05/04/2016
Victimes d'explosion: Pas de collier cervical
Cervical spine injuries in civilian victims of explosions: Should cervical collars be used?
Klein Y et Al. J Trauma Acute Care Surg. 2016 Mar 18. [Epub ahead of print]
---------------------------------------------------
En contexte de terrorisme civil, la pose d'un collier cervical apparaît plutôt inutile et source de perte de temps.
---------------------------------------------------
BACKGROUND:
Semi-rigid cervical collars (SRCC) are routinely applied to victims of explosions as part of the pre-hospital trauma protocols. Previous studies have shown that the use of SRCC in penetrating injuries is not justified due to the scarcity of unstable cervical spine injuries and the risk of obscuring other neck injuries. Explosion can inflict injuries by fragments penetration, blast injury, blunt force and burns. The study purpose was to determine the occurrence of cervical spine instability without irreversible neurological deficit and other potentially life threatening non-skeletal neck injuries among victims of explosions. The potential benefits and risks of SRCC application in explosion related injuries (ERI) was Evaluated.
METHODS:
a retrospective cohort study of all explosions civilian victims admitted to Israeli hospitals during the years 1998-2010. Data collection was based on the Israeli national trauma registry and the hospital records, and included demographic, clinical and radiological details of all patients with documented cervical spine injuries.
RESULTS:
the cohort included 2,267 patients. All of them were secondary to terrorist attacks. SRCC was applied to all the patients at the scene. Nineteen patients (0.83%) had cervical spine fractures. Nine patients (0.088%) had unstable cervical spine injury. All but one had irreversible neurological deficit on admission. 151 patients (6.6%) had potentially life threatening penetrating non-skeletal neck injuries.
CONCLUSIONS:
Unstable cervical spine injuries secondary to explosion are extremely rare. The majority of unstable cervical spine fractures were secondary to penetrating injuries, with irreversible neurological deficits on admission. The application of SRCC did not seem to be of any benefit in these patients and might pose a risk of obscuring other neck injuries. We recommend that SRCC will not be used in the pre-hospital management of victims of explosions.
LEVEL OF EVIDENCE:
Retrospective observational study, level III.
| Tags : immobilisation
19/12/2015
Amputé des jambes: Le bassin aussi !
The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices
Cross AM et Al. J R Nav Med Serv 2014;100(2):152-6
---------------------------------------------
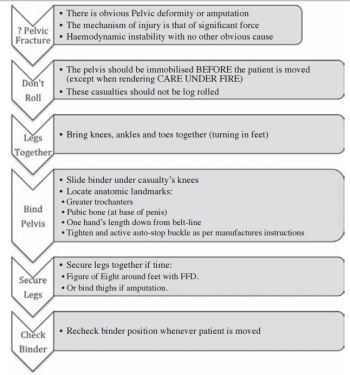
Excepté l'extraction d'urgence de blessés sous le feu, la prise en charge den cas d'amputation traumatique doit inclure la forte probabilité de traumatisme du bassin. Une utilisation large des immobilisations pelviennes doit donc être à l'esprit. On rappelle simplement la gravité et la difficulté de prise en charge des hémorragies liées aux fractures de bassin.
---------------------------------------------
AIMS:
A frequently-seen injury pattern in current military experience is traumatic lower limb amputation as a result of improvised explosive devices (IEDs). This injury can coexist with fractures involving the pelvic ring. This study aims to assess the frequency of concomitant pelvic fracture in IED-related lower limb amputation.
METHODS:
A retrospective analysis of the trauma charts, medical notes, and digital imaging was undertaken for all patients arriving at the Emergency Department at the UK military field hospital in Camp Bastion, Afghanistan, with a traumatic lower limb amputation in the six months between September 2009 and April 2010, in order to determine the incidence of associated pelvic ring fractures.
RESULTS:
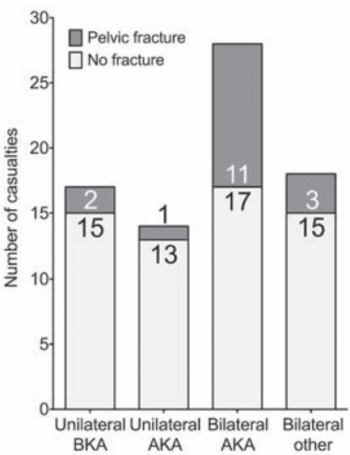
Of 77 consecutive patients with traumatic lower limb amputations, 17 (22%) had an associated pelvic fracture (eleven with displaced pelvic ring fractures, five undisplaced fractures and one acetabular fracture). Unilateral amputees (n = 31) had a 10% incidence of associated pelvic fracture, whilst 30 % of bilateral amputees (n = 46) had a concurrent pelvic fracture. However, in bilateral, trans-femoral amputations (n = 28) the incidence of pelvic fracture was 39%.
