18/02/2016
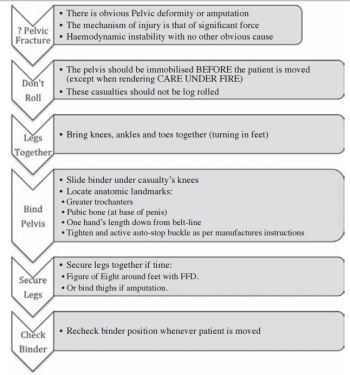
Stabilisation pelvienne: Les genoux sont importants
Pelvic pressure changes after a fracture: A pilot cadaveric study assessing the effect of pelvic binders and limb bandaging
Morris R et Al. Injury http://dx.doi.org/10.1016/j.injury.2015.12.009
-------------------------
Stabiliser un bassin pour lequel il existe une suspicion de fracture est une des composantes majeures du sauvetage au combat. Ceci vise à réduire la mortalité par hémorragie non garrotable ou non comprimable. Il existe des ceintures spécifiques pour cela. Ce travail est intéressant car il illustre la complémentarité des ceintures pelviennes ET de l'immobilisation des genoux. Cette dernière permet à elle seule d'augmenter la pression intra-abdominale et partant probablement de réduire le saignement. Donc n'oublier pas d'immobiliser les genoux. Que vous disposez ou pas de ceinture pelvienne, cela sert.
-------------------------
Objectives: Pelvic binders are a life-saving intervention for hypovolaemic shock following displaced pelvic fractures, thought to act through increasing intra-pelvic pressure to reduce venous bleeding. This cadaveric study assesses changes in intra-pelvic pressure with different binders augmented by bandaging the thighs to recruit the femora as levers to close the pelvis. Access to femoral vessels via an in situ binder was also assessed.
Methods: Two embalmed cadavers were used with unstable pelvic injuries (OA/OTA 61-C1) created through disrupting the pelvic ring anteriorly and posteriorly. To measure intravesical pressure, which reflects intra-pelvic pressure, a supra-pubic catheter was inserted and connected to a water manometer whilst a spigot was placed in a urethral catheter to reduce leakage of fluid. The common and superficial femoral arteries were dissected in the left groin for each specimen prior to any intervention to allow inspection following binder application. A SAM pelvic sling II, Trauma Pelvic Orthotic Device (T-POD), Prometheus pelvic splint and an improvised pelvic binder were used on each cadaver, with each applied following lower limb bandaging with the knees slightly flexed. The groins were then inspected to assess if the femoral vessels were visible. Statistical analysis was performed in SPSS using a paired samples t test to determine if any difference existed between initial pelvic pressure in specimens compared to pressures with bandaging on and binders applied.
Results: Bandaging the lower limbs alone produced a significant increase in both peak and steady mean intra-pelvic pressure, 15.69 cmH2O and 12.38 cmH2O, respectively, compared to the baseline pressure, 8.73 cmH2O (p = 0.002 and p = 0.001, respectively). Applying the pelvic binder with the bandaging in place increased intra-pelvic pressure compared to the baseline (peak pressure of 25.38 cmH2O (p < 0.001) and steady pressure of 15.13 cmH2O (p = 0.003)). Steady mean pressures between bandaging alone and bandaging with the binder applied were not significantly different (p = 0.09), whilst the peak pressures were significantly greater when the binder was applied (p = 0.005). The improvised binder and T-POD both required cutting to access the femoral vessels which resulted in decreasing efficacy.
Conclusions: Intra-pelvic pressure was significantly increased through bandaging the lower limbs alone, and this represents a simple measure to increase intra-pelvic pressure and therefore efficacy of the binder. Access to the femoral vessels varied with binder type and represents an important consideration in polytrauma patients.
21/01/2016
Le graal plaquettaire hémostatique ?
Thrombosomes: a platelet-derived hemostatic agent for control of noncompressible hemorrhage
Fitzpatrick GM et Al. Transfusion. 2013 Jan;53 Suppl 1:100S-106S
----------------
Un thrombosome est en quelque sorte une plaquette lyophilisée dans laquelle l'eau est remplacée par un sucre particulier: le trehalose. Ré exposé à une atmosphère humide, il se réhydrate pour retrouver toutes ses propriétés. Cela ne semble pas être une simple théorie car il initierait une génération de thrombine permettant la formation d'un caillot de manière satisfaisante. Des thrombosmes, du fibrinogène et du PLyo, on peut espérer !
----------------
BACKGROUND: Uncontrolled hemorrhage is responsible for ~80% of the potentially survivable deaths in combat and over 40% of early mortality in the under 65 age group in the United States. Providing an easily used infusible hemostatic agent to first responders could significantly reduce these fatalities. We report on an infusible lyophilized platelet-derived hemostatic agent stabilized with trehalose and polysucrose prior to and during lyophilization.
STUDY DESIGN AND METHODS: Characterization included determining the particle population size range, surface marker expression GPIb, GPIIbIIIa, and Annexin V binding. Function was assessed by aggregation, thromboelastography, and thrombin generation. Pharmacokinetics, biodistribution, and immunogenicity established using Indium111 labeled Thrombosomes in healthy New Zealand white rabbits (NZWRs), efficacy in thrombocytopenic NZWR, and safety in NZWRs, canines, and nonhuman primates.
RESULTS: Thrombosomes retained GPIIbIIIa expression (98.71% 0.18 of the rehydrated particles), a reduced expression of GPIb (47.77% 6.65), and Annexin V binding (86.05% 2.65). Aggregation to all agonists except thrombin in buffer (78.15% 2.5) was <50%. Thrombin generation and thromboelastography results demonstrated a concentration gradient that was consistent from lot to lot. There were no observed adverse events in any safety study and blood loss was reduced by >80% in the thrombocytopenic ear bleed model.
CONCLUSION: Our in vitro characterization studies in conjunction with preclinical animal safety and efficacy studies demonstrated lot consistency in manufacturing, maintenance of hemostatic functions of Thrombosomes, safety at high dose concentrations, and the potential to provide an effective hemostatic agent at the site of injury.
09/01/2016
1/1/1 ou 1/1/2 ?
Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial
Holcomb JB et All. JAMA Surg. 2013 Feb;148(2):127-36
______________________________
La reconnaissance et la mise en place de la meilleure stratégie thérapeutique du choc hémorragique traumatique sont des enjeux fondamentaux qui se posent aux équipes de réanimation préhospitalières et hospitalières. L'application du concepts du damage control resuscitation (1) vise par la mise en place d'un stratégie raisonnée d'arrêt des hémorragies (2), d'un remplissage vasculaire mesuré (3) et d'une politique transfusionnelle spécifique (4). Parmi ces mesures, il apparaît important de garantir l'apport équilibré de plasma, de plaquettes et de CGR dans un ration élevé 1/1/1 ou 1/1/2. Deux études se sont attachées à ce point: L'étude PROMMTT et l'étude PROPPR ici présentée. La première confirme le bénéfice d'une telle stratégie avec une moindre mortalité chez les patients bénéficiant de rapport élevé supérieur mais uniquement dans les 6 premières heures. L'étude PROPPR semble confirmer ces données avec une moindre mortalité précoce par hémorragie mais ne réussit pas à confirmer l'intérêt d'un ratio 1/1/1 par rapport à un ratio 1/1/2 sur la mortalité à long terme.
______________________________
IMPORTANCE:
Severely injured patients experiencing hemorrhagic shock often require massive transfusion. Earlier transfusion with higher blood product ratios (plasma, platelets, and red blood cells), defined as damage control resuscitation, has been associated with improved outcomes; however, there have been no large multicenter clinical trials.
OBJECTIVE:
To determine the effectiveness and safety of transfusing patients with severe trauma and major bleeding using plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio.
DESIGN, SETTING, AND PARTICIPANTS:
Pragmatic, phase 3, multisite, randomized clinical trial of 680 severely injured patients who arrived at 1 of 12 level I trauma centers in North America directly from the scene and were predicted to require massive transfusion between August 2012 and December 2013.
INTERVENTIONS:
Blood product ratios of 1:1:1 (338 patients) vs 1:1:2 (342 patients) during active resuscitation in addition to all local standard-of-care interventions (uncontrolled).
MAIN OUTCOMES AND MEASURES:
Primary outcomes were 24-hour and 30-day all-cause mortality. Prespecified ancillary outcomes included time to hemostasis, blood product volumes transfused, complications, incidence of surgical procedures, and functional status.
RESULTS:
No significant differences were detected in mortality at 24 hours (12.7% in 1:1:1 group vs 17.0% in 1:1:2 group; difference, -4.2% [95% CI, -9.6% to 1.1%]; P = .12) or at 30 days (22.4% vs 26.1%, respectively; difference, -3.7% [95% CI, -10.2% to 2.7%]; P = .26). Exsanguination, which was the predominant cause of death within the first 24 hours, was significantly decreased in the 1:1:1 group (9.2% vs 14.6% in 1:1:2 group; difference, -5.4% [95% CI, -10.4% to -0.5%]; P = .03). More patients in the 1:1:1 group achieved hemostasis than in the 1:1:2 group (86% vs 78%, respectively; P = .006). Despite the 1:1:1 group receiving more plasma (median of 7 U vs 5 U, P < .001) and platelets (12 U vs 6 U, P < .001) and similar amounts of red blood cells (9 U) over the first 24 hours, no differences between the 2 groups were found for the 23 prespecified complications, including acute respiratory distress syndrome, multiple organ failure, venous thromboembolism, sepsis, and transfusion-related complications.
CONCLUSIONS AND RELEVANCE:
Among patients with severe trauma and major bleeding, early administration of plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio did not result in significant differences in mortality at 24 hours or at 30 days. However, more patients in the 1:1:1 group achieved hemostasis and fewer experienced death due to exsanguination by 24 hours. Even though there was an increased use of plasma and platelets transfused in the 1:1:1 group, no other safety differences were identified between the 2 groups.
| Tags : hémorragie
25/12/2015
Transfusion de CGR: Les + graves seulement
Red Blood Cell Transfusion and Mortality in Trauma Patients: Risk-Stratified Analysis of an Observational Study
Perel P et Al. PLoS Med. 2014 Jun 17;11(6):e1001664
-------------------------------------
Les données qui suivent sont extraites de la cohorte des patients inclus dans l'étude CRASH2. Cette réinterprétation des données a pour objectif d'analyser le lien entre la mortalité à 28 jours et la transfusion de CGR. Les auteurs retrouvent un effet délétère de la transfusion de CGR pour les patients les moins à risque de mortalité. Ceci est en faveur des démarches de stratégies transfusionnelles sinon restrictives du moins raisonnées en fonction du contexte notamment préhospitalier où cette pratique associée à l'apport de fractions coagulantes semble être d'un grand intérêt(1).
-------------------------------------
Background:
Haemorrhage is a common cause of death in trauma patients. Although transfusions are extensively used in the care of bleeding trauma patients, there is uncertainty about the balance of risks and benefits and how this balance depends on the baseline risk of death. Our objective was to evaluate the association of red blood cell (RBC) transfusion with mortality according to the predicted risk of death.
Methods and Findings:
A secondary analysis of the CRASH-2 trial (which originally evaluated the effect of tranexamic acid on mortality in trauma patients) was conducted. The trial included 20,127 trauma patients with significant bleeding from 274 hospitals in 40 countries. We evaluated the association of RBC transfusion with mortality in four strata of predicted risk of death: ,6%, 6%–20%, 21%–50%, and .50%. For this analysis the exposure considered was RBC transfusion, and the main outcome was death from all causes at 28 days. A total of 10,227 patients (50.8%) received at least one transfusion. We found strong evidence that the association of transfusion with all-cause mortality varied according to the predicted risk of death (p-value for interaction ,0.0001). Transfusion was associated with an increase in all-cause mortality among patients with , 6% and 6%–20% predicted risk of death (odds ratio [OR] 5.40, 95% CI 4.08–7.13, p,0.0001, and OR 2.31, 95% CI 1.96–2.73, p,0.0001, respectively), but with a decrease in all-cause mortality in patients with .50% predicted risk of death (OR 0.59, 95% CI 0.47–0.74, p,0.0001). Transfusion was associated with an increase in fatal and non-fatal vascular events (OR 2.58, 95% CI 2.05–3.24, p,0.0001). The risk associated with RBC transfusion was significantly increased for all the predicted risk of death categories, but the relative increase was higher for those with the lowest (,6%) predicted risk of death (p-value for interaction ,0.0001). As this was an observational study, the results could have been affected by different types of confounding. In addition, we could not consider haemoglobin in our analysis. In sensitivity analyses, excluding patients who died early; conducting propensity score analysis adjusting by use of platelets, fresh frozen plasma, and cryoprecipitate; and adjusting for country produced results that were similar.
