22/07/2018
Chitine: Prudence quand même ?
Chitin and Its Effects on Inflammatory and Immune Responses
-------------------------------------------
Les pansements hémostatiques à base de chitine sont largement utilisés et ne semblent pas actuellement poser de problème allergique (1). Néanmoins se pose la question de leur innocuité immune. Le développement des allergies croisées avec les produits dérivés de la mer et l'emploi de chitine comme complément alimentaire sont autant de facteurs de rencontre avec un allergène vrai. De telles allergies croisées s'observent également avec d'autres composants tels que la paravalbumine et le collagène des produits de la mer. Les pansements hémostatiques ne contenant pas de chitine ne semble pas exposer à ce risque potentiel.

-------------------------------------------
Chitin, a potential allergy-promoting pathogen-associated molecular pattern (PAMP), is a linear polymer composed of N-acetylglucosamine residues which are linked by β-(1,4)-glycosidic bonds. Mammalians are potential hosts for chitin-containing protozoa, fungi, arthropods, and nematodes; however, mammalians themselves do not synthetize chitin and thus it is considered as a potential target for recognition by mammalian immune system. Chitin is sensed primarily in the lungs or gut where it activates a variety of innate (eosinophils, macrophages) and adaptive immune cells (IL-4/IL-13 expressing T helper type-2 lymphocytes). Chitin induces cytokine production, leukocyte recruitment, and alternative macrophage activation. Intranasal or intraperitoneal administration of chitin (varying in size, degree of acetylation and purity) to mice has been applied as a routine approach to investigate chitin's priming effects on innate and adaptive immunity. Structural chitinpresent in microorganisms is actively degraded by host true chitinases, including acidic mammalian chitinases and chitotriosidase into smaller fragments that can be sensed by mammalian receptors such as FIBCD1, NKR-P1, and RegIIIc. Immune recognition of chitin also involves pattern recognition receptors, mainly via TLR-2 and Dectin-1, to activate immune cells to induce cytokine production and creation of an immune network that results in inflammatory and allergic responses. In this review, we will focus on various immunological aspects of the interaction between chitin and host immune system such as sensing, interactions with immune cells, chitinases as chitin degrading enzymes, and immunologic applications of chitin.
01/06/2018
Curare pour intuber: Oui, mais aussi !
Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review.
Il est communément admis que l'emploi de curares facilite l'intubation et réduit les complications liées à ce geste. C'est bien ce que confirme cette publication. Mais cette dernière conclue également à l'importance de peser le risque bénéfice risque. Dans les conditions extrêmes d'isolement et de prise en charge de trauma maxillo-faciaux/cranien ballistique l'objectif principal doit rester l'oxygénation des blessés/accidentés. Si l'induction en séquence rapide reste la référence, l'éventualité d'une intubation sans curare sous anesthésie locale doit être évoquée en cas de risque d'impossibilité de ventilation manuelle ou spontanée et de difficulté d'intubation. Dans tous les cas il reste nécessaire de pouvoir réaliser un abord chirurgical des voies aériennes.
Lire ici les recommandations de la SFAR: Intubation difficile en anesthésie, en réanimation
---------------------------------------------
Cohort studies have indicated that avoidance of neuromuscular blocking agents (NMBA) is a risk factor for difficult tracheal intubation. However, the impact of avoiding NMBA on tracheal intubation, possible adverse effects, and postoperative discomfort has not been evaluated in a systematic review of randomised trials. We searched several databases for trials published until January 2017. We included randomised controlled trials comparing the effect of avoiding vs using NMBA. Two independent authors assessed risk of bias and extracted data. The risk of random errors was assessed by trial sequential analysis (TSA). We included 34 trials (3565 participants). In the four trials judged to have low risk of bias, there was an increased risk of difficult tracheal intubation with no use of NMBA [random-effects model, risk ratio (RR) 13.27, 95% confidence interval (CI) 8.19-21.49, P<0.00001, TSA-adjusted CI 1.85-95.04]. The result was confirmed when including all trials, (RR 5.00, 95% CI 3.49-7.15, P<0.00001, TSA-adjusted CI 1.20-20.77). There was a significant risk of upper airway discomfort or injury by avoiding NMBA (RR=1.37, 95% CI 1.09-1.74, P=0.008, TSA-adjusted CI 1.00-1.86). None of the trials reported mortality. Avoiding NMBA was significantly associated with difficult laryngoscopy, (RR 2.54, 95% CI 1.53-4.21, P=0.0003, TSA-adjusted CI 0.27-21.75). In a clinical context, one must balance arguments for using NMBA when performing tracheal intubation.
03/01/2018
Fibrinogène: En 1er chez les canadiens
Fibrinogen Concentrate in the Special Operations Forces Environment
Sanders S et al. Military Medecine, 00, 0/0:1, 2017
------------------------------------
Un choix raisonné et différent (Apport de 6 g de fibrinogène) des armées françaises qui s'intègre dans les nouvelles stratrégies transfusionnelles de prise en charge du blessé de guerre où la place de la transfusion de sang frais le fibrinogène et le plasma ont une place essentielle (1,2)
Aller sur le forum coagulopathie
------------------------------------
Introduction:
Hemorrhage is the most common cause of death among Special Operations Force (SOF) soldiers. Bringing remote damage control resuscitation into the far-forward combat environment is logistically challenging, as it requires blood products that generally require a robust cold chain. Alternatively, lyophilized products such as fibrinogen concentrate, which does not require thawing or blood group compatibility testing before use, might be advantageous in damage control resuscitation in the battlefield. In this report, we review the evidence for the use of fibrinogen concentrate in the Canadian SOF environment.
Materials and Methods:
The literature on the use of fibrinogen concentrate in the trauma setting was reviewed by Canadian Forces Services Working Group, in three separate meetings. Multiple stakeholders were consulted to obtain authoritative perspectives from subject matter experts on the use of fibrinogen concentrate in the Canadian SOF environment.
We also conducted a comparison review of fibrinogen content, pathogen risk, shelf life, and methods required for use for fresh frozen plasma, cryoprecipitate, and fibrinogen concentrate relevant to their application in the far-forward combat environment.
Results:
Indications and a protocol for the use of fibrinogen as an adjunct to fresh whole blood were formulated based on a literature review and clinical expert opinion. Alternative strategies and other lyophilized blood products were considered before selecting fibrinogen concentrate as the lyophilized blood product of choice. Fibrinogen concentrate is an ABO-universal blood product with an excellent safety profile. Training was conducted by subject matter experts within civilian trauma centers and at military training facilities. The clinical efficacy and safety were confirmed by monitoring the use of fibrinogen concentrate in deployed combat settings.
Conclusion:
Fibrinogen concentrate is a useful adjunct to remote damage control resuscitation in the SOF environment. Fibrinogen concentrate was found to be robust for transport into the SOF environment and is widely accepted among SOF operators and medics
24/12/2017
AAST 2017: Utilité du TXA encore questionnée
Late TXA utilization is associated with Iincreased blood product transfusion: A secondary analysisof the pragmatic randomized optimal platelet and plasma ratios (PROPPR) study
Aravind K. et AL . Session: XIIIA: Papers 45-54: Preclincial/Translational Science Paper 52
-----------------------------------
Ce poster présenté au dernier AAST 2017 est une ré-interprétation de données de l'étude POPR. Il semblerait qu'au delà des premières heures l'administration précoce (dans la 1ère heure) de TXA n'améliore pas la survie à 24h et un mois. L'administration tardive (après la 1ère heure mais avant la 3ème) majorerait les besoins transfusionnels. Les auteurs de ce poster attirent l'attention sur la disparité des groupes comparés, ce qui peut expliquer leurs résultats.