CONCLUSIONS:
The study demonstrates a high incidence of pelvic fractures in patients with traumatic lower limb amputations, supporting the routine pre-hospital application of pelvic binders in this patient group
| Tags : hémorragie, immobilisation, blast
19/07/2015
Immobilisation: Matériel spécifique ?
Improvised traction splints: a wilderness medicine tool or hindrance?
Weichenthal L et Al. Wilderness Environ Med. 2012 Mar;23(1):61-4
------------------------------------------------
Immobiliser un membre le plus tôt possible et ce de manière efficace est un des enjeux de la mise en condition d'évacuation. Il s'agit là de prévenir le mieux possible toute complication secondaire, de réduire le saignement et la douleur. Pour cela existe de nombreux équipements proposés par l'industrie. Miass sont ils vraiment utiles ? Pas si évident si l'on en croit le document proposé. Il pourrait exister à l'évidence des moyens simples et efficaces surtout moins coûteux d'atteindre ces objectifs.
------------------------------------------------
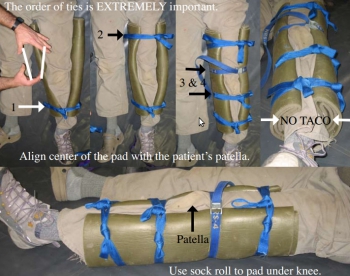
OBJECTIVES:
To investigate whether a traction splint made from improvised materials is as efficacious as commercially available devices in terms of traction provided and perceived comfort and stability.
METHODS:
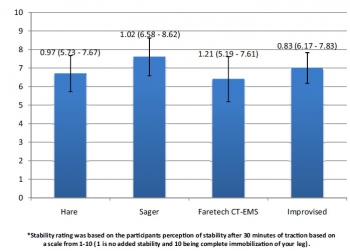
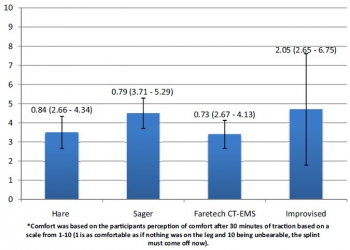
This was a prospective randomized crossover study utilizing 10 healthy, uninjured volunteers. The subjects were randomized to be placed in 4 different traction devices, in differing order, each for 30 minutes. Three of the traction splints are commercially available: The HARE, Sager, and Faretech CT-EMS. The fourth traction device was an improvised splint made as described in Medicine for the Backcountry: A Practical Guide to Wilderness First Aid. At the end of 30 minutes the pounds of force created by each device was measured. The volunteers were also asked at that time to subjectively report the comfort and stability of the splint separately on a scale from 1 to 10.
RESULTS:
All traction splints performed similarly with regard to the primary outcome measure of mean pounds of traction created at the end of 30 minutes of application with results ranging from 10.4 to 13.3 pounds. There was little difference reported by participants in regard to stability or comfort between the 4 traction devices.
CONCLUSIONS:
In this small pilot study, an improvised traction splint was not inferior to commercially available devices. Further research in needed in this area.
| Tags : immobilisation
07/07/2015
Quelle attelle de fémur ?
Evaluation of commercially available traction splints for battlefield use
Studer NM et All. J Spec Oper Med. 2014 Summer;14(2):46-55
------------------------------------------------------
L'immobilisation d'une fracture de fémur nécessite idéalement une traction. Les attelles de type thomas-lardenois ne sont pas utilisables en préhospitalier. La classique attelle de Donway n'est pas idéale dès lors que l'on est en combat à pied. Bien que l'intérêt de telles attelles reste discuté (1) , nous disposons à la nomenclature de l'atelle Faretec CT6. Le document présenté vante de manière très surprenante les qualités de l'attelle de slishman. Certes cette dernière semble plus rapide à poser mais avec un taux d'échec beaucoup plus important. La CT6 reste donc un excellent choix, c'est d'ailleurs ce qui est également dit dans ce document qui parait quelque peu orienté dans ces conclusions.
------------------------------------------------------
Background: Femoral fracture is a common battlefield injury with grave complications if not properly treated. Traction splinting has been proved to decrease morbidity and mortality in battlefield femur fractures. However, little standardization of equipment and training exists within the United States Armed Forces. Currently, four traction splints that have been awarded NATO Stock Numbers are in use: the CT-6 Leg Splint, the Kendrick Traction Device (KTD), the REEL Splint (RS), and the Slishman Traction Splint (STS).
Objective: The purpose of this study was to determine the differences between the four commercially available traction devices sold to the U.S. Government.