Conclusions:
The association of transfusion with all-cause mortality appears to vary according to the predicted risk of death. Transfusion may reduce mortality in patients at high risk of death but increase mortality in those at low risk. The effect of transfusion in low-risk patients should be further tested in a randomised trial.
| Tags : hémorragie
22/12/2015
Tourniquet: Contrefaçons=Danger
Le regain d'intérêt pour la mise en place de garrot en cas d'hémorragie massive des membres ne doit pas faire oublier deux choses: Avoir appris correctement et utiliser un matériel adhoc.
Concernant ce dernier point apparaissent sur le marché nombre de garrots qui soit n'ont pas été validés soit sont des contrefaçons de ce dernier, soit des garrots proposés dans le cadre d'activité de type Softball.
Plutôt que d'utiliser un garrot de piêtre qualité, il vaut probablement mieux avoir recours à un garrot artisanal dont l'efficacité n'est pas remise en cause sous réserve d'une technique de pose maîtrisée.
On rappelle que les 3 seuls garrots validés par l'armée américaine sont le CAT, le SOFTT et le Delfi EMT. Les SEULS garrots en service dans l'armée française sont le SOFTT et le Delfi EMT. Ces garrots sont produits par des industriels au terme de travaux de recherche et de démarche d'évolution et de politique qualité aboutis, toutes démarches absentes chez les copieurs et les contrefacteurs.
Tous les autres garrots n'ont pas suivis les mêmes process de développement, ce qui ne permet pas de garantir ni leur efficacité dans le temps, ni leur fiabilité.
Un exemple de copie du SOFTT est ici présenté
Un point d'alerte majeur aux USA
| Tags : tourniquet
20/12/2015
Coagulopathie: Du fibrinogène avant tout
Trauma-induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs
Nardi G et al. Critical Care (2015) 19:83
------------------------------------
Le damage control resuscitation fait largement appel à l'apport de plasma, concentrés de globules rouges et de plaquettes dans un rapport de 1/1/1 (1). Malgré la relative correction de la coagulopathie la survie à long terme ne semble pas être améliorée (2). Aussi certains proposent d'avoir plutôt recours à l'administration précoce de fibrinogène plutôt que l'administration de plasma. Le travail suivant qui propose l'apport précoce de 2g de fibrinogène est en faveur d'une telle démarche.
------------------------------------
INTRODUCTION:
Hemorrhage is the principal cause of death in the first few hours following severe injury. Coagulopathy is a frequent complication of critical bleeding. A network of Italian trauma centers recently developed a protocol to prevent and treat trauma-induced coagulopathy. A pre-post cohort multicenter study was conducted to assess the impact of the early coagulation support (ECS) protocol on blood products consumption,mortality and treatment costs.
METHODS:
We prospectively collected data from all severely injured patients (Injury Severity Score (ISS) >15) admitted to two trauma centers in 2013 and compared these findings with the data for 2011. Patients transfused with at least 3 units of packed red blood cells (PRBCs) within 24 hours of an accident were included in the study. In 2011, patients with significant hemorrhaging were treated with early administration of plasma with the aim of achieving a high (≥1:2) plasma-to-PRBC ratio. In 2013, the ECS protocol was the treatment strategy. Outcome data, blood product consumption and treatment costs were compared between the two periods.
RESULTS:
The two groups were well matched for demographics, injury severity (ISS: 32.9 in 2011 versus 33.6 in 2013) and clinical and laboratory data on admission. In 2013, a 40% overall reduction in PRBCs was observed, together with a 65% reduction in plasma and a 52% reduction in platelets. Patients in the ECS group received fewer blood products: 6.51 units of PRBCs versus 8.14 units. Plasma transfusions decreased from 8.98 units to 4.21 units (P <0.05), and platelets fell from 4.14 units to 2.53 units (P <0.05). Mortality in 2013 was 13.5% versus 20% in 2011 (13 versus 26 hospital deaths, respectively) (nonsignificant). When costs for blood components, factors and point-of-care tests were compared, a €76,340 saving in 2013 versus 2011 (23%) was recorded.
CONCLUSIONS:
The introduction of the ECS protocol in two Italian trauma centers was associated with a marked reduction in blood product consumption, reaching statistical significance for plasma and platelets, and with a non-significant trend toward a reduction in early and 28-daymortality. The overall costs for transfusion and coagulation support (including point-of-care tests) decreased by 23% between 2011 and 2013.
| Tags : coagulopathie
19/12/2015
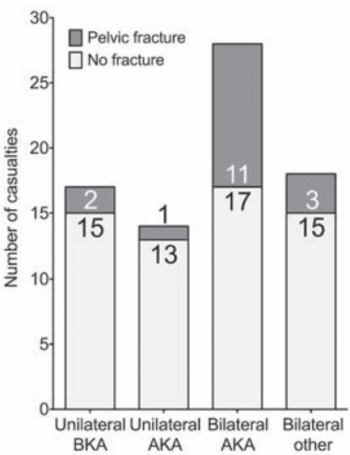
Amputé des jambes: Le bassin aussi !
The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices
Cross AM et Al. J R Nav Med Serv 2014;100(2):152-6
---------------------------------------------
Excepté l'extraction d'urgence de blessés sous le feu, la prise en charge den cas d'amputation traumatique doit inclure la forte probabilité de traumatisme du bassin. Une utilisation large des immobilisations pelviennes doit donc être à l'esprit. On rappelle simplement la gravité et la difficulté de prise en charge des hémorragies liées aux fractures de bassin.
---------------------------------------------
AIMS:
A frequently-seen injury pattern in current military experience is traumatic lower limb amputation as a result of improvised explosive devices (IEDs). This injury can coexist with fractures involving the pelvic ring. This study aims to assess the frequency of concomitant pelvic fracture in IED-related lower limb amputation.
METHODS:
A retrospective analysis of the trauma charts, medical notes, and digital imaging was undertaken for all patients arriving at the Emergency Department at the UK military field hospital in Camp Bastion, Afghanistan, with a traumatic lower limb amputation in the six months between September 2009 and April 2010, in order to determine the incidence of associated pelvic ring fractures.
RESULTS:
Of 77 consecutive patients with traumatic lower limb amputations, 17 (22%) had an associated pelvic fracture (eleven with displaced pelvic ring fractures, five undisplaced fractures and one acetabular fracture). Unilateral amputees (n = 31) had a 10% incidence of associated pelvic fracture, whilst 30 % of bilateral amputees (n = 46) had a concurrent pelvic fracture. However, in bilateral, trans-femoral amputations (n = 28) the incidence of pelvic fracture was 39%.