-----------------------------------
Introduction:
Exsanguination is the leading cause of preventable death after trauma. In addition to a balanced ratio blood component strategy, tranexamic acid (TXA) is used as an adjunct in hemorrhaging patients. This secondary analysis was performed to determine the incidence of TXA utilization and outcome in patients predicted to receive a massive transfusion (MT) in level 1 trauma centers.
Methods:
Trauma patients who were predicted to require a MT and admitted to 12 level I North American trauma centers were studied. Patients were divided into those who received TXA and those who did not. We examined 3 hour, 24 hour, and 30 day mortality. We also examined incidence of thromboembolic events, blood product administration within the first 24 hours, length of stay (hospital free days), ICU free days, as well as development of complications including acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), sepsis, and multisystem organ failure (MOF). In our multivariate analysis, we controlled for Injury Severity Score (ISS), Glasgow Coma Scale (GCS), treatment group, mechanism of injury, hypotension and/or tachycardia on admission, geriatric patient (age > 65), and site as independent variables.
Results:
137 out of 680 (20.1%) patients in the PROPPR study received TXA with 130 patients receiving TXA within the first 3 hours after admission. Other adjunctive therapies administered included cryoprecipitate (25.4%), and others (6.6%). The incidence of TXA administration did not differ between the ratio groups (50.3% vs 47.4%, p=0.55), but patients receiving TXA were more severely injured with a median ISS of 34(21) vs 26(20), p<0.01 and a lower median(IQR) GCS of 9(12) vs 14(12), p<0.01. Multivariate linear regression analysis revealed no association between TXA administration and blood transfusion requirements (Table 1). Further analysis revealed that patients who received late (from >1 hour to ≤3 hours after arrival) TXA (41 patients) experienced increased blood requirements in the first 24 hours (Table 1) compared to those remaining 543 patients that did not receive TXA. There was no difference in blood product requirement in those patients who received TXA early (≤1 hour) (89 patients) versus those that did not receive TXA. In patients that receiv ed TXA, there was an increased incidence of ARDS(OR (95% CI) 1.99 (1.06,3.73), p=0.03), AKI (1.90 (1.13,3.20), p=0.01), and MOF (4.18 (1.52,11.48), p<0.01) even when controlling for the factors mentioned above. There was also a difference in adjusted 3 hour mortality (OR (95% CI) 0.22 (0.07,0.73), p=0.01) but not 24 hour (0.61 (0.30,1.24), p=0.18) or 30 day mortality (1.42 (0.78,2.59), p=0.25) for any TXA administration. There was no difference in adjusted thromboembolic events or adjusted length of stay. Subgroup analysis with additional variables that were found to have a difference between groups with a p<0.20 were added to the regression model including hematocrit, platelet count, international normalized ratio, creatinine, lactate, and R value on thrombelastography. This analysis showed an increase in PRBC transfusion with late TXA administration (16 out of 232 patients, 7.51 (0.46,14.56), p=0.04), but showed no difference in FFP or platelet administration.
Conclusion: Early TXA use was not associated with improved outcomes. Late TXA use was associated with increased blood product resuscitation. TXA administration in general was associated with improved 3 hour mortality. This did not translate to an improvement in mortality at 24 hours or 30 days. There was a significant increase in the incidence of ARDS, AKI, and MOF in patients who received TXA but this analysis is limited by the differences in the 2 populations despite attempts to control for them
08/05/2017
Hémorragie: De la glace sur le visage ?
Face Cooling Increases Blood Pressure during Simulated Blood Loss
B. Johnson et Al. Proceedings of Experimental Biology 2017 Chicago
-------------------------------------
Une constatation qui ne devrait pas surprendre ceux qui s'intéressent à la médecine de plongée et au réflexe d'immersion (1, 2, 3, 4), dont le facteur principal de déclenchement est l'exposition de la face à de l'eau froide.
-------------------------------------
Introduction
Blood loss causes central hypovolemia and in severe instances, it can decrease blood pressure and lead to cardiovascular decompensation. Simple and quick interventions that can be used to prevent cardiovascular decompensation in pre-hospital settings could be a valuable tool for first responsders. Cooling the forehead and cheeks using an ice/water slurry mixture has been shown to increase blood pressure for over 15 minutes. Therefore, face cooling could be used to mitigate decreases in blood pressure during blood loss.
Purpose
We tested the hypothesis that face cooling during simulated blood loss will increase blood pressure. Methods Ten healthy participants (22 ± 2 years, 3 women) completed two randomized trials on separate days. Both trials began with 30 mmHg of lower body negative pressure (LBNP) to simulate blood loss for 6 minutes. Then, either a 2.5 L plastic bag of an ice/water slurry mixture (0 ± 0°C) (LBNP+FC) or a 2.5 L plastic bag of thermoneutral water (34 ± 1°C) (LBNP+SHAM) was placed on the forehead and eyes and 30 mmHg of LBNP was maintained for an additional 15 minutes.

We continuously measured blood pressure (Penaz method), heart rate (ECG), stroke volume (Modelflow), cardiac output, total peripheral resistance, and forehead temperature throughout the protocol.
Results
Forehead temperature did not change from LBNP (34.2 ± 0.6°C) to LBNP+SHAM (33.9 ± 1.4°C, P > 0.999) and decreased from LBNP (34.4 ± 0.5°C) to LBNP+FC (11.0 ± 1.6°C, P < 0.001). Mean arterial pressure did not change from LBNP (82 ± 10 mmHg) to LBNP+SHAM (80 ± 8 mmHg, P = 0.978), but markedly increased during LBNP+FC. The peak increase from LBNP (77 ± 9 mmHg) was observed after 3 minutes of LBNP+FC (98 ± 15 mmHg, P < 0.001). Heart rate during LBNP (76 ± 14 bpm, P = 0.978) was not different from LBNP+SHAM (75 ± 13 bpm). Heart rate was lower throughout LBNP+FC beginning at 2 minutes of FC (60 ± 16 bpm) versus LBNP (80 ± 19 bpm, P < 0.001). Stroke volume did not change from LBNP (72 ± 15 mL) to LBNP+SHAM (67 ± 18 mL, P = 0.857). However, stroke volume increased from LBNP (78 ± 16 mL) to LBNP+FC, and peaked after 5 minutes of FC (97 ± 32 mL, P < 0.001). Cardiac output did not change from LBNP (5.4 ± 1.0 L/min) to LBNP+SHAM (4.9 ± 1.0 L/min, P > 0.415). Cardiac output slightly decreased from LBNP (6.2 ± 1.5 L/min) to 2 minutes of LBNP+FC (5.3 ± 1.6 L/min, P = 0.038). Total peripheral resistance did not change from LBNP (15.6 ± 3.7 mmHg/L/min) to LBNP+SHAM (17.3 ± 3.2 mmHg/L/min, P = 0.613). Total peripheral resistance throughout LBNP+FC was greater than LBNP. The peak increase in total peripheral resistance was observed after 2 minutes of LBNP+FC (20.0 ± 6.2 mmHg/L/min) versus LBNP (13.2 ± 3.9 mmHg/L/min, P < 0.001).
