01/11/2014
N'oublions pas: Comprimer est essentiel
Laboratory assessment of out-of-hospital interventions to control junctional bleeding from the groin in a manikin model l.
Kragh JF et Al Am J Emerg Med. 2013 Aug;31(8):1276-8
Junctional body regions between the trunk and its appendages, such as the groin, are too proximal for a regular limb tourniquet to fit [1,2]. Not since 1993’s Black Hawk Down has junctional hemorrhage control become such a hot topic in military casualty care [1–7]. In February 2013, the US military’s Task Force Medical Afghanistan requested a fill of a gap in junctional hemorrhage control as an urgent operational need, meaning that junctional hemorrhage control devices should be considered urgently to fill a gap in medical care in war. A small but growing body of evidence indicates that hemorrhage control can be attained out-of-hospital with mechanical compression, using such interventions as medical devices, on a pressure point proximal to a bleeding wound [3–9]. To evaluate laboratory use of junctional hemorrhage control interventions, we gathered data on stopping groin bleeding in a manikin model to understand the plausibility of such interventions for future human subject research.
Under an approved protocol, we tested efficacy of interventions in a manikin designed to train medics in out-of-hospital hemorrhage control (Combat Ready Clamp [CRoC] Trainer Manikin, Operative Experience, Inc, North East, MD). We filled the blood reservoir with 4 liters of water; we refilled the reservoir after 5 iterations or 1.5 liters of lost fluid, whichever came first. The manikin had a right-groin gunshot wound through the proximal thigh where the common femoral artery flow was controllable by skin compression over it at the level of the inguinal fold. There was 3 cm between the pressure point where compression was applied and the proximal extent of the wound. Interventions were timed, blood loss was measured, and efficacy was noted. Efficacy was operationally defined as visually stopped flow into the wound from the vessel lumen. Pearls and pitfalls of intervention use were recorded.
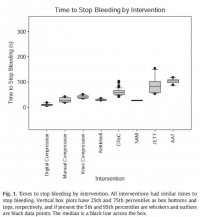
Interventions to control hemorrhage included medical device use, manual or digital compression, and improvised use of a rock-like kettlebell (to simulate a rock used in care on the battlefield in a case recorded in the Department of Defense Trauma Registry in 2012). Interventions included digital (finger) compression, manual compression (heel of the hand), knee compression, compression by a 50lb kettlebell (Hampton Fitness Products, Ventura, CA), and medical device use (Combat Ready Clamp, CRoC, Combat Medical Systems, Fayetteville, NC; SAM Junctional Tourniquet, SAM, SAM Medical Products, Portland, OR; Junctional Emergency Treatment Tool, JETT, North American Rescue Products, Greer, SC; Abdominal Aortic Tourniquet, AAT, Compression Works, Hoover, AL). The first device assessed was the CRoC which, of the devices studied, was cleared first by the US Food and Drug Administration on August 11, 2010. The first setting of the evaluation (which was for the CRoC) was in a simulation center as previously reported with three to five people, and the other setting of the evaluation was on a table with one to three people [5]. The data from that initial setting is included here for comparison of time to stop bleeding, blood loss volume, and device efficacy [5]. Since the blood loss rate was non-linear (as it is in real situations for casualties because bleeding is brisker initially rather than later), we did not refill the bladder after each iteration. The manikin was not designed to differentiate between performance of devices, so we only compared results to acceptable benchmarks. The benchmark for time to stop bleeding was 300 seconds (s), and the benchmark for blood loss was a normal adult male blood volume, 5 L. Hemorrhage was controlled with 100% efficacy in the manikin model for each intervention. The times to stop bleeding and volumes of blood lost were acceptable for all devices and iterations (Figs. 1 and 2; Tables 1 and 2). Advantages and disadvantages were learned with experience in the use of each intervention (Table 3). Traits of interventions varied through wide ranges (Table 4).


Les commentaires sont fermés.