03/01/2016
Kétamine: Prudence quand même
Is ketamine ready to be used clinically for the treatment of depression ?
Colleen L. Med J Aust 2015 Dec 14;203(11):425.
A single dose of ketamine produces rapid antidepressant effects, but attaining lasting remission remains a challenge
Il existe un engouement très important pour l'emploi de kétamine pour la prise en charge de la dépression (1,2). Pour autant il ne faut pas oublier les effets secondaires de cette dernière lorsqu'elle est administrée de manière chronique. De nombreuses données issues de l'emploi récréatif de la kétamine mettent en avant de nombreux effets secondaires comme l'hépatotoxicité, les dysfonctions vésicales et, possiblement des troubles cognitifs. Même si aucun effets de ce type n'est retrouvé lors d'emploi encadré médicalement, la prudence reste de mise.
01/01/2016
Kétamine et dépression: Raz de marée
Anesthesiologists Take Lead As Ketamine Clinics Proliferate
A growing number of anesthesiologists are opening private clinics that provide off-label infusions of ketamine to patients suffering from treatment-resistant unipolar and bipolar depression, post-traumatic stress disorder (PTSD), anxiety, suicidality and other disorders. Psychiatrists and other physicians have also recently opened clinics.
The cost per infusion ranges from $400 to $1700, with most clinics charging about $500. Patients pay out-of-pocket since most health insurance plans do not cover the off-label procedure.
Despite the cost, patients seek the treatments after their antidepressants and other therapies prove ineffective. Proponents claim that, when administered as an IV infusion in a subanesthetic dose (typically 0.5 mg/kg body weight) over 40 to 45 minutes, ketamine begins reversing symptoms of depression for two of three patients in less than 24 hours, with effects persisting for a week or more. Nearly three of four patients suffering from suicidality experience an almost immediate reversal in thinking.
“The results are amazing,” said anesthesiologist Glen Z. Brooks, MD, founder and medical director of New York Ketamine Infusions LLC, in New York City, and one of the pioneers in the field. His success rate averages about 65% when measured by standardized mood and function surveys, and is even greater for younger adults, he said. The typical course of treatment is six infusions administered every other day for two weeks followed by “maintenance” or “booster” infusions as needed, typically every six weeks afterward.
“The procedure is very well tolerated. We have seen no complications during or after the 45-minute infusions in now close to 8,000 treatments,” Dr. Brooks told Anesthesiology News. “I have been treating some patients for as long as three years with ongoing remission of their symptoms, so efficacy can be very long term.”
Ketamine Can Work Quickly
Ketamine was synthesized in the early 1960s and approved for human anesthesia a decade later. It has been administered to millions of patients worldwide, and continues to be an anesthetic of choice for pediatric patients who may experience adverse reactions to other agents. It also is used in pain clinics and when changing dressings of severe burn victims.
For treating depression, it only takes two ketamine infusions to determine whether a patient will respond favorably, whereas traditional antidepressants can take four to six weeks and will work about 30% of the time. During the ketamine infusion, patients remain awake or in a twilight state. Dizziness or a sensation of dissociation is common, and generally disappears shortly after the infusion. “We notice a 50% improvement in depression scores within the first three infusions, which take six days,” said anesthesiologist Enrique Abreu, MD, medical director at Portland Ketamine Clinic in Oregon. “Overall, 75% to 80% of patients see improvement in depression, mood and anxiety after six treatments,” he told Anesthesiology News.
Some experts in depression research have called ketamine’s “rapid and robust” antidepressant properties “arguably the most important discovery in half a century” (Science 2012;338:68-72). Others urge caution, citing concerns over long-term side effects and potential for abuse. The latter concern stems from ketamine being an illicit “rave” drug (nicknamed “Special K” or “Vitamin K”) that creates intense, short-term hallucinations, dissociation and psychotomimetic effects. Ketamine also is pharmacologically similar to PCP (phencyclidine), a powerful psychotomimetic drug.
While the World Health Organization has long included ketamine on its model list of essential medicines for anesthesia, the drug also has been placed under national control in more than 60 countries, especially in Asia, where abuse is common. Bladder problems and cognitive declines have been observed in long-term recreational ketamine abusers, but none of these effects has been observed in clinical trials.
The anesthesiologists and psychiatrists who administer ketamine infusions for severe depression report overwhelmingly positive outcomes. New Jersey psychiatrist Steven Levine, MD, decided to explore ketamine after reading reports of clinical studies conducted at the National Institute of Mental Health (NIMH). “The results were unlike anything we had seen before, with positive outcomes emerging within days or weeks,” Dr. Levine said. “Some really sick people were getting significantly better within hours. I couldn’t convince myself to not do it.”
Dr. Levine quizzed several anesthesiologist friends about potential dangers before opening his clinic. “They were totally nonplussed about the low dosage used in the infusion, unconcerned about any potential for bad side effects,” Dr. Levine told Anesthesiology News. “They were used to giving it in much higher doses for anesthesia and even higher doses in burn units when changing dressings.” Dr. Levine opened Ketamine Treatment Centers of Princeton LLC, in New Jersey, in 2011 and has since treated about 500 patients. He plans to open clinics in Baltimore, Florida and Denver in early 2016.
Mechanisms of Action
Typical FDA-approved antidepressants target neurons that inhibit the reuptake of serotonin, norepinephrine and dopamine. Ketamine works more broadly by blocking the N-methyl-D-aspartate (NMDA) receptor, a component of the fast-signaling glutamate system that affects nearly all neurons. Brain scans reveal that ketamine rapidly induces synaptogenesis, repairing damage caused by chronic stress.
Many clinical trials of ketamine for depression have been, and continue to be, conducted at NIMH. A seminal study published in 2006 was a randomized, placebo-controlled, double-blind crossover trial led by Carlos A. Zarate Jr., MD, chief of NIMH’s neurobiology and mood disorders treatment section. In this year-long study, patients receiving ketamine showed significant improvement in depression compared with placebo after 24 hours, with effects remaining “moderate to large” after one week (Arch Gen Psych 2006;63:856-864). “This line of research holds considerable promise for developing new treatments for depression with the potential to alleviate much of the morbidity and mortality associated with the delayed onset of action of traditional antidepressants,” Dr. Zarate and colleagues wrote, citing the need to improve the drug’s long-term effectiveness.
