31/03/2015
Intubation: Le médecin ou L'infirmier ? En fait il faut être bien formé
Role Allocation and Team Dynamics during Pre-Hospital Rapid Sequence Induction of Anaesthesia by a Physician-Critical Care Paramedic Team in the United Kingdom: A 12 Months Review of Practice
Crombie et al., J Anesth Clin Res 2015, 6:2
------------------------------------------------------------------
La procédure du sauvetage au combat prévoit que les IDE puissent être amenés à intuber un blessé au combat, y compris si un médecin n'est pas présent. Le travail proposé montre que cela est parfaitement possible grâce à une formation adaptée.
------------------------------------------------------------------
Background: Critical care paramedics working alongside physicians in the West Midlands MERIT scheme Medical Emergency Response Incident Team (MERIT) have been shown to demonstrate high levels of proficiency in laryngoscopy during Rapid Sequence Induction of anaesthesia (RSI). The MERIT SOP does not stipulate the team member who should be allocated the role of laryngoscopy during RSI. The aim of this study is to analyse and identify factors that influence role allocation in pre-hospital RSI performed by MERIT scheme personnel in the West Midlands.
Methods: We conducted a retrospective review from 12 months of our mission database for patients who had undergone pre-hospital RSI performed by MERIT. Data collected included the indication for RSI, the number of intubation attempts (including documented failures to intubate), documentation of predicted difficulty in intubation and the degree of airway soiling prior to RSI. The clinical role of the operator performing laryngoscopy was recorded for each attempt.
Results: 113 cases or pre-hospital RSI were identified. Critical care paramedics successfully intubated 49/58 (84.48%) cases in which they were allocated the first attempt at laryngoscopy. Success at first attempt lower for physicians (76.92%) but greater proportions of such cases involved patients at the extremes of age and heavy airway soiling with a wider range of indications.
Conclusions: As part of a multidisciplinary team working alongside physicians, Critical Care Paramedics successfully intubate the majority of patients at the first attempt in carefully selected groups. Further research to investigate other factors at scene that influence role allocation and team dynamics in pre-hospital RSI is required
| Tags : airway
Focus assessed transthoracic Echo (FATE)
Un document pdf qui synthétise les données à connaître pour l'examen échographique cardio-respiratoire. Une approche standardisée appelée est visualisable ici.
| Tags : échographie
29/03/2015
O2 pas mieux extrait lors de l'effort en altitude !
Systemic oxygen extraction during exercise at high altitude
Martin DS et Al. British Journal of Anaesthesia 114 (4): 677–82 (2015)
-----------------------------------------------------------------------------------
On pourrait penser que qu'un des mécanismes d'adaptation à l'effort conduit en haute altitude soit l'augmentation de l'extraction d'oxygène, il semble qu'il n'en soit rien. C'est ce que suggère le travail proposé qui avance par ailleurs que ceci serait en relation avec:
1. Une anomalie de diffusion tissulaire de l'oxygène notamment à cause de la baisse du gradient de pression partielle entre capillaire et mitochondrie, ceci étant associé à la réduction du temps de transit capillaire musculaire en rapport avec l 'effort.
2. Des anomalies régionales de besoins en oxygène avec hétérogénéité des débits sanguins régionaux.
3. La redistribution des débits sanguins musculaires vers les organes dits "nobles"
4. La réduction de la consommation au niveau mitochondrial
En altitude la consommation en oxygène est plus en rapport avec la consommation mitochondriale qu'avec la délivrance d'oxygène aux tissus.
Ces observations vont l 'opposé de ce que l'on peut observer en cas d'hémorragie. On peut se poser la question des mécanismes d'adaptations en cas d'hémorragie survenant dans les mêmes conditions. EN tous cas ne changeons rien, continuons d'en apporter.
-----------------------------------------------------------------------------------
Background.
Classic teaching suggests that diminished availability of oxygen leads to increased tissue oxygen extraction yet evidence to support this notion in the context of hypoxaemia, as opposed to anaemia or cardiac failure, is limited.
Methods.
At 75 m above sea level, and after 7–8 days of acclimatization to 4559 m, systemic oxygen extraction [C(a2v)O2] was calculated in five participants at rest and at peak exercise. Absolute [C(a2v)O2] was calculated by subtracting central venous oxygen content (CcvO2) from arterial oxygen content (CaO2 ) in blood sampled from central venous and peripheral arterial catheters, respectively. Oxygen uptake (VO˙ 2) was determined from expired gas analysis during exercise.
Results.