Methods: After standardized instruction, subjects were timed and evaluated in the application of each of the four listed splints. Participant confidence and preferences were assessed by using Likertscaled surveys. Free response remarks were collected before and after timed application.
Results: Subjects had significantly different application times on the four devices tested (analysis of variance [ANOVA], p < .01). Application time for the STS was faster than that for both the CT-6 (t-test, p < .0028) and the RS (p < .0001). Subjects also rated the STS highest in all post-testing subjective survey categories and reported significantly higher confidence that the STS would best treat a femoral fracture (p < .00229).
Conclusions: The STS had the best objective performance during testing and the highest subjective evaluation by participants. Along with its ability to be used in the setting of associated lower extremity amputation or trauma, this splint is the most suitable for battlefield use of the three devices tested
| Tags : immobilisation
26/03/2015
Techniques d'immobilisations
| Tags : immobilisation
03/03/2015
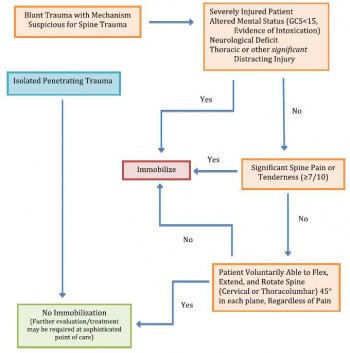
Stabilisation du rachis: C'est particulier en milieu hostile
Recommandation 1 (grade:1C) :
Neutral alignment should be restored and maintained with light or moderate manual cervical traction during extrication, unless such a maneuver is met with resistance, increased pain, or new or worsening neurologic deficit.
Recommandation 2 (grade:1C):
Patients requiring extrication, when the cervical spine cannot be cleared before extrication, should be placed in a cervical collar and allowed to exit the situation under their own volition if alert and reliable. Otherwise extrication should be performed with a KED (or similar device) plusc ervical collar,and the immobilized patient moved in a sitting position onto a long spine board, vacuum mattress, orsimilar device.
Recommandation 3 (grade:1C):
The lift and slide transfer with trap squeeze is preferred to the log roll when transferring patients to and from a backboard
Recommandation 4 (grade:2C):
Spinal immobilization should be considered in patients with evidence of spinal injury, including those with neurologic injury, and those patients who have experienced severe trauma and are unconscious or exhibit altered mental status.
Recommandation 5 (grade:2B):
The cervical collar (or improvised equivalent) should beconsidered one ofs everal tools available to aid in immobilization of the cervical spine. It should not be considered adequate immobilization in and of itself, nor should it beconsidered necessary if adequate immobilization can be accomplished by other means, or if the presence of the collar in itself compromises emergent patient care.
Recommandation 6 (grade:1B):
Use of the cervical collar is contraindicated in ankylosing spondylitis. Patients with suspected injury should hav etheir neck supported in a position of comfort
Recommandation 6 (grade:1C):
Vacuum mattress provides superior immobilization, with or without a standard cervical collar, and improved patient comfort (with corresponding decreased risk of pressure sores) and is preferred over a backboard for immobilization of either the entire spine or specific segments of concern.
Recommandation 6 (grade:1A):
Appropriately trained personnel, using either the NEXUS criteria or the Canadian C- spine rule, can safely and effectively make decisions in the prehospital setting about whether or not ac ervical spine should be immobilized.
Recommandation 7(grade:1B):
Spinal immobilization should not be performed in the presence of penetrating trauma
Clic sur l'image pour accéder au document
| Tags : rachis, immobilisation
Tapis de sol: Pour immobiliser
| Tags : immobilisation
23/09/2014
Stabilisation pelvienne:
Les attelles de type Sam Splint sont INCONTOURNABLES en médecine militaire comme on peut le voir dans une brochure spécifique. Certains proposent de l'utiliser comme base d'une stabilisation pelvienne.
| Tags : immobilisation, pelvis
20/11/2011
Stabilisation pelvienne: Au bon niveau
Ce document est à mettre en lien avec l'impotrance d'un positionnement correct de ces dispositifs. Il s'agit seulement d'une fois sur 2 d'un positionnement au niveau des grands trochanter. Dans près de 40% des cas le positionnement était trop haut.
| Tags : immobilisation, pelvis
Stabilisation pelvienne: Sam Sling, Tpod ou autre chose ?
Une présentation d'une publication portant sur la comparaison du T Pod, de la Sam Pelvic sling et du Pelvic binder qui sont les 3 dispositifs les plus couramment utilisés.
http://www.medicalsca.com/files/jb__js_-_pelvic_devices_c...
| Tags : immobilisation, pelvis
Pelvic Fracture Hemorrhage—Update and Systematic Review
| Tags : immobilisation, pelvis