Since then, studies at NIMH and elsewhere have demonstrated ketamine’s efficacy for rapidly diminishing suicidal ideation (Drugs R D 2015;15:37-43), unipolar and bipolar depression (Cochrane Database Syst Rev 2015;23:CD011612; Cochrane Database Syst Rev 2015;29:CD-011611), and for PTSD and other anxiety disorders (JAMA Psychiatry 2014;71:681-688).
The American Psychiatric Association’s Task Force on Novel Biomarkers and Treatments urges caution when it comes to clinical use of ketamine. In a systematic review and meta-analysis of randomized clinical trials of ketamine and other NMDA receptor antagonists (Am J Psych 2015;172:950-966), the task force concluded: “The antidepressant efficacy of ketamine … holds promise for future glutamate-modulating strategies.” However, the “fleeting nature of ketamine’s therapeutic benefit, coupled with its potential for abuse and neurotoxicity, suggest that its use in the clinical setting warrants caution.”
When asked to comment on anesthesiologists performing off-label ketamine infusions, the American Society of Anesthesiologists (ASA) provided this statement to Anesthesiology News: “The American Society of Anesthesiologists is committed to promoting the highest standards of care for the patients they serve. This new practice area has been brought to ASA’s attention and will be carefully reviewed.”
Gaining Legitimacy
According to ketamine advocate Dennis Hartman, at least 60 private clinics in the United States offer off-label infusions, and the number is growing. The former business executive says ketamine infusions rescued him from suicide in 2012, and ongoing treatments have brought his depression into remission. As founder and CEO of the nonprofit Ketamine Advocacy Network, Mr. Hartman now works full time with practitioners and patients to help gain legitimacy for the field. His website lists 18 ketamine practitioners in the United States, most of them anesthesiologists, with a smaller number of psychiatrists and neurologists, plus one emergency medicine physician and one family physician.
“There are others that we have not vetted and others that we’ve purposefully chosen not to include,” Mr. Hartman explained, most often because they charge too much money or require expensive additional tests or medical procedures for which clinical evidence is lacking. “There are still others who offer the treatment but want to be under the radar,” Mr. Hartman told Anesthesiology News.
Anesthesiologists generally believe they are uniquely qualified to administer ketamine infusions because of their expertise with anesthetics. “I want this to stay as something for anesthesiologists,” said Steven Mandel, MD, founder of Ketamine Clinics of Los Angeles. “Nevertheless, I don’t want there to be a conflict between anesthesiology and psychiatry, because ketamine definitely needs an anesthesiologist to administer it and definitely needs a psychiatrist or psychologist involved because they know about psychopathology,” he said. But ketamine does take “considerable vigilance and finesse” to infuse properly, he added, even for those with years of operating room experience. “This is different because the ‘sweet spot’ for treatment is this side of unconsciousness in the moderate- to deep-sedation range,” Dr. Mandel explained.
Many psychiatrists, on the other hand, believe they are best suited to oversee ketamine therapy because of their expertise in treating patients with depression, PTSD and other conditions. In those ketamine clinics run by psychiatrists, the IV insertion is generally performed by a nurse, not an anesthesiologist, and the infusion is overseen by a psychiatrist and a nurse. Clinics led by anesthesiologists generally do not employ a staff psychiatrist but coordinate with the patients’ mental health practitioners.
Virtually all practitioners—anesthesiologists and psychiatrists alike—recognize the importance of cooperation. Nearly all ketamine clinics require a referral from a psychiatrist or other mental health professional, with few accepting walk-ins. “Three years ago, the relationships [between psychiatrists and anesthesiologists] were difficult, to say the least,” said anesthesiologist Mark Murphy, MD, who established Ketamine Wellness Centers in Phoenix, in 2013. “However, the momentum is shifting. Now we regularly receive referrals from mental health professionals.”
Those patients who do best tend to have psychiatrists or therapists supporting them throughout the treatment course and are engaged in a team approach, said anesthesiologist Isabel Legarda, MD, medical director at Boston MindCare LLC. “I believe anesthesiologists and psychiatrists must work collaboratively when it comes to ketamine infusion therapy; anything less shortchanges patients,” she said.
Insurance Coverage?
Because ketamine is generic, pharmaceutical companies have no financial incentive to sponsor the costly clinical trials needed to win FDA approval, generally a prerequisite for insurance coverage. Recognizing this, there is a movement in the ketamine community to gather and publish retrospective chart data and promulgate best practice guidelines. “There’s never going to be an FDA label for ketamine to treat depression,” said Dr. Levine. “But once more guidelines and protocols for using ketamine in clinical practice are published, it is very likely that insurers will consider covering it,” he predicted.
At least two drug companies are developing new ketamine variants that might be easier to administer and which lack some of the generic’s less-favorable short-term side effects, such as dissociation, and which insurers may be willing to cover. Johnson & Johnson’s subsidiary Janssen Pharmaceuticals is conducting late-stage clinical trials of esketamine, a variant that can be administered via a nasal spray. The FDA granted the drug “breakthrough” status in 2013, which streamlines the regulatory approval process. Allergan’s subsidiary Naurex Inc. is testing GLYX-13, an IV NMDA receptor variant that reportedly is effective in about half of patients in 24 hours, but without ketamine’s dissociative side effects. NeuroRx Inc. is testing a drug, Cyclurad, whose ingredients include D-cycloserine, an NMDA receptor modulator.
Dr. Levine and other physicians caution colleagues against starting a ketamine clinic to make quick money. “If someone is thinking of doing this part time to pad their income, there could be bad outcomes because these patients are very vulnerable,” Dr. Levine said. “This is an area that could use some regulation and standardization so that patients don’t get hurt, and what is a very important treatment becomes lost.”