Ascent to altitude resulted in significant hypoxaemia; median (range) SpO2 87.1 (82.5–90.7)% and PaO2 6.6 (5.7–6.8) kPa. While absolute C(a-v)O2 was reduced at maximum exercise at 4559 m [83.9 (67.5–120.9) ml litre-1 vs 99.6 (88.0–151.3) ml litre-1 at 75 m, P¼0.043], there was no change in oxygen extraction ratio (OER) [C(a-v)O2/CaO2] between the two altitudes [0.52 (0.48–0.71) at 4559 m and 0.53 (0.49–0.73) at 75 m, P¼0.500]. Comparison of C(a-v)O2 at peak VO˙ 2 at 4559 m and the equivalent VO˙ 2 at sea level for each participant also revealed no significant difference [83.9 (67.5–120.9) ml litre1 vs 81.2 (73.0–120.7) ml litre-1 , respectively, P¼0.225].
Conclusion.
In acclimatized individuals at 4559 m, there was a decline in maximum absolute C(a-v)O2 during exercise but no alteration in OER calculated using central venous oxygen measurements. This suggests that oxygen extraction may have become limited after exposure to 7–8 days of hypoxaemia.
28/03/2015
Blast et squelette osseux: Lésions spécifiques ?
Blast Injury and the Human Skeleton: An Important Emerging Aspect of Conflict-Related Trauma.
Dussault C. et Al. J Forensic Sci. 2014 May;59(3):606-12 [Thèse]
--------------------------------------------------------------------
La rupture de la membrane du tympan en cas serait un marqueur peu fiable du blast et de sa gravité (1,2, 3). Il semblerait que certaines lésions osseuses soient assez spécifiques de blast osseux. Ceci a son intérêt en médecine médico-légale quand les circonstances de décès ne sont pas connues.
--------------------------------------------------------------------
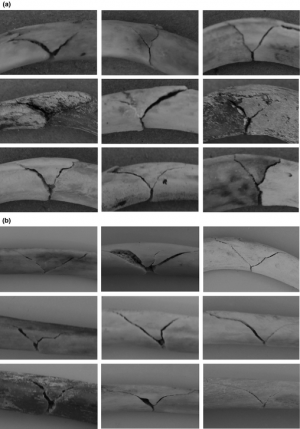
Recent decades have seen an accelerating trend in warfare whereby a growing proportion of conflict-related deaths have been caused by explosions. Analysis of blast injury features little in anthropological literature. We present a review of clinical literature that includes prevalence of injury to anatomical regions and potential indicators of blast injury which can be used by forensic anthropologists. This includes high prevalence of extremity (22.8–91.2%) and facial (19.6–40%) injury in combat contexts, lower limb fractures (19–74.3%) in suicide bombing, traumatic amputation (3–43%) and diffuse fracture patterns in terrorist bombings. Potential indicators of blast trauma include blowout fractures in sinus cavities from blast overpressure, transverse mandibular fractures, and visceral surface rib fractures. Ability to recognize blast trauma and distinguish it in the skeleton is of importance in investigations and judicial proceedings relating to war crimes, terrorism, and human rights violations and likely to become increasingly crucial to forensic anthropology knowledge.
--------------------------------------------------------------------
1. Les factures mandibulaires transverses
[Mandibular fractures in British military personnel secondary to blast trauma sustained in Iraq and Afghanistan. Breeze et al. Br J Oral Maxillofac Surg. 2011 Dec;49(8):607-11]
Elles portent essentiellement sur la symphyse et le corps alors qu'en traumatologie civile il s'agit essentiellement d'atteintes du condyle et de l'angle
2. Les fractures de plancher de type "Blow out"
Le cadre orbitaire reste intact. Le plancher de l'orbite est atteint. Il y a irruption du contenu orbitaire dans le sinus. Le risque est que ces fractures passent inaperçues. Cliniquement elle se traduise par une anomalie de l'occulomotricité.
3. Les fractures de cotes en aile de papillon
[Rib Butterfly Fractures as a Possible Indicator of Blast Trauma. Christensen et Al. J Forensic Sci. 2013 Jan;58 Suppl 1:S15-9.]

| Tags : blast
27/03/2015
Hypersalé: Mieux avec de la lidocaïne , du magnésium et de l'adénosine ?
Correction of acute traumatic coagulopathy with small-volume 7.5% NaCl adenosine, lidocaine, and Mg2+ occurs within 5 minutes: A ROTEM analysis
Hayley L. et Al. J Trauma Acute Care Surg. 2015;78: 773-783
------------------------------------------------------------------------------------------------
La prévention/correction de la coagulopathie traumatique est un axe essentiel de la réanimation du traumatisé grave. Le choix du soluté a son importance. L'adjonction de lidocaïne, de magnésium et d'adénosine au NaCl7,5% serait bénéfique. On observerait une fibrinolyse beaucoup moins importante qu'avec le salé hypertonique seul.
