley catheter tamponade with those obtained with traditional use of external pressure.
METHODS:
This retrospective cohort study evaluated all cases of persistent bleeding caused by penetrating neck or maxillofacial trauma received at one forward aid station between December 2009 and October 2011. Cohorts included those who were treated with Foley catheter tamponade and those managed with external pressure. Which treatment option was applied depended solely on the availability of Foley catheters at the time. The effectiveness of each technique in controlling initial and delayed hemorrhage is described, and the impact on mortality is analyzed using the Student’s t test and Fisher’s exact test.
RESULTS:
Seventy-seven subjects met the inclusion criteria with 42 subjects in the Foley group and 35 subjects in the external pressure group. A statistically significant difference was found between the groups regarding delayed failure, experienced by three patients (7%) in the Foley group and nine patients (26%) in the external pressure group ( p G 0.05). The difference in mortality, 5% (two patients) in the Foley tamponade group and 23% (eight patients) in the external pressure group, was statistically significant ( p G 0.05).
CONCLUSION:
For penetrating neck and maxillofacial injuries in a combat environment, Foley catheter balloon tamponade significantly reduced mortality when compared with direct pressure techniques through its effect on preventing delayed bleeding.
--------------------------------------------------------------------
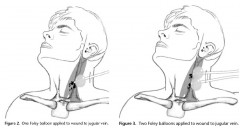 The Foley catheter tamponade is relatively simple and very easy to perform rapidly. Before its insertion in the cases examined in this study, a hemorrhaging wound was identified in the neck ormaxillofacial area, and a hemostat was applied to the distal endof an 18 Fr Foley catheter (30 cm3). The catheter was then introduced with a finger into the wound and directed along the wound track to the estimated or palpated source of bleeding, after which the Foley balloon was inflated with sterile water until the bleeding stopped or moderate resistance felt. If this technique did not stop the hemorrhage and either a deep wound or large defect was present in the bleeding vessel, it was considered that the balloon may have only been able to provide distal control. In such cases, a second catheter was introduced into the wound and inflated to provide more proximal control.
The Foley catheter tamponade is relatively simple and very easy to perform rapidly. Before its insertion in the cases examined in this study, a hemorrhaging wound was identified in the neck ormaxillofacial area, and a hemostat was applied to the distal endof an 18 Fr Foley catheter (30 cm3). The catheter was then introduced with a finger into the wound and directed along the wound track to the estimated or palpated source of bleeding, after which the Foley balloon was inflated with sterile water until the bleeding stopped or moderate resistance felt. If this technique did not stop the hemorrhage and either a deep wound or large defect was present in the bleeding vessel, it was considered that the balloon may have only been able to provide distal control. In such cases, a second catheter was introduced into the wound and inflated to provide more proximal control.
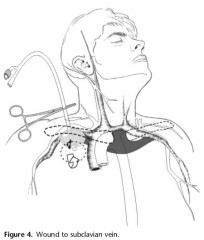
When treating Zone I injuries of the supraclavicular fossa, the catheter was introduced as far as possible past the defect in the vessel, allowing the balloon to be inflated before being pulled back firmly and then held in place with a hemostat. Doing so compressed the injured vessel onto the first rib and clavicle, which was intended to tamponade bleeding into the chest. If external hemorrhage continued following insertion of the Foley catheter, a second catheter may have been inserted to control bleeding
26/01/2013
Lésions du cou: Le point UK
Outcomes from Penetrating Ballistic Cervical Injury
Breeze J et all.J R Army Med Corps 158(2): 96-100
Aims:
Ballistic cervical injury has become a significant source of both morbidity and mortality for the deployed UK soldier. The aim of this paper was to document a case series of ballistic cervical wounds to describe the pattern of these injuries and relate them to outcome.
Methods:
The records of all UK service personnel sustaining wounds to the neck in Iraq or Afghanistan between 01 August 2004 and 01 January 2008 were analysed following identification by the Joint Theatre Trauma Registry. Blunt or thermal injuries were excluded.
Results:
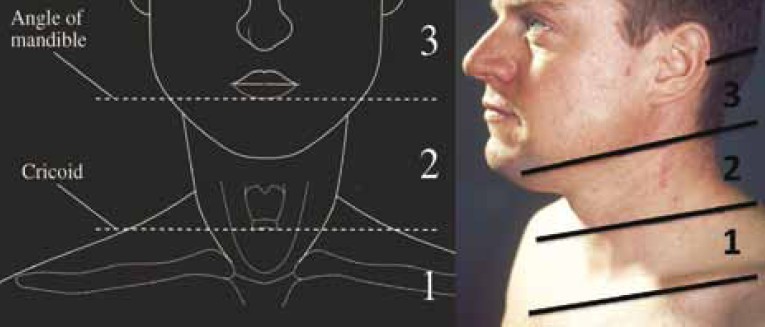
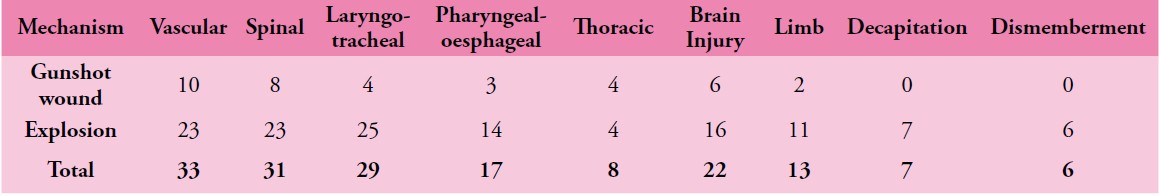
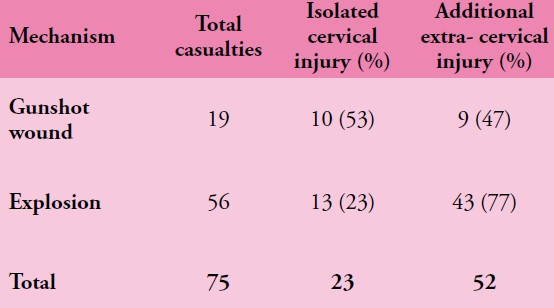
The records of 75/76 service personnel sustaining penetrating cervical injury during this period were available for analysis. 56/75 (75%) were due to explosive fragmentation and the remainder due to gunshot wounds (GSW). 33/75 (44%) of soldiers sustained vascular injury, 32/75 (43%) injury to the spine or spinal cord, 29/75 (39%) injury to the larynx or trachea and 11/75 (15%) injury to the pharynx or oesophagus. 14/75 (19%) patients in this series underwent surgery in a hospital facility for treatment of potentially life threatening cervical injuries, with a survival rate after surgery of 12/14 (86%). The overall mortality from this series of battlefield penetrating neck injury was 63%.
Conclusions:
Penetrating cervical ballistic injury is a significant source of injury to deployed UK service personnel, predominantly due to neurovascular damage. Neck collars if worn would likely prevent many of the injuries in this case series but such protection is uncomfortable and may interfere with common military tasks. Newer methods of protecting the neck should be investigated that will be acceptable to the deployed UK soldier.
| Tags : maxillo, cou, balistique