CONCLUSIONS:
The study demonstrates a high incidence of pelvic fractures in patients with traumatic lower limb amputations, supporting the routine pre-hospital application of pelvic binders in this patient group
| Tags : hémorragie, immobilisation, blast
17/12/2015
Tourniquet:Oui, mais bien posé= Serrer FORT
Evaluation of rapid training in ultrasound guided tourniquet application skills
Jaffer U. et Al. International Journal of Surgery 10 (2012) 563-567
-------------------------------------------------
Il existe actuellement un engouement justifié pour l'emploi du tourniquet comme moyen d'hémostase. Néanmoins il est important de rappeler que la pose d'un garrot a pour objectif l'arrêt d'un saignement important le plus souvent d'origine artérielle. Ils se doivent donc d'être serrés fort. Le travail proposé rappelle que la formation à la pose d'un garrôt n'est pas simplement sa manipulation mais qu'elle doit porter de manière spécifique sur les critères d'arrêt du saignement. En effet dans un modèle classique d'instruction de pose sur patient sain, les critères d'arrêt du serrage ne correspondent pas à ceux nécessaires en réel. Dans le travail proposé la pose à l'aveugle d'un garrot ne permet d'obtenir l'arrêt du saignement que dans moins d'1/4 à 1/5 des cas. Un enseignement donc à conduire par ceux qui en ont une pratique avancée. L'apport de simulateurs de saignement objectif comme celui du TOMMAN est certainement très intéressant.
Pour info: Fiche memento Garrot tactique
-------------------------------------------------
Tourniquet application has been widely accepted to improve survival for major limb trauma. Colour duplex ultrasound (US) can be used as a non-invasive method of confirming cessation of arterial flow. Participants with no or limited experience of ultrasound were taught to apply the Tourniquet with ultrasound guidance. Following this, participants were tested in effective tourniquet application: Blind and with ultrasound guidance. US guidance improved abolition of limb perfusion from 22 to 93 per cent in upper limb; from 25 to 100 per cent in lower limb (p ¼ 0.0027 and <0.0001).


Membre Sup Membre inf
No significant difference was found in application time for the lower limb; less time was taken for application with US guidance in the upper limb 8.1 (7.1, 8.6) vs 4.5 s (4.0, 5.3; median (IQR)), p ¼ 0.002. Tourniquet ultrasound skills are rapidly acquired by novice operators. Accuracy improves with ultrasound guidance, this may have a role in improving survival.
03/11/2015
Vers la machine à coaguler: Horizon 2040 ?
Deep Bleeder Acoustic Coagulation (DBAC)—part II: in vivo testing of a research prototype system
Sekins KM et Al. Sekins et al. Journal of Therapeutic Ultrasound (2015) 3:17
Background:
Deep Bleeder Acoustic Coagulation (DBAC) is an ultrasound image-guided high-intensity focused ultrasound (HIFU) method proposed to automatically detect and localize (D&L) and treat deep, bleeding, combat wounds in the limbs of soldiers. A prototype DBAC system consisting of an applicator and control unit was developed for testing on animals. To enhance control, and thus safety, of the ultimate human DBAC autonomous product system, a thermal coagulation strategy that minimized cavitation, boiling, and non-linear behaviors was used.
Material and methods:

The in vivo DBAC applicator design had four therapy tiles (Tx) and two 3D (volume) imaging probes (Ix) and was configured to be compatible with a porcine limb bleeder model developed in this research. The DBAC applicator was evaluated under quantitative test conditions (e.g., bleeder depths, flow rates, treatment time limits, and dose exposure time limits) in an in vivo study (final exam) comprising 12 bleeder treatments in three swine. To quantify blood flow rates, the “bleeder” targets were intact arterial branches, i.e., the superficial femoral artery (SFA) and a deep femoral artery (DFA). D&L identified, characterized, and targeted bleeders. The therapy sequence selected Tx arrays and determined the acoustic power and Tx beam steering, focus, and scan patterns. The user interface commands consisted of two buttons: “Start D&L” and “Start Therapy.” Targeting accuracy was assessed by necropsy and histologic exams and efficacy (vessel coagulative occlusion) by angiography and histology.
Results:
The D&L process (Part I article, J Ther Ultrasound, 2015 (this issue)) executed fully in all cases in under 5 min and targeting evaluation showed 11 of 12 thermal lesions centered on the correct vessel subsection, with minimal damage to adjacent structures. The automated therapy sequence also executed properly, with select manual steps. Because the dose exposure time limit (tdose ≤ 30 s) was associated with nonefficacious treatment, 60-s dosing and dual-dosing was also pursued. Thrombogenic evidence (blood clotting) and collagen denaturation (vessel shrinkage) were found in necropsy and histologically in all targeted SFAs. Acute SFA reductions in blood flow (20–30 %) were achieved in one subject, and one partial and one complete vessel occlusion were confirmed angiographically. The complete occlusion case was achieved with a dual dose (90 s total exposure) with focal intensity ≈500 W/cm2 (spatial average, temporal average).
23/10/2015
Quelle place pour les facteurs de la coagulation ?
| Tags : hémorragie, coagulopathie, choc
30/09/2015
REBOA: Un savoir faire à maîtriser ?
Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage
Moor LJ et Al. J Trauma Acute Care Surg. 2015;79: 523-532
L'application du concept du garrot tactique a fait évoluer la répartition des causes évitables de décès à l'avant et met actuellement au premier plan les hémorragies du tronc (Eastridge) . SI le bon usage du garrot reste un enjeu essentiel, les efforts portent maintenant sur la prise en charge d'une part des hémorragies jonctionnelles avec le recours de dispositifs tels que le CRoC, le Sam Junctional tourniquet ou l'abdominal tourniquet et d'autre part sur la prise en charge des hémorragies du tronc. Une autre approche, connue depuis de nombreuses années mais tombée en désuétude, refait surface. L'occlusion endovasculaire de l'aorte abdominale apparaît être d'un intérêt certain. C'est ce que documente le travail présenté ci dessous. Réaliser un tel geste en préhospitalier est possible (1,2). En ce qui concerne les applications militaires dans les structures chirurgicales de role 2 voire dans certaines moyens de transport préhospitalier une réflexion apparaît nécessaire.
------------------------------------------
BACKGROUND:
Hemorrhage remains the leading cause of death in trauma patients. Proximal aortic occlusion, usually performed by direct aortic cross-clamping via thoracotomy, can provide temporary hemodynamic stability, permitting definitive injury repair. Resuscitative endovascular balloon occlusion of the aorta (REBOA) uses a minimally invasive, transfemoral balloon catheter, which is rapidly inserted retrograde and inflated for aortic occlusion, and may control inflow and allow time for hemostasis. We compared resuscitative thoracotomy with aortic cross-clamping (RT) with REBOA in trauma patients in profound hemorrhagic shock.