Most ketamine practitioners say their motivation stems from having had patients or family members who were treatment resistant and, in some cases, even committed suicide. For them, money is secondary to the satisfaction they gain. “For me, this has been a much more demanding and professionally rewarding practice than being in a hospital operating room,” said Dr. Brooks. “It requires a special dedication and availability.”
20/12/2015
Coagulopathie: Du fibrinogène avant tout
Trauma-induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs
Nardi G et al. Critical Care (2015) 19:83
------------------------------------
Le damage control resuscitation fait largement appel à l'apport de plasma, concentrés de globules rouges et de plaquettes dans un rapport de 1/1/1 (1). Malgré la relative correction de la coagulopathie la survie à long terme ne semble pas être améliorée (2). Aussi certains proposent d'avoir plutôt recours à l'administration précoce de fibrinogène plutôt que l'administration de plasma. Le travail suivant qui propose l'apport précoce de 2g de fibrinogène est en faveur d'une telle démarche.
------------------------------------
INTRODUCTION:
Hemorrhage is the principal cause of death in the first few hours following severe injury. Coagulopathy is a frequent complication of critical bleeding. A network of Italian trauma centers recently developed a protocol to prevent and treat trauma-induced coagulopathy. A pre-post cohort multicenter study was conducted to assess the impact of the early coagulation support (ECS) protocol on blood products consumption,mortality and treatment costs.
METHODS:
We prospectively collected data from all severely injured patients (Injury Severity Score (ISS) >15) admitted to two trauma centers in 2013 and compared these findings with the data for 2011. Patients transfused with at least 3 units of packed red blood cells (PRBCs) within 24 hours of an accident were included in the study. In 2011, patients with significant hemorrhaging were treated with early administration of plasma with the aim of achieving a high (≥1:2) plasma-to-PRBC ratio. In 2013, the ECS protocol was the treatment strategy. Outcome data, blood product consumption and treatment costs were compared between the two periods.
RESULTS:
The two groups were well matched for demographics, injury severity (ISS: 32.9 in 2011 versus 33.6 in 2013) and clinical and laboratory data on admission. In 2013, a 40% overall reduction in PRBCs was observed, together with a 65% reduction in plasma and a 52% reduction in platelets. Patients in the ECS group received fewer blood products: 6.51 units of PRBCs versus 8.14 units. Plasma transfusions decreased from 8.98 units to 4.21 units (P <0.05), and platelets fell from 4.14 units to 2.53 units (P <0.05). Mortality in 2013 was 13.5% versus 20% in 2011 (13 versus 26 hospital deaths, respectively) (nonsignificant). When costs for blood components, factors and point-of-care tests were compared, a €76,340 saving in 2013 versus 2011 (23%) was recorded.
CONCLUSIONS:
The introduction of the ECS protocol in two Italian trauma centers was associated with a marked reduction in blood product consumption, reaching statistical significance for plasma and platelets, and with a non-significant trend toward a reduction in early and 28-daymortality. The overall costs for transfusion and coagulation support (including point-of-care tests) decreased by 23% between 2011 and 2013.
| Tags : coagulopathie
26/11/2015
Kétamine pour le PTSD: Oui!
Efficacy of Intravenous Ketamine for Treatment of Chronic Posttraumatic Stress Disorder. A Randomized Clinical Trial
Feder A. et Al. JAMA Psychiatry. 2014 Jun;71(6):681-8. doi: 10.1001/jamapsychiatry.2014.62
Importance Few pharmacotherapies have demonstrated sufficient efficacy in the treatment of posttraumatic stress disorder (PTSD), a chronic and disabling condition.
Objective To test the efficacy and safety of a single intravenous subanesthetic dose of ketamine for the treatment of PTSD and associated depressive symptoms in patients with chronic PTSD.
Design, Setting, and Participants Proof-of-concept, randomized, double-blind, crossover trial comparing ketamine with an active placebo control, midazolam, conducted at a single site (Icahn School of Medicine at Mount Sinai, New York, New York). Forty-one patients with chronic PTSD related to a range of trauma exposures were recruited via advertisements.
Interventions Intravenous infusion of ketamine hydrochloride (0.5 mg/kg) and midazolam (0.045 mg/kg).
Main Outcomes and Measures The primary outcome measure was change in PTSD symptom severity, measured using the Impact of Event Scale–Revised. Secondary outcome measures included the Montgomery-Asberg Depression Rating Scale, the Clinical Global Impression–Severity and –Improvement scales, and adverse effect measures, including the Clinician-Administered Dissociative States Scale, the Brief Psychiatric Rating Scale, and the Young Mania Rating Scale.
Results Ketamine infusion was associated with significant and rapid reduction in PTSD symptom severity, compared with midazolam, when assessed 24 hours after infusion (mean difference in Impact of Event Scale–Revised score, 12.7 [95% CI, 2.5-22.8]; P = .02). Greater reduction of PTSD symptoms following treatment with ketamine was evident in both crossover and first-period analyses, and remained significant after adjusting for baseline and 24-hour depressive symptom severity. Ketamine was also associated with reduction in comorbid depressive symptoms and with improvement in overall clinical presentation. Ketamine was generally well tolerated without clinically significant persistent dissociative symptoms.

Conclusions and Relevance This study provides the first evidence for rapid reduction in symptom severity following ketamine infusion in patients with chronic PTSD. If replicated, these findings may lead to novel approaches to the pharmacologic treatment of patients with this disabling condition.
| Tags : ptsd
12/11/2015
Et l'albumine ?