Conclusions
Face cooling during simulated moderate blood loss increases blood pressure through an increase in total peripheral resistance. Although more research is warranted, face cooling during blood loss is a potential simple and quick intervention that could delay cardiovascular decompensation. Support or Funding InformationUniversity at Buffalo IMPACT Award
| Tags : choc, hémorragie
15/01/2017
ISR: Plutôt kétamine ?
Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia.
Lyon RM et Al. Crit Care. 2015 Apr 1;19:134
-------------------------------------------
Faut-il utiliser la kétamine ou l'étomidate ? Le travail présenté milite pour l'emploi de la kétamine, mais ceci reste controversé (voir également ici)). C'est aussi le choix présenté dans la procédure du sauvetage au combat, du fait de la polyvalence d'emploi de la kétamine tant dans ses indications que de ses voies d'administration. On rappelle quand même que si l'ISR facilite grandement les conditions de l'intubation oro-trachéale en médecine préhospitalière métropolitaine, nos conditions spécifiques d'exercice ne correspondent pas à cette dernière. Avant de réaliser une telle induction, encore faut-il être valider l'indication de l'intubation au milieu de nulle part. Par ailleurs la réalisation de ce geste sous anesthésie locale doit également être envisagée. Ceci est conforme aux recommandations sur le sujet.
-------------------------------------------
INTRODUCTION:
Rapid Sequence Induction of anaesthesia (RSI) is the recommended method to facilitate emergency tracheal intubation in trauma patients. In emergency situations, a simple and standardised RSI protocol may improve the safety and effectiveness of the procedure. A crucial component of developing a standardised protocol is the selection of induction agents. The aim of this study is to compare the safety and effectiveness of a traditional RSI protocol using etomidate and suxamethonium with a modified RSI protocol using fentanyl, ketamine and rocuronium.
METHODS:
We performed a comparative cohort study of major trauma patients undergoing pre-hospital RSI by a physician-led Helicopter Emergency Medical Service. Group 1 underwent RSI using etomidate and suxamethonium and Group 2 underwent RSI using fentanyl, ketamine and rocuronium. Apart from the induction agents, the RSI protocol was identical in both groups. Outcomes measured included laryngoscopy view, intubation success, haemodynamic response to laryngoscopy and tracheal intubation, and mortality.
RESULTS:
Compared to Group 1 (n = 116), Group 2 RSI (n = 145) produced significantly better laryngoscopy views (p = 0.013) and resulted in significantly higher first-pass intubation success (95% versus 100%; p = 0.007). A hypertensive response to laryngoscopy and tracheal intubation was less frequent following Group 2 RSI (79% versus 37%; p < 0.0001). A hypotensive response was uncommon in both groups (1% versus 6%; p = 0.05). Only one patient in each group developed true hypotension (SBP < 90 mmHg) on induction.
CONCLUSIONS:
In a comparative, cohort study, pre-hospital RSI using fentanyl, ketamine and rocuronium produced superior intubating conditions and a more favourable haemodynamic response to laryngoscopy and tracheal intubation. An RSI protocol using fixed ratios of these agents delivers effective pre-hospital trauma anaesthesia.
15/12/2016
Sang total: Pas que chaud, de banque aussi
Coagulation function of stored whole blood is preserved for 14 days in austere conditions: A ROTEM feasibility study during a Norwegian antipiracy mission and comparison to equal ratio reconstituted blood.
BACKGROUND:
Formulation of a medical preparedness plan for treating severely bleeding casualties during naval deployment is a significant challenge because of territory covered during most missions. The aim of this study was to evaluate the concept of "walking blood bank" as a supportable plan for supplying safe blood and blood products.
METHODS:
In 2013, the Royal Norwegian Navy conducted antipiracy operations from a frigate, beginning in the Gulf of Aden and ending in the Indian Ocean. Crews were on 24-hour emergency alert in preparation for an enemy assault on the frigate. Under an approved command protocol, a "walking blood bank," using crew blood donations, was established for use on board and on missions conducted in rigid-hulled inflatable boats, during which freeze-dried plasma and leukoreduced, group O low anti-A/anti-B titer, cold-stored whole blood were stored in Golden Hour Boxes. Data demonstrating the ability to collect, store, and provide whole blood were collected to establish feasibility of implementing a whole blood-focused remote damage-control resuscitation program aboard a naval vessel. In addition, ROTEM data were collected to demonstrate feasibility of performing this analysis on a large naval vessel and to also measure hemostatic efficacy of cold-stored leukoreduced whole blood (CWB) stored during a period of 14 days. ROTEM data on CWB was compared with reconstituted whole blood.
RESULTS:
Drills simulating massive transfusion activation were conducted, in which 2 U of warm fresh whole blood with platelet sparing leukoreduction were produced in 40 minutes, followed by collection of two additional units at 15-minute increments. The ROTEM machine performed well during ship-rolling, as shown by the overlapping calculated and measured mechanical piston movements measured by the ROTEM device. Error messages were recorded in 4 (1.5%) of 267 tests. CWB yielded reproducible ROTEM results demonstrating preserved fibrinogen function and platelet function for at least 3.5 weeks and 2 weeks, respectively. The frequency of ROTEM tests were as follows: EXTEM (n = 88), INTEM (n = 85), FIBTEM (n = 82), and APTEM (n = 12). CWB results were grouped. Compared with Days 0 to 2, EXTEM maximum clot firmness was significantly reduced, beginning on Days 10 to 14; however, results through that date remained within reference ranges and were comparable with the EXTEM maximum clot firmness for the reconstituted whole blood samples containing Day 5 room temperature-stored platelets.
CONCLUSION:
A "walking blood bank" can provide a balanced transfusion product to support damage-control resuscitation/remote damage-control resuscitation aboard a frigate in the absence of conventional blood bank products. ROTEM analysis is feasible to monitor damage-control resuscitation and blood product quality. ROTEM analysis was possible in challenging operational conditions.
| Tags : coagulopathie, transfusion
11/12/2016
Suppression métabolique ?
Inducing metabolic suppression in severe hemorrhagic shock: Pilot study results from the Biochronicity Project.
BACKGROUND:
Suspended animation-like states have been achieved in small animal models, but not in larger species. Inducing metabolic suppression and temporary oxygen independence could enhance survivability of massive injury. Based on prior analyses of key pathways, we hypothesized that phosphoinositol-3-kinase inhibition would produce metabolic suppression without worsening organ injury or systemic physiology.
METHODS:
Twenty swine were studied using LY294002 (LY), a nonselective phosphoinositol-3-kinase inhibitor. Animals were assigned to trauma only (TO, n = 3); dimethyl sulfoxide only (DMSO, n = 4), LY drug only (LYO, n = 3), and drug + trauma (LY + T, n = 10) groups. Both trauma groups underwent laparotomy, 35% hemorrhage, severe ischemia/reperfusion injury, and protocolized resuscitation. Laboratory, physiologic, cytokine, and metabolic cart data were obtained. Histology of key end organs was also compared.