METHODS: Trauma registry data was used to compare all patients undergoing RTor REBOA during an 18-month period from two Level 1 trauma centers.
RESULTS: There was no difference between RT (n = 72) and REBOA groups (n = 24) in terms of demographics, mechanism of injury, or Injury Severity Scores (ISSs). There was no difference in chest and abdominal Abbreviated Injury Scale (AIS) scores between the groups. However, the RT patients had lower extremity AIS score as compared with REBOA patients (1.5 [0-3] vs. 4 [3-4],p G 0.001). Of the 72 RT patients, 45 (62.5%) died in the emergency department, 6 (8.3%) died in the operating room, and 14 (19.4%) died in the intensive care unit. Of the 24 REBOA patients, 4 (16.6%) died in the emergency department, 3 (12.5%) died in the operating room, and 8 (33.3%) died in the intensive care unit. In comparing location of death between the RT and REBOA groups, there were a significantly higher number of deaths in the emergency department among the RT patients as compared with the REBOA patients (62.5% vs. 16.7%, p G 0.001). REBOA had fewer early deaths and improved overall survival as compared with RT (37.5% vs. 9.7%, p = 0.003).
CONCLUSION: REBOA is feasible and controls noncompressible truncal hemorrhage in trauma patients in profound shock. Patients undergoing REBOA have improved overall survival and fewer early deaths as compared with patients undergoing RT.
| Tags : junctionnel
18/07/2015
Tourniquet et chaleur extrême ?
Laboratory testing of emergency tourniquets exposed to prolonged heat
Davidson JP et Al. J Spec Oper Med. 2015 Spring;15(1):34-8.
----------------------------------------------------------
Il a été démontré que la fiabilité mécanique des tourniquets pouvait être altérée si ces derniers n'étaient pas protégés (1,2,3). Le travail présenté porte sur l'effet de l'exposition prolongée à de hautes températures sur l'efficacité des garrots. Apparemment il n'y aurait pas d'effet propre.
----------------------------------------------------------
BACKGROUND:
Environmental exposure of tourniquets has been associated with component damage rates, but the specific type of environmental exposure, such as heat, is unknown. Emergency-tourniquet damage has been associated with malfunction and loss of hemorrhage control, which may risk loss of life during first aid. The purposes of the study are to determine the damage rate of tourniquets exposed to heat and to compare the rate to that of controls.
METHODS:
Three tourniquet models (Combat Application Tourniquet®; SOF® Tactical Tourniquet; Ratcheting Medical Tourniquet®) were tested using a manikin (HapMed Leg Tourniquet Trainer; www.chisystems.com) that simulates extremity hemorrhage. The study group of 15 tourniquets (five devices per model, three models) was exposed to heat (oven at 54.4° C [130° F] for 91 days), and 15 tourniquets similarly constituted the control group (unexposed to heat). Damage, hemorrhage control, distal pulse stoppage, time to effectiveness, pressure (mmHg), and blood loss volumes were measured.
RESULTS:
Three tourniquets in both groups had damage not associated with heat exposure (p = 1). Heat exposure was not associated with change in effectiveness rates (p = .32); this lack of association applied to both hemorrhage control and pulse stoppage. When adjusted for the effects of user and model, the comparisons of time to effectiveness and total blood loss were statistically significant (p < .0001), but the comparison of pressure was not (p = .0613).
CONCLUSION:
Heat exposure was not associated with tourniquet damage, inability to gain hemorrhage control, or inability to stop the distal pulse.
| Tags : tourniquet
17/07/2015
Tourniquet: Une histoire de pression pas si simple
Tourniquets and Occlusion: The Pressure of Design
Wall PL et Al. Mil Med. 2013 May;178(5):578-87
-----------------------------------------------
Un travail très intéressant qui exprime bien que l'efficacité d'un garrot nécessite un ensemble de gestes parfaitement réalisés, notamment un serrage suffisant qui doit être vérifié après la pose. Il existe en effet avec les garrots de type tourniquet ou pneumatique une chute plus ou moins importante de la pression d'occlusion donc de perte d'occlusion, ce d'autant qu'un relâchement musculaire peut apparaître réduisant d'autant plus cette pression d'occlusion. Les garrots élastiques n'aurait pas cet inconvénient.
-----------------------------------------------
Abstracts: Nerve injuries result from tourniquet pressure. The objective was to determine arterial occlusion and completion pressures with the 3.8-cm-wide windlass Combat Application Tourniquet (CAT) and the 10.4-cm-wide Stretch, Wrap, and Tuck Tourniquet (SWAT-T).
Methods: Sixteen volunteers self-applied and had tourniquets applied to their thighs and arms (CAT and SWAT-T, random order, then blood pressure cuffs).
Results: Occlusion (Doppler signal elimination) pressures were higher than predicted ( p < 0.0001), highest with the CAT ( p < 0.0001), and often lower than completion pressures (completion median, range: CAT 360, 147–745 mm Hg; SWAT-T 290, 136–449 mm Hg; cuff 184, 108–281 mm Hg). Three CAT thigh and 9 CAT arm completion pressures were >500 mm Hg. Pressure decreases and occlusion losses occurred over 1 minute (pressure decrease: CAT 44 ± 33 mm Hg; SWAT-T 6 ± 8 mm Hg; cuff 14 ± 19 mm Hg; p < 0.0001; loss/initially occluded: CAT 17 of 61, SWAT-T 5 of 61, cuff 40 of 64, p < 0.01). CAT pressures before turn did not have a clear relationship with turns to occlusion.
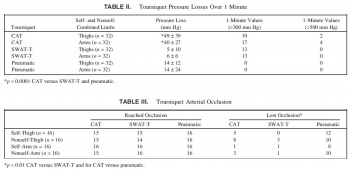 Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss.
| Tags : tourniquet
21/03/2015
Tourniquet: Efficace, uniquement si serré fort
Forward Assessment of 79 Prehospital Battlefield Tourniquet Use in the Current War
King DR et Al. J Spec Oper Med. 2012 Winter;12(4):33-8.
----------------------------------------------------------------------
La pose libérale d'un garrot est présentée comme étant un facteur essentiel de survie des blessés des membres. Encore faut il que ces derniers soient posés de manière correcte. Le document présenté laisse planer un gros doute. En effet il met en évidence qu'un garrot est mis en place 3 fois sur 4 alors qu'il n'y a pas de lésion vasculaire notable et que la plupart des garrots posés ne sont pas suffisamment serrés et sont en fait des garrots veineux. Pire seuls 1/3 des blessés ayant des lésions artérielles se voient appliquer un garrot artériel. C'est dire qu'une attention particulière doit être portée sur l'abolition du pouls artériel distal. Il s'agit là d'un enjeu pédagogique majeur.