Is limited prehospital resuscitation with plasma more beneficial than using a synthetic colloid? An experimental study in rabbits with parenchymal bleeding
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2015;78: 752-759
--------------------------------------
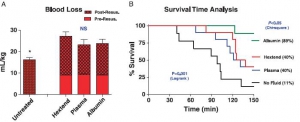
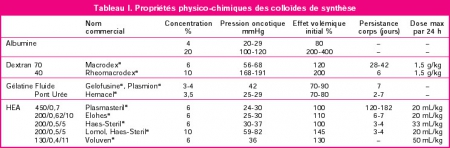
Il existe de grands débats sur la manière optimale d'assurer le remplissage vasculaire des blessés de guerre. Pour certains le fluide de référence est un hydroxyéthylamidon, pour d'autres un cristalloïde isotonique et en ce qui nous concerne les deux avec la mise en avant du sérum salé hypertonique premier suivi d'HEA. Actuellement il existe une tendance à promouvoir une autre stratégie faisant appel pour les blessés les plus graves au plasma voire la transfusion de sang frais. L'étude proposée avait pour objectif de confirmer l'intérêt d'une démarche "plasma premier". Une des surprises a été de constater que ce n'est pas cette dernière qui permettait d'obtenir le meilleur taux de survie mais l'emploi d'albumine, et ce de loin. Ces données expérimentales certes très partielles permettent aux auteurs (?) de rediscuter les conclusions de travaux anciens notamment de l'étude SAFE (1,2). Les solutés d'albumine utilisés par cette dernière ont une osmolarité de 260 mosm/kg (versus 305 mosm/kg pour le sérum salé). Les effets délétères notamment chez le traumatisé crânien pourraient être dus non pas à l'extravasation d'albumine dans le parenchyme cérébral lésé mais à l'hypoosmolarité de l'albumex 4%, ces deux mécanismes concourrant à la plus grande fréquence d'HTIC dans le groupe albumine (3). A méditer
--------------------------------------
BACKGROUND:
Reports of survival benefits of early transfusion of plasma with red blood cells (1:1 ratio) in trauma patients suggest that plasma may be a better fluid to replace Hextend for battlefield resuscitation. We studied possible advantages of prehospital resuscitation with plasma compared with Hextend or albumin in a model of uncontrolled hemorrhage.
METHODS:
Male New Zealand white rabbits (3.3 T 0.1 kg) were anesthetized, instrumented, and subjected to a splenic injury with uncontrolled bleeding. Ten minutes after injury (mean arterial pressure [MAP] G 40 mm Hg), the rabbits received small and equal volumes (15 mL/kg) of rabbit plasma (n = 10), Hextend (n = 10), or 5% human albumin (n = 9) or no fluid. Fluids were administered in two bolus injections (20 minutes apart) and targeted to aMAP of 65 mm Hg. Animals were monitored for 2.5 hours or until death, and their blood losses were measured. Arterial blood samples were collected at different times and analyzed for ABG, CBC, and coagulation tests.
RESULTS:
There were no differences in baseline measures among groups. Splenic injury caused similar hemorrhages (9.1 T 0.4 mL/kg at 10 minutes) and decreased MAP in all subjects. Subsequent resuscitation initiated additional bleeding. At 60 minutes after injury (20 minutes after resuscitation), longer activated partial thromboplastin time and lower fibrinogen concentrations were apparent compared with baseline values with differences among groups. Thrombelastography analysis indicated faster and stronger clot formation with plasma and albumin resuscitation than with Hextend use. Shock indices were increased in all groups, but smaller changes were measured in the albumin group. Total blood loss did not differ among resuscitated rabbits but was higher (p G 0.05) than among nonresuscitated animals. Survival rates were 11% (untreated), 40% (Hextend and plasma), and 89% (albumin, p G 0.05).
CONCLUSION:
Resuscitation with plasma or albumin better preserved coagulation function than did Hextend. However, despite these improvements, plasma resuscitation did not reduce blood loss or improve survival, while albumin administration seemed beneficial
| Tags : remplissage, coagulopathie
Lent/régulier: Mieux pour le crâne ?
Resuscitation speed affects brain injury in a large animal model of traumatic brain injury and shock
Sillesen M et Al. Scand J Trauma Resusc Emerg Med. 2014 Aug 14;22:46
----------------------------------------
En matière de remplissage vasculaire, on s'intéresse souvent à la nature des solutés et aux quantités perfusées. On s'intéresse moins aux vitesses de perfusion. Pourtant cette dernière a son importance. Le travail présenté est intéressant car il rapport qu'outre la nature du soluté importante mais aussi sa vitesse d'administration. Ainsi il semblerait que dans un modèle expérimental de traumatisme crânien l'emploi de solutés cristalloïdes de sérum salé isotonique soit responsable d'une augmentation de l'oedeme cérébal et du volume des lésions intracraniennes quel que soit le régime d'administration. Ce travail retrouve par ailleurs l'intérêt sur la maîtrise de l'oedeème cérébral de l'apport de fraction coagulantes de manière procédurée par rapport au bolus. Si l'on replace ce document dans le contexte d'isolement et de maintien en survie de nos blessés notamment cranio-cérébraux en état de choc, cela implique une formation spécifique des équipes qui devront par ailleurs pouvoir disposer d'équipements adaptés comme celui_ci (1)
----------------------------------------
BACKGROUND:
Optimal fluid resuscitation strategy following combined traumatic brain injury (TBI) and hemorrhagic shock (HS) remain controversial and the effect of resuscitation infusion speed on outcome is not well known. We have previously reported that bolus infusion of fresh frozen plasma (FFP) protects the brain compared with bolus infusion of 0.9% normal saline (NS). We now hypothesize reducing resuscitationinfusion speed through a stepwise infusion speed increment protocol using either FFP or NS would provide neuroprotection compared with a highspeed resuscitation protocol.
METHODS:
23 Yorkshire swine underwent a protocol of computer controlled TBI and 40% hemorrhage. Animals were left in shock (mean arterial pressure of 35 mmHg) for two hours prior to resuscitation with bolus FFP (n = 5, 50 ml/min) or stepwise infusion speed increment FFP (n = 6), bolus NS (n = 5, 165 ml/min) or stepwise infusion speed increment NS (n = 7). Hemodynamic variables over a 6-hour observation phase were recorded. Following euthanasia, brains were harvested and lesion size as well as brain swelling was measured.