RESULTS:
Baseline values were similar among the groups. Compared with the TO group, the LYO group had reversible decreases in heart rate, mean arterial pressure, cardiac output, oxygen consumption, and carbon dioxide production. Compared with TO, LY + T showed sustained decreases in heart rate (113 vs. 76, p = 0.03), mean arterial pressure (40 vs. 31 mm Hg, p = 0.02), and cardiac output (3.8 vs. 1.9 L/min, p = 0.05) at 6 hours. Metabolic parameters showed profound suppression in the LY + T group. Oxygen consumption in LY + T was lower than both TO (119 vs. 229 mL/min, p = 0.012) and LYO (119 vs. 225 mL/min, p = 0.014) at 6 hours. Similarly, carbon dioxide production was decreased at 6 hours in LY + T when compared with TO (114 vs. 191 mL/min, p = 0.043) and LYO (114 vs. 195 mL/min, p = 0.034) groups. There was no worsening of acidosis (lactate 6.4 vs. 8.3 mmol/L, p = 0.4) or other endpoints. Interleukin 6 (IL-6) showed a significant increase in LY + T when compared with TO at 6 hours (60.5 vs. 2.47, p = 0.043). Tumor necrosis factor α and IL-1β were decreased, and IL-10 increased in TO and LY + T at 6 hours. Markers of liver and kidney injury were no different between TO and LY + T groups at 6 hours.
CONCLUSIONS:
Phosphoinositol-3-kinase inhibition produced metabolic suppression in healthy and injured swine without increasing end-organ injury or systemic physiologic markers and demonstrated prolonged efficacy in injured animals. Further study may lead to targeted therapies to prolong tolerance to hemorrhage and extend the "golden hour" for injured patients.
PEG-20k: Le graall du prolongef field care ?
Low-volume resuscitation using polyethylene glycol-20k in a preclinical porcine model of hemorrhagic shock
Plant V. et Al. J Trauma Acute Care Surg. 2016 Dec;81(6):1056-1062.
-----------------------------------
Une nouvelle approche de la prise en compte des lésions induites par l'ischémie tissulaire qui est basée sur l'expérience de l'emploi des solutés utilisés pour conserver les organes en instance de transplantation. Grosso-modo: Remplir les espaces interstitiels par des solutés ne dépendant pas de mécanismes énergétiques. Une explication ici.
-----------------------------------
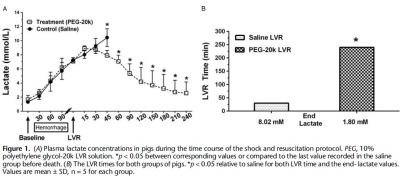
INTRODUCTION:
Polyethylene glycol-20k (PEG-20k) is highly effective for low-volume resuscitation (LVR) by increasing tolerance to the low-volume state. In our rodent shock model, PEG-20k increased survival and expanded the "golden hour" 16-fold compared to saline. The molecular mechanism is largely attributed to normalizations in cell and tissue fluid shifts after low-flow ischemia resulting in efficient microvascular exchange. The objective of this study was to evaluate PEG-20k as an LVR solution for hemorrhagic shock in a preclinical model.
METHODS:
Anesthetized male Yorkshire pigs (30-40 kg) were hemorrhaged to a mean arterial pressure (MAP) of 35 to 40 mm Hg. Once lactate reached 7 mmol/L, either saline (n = 5) or 10% PEG-20k (n = 5) was rapidly infused at 10% calculated blood volume. The primary outcome was LVR time, defined by the time from LVR administration to the time when lactate again reached 7 mmol/L. Other outcomes measured included MAP, heart rate, cardiac output, mixed venous oxygen saturation, splanchnic blood flow, and hemoglobin.
RESULTS:
Relative to saline, PEG-20k given after controlled hemorrhage increased LVR time by 16-fold, a conservative estimate given that the lactate never rose after LVR in the PEG-20k group. Survival was 80% for PEG-20k LVR compared to 0% for the saline controls (p < 0.05).
Polyethylene glycol-20k also significantly decreased heart rate after hemorrhage and increased cardiac output, MAP, splanchnic flow, and mixed venous oxygen saturation. Falling hemoglobin concentrations suggested sizable hemodilution from fluid shifts into the intravascular compartment.
CONCLUSIONS:
In a preclinical model of controlled hemorrhagic shock, PEG-20k-based LVR solution increased tolerance to the shock state 16-fold compared to saline. Polyethylene glycol-20k is a superior crystalloid for LVR that may increase safe transport times in the prehospital setting and find use in hospital emergency departments and operating rooms for patients awaiting volume replacement or normalization of cell, tissue, and compartment fluid volumes.
NaCl 7,5% ? A voir mais sans Colloïdes.
Pre-Hospital Resuscitation of Traumatic Hemorrhagic Shock with Hypertonic Solutions Worsen Hypo-Coagulation and Hyper-Fibrinolysis
Delano M. et Al. Shock. 2015 Jul;44(1):25-31
-----------------------------------------------
Le choix d'un liquide de remplissage vasculaire n'est pas simple. Au delà des contraintes d'efficacité en termes de remplissage vasculaire, de bonne tolérance notamment rénale il y a également les effets de ce dernier sur la coagulation. On sait qu'une partie importante des blessés actuellement pris en charge présentent une coagulopathie traumatique (1). Le NaCl 7.5% est le soluté recommandé par la procédure du sauvetage au combat (2) car il représente le meilleur compromis intérêt médical/logistique. Le travail ici présenté met en évidence les effets délétères des solutés hypertoniques sur la coagulation. Ce document mérite cependant d'être pondéré car il s'appuie sur une petite cohorte de patients de traumatologie civile, que le profil du remplissage vasculaire préhospitalier n'est pas clairement rapporté hormis le premier liquide, qu'il ne précise pas le niveau de calcémie plasmatique car ce dernier peut être affecté selon la nature des solutés utilisés (4), que le groupe HS a des marqueurs d'hypoperfusion tissulaire identique au groupe NS, que la comparaison se fait avec un groupe de sujets sains et non entre les groupes. Par ailleurs on sait également qu'il est mis en avant l'intérêt des solutions HS en matière de prise en charge des HTIC des plaies cranio-cérébrales (4) et la réduction de l'activation des polynucléaires neutrophiles (5). Donc il ne s'agit pas de remettre en question le choix actuel, mais de le repositionner dans le débat notamment avec l'emploi du Plama lyophylisé comme soluté de remplissage premier des blessés les plus graves (6). Une chose apparait certaine: Ne plus utiliser une association HS/Dextran type RescueFlow (7).