----------------------------------------------------------------------
Introduction:
Battlefield tourniquet use can be lifesaving, but most reports are from hospitals with knowledge gaps remaining at the forward surgical team (FST). The quality of tourniquet applications in forward settings remain unknown. The purpose of this case series is to describe observations of tourniquet use at an FST in order to improve clinical performance.
Methods:
War casualties with tourniquet use presenting to an FST in Afghanistan in 2011 were observed. We identified appliers by training, device effectiveness, injury pattern, and clinical opportunities for improvement. Feedback was given to treating medics.
Results:
Tourniquet applications (79) were performed by special operations combat medics (47, 59%), flight medics (17, 22%), combat medics (12, 15%), and general surgeons (3, 4%). Most tourniquets were Combat Application Tourniquets (71/79, 90%). With tourniquets in place upon arrival at the FST, most limbs (83%, 54/65) had palpable distal pulses present; 17% were pulseless (11/65). Of all tourniquets, the use was venous in 83% and arterial in 17%. In total, there were 14 arterial injuries, but only 5 had effective arterial tourniquets applied.
Discussion:
Tourniquets are liberally applied to extremity injuries on the battlefield. 17% were arterial and 83% were venous tourniquets. When ongoing bleeding or distal pulses were appreciated, medics tightened tourniquets under surgeon supervision until distal pulses stopped. Medics were generally surprised at how tight a tourniquet must be to stop arterial flow–convert a venous tourniquet into an arterial tourniquet. Implications for sustainment training should be considered with regard to this life-saving skill.
| Tags : tourniquet, garrot, hémorragie
13/01/2015
Attentats: Importance du garrot
The Initial Response to the Boston Marathon Bombing. Lessons Learned to Prepare for the Next Disaster
Gates JD et AL. Ann Surg. 2014 Dec;260(6):960-6
-----------------------------------------------------------------------------------
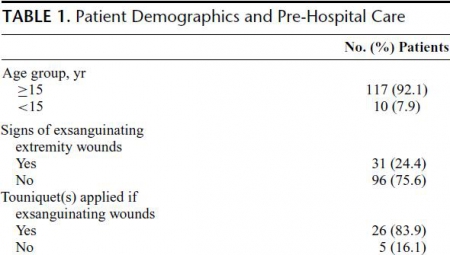
Le concept du garrot tactique est familier aux équipes militaires. L'expérience rapportée montre que ce concept doit également le devenir dans le monde de la médecine préhospitalière. 26 soit près de 10% blessés pris en charge ont fait l'objet d'une pose de garrot. Ainsi en cas d'attentat la pose précoce d'un garrot en cas d'hémorragie des membres est elle une mesure fondamentale de mise en condition de survie.
-----------------------------------------------------------------------------------
OBJECTIVE:
We discuss the strengths of the medical response to the Boston Marathon bombings that led to the excellent outcomes. Potential shortcomings were recognized, and lessons learned will provide a foundation for further improvements applicable to all institutions.
BACKGROUND:
Multiple casualty incidents from natural or man-made incidents remain a constant global threat. Adequate preparation and the appropriate alignment of resources with immediate needs remain the key to optimal outcomes.
METHODS:
A collaborative effort among Boston's trauma centers (2 level I adult, 3 combined level I adult/pediatric, 1 freestanding level I pediatric) examined the details and outcomes of the initial response. Each center entered its respective data into a central database (REDCap), and the data were analyzed to determine various prehospital and early in-hospital clinical and logistical parameters that collectively define the citywide medical response to the terrorist attack.
RESULTS:
A total of 281 people were injured, and 127 patients received care at the participating trauma centers on that day. There were 3 (1%) immediate fatalities at the scene and no in-hospital mortality. A majority of the patients admitted (66.6%) suffered lower extremity soft tissue and bony injuries, and 31 had evidence for exsanguinating hemorrhage, with field tourniquets in place in 26 patients. Of the 75 patients admitted, 54 underwent urgent surgical intervention and 12 (22%) underwent amputation of a lower extremity.
CONCLUSIONS:
Adequate preparation, rapid logistical response, short transport times, immediate access to operating rooms, methodical multidisciplinary care delivery, and good fortune contributed to excellent outcomes.
| Tags : tourniquet, garrot, hémorragie
13/12/2014
Quikclot: Un bon choix, mais les autres aussi
Comparison of novel hemostatic dressings with QuikClot combat gauze in a standardized swine model of uncontrolled hemorrhage.
Rall JM et AL. J Trauma Acute Care Surg. 2013 Aug;75(2 Suppl 2):S150-6
L'emploi des pansements hémostatiques en médecine de l'avant est devenue une pratique courante, même si cette dernière s'appuie sur relativement peu d'arguments avérés. Leur efficacité repose sur leur application au contact de la lésion qui saigne et une compression initiale. Hors ces deux critères de performance sont pas toujours remplis en condition de combat. C'est ce qui explique que certains soient relativement critiques par rapport à leur intérêt réel en condition de combat et on insiste beaucoup actuellement sur la notion de pansement compressif et de packing de plaie. Il n'en demeure pas moins indispensable de connaître ce que propose l'industrie en la matière. Le document proposé fait le point sur le différents produits utilisables. Il utilise pour cela un modèle expérimental de plaie artérielle. Sont comparés trois produits le Quikclot, le Celox et le Chitogauze. 5 versions au total sont analysées car le Quikclot et le Celox sont proposés en deux versions qui diffèrent par leur masse.
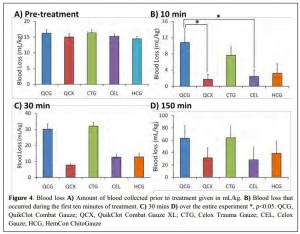

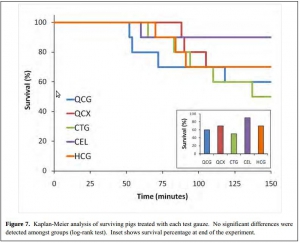
Très globalement plus la masse de produit est grande et plus l'efficacité est au rendez vous (Le Quikclot XL et le Celox, masse de 50 g de pansement) . Parmi les présentations qui proposent une masse de pansement de l'ordre de 20g l'Hemcon Chitogauze apparaît être immédiatement le plus efficace malheureusement est observé un pourcentage de resaignement élevé. Finalement de ce document on peut retenir que l'Hemcon Chitogauze, le CeloxTrauma gauze et le Quikclot Gauze ont des performances similaires. On remarque que pour le Quikclot Gauze la survie à 150 min est la plus élevée pour les pansements de 20 g, même si ceci n'est pas significatif au plan statistique. Ce dernier reste donc un très bon choix. Il est en dotation dans l'armée française .