RESULTS:
Bolus FFP resuscitation resulted in greater brain swelling (22.36 ± 1.03% vs. 15.58 ± 2.52%, p = 0.04), but similar lesion size compared with stepwise resuscitation. This was associated with a lower cardiac output (CO: 4.81 ± 1.50 l/min vs. 5.45 ± 1.14 l/min, p = 0.03). In the NS groups, bolus infusion resulted in both increased brain swelling (37.24 ± 1.63% vs. 26.74 ± 1.33%, p = 0.05) as well as lesion size (3285.44 ± 130.81 mm(3) vs. 2509.41 ± 297.44 mm3, p = 0.04). This was also associated with decreased cardiac output (NS: 4.37 ± 0.12 l/min vs. 6.35 ± 0.10 l/min, p < 0.01).
CONCLUSIONS:
In this clinically relevant model of combined TBI and HS, stepwise resuscitation protected the brain compared with bolusresuscitation.

| Tags : tbi, remplissage
10/11/2015
Dépakine chez le blessé cranien en choc ?
Treatment with a histone deacetylase inhibitor, valproic acid, is associated with increased platelet activation in alarge animal model of traumatic brain injury and hemorrhagic shock
Dekker SE et Al. J Surg Res. 2014 Jul;190(1):312-8
---------------------------
Le concept du damaged control resuscitation fait appel en partie à de nouvelles modalités transfusionnelles et d'emploi de fractions coagulantes. D'autres approches sont possibles comme celles visant à restuarer la fonction plaquettaire. C'est ce que permettrait l'adminsitration de médicaments appartenant à la classe des inhibiteurs des histone deacetylase et dont les effets neuroprotecteurs pourraient ainsi être mis à profit. Le document proposé semble conforter cette approche.
---------------------------
BACKGROUND:
We have previously shown that resuscitation with fresh frozen plasma (FFP) in a large animal model of traumatic brain injury (TBI) and hemorrhagic shock (HS) decreases the size of the brain lesion, and that addition of a histone deacetylase inhibitor, valproic acid (VPA), provides synergistic benefits. In this study, we hypothesized that VPA administration would be associated with a conservation of platelet function as measured by increased platelet activation after resuscitation.
MATERIALS AND METHODS:
Ten swine (42-50 kg) were subjected to TBI and HS (40% blood loss). Animals were left in shock for 2 h before resuscitation with either FFP or FFP+VPA (300 mg/kg). Serum levels of platelet activation markers transforming growth factor beta, CD40 L, P-selectin, and platelet endothelial cell adhesion molecule (PECAM) 1 were measured at baseline, postresuscitation, and after a 6-h observation period. Platelet activation markers were also measured in the brain whole cell lysates and immunohistochemistry.
RESULTS:
Circulating P-selectin levels were significantly higher in the FFP+VPA group compared with the FFP alone group (70.85±4.70 versus 48.44±7.28 ng/mL; P<0.01). Likewise, immunohistochemistry data showed elevated P-selectin in the VPA treatment group (22.30±10.39% versus 8.125±3.94%, P<0.01). Serum sCD40L levels were also higher in the FFP+VPA group (3.21±0.124 versus 2.38±0.124 ng/mL; P<0.01), as was brainsCD40L levels (1.41±0.15 versus 1.22±0.12 ng/mL; P=0.05). Circulating transforming growth factor beta levels were elevated in the FFP+VPA group, but this did not reach statistical significance (11.20±1.46 versus 8.09±1.41 ng/mL; P=0.17). Brain platelet endothelial cell adhesion molecule 1 levels were significantly lower in the FFP+VPA group compared with the FFP group (5.22±2.00 pg/mL versus 7.99±1.13 pg/mL; P=0.03).
CONCLUSIONS:
In this clinically relevant large animal model of combined TBI+HS, the addition of VPA to FFP resuscitation results in an early upregulation of platelet activation in the circulation and the brain. The previously observed neuroprotective effects of VPA may be due to a conservation of platelet function as measured by a higher platelet activation response after resuscitation.
| Tags : tbi, coagulopathie
02/11/2015
Mg++: Médicament de la coagulopathie ?
Both acute delivery of and storage with magnesium sulfate promote cold-stored platelet aggregation and coagulation function
Meledeo MA et Al. J Trauma Acute Care Surg. 2015 Oct;79(4 Suppl 2):S139-45
----------------------------------------
Il y a quelque mois était publié un travail de recherche portant sur l'intérêt de l'administration de Adénosine/Lidocaïne/Mg2+ ALM (1, 2, 3). Une hypothèse faite par les auteurs serait que L'ALM agirait comme un antifibrinolytique en activant la voie du thrombin-activatable fibrinolysis inhibitor (TAFI) plutôt que celle de la protéine C. Cette action passerait par un mécanisme antiinflammatoire, une modification de la polarité endothéliale et une action sur la fonction plaquettaire. Le travail expérimental dont l'abstract est présenté met en avant l'intérêt de l'adminsitration de magnésium pour la restauration de la fonction plaquettaire après conservation de palquettes d'aphérèse au delà de 5 jours.
----------------------------------------
BACKGROUND:
The platelet storage lesion causes loss of function and viability over time. A new paradigm for platelet storage is desired to enable safer, more effective transfusions while reducing waste. We hypothesized that repletion of Mg, which is chelated by citrate anticoagulant, could reduce platelet storage lesion severity when given in conjunction with storage at a refrigerated temperature.
METHODS:
Apheresis platelet units were collected from healthy donors and stored at 22°C or 4°C. On Days 0, 2, 4, and 8, samples were collected for analyses of receptor-mediated aggregation, coagulation, adhesion to collagen under flow, and viability. In the first series, samples were given anacute dose of MgSO4 before testing; in the second series, storage bags were supplemented with 0-, 3-, or 6-mM MgSO4.
RESULTS:
Acutely delivered MgSO4 induced a more rapid coagulation time in apheresis platelets, further enhanced by storage at 4°C. Plateletadhesion to a collagen surface while exposed to arterial shear rates (920 s) was enhanced by MgSO4 supplementation-acute MgSO4 had a large effect on adhesion of fresh platelets, which diminished more rapidly in 22°C samples, while storage with MgSO4 showed significant benefits even out to Day 4 at both temperatures. Although 4°C storage improves the longevity of platelet aggregation responses to agonists, MgSO4 supplementation did not change those responses.