-----------------------------------------------
Impaired hemostasis frequently occurs after traumatic shock and resuscitation. The prehospital fluid administered can exacerbate subsequent bleeding and coagulopathy. Hypertonic solutions are recommended as first-line treatment of traumatic shock; however, their effects on coagulation are unclear. This study explores the impact of resuscitation with various hypertonic solutions on early coagulopathy after trauma. We conducted a prospective observational subgroup analysis of large clinical trial on out-of-hospital single-bolus (250 mL) hypertonic fluid resuscitation of hemorrhagic shock trauma patients (systolic blood pressure, e70 mmHg). Patients received 7.5% NaCl (HS), 7.5% NaCl/6% Dextran 70 (HSD), or 0.9% NaCl (normal saline [NS]) in the prehospital setting. Thirty-four patients were included: 9 HS, 8 HSD, 17 NS. Treatment with HS/HSD led to higher admission systolic blood pressure, sodium, chloride, and osmolarity, whereas lactate, base deficit, fluid requirement, and hemoglobin levels were similar in all groups. The HSD-resuscitated patients had higher admission international normalized ratio values and more hypocoagulable patients, 62% (vs. 55% HS, 47% NS; P G 0.05). Prothrombotic tissue factor was elevated in shock treated with NS but depressed in both HS and HSD groups. Fibrinolytic tissue plasminogen activator and antiYfibrinolytic plasminogen activator inhibitor type 1 were increased by shock but not thrombin-activatable fibrinolysis inhibitor. The HSD patients had the worst imbalance between procoagulation/anticoagulation and profibrinolysis/antifibrinolysis, resulting in more hypocoagulability and hyperfibrinolysis. We concluded that resuscitation with hypertonic solutions, particularly HSD, worsens hypocoagulability and hyperfibrinolysis after hemorrhagic shock in trauma through imbalances in both procoagulants and anticoagulants and both profibrinolytic and antifibrinolytic activities
24/09/2016
Transfusion en vol: Sécurité assurée
Risk Management Analysis of Air Ambulance Blood Product Administration in Combat Operations
BACKGROUND:
Between June-October 2012, 61 flight-medic-directed transfusions took place aboard U.S. Army Medical Evacuation (medevac) helicopters in Afghanistan. This represents the initial experience for pre-hospital blood product transfusion by U.S. Army flight medics.
METHODS:
We performed a retrospective review of clinical records, operating guidelines, after-action reviews, decision and information briefs, bimonthly medical conferences, and medevac-related medical records.
RESULTS:
A successful program was administered at 10 locations across Afghanistan. Adherence to protocol transfusion indications was 97%. There were 61 casualties who were transfused without any known instance of adverse reaction or local blood product wastage. Shock index (heart rate/systolic blood pressure) improved significantly en route, with a median shock index of 1.6 (IQR 1.2-2.0) pre-transfusion and 1.1 (IQR 1.0-1.5) post-transfusion (P < 0.0001). Blood resupply, training, and clinical procedures were standardized across each of the 10 areas of medevacoperations.
DISCUSSION:
Potential risks of medical complications, reverse propaganda, adherence to protocol, and diversion and/or wastage of limited resources were important considerations in the development of the pilot program. Aviation-specific risk mitigation strategies were important to ensure mission success in terms of wastage prevention, standardized operations at multiple locations, and prevention of adverse clinical outcomes. Consideration of aviation risk mitigation strategies may help enable other helicopter emergency medical systems to develop remote pre-hospital transfusion capability. This pilot program provides preliminary evidence that blood product administration by medevac is safe.
| Tags : transfusion
31/07/2016
Kétamine: Moins performant après !
Comparison of the effects of ketamine and morphine on performance of representative military tasks
Gaydos SJ et Al. J Emerg Med. 2015 Mar;48(3):313-24
BACKGROUND:
When providing care under combat or hostile conditions, it may be necessary for a casualty to remain engaged in military tasks after being wounded. Prehospital care under other remote, austere conditions may be similar, whereby an individual may be forced to continue purposeful actions despite traumatic injury. Given the adverse side-effect profile of intramuscular (i.m.) morphine, alternative analgesics and routes of administration are of interest. Ketamine may be of value in this capacity.
OBJECTIVES:
To delineate performance decrements in basic soldier tasks comparing the effects of the standard battlefield analgesic (10 mg i.m. morphine) with 25 mg i.m. ketamine.
METHODS:
Representative military skills and risk propensity were tested in 48 healthy volunteers without pain stimuli in a double-blind, placebo-controlled, crossover design.
RESULTS:
Overall, participants reported more symptoms associated with ketamine vs. morphine and placebo, chiefly dizziness, poor concentration, and feelings of happiness. Performance decrements on ketamine, when present, manifested as slower performance times rather than procedural errors.
CONCLUSIONS:
Participants were more symptomatic with ketamine, yet the soldier skills were largely resistant to performance decrements, suggesting that a trained task skill (autonomous phase) remains somewhat resilient to the drugged state at this dosage. The performance decrements with ketamine may represent the subjects' adoption of a cautious posture, as suggested by risk propensity testing whereby the subject is aware of impairment, trading speed for preservation of task accuracy. These results will help to inform the casualty care community regarding appropriate use of ketamine as an alternative or opioid-sparing battlefield analgesic.
27/06/2016
Albumine 20% plutôt que fibrinogène ?
Influences of limited resuscitation with plasma or plasma protein solutions on hemostasis and survival of rabbits with noncompressible hemorrhage
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2016;81: 42–49
--------------------------------
Dans ce travail et alors que l'albumine diluée n'est pas recommandée, les auteurs évoquent la possibilité que les effets favorables d'une réanimation basée sur l'apport de plasma serait lié à l'apport de protéine et en particulier d'albumine qui aurait un effet tampon élevé, réduisant l'acidose métabolique, un des facteurs de la triade létale.
--------------------------------
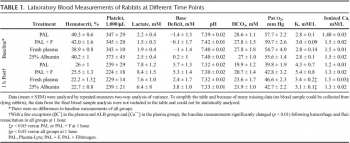
BACKGROUND:
Plasma infusion with or without red blood cells is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
Anesthetized spontaneously breathing rabbits (3.3 ± 0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 minutes with Plasma-Lyte (PAL; 30 mL/kg), PAL + fibrinogen (PAL + F; 30 mL + 100 mg/kg), fresh rabbit plasma (15 mL/kg), or 25% albumin (ALB; 5 mL/kg) solution, all given in two bolus intravenous injections (15 minutes apart) to achieve a mean arterial pressure of 65 mm Hg, n = 8 to 9/group. Animals were monitored for 2 hours or until death, and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 minutes. At 60 minutes after injury, mean arterial pressure was higher with ALB than with crystalloids (PAL or PAL + F), but shock indices were not different despite the large differences in resuscitation volumes. Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein and increased survival rate to 100% (p < .05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSIONS:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate; however, its effects did not differ from those obtained with 25% ALB at one-third of the volume. The ALB advantage was consistent with our previous findings in which 5% ALB was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its ALB content rather than its coagulation proteins
| Tags : coagulopathie, remplissage
22/06/2016
AL pour intuber: A ressortir de l'oubli
The Myth of Rescue Reversal in “Can’t Intubate, Can’t Ventilate” Scenarios
Naguib N. et Al. Anesth Analg. 2016 Jul;123(1):82-92
__________________________
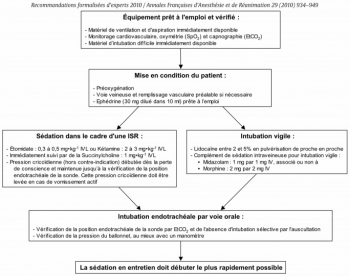
Ce travail met en avant l'insuffisance des démarches d'antagonisation pour restaurer une ventilation adéquate dans les situations de CICV. En ce qui concerne la gestion des voies aériennes en situation tactique, le principe de la préservation de la ventilation spontanée lors de l'accès aux voies aériennes mérite d'être rappelé. Si la réalisation d'une induction en séquence rapide reste la référence, en cas de difficulté prévisible le recours à une anesthésie locale doit être préférée (lire ce post).