On rappelle que ce dernier existe en deux version la version rolled et la version Z folded qui est plus particulièrement mise en avant par le fabricant pour les applications militaires.
07/12/2014
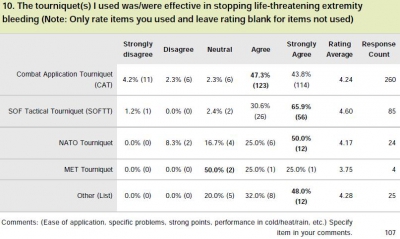
Tourniquet: Que disent les utilisateurs ?
Le garrot en dotation dans l'armée française est le Special Operation Tactical Tourniquet (SOFT-T) , concurrent du Combat Application Tourniquet (CAT). Il existe de nombreux travaux qui cherchent à comparer entre eux les divers produits proposés par l'industrie. Tel garrot semble plus efficace sur des modèles expériemetaux, un autre voit sa barre de torsion se briser, un autre est plus fragile que son concurrent lorsque les conditions de stockage ne sont pas optimales.

Une autre démarche consiste à demander à ceux qui les ont employé en conditions réelles. Une idée est donnée par le tableau qui suit et qui est tiré d'un questionnaire de suivi de mise en oeuvre des équipements du TCCC. Le modèle actuellement en dotation apparaît parfaitement adapté.
Clic sur l'image pour accéder au suivi des équipemens du TCCC
| Tags : tourniquet
01/11/2014
Garrot: A partir de quand est on fiable ?
Single versus Double Routing of the Band in the Combat Application Tourniquet.
J Spec Oper Med. 2013 Spring;13(1):34-41.
Le sauvetage au combat met en avant l'importance d'arrêter toute hémorragie le plus tôt possible. Le garrot tient là une place essentielle. Mais à partir de quand l'apprentissage de cette technique peut il être considéré comme optimal. Une réponse est apporté par ce travail: La maîtrise de ce geste semble être obtenue à partir de 30 poses.
Background: Common first aid tourniquets, like the Combat Application Tourniquet (CAT) of a windlass and band design, can have the band routed through the buckle in three different ways, and recent evidence indicates users may be confused with complex doctrine.
Objective: The purpose of the present study is to measure the differential performance of the three possible routings in order to better understand good tourniquet practice.
Methods: A training manikin was used by two investigators to measure tourniquet effectiveness, time to stop bleeding, and blood loss.
Results: The effectiveness rate was 99.6% (239/240) overall. Results were similar for both single-slit routings (inside vs. outside, p > 0.05). Effectiveness rates (yes-no results for hemorrhage control expressed as a proportion of iterations) were not statistically different between single and double routing. However, the time to stop bleeding and blood loss were statistically different (p < 0.05).
Conclusions: CAT band routing, through the buckle either singly or doubly, affects two key performance criteria: time to stop bleeding and volume of blood lost. Single routing proved to be faster, thereby saving more blood. Learning curves required to optimize user performance varied over 30-fold depending on which variable was selected (e.g., effectiveness vs. blood loss).
| Tags : tourniquet
N'oublions pas: Comprimer est essentiel
Laboratory assessment of out-of-hospital interventions to control junctional bleeding from the groin in a manikin model l.
Kragh JF et Al Am J Emerg Med. 2013 Aug;31(8):1276-8
Junctional body regions between the trunk and its appendages, such as the groin, are too proximal for a regular limb tourniquet to fit [1,2]. Not since 1993’s Black Hawk Down has junctional hemorrhage control become such a hot topic in military casualty care [1–7]. In February 2013, the US military’s Task Force Medical Afghanistan requested a fill of a gap in junctional hemorrhage control as an urgent operational need, meaning that junctional hemorrhage control devices should be considered urgently to fill a gap in medical care in war. A small but growing body of evidence indicates that hemorrhage control can be attained out-of-hospital with mechanical compression, using such interventions as medical devices, on a pressure point proximal to a bleeding wound [3–9]. To evaluate laboratory use of junctional hemorrhage control interventions, we gathered data on stopping groin bleeding in a manikin model to understand the plausibility of such interventions for future human subject research.
Under an approved protocol, we tested efficacy of interventions in a manikin designed to train medics in out-of-hospital hemorrhage control (Combat Ready Clamp [CRoC] Trainer Manikin, Operative Experience, Inc, North East, MD). We filled the blood reservoir with 4 liters of water; we refilled the reservoir after 5 iterations or 1.5 liters of lost fluid, whichever came first. The manikin had a right-groin gunshot wound through the proximal thigh where the common femoral artery flow was controllable by skin compression over it at the level of the inguinal fold. There was 3 cm between the pressure point where compression was applied and the proximal extent of the wound. Interventions were timed, blood loss was measured, and efficacy was noted. Efficacy was operationally defined as visually stopped flow into the wound from the vessel lumen. Pearls and pitfalls of intervention use were recorded.
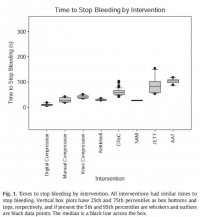
Interventions to control hemorrhage included medical device use, manual or digital compression, and improvised use of a rock-like kettlebell (to simulate a rock used in care on the battlefield in a case recorded in the Department of Defense Trauma Registry in 2012). Interventions included digital (finger) compression, manual compression (heel of the hand), knee compression, compression by a 50lb kettlebell (Hampton Fitness Products, Ventura, CA), and medical device use (Combat Ready Clamp, CRoC, Combat Medical Systems, Fayetteville, NC; SAM Junctional Tourniquet, SAM, SAM Medical Products, Portland, OR; Junctional Emergency Treatment Tool, JETT, North American Rescue Products, Greer, SC; Abdominal Aortic Tourniquet, AAT, Compression Works, Hoover, AL). The first device assessed was the CRoC which, of the devices studied, was cleared first by the US Food and Drug Administration on August 11, 2010. The first setting of the evaluation (which was for the CRoC) was in a simulation center as previously reported with three to five people, and the other setting of the evaluation was on a table with one to three people [5]. The data from that initial setting is included here for comparison of time to stop bleeding, blood loss volume, and device efficacy [5]. Since the blood loss rate was non-linear (as it is in real situations for casualties because bleeding is brisker initially rather than later), we did not refill the bladder after each iteration. The manikin was not designed to differentiate between performance of devices, so we only compared results to acceptable benchmarks. The benchmark for time to stop bleeding was 300 seconds (s), and the benchmark for blood loss was a normal adult male blood volume, 5 L. Hemorrhage was controlled with 100% efficacy in the manikin model for each intervention. The times to stop bleeding and volumes of blood lost were acceptable for all devices and iterations (Figs. 1 and 2; Tables 1 and 2). Advantages and disadvantages were learned with experience in the use of each intervention (Table 3). Traits of interventions varied through wide ranges (Table 4).