CONCLUSION:
Acute MgSO4 reduces clot time likely through the transient increase of free Ca. Limited differences between platelet function inacute delivery of and storage with MgSO4 diminish the possibility that Mg-induced metabolic inhibition of platelets synergizes with 4°C storage. Regardless, magnesium supplementation to platelets is an exciting possibility in transfusion because the adhesion response of 22°C-stored platelets on Day 4 is significantly enhanced when stored with 6-mM MgSO4
| Tags : coagulopathie
23/10/2015
Quelle place pour les facteurs de la coagulation ?
| Tags : hémorragie, coagulopathie, choc
10/08/2015
Célo: Au frigo, c'est vraiment mieux
Impact of Temperature Exposure on Stability of Drugs in a Real-World Out-of-Hospital Setting
De Winter S. et Al. Ann Emerg Med. 2013 Oct;62(4):380-387
------------------------------------------
Le maintien au frais des médicaments de l'urgence est réglementé. Malheureusement le maintien à +4c de plusieurs médicaments de l'urgence n'est pas toujours possible. Ce travail plutôt récent confirme la sensibilité des ces derniers aux conditions de stockage. Il faut donc dès lors envisager le renouvellement très régulier de ces produits quand ils sont stockés de manière non conforme aux spécifications des fabriquants et quand les conditions sont extrêmes avoir recours à des solutions de transports comme celui-ci
------------------------------------------
Study objective:
The aim of this study is to determine the content of 5 important emergency medical services
(EMS) drugs after being stored at the recommended refrigerated temperature, room temperature, or in an emergency physician transport vehicle operating under real-world working conditions.
Methods:
Adrenaline hydrochloride, cisatracurium besylate, lorazepam, methylergonovine maleate, and succinylcholine chloride were stored for 1 year under the 3 conditions. For each storage condition, samples of the drugs were taken after 1, 2, 3, and 4 weeks and after 2, 4, 6, 8, 10, and 12 months. For adrenaline hydrochloride, however, the samples were taken after 1, 2, 4, 6, 8, 10, and 12 months. The samples were analyzed with a validated high-performance liquid chromatography assay. A drug was considered stable if its content was above 90%.
Results:
Adrenaline hydrochloride and methylergonovine maleate remained stable for 1 year at room temperature and in the emergency physician transport vehicle. At room temperature and in the emergency physician transport vehicle, lorazepam became unstable within 4 weeks. Succinylcholine chloride was stable for 2 months at room temperature and for 1 month in the emergency physician transport vehicle. Cisatracurium besylate became unstable within 4 months at room temperature. However, it remained stable for 4 months in the emergency physician transport vehicle.
Conclusion:
When stored at room temperature or in the emergency physician transport vehicle, lorazepam became unstable within weeks, whereas succinylcholine chloride and cisatracurium besylate became unstable within months. Adrenaline hydrochloride and methylergonovine maleate remained stable for several months, even under room temperature and emergency physician transport vehicle conditions. Thus, real-world EMS working conditions pose challenges for maintaining optimal efficacy of these important EMS drugs.
14/07/2015
Intranasal ? sans hésiter !
| Tags : intranasal
08/06/2015
Kétalar/Célo et plus de 40°C ?
Drugs and drug administration in extreme environments
Kupper TE et AL. J Travel Med. 2006 Jan-Feb;13(1):35-47.
------------------------------------------------------------
La question de la stabilité thermique des médicaments se pose dès lors les conditions de stockage sont extrêmes. C'est le cas actuellement dans la BSS. Récemment l'incidence plus élevée d'accidents allergiques à la succinylcholine a été rapportée, avec pour corollaire des recommandations spécifiques émises par l'ANSM. Ces dernières découlent d'une analyse bénéfice/risque au cours d'un exercice métroplitain. Le document qui suit est une revue de l'effet des conditions de stockage sur les médicaments de l'urgence. Dans bien des cas un emploi reste possible, notamment pour la kétamine et la succynilcholine, au prix d'une adaptation posologique. La destruction des ces produits doit rester la règle au delà de 15 j.
------------------------------------------------------------
Emergency medicine must often cope with harsh climates far below freezing point or high temperatures, and sometimes, an alternative to the normal route of drug administration is necessary. Most of this information is not yet published. Therefore, we summarized the information about these topics for most drugs used in medical emergencies by combining literature research with extensive personal communications with the heads of the drug safety departments of the companies producing these drugs. Most drugs can be used after temperature stress of limited duration. Nevertheless, we recommend replacing them at least once per year or after extreme heat. Knowledge about drugs used in extreme environments will be of increasing importance for medical personnel because in an increasingly mobile society, more and more people, and especially elderly — often with individual medical risks — travel to extreme regions such as tropical or arctic regions or to high altitude, and some of them need medical care during these activities. Because of this increasing need to use drugs in harsh climates (tourism, expeditions, peace corps, military, etc) the actual International Congress of Harmonization recommendations should be added with stability tests at +50°C, freezing and oscillating temperatures, and UV exposure to simulate the storage of the drugs at “ outdoor conditions. ”
17/01/2015
Le Gamma OH: Ne pas l'oublier
Utilisation du gamma-OH en médecine de guerre
Le Gamma OH est un vieux produit, bien mieux connu actuellement dans le monde de la toxicomanie et du dopage (1). Pourtant c'est aussi un agent d'induction et d'entretien d'anesthésie qui a été très utilisé. Il est progressivement tombé en désuétude du fait de la mise à disposition d'agents plus maniables comme le propofol, l'étomidate et le midazolam. C'est un neurotransmetteur inducteur de sommeil physiologique. Il réduit la pression intracrânienne et intraoculaire. Ses effets respiratoires sont minimes. Il augmente le tonus utérin. Il préserve une grande stabilité hémodynamique. Il est métabolisé en CO2 donc sans risque d'accumulation de métabolites, bien que certains être retrouvés dans les urines (pas longtemps) ou les cheveux (2). Il est responsable d'hypokaliémie, abaisse le seul épileptogène et utilisé seul entraîne une mydriase. (3)
Il n'est plus utilisé en anesthésie du fait de la lenteur de l'induction (au moins 10 min Après administration IV obligeant de l'associer à un agent d'induction de cinétique courte), la durée de ses effets (de l'ordre de 90 min en injection unique ne permettant pas un réveil rapide) et d'effets secondaires (notamment la survenue d'hypokaliémie)
Son emploi est pourtant simple, peu coûteux et ne nécessite pas de seringue autopulsée (50 à 70 mg/kg IV pour l'induction, puis 25 à 35 mg/kg toutes les heures IV) . Sa grande durée d’action peut être mise à profit lors de sédation pour des évacuations sanitaires longues. Ses effets secondaires peuvent ainsi être exploités dans certains contextes particuliers (afflux massif de blessé, lieu isolé) pour l’entretien de la sédation du patient intubé-ventilé, dans le contexte de traumatisés graves et notamment des traumatisés crâniens avec rhabdomyolyse et hyperkaliémie, voire un état de choc hypovolémique du syndrome des ensevelis ou crush syndrome. Tout autant de situations qui sont fréquents en contexte militaire.