Ceci est parfaitement stipulé dans les RFE "Sédation et analgésie en structure d’urgence" dont on rappelle après la présentation de l'abstract les termes de la question N3.
__________________________
BACKGROUND:
An unanticipated difficult airway during induction of anesthesia can be a vexing problem. In the setting of can't intubate, can't ventilate (CICV), rapid recovery of spontaneous ventilation is a reasonable goal. The urgency of restoring ventilation is a function of how quickly a patient's hemoglobin oxygen saturation decreases versus how much time is required for the effects of induction drugs to dissipate, namely the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade. It has been suggested that prompt reversal of rocuronium-induced neuromuscular blockade with sugammadex will allow respiratory activity to recover before significant arterial desaturation. Using pharmacologic simulation, we compared the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade in normal, obese, and morbidly obese body sizes in this life-threatening CICV scenario. We hypothesized that although neuromuscular function could be rapidly restored with sugammadex, significant arterial desaturation will occur before the recovery from unresponsiveness and/or central ventilatory depression in obese and morbidly obese body sizes.
METHODS:
We used published models to simulate the duration of unresponsiveness and ventilatory depression using a common induction technique with predicted rates of oxygen desaturation in various size patients and explored to what degree rapid reversal of rocuronium-induced neuromuscular blockade with sugammadex might improve the return of spontaneous ventilation in CICV situations.
RESULTS:
Our simulations showed that the duration of neuromuscular blockade was longer with 1.0 mg/kg succinylcholine than with 1.2 mg/kg rocuronium followed 3 minutes later by 16 mg/kg sugammadex (10.0 vs 4.5 minutes). Once rocuronium neuromuscular blockade was completely reversed with sugammadex, the duration of hemoglobin oxygen saturation >90%, loss of responsiveness, and intolerable ventilatory depression (a respiratory rate of ≤4 breaths/min) were dependent on the body habitus and duration of oxygen administration. There is a high probability of intolerable ventilatory depression that extends well beyond the time when oxygen saturation decreases <90%, especially in obese and morbidly obese patients. If ventilatory rescue is inadequate, oxygen desaturation will persist in the latter groups, despite full reversal of neuromuscular blockade. Depending on body habitus, the duration of intolerable ventilatory depression after sugammadex reversal may be as long as 15 minutes in 5% of individuals.
CONCLUSIONS:
The clinical management of CICV should focus primarily on restoration of airway patency, oxygenation, and ventilation consistent with the American Society of Anesthesiologist's practice guidelines for management of the difficult airway. Pharmacologic intervention cannot be relied upon to rescue patients in a CICV crisis.
__________________________
Question 3 - Intubation sous ISR et sous AL : Quelles sont les modalités de réalisation d’une sédation et/ou d’une analgésie pour l’intubation trachéale ?
Les experts recommandent d’administrer une sédation pour toutes les indications de l’intubation trachéale, excepté chez le patient en arrêt cardiaque qui ne nécessite pas de sédation. Lorsque l’intubation trachéale est présumée diffi cile, il est possible d’effectuer une anesthésie locale réalisée de proche en proche, associée ou non à une sédation légère et titrée par voie générale
L’utilisation de médicaments anesthésiques lors de l’intubation trachéale a pour but de faciliter le geste et d’assurer le confort du patient. Cette sédation doit être rapidement réversible pour restaurer une ventilation effi cace en cas de diffi culté d’intubation. Le risque d’inhalation bronchique doit être minimisé au cours de la procédure et ce d’autant que les patients sont considérés comme ayant un estomac plein.
Les experts recommandent d’utiliser les techniques d’intubation en séquence rapide (ISR) associant un hypnotique d’action rapide (étomidate ou kétamine) et un curare d’action brève (succinylcholine) ........................................................
Lorsque l’intubation trachéale est présumée difficile, le protocole recommandé par les experts pour une intubation vigile est le suivant : - Lidocaïne entre 2 et 5% en pulvérisation de proche en proche - Complément de sédation intraveineuse pour intubation vigile : • midazolam : 1 mg par 1 mg IV • associé ou non à de la morphine : 2 mg par 2 mg IV
04/06/2016
PLyo: Une révolution ? Pas vraiment, une redécouverte
Pusateri AE et Al. Transfusion. 2016 Apr;56 Suppl 2:S128-39
------------------------------------------
Les nouvelles modalités de transfusion mettent en avant le bénéfice de l'apport précoce de plasma. Les contraintes logistiques liées à l'emploi de plasma frais sont réelles. L'emploi de plasma lyophilisé permet de raccourcir ce délai et peut représenter dans certaines conditions d'isolement la seule source disponibles de fractions coagulantes. Le plasma lyophylisé est un vieux monsieur, mais dont la place est fondamentale. Largement utilisé notamment par l'armée française pendant la guerre d'indocchine, le SSA a maintenu sa production jusqu'à ce que l'épidémie de VIH ne survienne. Depuis les années 1980, le SSA a travaillé sans relâche pour sécuriser un produit qui retrouve la place qui lui est due dans la stratégie transfusionnelle du blessé de guerre (1) Il s'agit donc d'une redécouverte avec un emploi effectif en opération dès 1996 (2), plutôt que de révolution. Le document proposé à la lecture fait le point sur cette historique et les développements à venir. La lecture de ce document ne doit pas faire oublier la réflexion de plus en plus présente sur l'emploi en situation d'isolement de l'intérêt de la transfusion de sang total, seule source de plaquettes, associé au recours à des fractions coagulantes comme le fibrinogène et les complexes prothrombiques. Une telle association représente probablement l'avenir de la réanimation hémostatique préhospitalière (3, 4).
------------------------------------------
Historical dried plasma development Event Selected References
1930s Plasma lyophilization developed in the 1930s.
1940—Large scale production of pooled, lyophilized plasma by both the US and British established for war time use (to meet logistical constraints of whole blood and frozen/liquid plasma).ans les années
1941—Spray dried plasma produced for the Swedish Defense Department. 21 WWII Production 20-22 British produced >500,000 U lyophilized plasma during WWII. US produced >6,000,000 U lyophilized plasma during WWII. US/British distributed world-wide. Sweden produced approximately 17,000 U spray dried plasma for Sweden and Finland.
1945—Hepatitis 23 Hepatitis as a result of plasma transfusion recognized by the end of WWII. Believed that benefits outweighed the risk.
1945-1952—Hepatitis 24 Attempts at pathogen reduction and reducing pool size not successful. Several deaths in clinical studies of ultraviolet irradiated pooled plasma.
1953
—Department of the Army (Circular 73) directed that, because of the risk of serum hepatitis, the higher cost, and the need to use it for the production of specific globulins, plasma would not be used “to support blood volume” unless dextran was not available.