N'oublions pas le packing de plaie
A manikin model for study of wound-packing interventions to control out-of-hospital hemorrhage
Kragh JF et Al. Am J Emerg Med. 2014 Sep;32(9):1130-1
To the Editor,
With hemorrhage being the primary cause of mortality on the battlefield [1-3], wound-packing practice by US military medics in the wars since September 11, 2001, has changed from a conservative to an assertive approach. The foremost emphasis changed from preventing contamination to controlling hemorrhage. As no specific hemostatic dressings were available at the start of the wars, after such dressings were fielded, medics changed their approach by packing wounds with more gauze earlier in casualty care and deeper into subfascial cavitary wounds as a way to control hemorrhage. Although experienced medics and trainers favor an assertive approach, there is limited empirical evidence of improvements. In addition, with the development of various dressings with hemostatic properties [4-6], no systematic approach to trial wound-packing techniques easily has been developed. When a war ends and military medical care shifts toward peacetime duties and garrison work, skill sets in trauma care degrade as skill performance is less often. Furthermore, peacetime training reverts back toward everyday work such as sick call and away from future combat casualty care. The reversion tendency allows less training of new medics in combat casualty care than those who were trained during busy years of sustained combat; like nothing in peacetime, the present danger of combat during wartime focuses attention on hemorrhage control. A challenge for medics to be as well trained in peacetime in combat casualty care as during wartime is a recurring theme of military medicine.
Of the medical advances in prehospital combat casualty care during the current wars, we feel that the most important are regular tourniquets, junctional tourniquets, and wound packing because of their potential capacity to save numerous casualties from the most common cause of death on the battlefield—wound exsanguination. To not backslide on these 3 skills, we continue scholarly work to refine them. We call these skills the “Big 3,” and we have published mostly on tourniquets. To stimulate development of best practices in wound packing, we now focus the present report on an introductory test method to increase awareness of knowledge gaps within the science of wound packing.
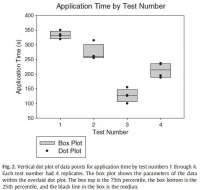
The purpose of the present study is to introduce a laboratory model of hemorrhage with data comparing gauze wound packing and medical device use to better understand out-of-hospital hemorrhage control. In an approved protocol, we used a manikin model designed for the capacity to train medics in techniques of gauze wound packing for hemorrhage control in trauma care. The manikin trainer (Combat Ready Clamp [CRoC] Trainer Manikin; Operative Experience, Inc, North East, MD) had a gunshot wound of the right groin that bled water from the common femoral artery; the wound track went through the thigh posterior to anterior. We measured blood volume lost from bleeding, the application time, and hemorrhage control (yes-no). We had only 1 user who had never packed a wound prehospital and had never been trained in this task. We made 4 tests. The first test was that we used a type of gauze (QuikClot Combat Gauze; Z-Medica, Wallingford, CT) alone in accordance with its instructions for use (IFU) except we used no overwrap for pressure; the overwrap is the fourth and final step of the gauze IFU. The second test was like the first, but we used the full IFU that included use of an overwrap (AirWrap, RevMedx, Wilsonville, OR). The third test was only the A manikin model for study of wound-packing interventions to control out-of-hospital hemorrhage
use of the overwrap and no gauze; this test included no inflation of the pneumatic bladder within the overwrap. The fourth test included the gauze, the overwrap, and the inflation of the overwrap. Each test had 4 replicates.
The results showed an apparent differential performance of the methods of hemorrhage control, but the test order indicated possible learning that may be a confounder. The fourth test performed better than the first 3 with respect to reduced blood loss (Fig. 1), which may mean that the fourth method is best or that the user learned with experience. Perhaps both are true. Application time also improved (Fig. 2), and the evaluation was sensitive enough to detect longer application times with additional steps in the wound-wrapping process.
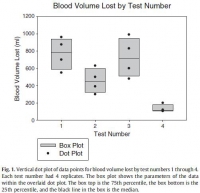

There was no surprise that the gauze performed better as indicated by reduced blood loss (Fig. 1) when it was used fully in accordance with its IFU in that the second test performed better than the first. In addition, there was no surprise that the overwrap performed better when it was used fully in accordance with its intent in that the fourth test performed better than the third since the overwrap was designed to wrap over gauze.
The strength of this report is that it introduces a method of analyzing wound-packing techniques that generated hypotheses for testing. Hypothesis-driven experiments will follow this hypothesis generating report to check differential performance of techniques such as preliminarily studied here. The method permits learning curve analysis to see how fast users can be in hemorrhage control; we have previously found that tourniquet use, for example, appears to take more than 30 tests before users flatten their learning curve [7].
Determining optimal care techniques and training regimens may help to improve clinical performance. The limitation of the present report is its introductory design; the preliminary finding is only able to generate hypotheses. Future directions include analyses of techniques and learning curves.
John F. Kragh Jr., MD
US Army Institute of Surgical Research
Joint Base San Antonio
Fort Sam Houston, TX
Uniformed Services University of the Health Sciences
F. Edward Hébert School of Medicine Bethesda, MD
Corresponding author at: US Army Institute of Surgical Research
Damage Control Resuscitation, 3698 Chambers Pass
Ste B, Joint Base San Antonio
Fort Sam Houston, TX
E-mail address: john.f.kragh.civ@mail.mil
John Steinbaugh
RevMedx, Inc, Wilsonville, OR
Donald L. Parsons, PA-C
Combat Medic Training
US Army Medical Department Center and School
Joint Base San Antonio, Fort Sam Houston, TX
Robert L. Mabry, MD
Emergency Medical Services Fellowship
San Antonio Military Medical Center
Joint Base San Antonio
Fort Sam Houston, TX
Bijan S. Kheirabadi, PhD
Michael A. Dubick, PhD
Damage Control Resuscitation
US Army Institute of Surgical Research
Joint Base San Antonio
Fort Sam Houston, TX
| Tags : packing