Moins connu que la kétamine, cet agent d'anesthésie mérite qu'on s'y intéresse à nouveau (4).
16/01/2015
Kétamine dans le sac: On est serein
Ketamine: Use in Anesthesia
Marland S et Al. CNS Neurosci Ther. 2013 Jun;19(6):381-9
--------------------------------------------------------------
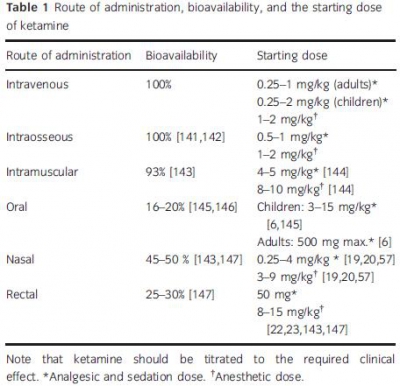
Une des raisons pour laquelle la Kétamine est d'intérêt majeur est la possibilité d'utiliser de multiples voies d'administration.
20/12/2014
La NAC: Intéressante en role 1: Probable ?
La N-acétylcystéine ou acétylcystéine ou NAC est un acide aminé non essentiel, qui stimule la production de glutathion, un antioxydant. Elle est surtout connue comme agent mucolytique. En médecine d'urgence son emploi lors d'intoxication au paracétamol est parfaitement validé. Moins connues sont les emplois de cet agent antioxydant dans deux types d'indication qui nous intéressent.
La première est le traumatisme sonore aigu notamment après explosion (1) ou tir (2) où il semblerait que la démarche classique [repos auditif, corticothérapie+/- vasodilatateurs] (3, 4) évoluerait vers une statégie associant le repos, la corticothérapie et unhe stratégie antioxydante précoce incluant le recours précoce à la N Acétyl Cystéine(5, 6).
La seconde porte sur la réduction des séquelles neurologiques après blast cérébral (7). Cet intérêt pour les effets anti-oxydants ne sont pas nouveaux et les effets «protecteurs» sont mis en avant également au niveau pulmonaire (8), rénale (9) et hépatique (10).
Si tout ceci reste à valider (11, 12), il semble que l'intégration de cette molécule ancienne soit d'un intérêt réel pour la prise en charge du combattant blasté ou exposéà un TSA à condition que l'administration soit précoce (<1h) (13) et donc que la N Acétyl Cystéine soit disponible en rôle 1
12/12/2014
HEA: Possible pour les trauma ouverts
Differences between blunt and penetrating trauma after resuscitation with hydroxyethyl starch
Casey JA et Al. J Trauma Acute Care Surg. 2014;77: 859-864
----------------------------------------------------------------
Ce travail effectué avec un HEA ancien (450/07: Hetastarch®, Hextent®) suggère que l'emploi des HEA lors de la prise en charge de trauma ouvert n'est pas associé à un risque accru de décès ou d'insuffisance rénale. On rappelle qu'il ne s'agit pas de la même classe d'HEA que celle que nous avons l'habitude d'utiliser (130/0.4: Voluven)
 ----------------------------------------------------------------
----------------------------------------------------------------
BACKGROUND: The purpose of this study was to test the hypothesis that a single bolus of 6% hydroxyethyl starch (HES 450/0.7 in lactated electrolyte injection) during initial resuscitation has a differential effect in blunt and penetrating trauma patients.
METHODS: Consecutive admissions to the trauma service were reviewed. Patients who died within 24 hours were excluded. Multivariate analysis defined individual predictors for the primary outcomes, acute kidney injury (AKI) and mortality within 90 days. Data were expressed as mean T SD, and significance was assessed at p G 0.05.
RESULTS: Therewere 1,410 patients (76% male; mean T SD, age 43 T 18 years; 68% blunt trauma; mean T SD Injury Severity Score [ISS] 14 T 11; AKI, 4.4%; and mortality, 3.4%). HES (0.5-1.5 L) was administered to 216 patients (15.3%). After multiple logistic regression, HES remained a significant independent predictor of AKI after blunt trauma (odds ratio [OR], 2.54; 95% confidence interval [CI], 1.24-5.19; area under the receiver operating characteristic curve [AUROC], 0.809) but not penetrating
trauma (OR, 0.90; 95% CI, 0.23-3.60; AUROC, 0.849). In separate logistic regression models, HES was a significant predictor of mortality after blunt trauma (OR, 3.77; 95% CI, 0.91-0.97; AUROC, 0.921) but not penetrating trauma (OR, 0.72; 95% CI, 0.13-3.94; AUROC, 0.904).
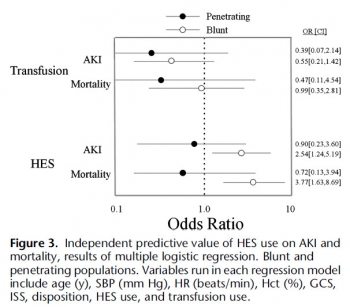
CONCLUSION: HES is an independent risk factor for AKI and death after blunt, but not penetrating, trauma, which underscores a fundamental difference between these two injury types.
| Tags : remplissage
30/10/2014
Plaquettes synthétiques: Possible ? Mais oui
Tuning Ligand Density on Intravenous Hemostatic Nanoparticles Dramatically Increases Survival Following Blunt Trauma
Proc Natl Acad Sci U S A. 2014 Jul 15;111 (28) 10293-10298
Des plaquettes synthétiques pour arrêter le saignement ? Certains l'ont fait grâce à la technologie des nanoparticules (1, 2). Un espoir qui reste à confirmer.