—Serum albumin replaced plasma as primary resuscitative product for US Forces in Korea.
1968—National Research Council Committee on Plasma and Plasma Substitutes recommended that “the use of whole, pooled human plasma be discouraged and even discontinued unless a clear cut case can be made for its unique requirements.”
The French Military Blood Institute produced dried plasma from 1949 to 1984, and provided over 40,000 units to French military forces during the Indochina War. In 1985, production was discontinued due to risk of HIV infection.
| Tags : coagulopathie, transfusion
Acide tranexaminique systématique: La roue tournerait-elle ?
Acute Fibrinolysis Shutdown after Injury Occurs Frequently and Increases Mortality: A Multicenter Evaluation of 2,540 Severely Injured Patients
Moore HB et Al. J Am Coll Surg. 2016 Apr;222(4):347-55.
------------------------------------------------------
La recommandation n°15 de la RFE Portant sur la réanimation du choc hémorragique stipule qu' il est recommandé d'administrer de l'acide tranexamique dès que possible chez les patients traumatisés à la dose de 1 g en bolus intraveineux en 10 min suivi de 1 g perfusé sur 8 h chez les patients traumatisés. Cette administration ne doit pas être initiée au delà de la 3e heure suivant la survenue d'un traumatisme avec choc hémorragique. Si l'étude CRASH-2 a montré que l'acide tranexamique réduisait significativement la mortalité. De nouvelles données disponibles depuis alimentent la discussion (1). Trois états du système de fibrinolyse peuvent être retrouvés: normal, hyperfibrinolyse, inhibition Les deux derniers sont associés à une surmortalité mais la fréquence des états d'inhibition de l'inhibition ne plaiderait pas pour une administration systématique mais ciblée d'exacyl. En qui nous concerne il faut à nouveau insister sur la précocité de l'administration d'exacyl dans l'heure chez les blessés sévères, pour lesquels le bénéfice en terme de mortalité est le plus grand (2). Une réflexion pour un emploi optimisé est en MARCHE (3, 4)
------------------------------------------------------
BACKGROUND:
Fibrinolysis is a physiologic process that maintains microvascular patency by breaking down excessive fibrin clot. Hyperfibrinolysis is associated with a doubling of mortality. Fibrinolysis shutdown, an acute impairment of fibrinolysis, has been recognized as a risk factor for increased mortality. The purpose of this study was to assess the incidence and outcomes of fibrinolysis phenotypes in 2 urban trauma centers.
STUDY DESIGN:
Injured patients included in the analysis were admitted between 2010 and 2013, were 18 years of age or older, and had an Injury Severity Score (ISS) > 15. Admission fibrinolysis phenotypes were determined by the clot lysis at 30 minutes (LY30): shutdown ≤ 0.8%, physiologic 0.9% to 2.9%, and hyperfibrinolysis ≥ 3%. Logistic regression was used to adjust for age, arrival blood pressure, ISS, mechanism, and facility.
RESULTS:
There were 2,540 patients who met inclusion criteria. Median age was 39 years (interquartile range [IQR] 26 to 55 years) and median ISS was 25 (IQR 20 to 33), with a mortality rate of 21%. Fibrinolysis shutdown was the most common phenotype (46%) followed by physiologic (36%) and hyperfibrinolysis (18%). Hyperfibrinolysis was associated with the highest death rate (34%), followed by shutdown (22%), and physiologic (14%, p < 0.001). The risk of mortality remained increased for hyperfibrinolysis (odds ratio [OR] 3.3, 95% CI 2.4 to 4.6, p < 0.0001) and shutdown (OR 1.6, 95% CI 1.3 to 2.1, p = 0.0003) compared with physiologic when adjusting for age, ISS, mechanism, head injury, and blood pressure (area under the receiver operating characteristics curve 0.82, 95% CI 0.80 to 0.84).
CONCLUSIONS:
Fibrinolysis shutdown is the most common phenotype on admission and is associated with increased mortality. These data provide additional evidence of distinct phenotypes of coagulation impairment and that individualized hemostatic therapy may be required.
| Tags : coagulopathie
03/06/2016
The 2015 Remote Damage Control Resuscitation Symposium
| Tags : transfusion, coagulopathie
24/01/2016
Succinylcholine et frigo: Non fondé ?
Froid et suxaméthonium : une recommandation non fondée
Dewachter P et AL. Ann. Fr. Med. Urgence DOI 10.1007/s13341-015-0600-1
Morceaux choisis:
L’Agence nationale de sécurité du médicament et des produits de santé (ANSM) a publié en 2012 une recommandation destinée aux médecins anesthésistes-réanimateurs et urgentistes décrivant les conditions d’utilisation du chlorure de suxaméthonium. .......Cette recommandation faisait suite à une enquête rétrospective de pharmacovigilance sur les réactions allergiques induites par les curares qui mettait en évidence une augmentation des notifications de réactions allergiques attribuées au suxaméthonium........Néanmoins, l’hypothèse émise par l’ANSM ne résiste pas à l’évaluation scientifique. En effet, aucune étude n’a démontré que le suxaméthonium conservé à température ambiante favorise la survenue d’une réaction allergique, ce qui avait déjà été souligné lors de la publication de cette recommandation..........................En revanche, depuis 20 ans, plusieurs équipes européennes et nord-américaines ont confirmé la stabilité des solutions de chlorure de suxaméthonium à température ambiante ou lors de variations extrêmes de température................... La succinylcholine (50 mg/mL) préservée dans l’ampoule est stable pendant deux mois à température ambiante (25°C) [5] alors que la solution à 20 mg/mL reste stable au moins sept jours après exposition à des variations extrêmes de température (de -6°C à +54°C).......................Par ailleurs, la solution de succinylcholine (20 mg/mL) conservée dans une seringue en plastique est stable trois mois à 25°C et deux mois à 40°C . Enfin, la stabilité de la succinylcholine stockée à bord d’ambulances, respectivement pendant sept mois [8] et un an , a été évaluée après exposition aux variations climatiques auxquelles ces équipes sont exposées. La succinylcholine (20 mg/mL) est stable pendant environ trois mois quand elle est soumise à des températures moyennes variant de -9°C à +32°C [8] alors que la solution à 100 mg/mL est stable pendant un peu plus d’un mois quand elle est exposée de -8°C à +36°C. D’autres études ont également confirmé la stabilité de la succinylcholine (10 mg/ml) dans une seringue en plastique pendant sept jours [9] et pendant au moins cinq mois, quand celle-ci est conservée dans l’ampoule (20 et 50 mg/ml) ..........Plus récemment, la stabilité de la succinylcholine à température ambiante (25°C) a été confirmée par l’ANSM pour qui les résultats obtenus sont « conformes aux spécifications à péremption décrites dans le dossier d’AMM................Ce rapport de conclure que « les données relatives à la qualité ne semblent donc pas être en mesure d’expliquer l’augmentation des réactions anaphylactiques sur la période étudiée............Le turn-over prévisible de l’utilisation du suxaméthonium stocké à température ambiante rend ainsi son utilisation possible par les équipes de Samu. En effet, l’éventuelle morbidité – voire mortalité – induite par cette recommandation ne peut être occultée. Nombreux sont les patients qui devant bénéficier d’une induction à séquence rapide, ont été intubés sans curare par les équipes qui ne disposaient pas d’un réfrigérateur à bord alors que l’appréciation de la balance risque/ bénéfice penche en faveur de l’utilisation du suxaméthonium dans cette situation clinique
Gammon DL, et al (2008) Alteration in prehospital drug concentration after thermal exposure. Am J Emerg Med 26:566–73.
| Tags : intubation
21/01/2016
Le graal plaquettaire hémostatique ?