-----------------------------------------------------------------------------------
Explosions account for 79% of combat-related injuries, leading to multiorgan hemorrhage and uncontrolled bleeding. Uncontrolled bleeding is the leading cause of death in battlefield traumas as well as in civilian life. We need to stop the bleeding quickly to save lives, but, shockingly, there are no treatments to stop internal bleeding. A therapy that halts bleeding in a site-specific manner and is safe, stable at room temperature, and easily administered is critical for the advancement of trauma care. To address this need, we have developed hemostatic nanoparticles that are administered intravenously. When tested in a model of blast trauma with multiorgan hemorrhaging, i.v. administration of the hemostatic nanoparticles led to a significant improvement in survival over the short term (1 h postblast). No complications from this treatment were apparent out to 3 wk. This work demonstrates that these particles have the potential to save lives and fundamentally change trauma care.
-----------------------------------------------------------------------------------
| Tags : hémorragie
14/09/2014
HEA: Peut être un peu de sérénité ?
Hydroxyethyl Starches: A Tale of Two Contexts: The Problem of Knowledge
Weiskopf R. Anesth Analg. 2014 Sep;119(3):509-13.
Un débat moins passionné est en train de se mettre en place au sujet de la toxicité des HES. Le texte proposé en est un exemple. Il propose une relecture pertinente des études 6S, CHEST et surtout CRISTAL qui d'une certaine façon remet en question les deux précédentes. Il nous demande de prendre en compte plusieurs éléments : La diversité des HES, les différences qui peuvent exister entre une administration répétée en réanimation et une administration ponctuelle péri-opératoire. Il s'appuie sur deux écrits publiés dans le même numéro.
Raghunathan K et all. (Intravenous Starches: Is Suspension the Best Solution?) suggèrent que les solutions colloïdes sont à réserver pour les hypovolémies aiguës alors que Irwin et all. (Volume Therapy with Hydroxyethyl Starches: Are We Throwing the Anesthesia Baby Out with the Intensive Care Unit Bathwater?) estiment que le recours aux HES 130/0.4 est pleinement justifié en environnement périopératoire.
Cette démarche correspond au positionnement de la SFAR. Rappelons que la position actuelle des instances européennes est la suivante:
" Les solutions à base d’HEA peuvent être utilisées pour la réanimation des patients avec une hypovolémie causée par une perte aiguë de sang, quand les alternatives comme la perfusion de cristalloïdes seuls sont insuffisantes. Afin de limiter les risques potentiels, les solutions contenant des HEA ne devront pas être utilisées plus de 24 heures et la fonction rénale devra être monitorée après administration des HEA "
| Tags : remplissage
14/12/2013
Kétamine: Son intérêt en médecine de guerre
| Tags : kétamine
21/11/2013
Le plasma lyophilisé: Bon pour le cerveau du traumatisé qui saigne
Early treatment with lyophilized plasma protects the brain in a large animal model of combined traumatic brain injury and hemorrhagic shock
Imam AM et Al. J Trauma Acute Care Surg. 2013;75: 976-983
accéder aux abstracts de la WTA publiés dans J trauma Acute care
_____________________________________
Bien sûr une étude animale, mais une de plus qui milite pour un emploi précoce du plasma lyophylisé.
_____________________________________
BACKGROUND: Combination of traumatic brain injury (TBI) and hemorrhagic shock (HS) can result in significant morbidity and mortality. We have previously shown that early administration of fresh frozen plasma (FFP) in a large animal model of TBI and HS reduces the size of the brain lesion as well as the associated edema. However, FFP is a perishable product that is not well suited for use in the austere prehospital settings. In this study, we tested whether a shelf-stable, low-volume, lyophilized plasma (LSP) product was as effective as FFP.
METHODS:
Yorkshire swine (42-50 kg) were instrumented to measure hemodynamic parameters, intracranial pressure, and brain tissue oxygenation. A prototype, computerized, cortical impact device was used to create TBI through a 20-mm craniotomy: 15-mm cylindrical tipimpactor at 4 m/s velocity, 100-millisecond dwell time, and 12-mm penetration depth. Volume-controlled hemorrhage was induced(40-45% total blood volume) concurrent with the TBI. After 2 hours of shock, animals were treated with (1) normal saline (NS, n = 5), (2) FFP (n = 5), and (3) LSP (n = 5). The volume of FFP and LSP matched the shed blood volume, whereas NS was 3 times the volume. Six hours after resuscitation, brains were sectioned and stained with TTC (2, 3, 5-Triphenyltetrazolium chloride), and lesion size (mm3) and swelling (percent change in volume compared with the contralateral, uninjured side) were measured.
RESULTS:
This protocol resulted in a highly reproducible brain injury, with clinically relevant changes in blood pressure, cardiac output, tissue hypoperfusion, intracranial pressure, and brain tissue oxygenation. Compared with NS, treatment with LSP significantly ( p G 0.05) decreased brain lesion size and swelling (51% and 54%, respectively).
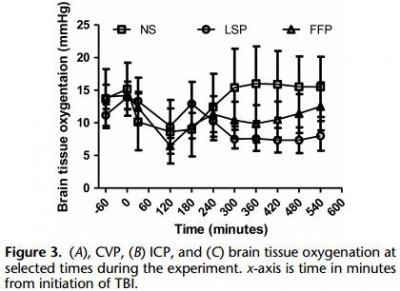
CONCLUSION: In a clinically realistic combined TBI + HS model, early administration of plasma products decreases brain lesion size and edema. LSP is as effective as FFP, while offering many logistic advantages.
| Tags : tbi, coagulopathie