Thrombosomes: a platelet-derived hemostatic agent for control of noncompressible hemorrhage
Fitzpatrick GM et Al. Transfusion. 2013 Jan;53 Suppl 1:100S-106S
----------------
Un thrombosome est en quelque sorte une plaquette lyophilisée dans laquelle l'eau est remplacée par un sucre particulier: le trehalose. Ré exposé à une atmosphère humide, il se réhydrate pour retrouver toutes ses propriétés. Cela ne semble pas être une simple théorie car il initierait une génération de thrombine permettant la formation d'un caillot de manière satisfaisante. Des thrombosmes, du fibrinogène et du PLyo, on peut espérer !
----------------
BACKGROUND: Uncontrolled hemorrhage is responsible for ~80% of the potentially survivable deaths in combat and over 40% of early mortality in the under 65 age group in the United States. Providing an easily used infusible hemostatic agent to first responders could significantly reduce these fatalities. We report on an infusible lyophilized platelet-derived hemostatic agent stabilized with trehalose and polysucrose prior to and during lyophilization.
STUDY DESIGN AND METHODS: Characterization included determining the particle population size range, surface marker expression GPIb, GPIIbIIIa, and Annexin V binding. Function was assessed by aggregation, thromboelastography, and thrombin generation. Pharmacokinetics, biodistribution, and immunogenicity established using Indium111 labeled Thrombosomes in healthy New Zealand white rabbits (NZWRs), efficacy in thrombocytopenic NZWR, and safety in NZWRs, canines, and nonhuman primates.
RESULTS: Thrombosomes retained GPIIbIIIa expression (98.71% 0.18 of the rehydrated particles), a reduced expression of GPIb (47.77% 6.65), and Annexin V binding (86.05% 2.65). Aggregation to all agonists except thrombin in buffer (78.15% 2.5) was <50%. Thrombin generation and thromboelastography results demonstrated a concentration gradient that was consistent from lot to lot. There were no observed adverse events in any safety study and blood loss was reduced by >80% in the thrombocytopenic ear bleed model.
CONCLUSION: Our in vitro characterization studies in conjunction with preclinical animal safety and efficacy studies demonstrated lot consistency in manufacturing, maintenance of hemostatic functions of Thrombosomes, safety at high dose concentrations, and the potential to provide an effective hemostatic agent at the site of injury.
17/01/2016
Cyanokit pour l'hémorragie massive ?
A prospective, randomized trial of intravenous hydroxocobalamin versus whole blood transfusion compared to no treatment for class III hemorrhagic shock resuscitation in a prehospital swine model
Bebarta VS et Al. Acad Emerg Med.2015 Mar;22(3):321-30
--------------------------------
La prise en charge des hémorragies traumatiques en préhospitalier est basée sur la miseen oeuvre des moyens d'arrêts de ces dernières et l'initiation d'une stratégie raisonnée de remplissage vasculaire et de transfusion. L'apport équilibrée de CGR, de plasma,de fractions coagulantes et même de plaquettes fait partie de cette démarche de damage control resuscitation de même que l'apport d'acide tranexaminique pour s'opposer à une fibrinolyse précoce souvent présente. D'autres axes de recherches sont proposés. AInsi l'hydroxocobalamine, connue en tant qu'antidote de l'acide cynahydrique permettrait sur des cochons auxquels on aurait soustrait 20 ml/kg de sang de préserver la pression artérielle et la lactatémie de manière identique à celle obtenue par l'apport de sang total.
--------------------------------
OBJECTIVES:
The objective was to compare systolic blood pressure (sBP) over time in swine that have had 30% of their blood volume removed (Class III shock) and treated with intravenous (IV) whole blood or IV hydroxocobalamin, compared to nontreated control animals.
METHODS:
Thirty swine (45 to 55 kg) were anesthetized, intubated, and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged a total of 20 mL/kg over a 20-minute period. Five minutes after hemorrhage, animals were randomly assigned to receive 150 mg/kg IV hydroxocobalamin solubilized in 180 mL of saline, 500 mL of whole blood, or no treatment. Animals were monitored for 60 minutes thereafter. A sample size of 10 animals per group was determined based on a power of 80% and an alpha of 0.05 to detect an effect size of at least a 0.25 difference (>1 standard deviation) in mean sBP between groups. sBP values were analyzed using repeated-measures analysis of variance (RANOVA). Secondary outcome data were analyzed using repeated-measures multivariate analysis of variance (RMANOVA).
RESULTS:
There were no significant differences between hemodynamic parameters of IV hydroxocobalamin versus whole blood versus control group at baseline (MANOVA; Wilks' lambda; p = 0.868) or immediately posthemorrhage (mean sBP = 47 mm Hg vs. 41 mm Hg vs. 37 mm Hg; mean arterial pressure = 39 mm Hg vs. 28 mm Hg vs. 34 mm Hg; mean serum lactate = 1.2 mmol/L vs. 1.4 mmol/L vs. 1.4 mmol/L; MANOVA; Wilks' lambda; p = 0.348). The outcome RANOVA model detected a significant difference by time between groups (p < 0.001). Specifically, 10 minutes after treatment, treated animals showed a significant increase in mean sBP compared to nontreated animals (mean sBP = 76.3 mm Hg vs. 85.7 mm Hg vs. 51.1 mm Hg; p < 0.001). RMANOVA modeling of the secondary data detected a significant difference in mean arterial pressure, heart rate, and serum lactate (p < 0.001). Similar to sBP, 10 minutes after treatment, treated animals showed a significant increase in mean arterial pressure compared to nontreated animals (mean arterial pressure = 67.7 mm Hg vs. 61.4 mm Hg vs. 40.5 mm Hg). By 10 minutes, mean heart rate was significantly slower in treated animals compared to nontreated animals (mean heart rate = 97.3 beats/min vs. 95.2 beats/min vs. 129.5 beats/min; p < 0.05). Serum lactate, an early predictor of shock, continued to rise in the control group, whereas it did not in treated animals. Thirty minutes after treatment, serum lactate values of treated animals were significantly lower compared to nontreated animals (p < 0.05). This trend continued throughout the 60-minute observation period such that 60-minute values for lactate were 1.4 mmol/L versus 1.1 mmol/L versus 3.8 mmol/L. IV hydroxocobalamin produced a statistically significant increase in systemic vascular resistance compared to control, but not whole blood, with a concomitant decrease in cardiac output.
CONCLUSIONS:
Intravenous hydroxocobalamin was more effective than no treatment and as effective as whole blood transfusion, in reversing hypotension and inhibiting rises in serum lactate in this prehospital, controlled, Class III swine hemorrhage model.
| Tags : choc