------------------------------------------------------------------------------------------------
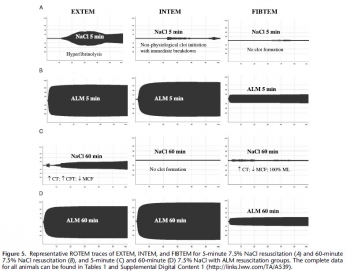
BACKGROUND: Acute traumatic coagulopathy is a major contributor to mortality and morbidity following hemorrhagic shock. Our aim was to examine the effect of small-volume 7.5% NaCl with adenosine, lidocaine, and Mg2+ (ALM) resuscitation on the timing of correction of coagulopathy in the rat model of severe hemorrhagic shock using ROTEM.
METHODS: Male rats (300Y450 g, n = 64) were randomly assigned to (1) baseline, (2) sham, (3) bleed, (4) shock, (5) 7.5% NaCl for 5 minutes, (6) 7.5% NaCl with ALM for 5 minutes, (7) 7.5% NaCl for 60 minutes, or (8) 7.5% NaCl with ALM for 60 minutes (all n = 8). For resuscitation, 0.3-mL intravenous bolus of 7.5% NaCl was administered with and without ALM (n = 8 each group). Hemodynamics and coagulopathy were assessed.
RESULTS: After hemorrhage, prothrombin time (PT) and activated partial thromboplastin time (aPTT) increased approximately four to six times, and ROTEM indicated hypocoagulopathy. After 60-minute shock, no sustainable clots could form. 7.5% NaCl increased mean arterial pressure (MAP) to 46 T 2 mm Hg at 5 minutes and generated a weak clot in EXTEM with hyperfibrinolysis in all tests. At 60 minutes, 7.5% NaCl failed to sustain MAP (43 T 5 mm Hg) and generate a viable clot. In direct contrast, 7.5% NaCl with ALM at 5 minutes resuscitatedMAP to 64 T 3 mm Hg, corrected PT and aPTT, and generated fully formed EXTEM and FIBTEM clots. At 60 minutes, MAP was 69 T 5 mm Hg, PT and aPTT were fully corrected, and > angle, clot amplitudes (A10, A30), as well as clot firmness and elasticity were not significantly different from baseline. ALM clot lysis at 60 minutes was significantly less than bleed, shock, or 7.5% NaCl, indicating protection against hyperfibrinolysis.
CONCLUSION: Small-volume 7.5% NaCl failed to resuscitate and correct coagulopathy. In contrast, 7.5% NaCl with ALM resuscitated MAP and corrected coagulopathy at 5 minutes, with further improvements at 60 minutes in clot kinetics, propagation, and firmness. ALM fully reversed hyperfibrinolysis to baseline. The possible mechanisms are discussed. (J Trauma Acute Care Surg. 2015;78:
| Tags : remplissage, coagulopathie
Salé, HEA, Plasma ou albumine ?
Is limited prehospital resuscitation with plasma more beneficial than using a synthetic colloid? An experimental study in rabbits with parenchymal bleeding
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2015;78: 752-759
----------------------------------------------------------
La recherche de la meilleure stratégie de remplissage vasculaire pour la prise en charge d'un traumatisé sévère relève de la quête du saint-Graal. L'article proposé rapporte un travail expérimental qui semble trouver in intérêt réel à l'emploi d'albumine 4%.
----------------------------------------------------------
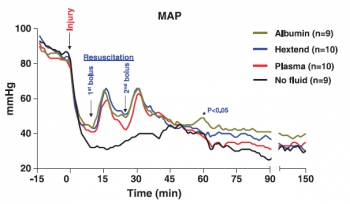
CONCLUSION:
Resuscitation with plasma or albumin better preserved coagulation function than did Hextend. However, despite these improvements, plasma resuscitation did not reduce blood loss or improve survival, while albumin administration seemed beneficial
| Tags : remplissage
26/03/2015
Techniques d'immobilisations
| Tags : immobilisation
24/03/2015
Airway et Echographie
| Tags : airway, échographie
22/03/2015
Western Journal of Emergency Médicine
PubMed Central Free Online Center
L'échographie: Investir de son temps pour avoir une pratique fiable
Ultrafest: A Novel Approach to Ultrasound in Medical Education Leads to Improvement in Written and Clinical Examinations
Connolly K et All. West J Emerg Med. 2015 Jan;16(1):143-8.
----------------------------------------------------------------------------------
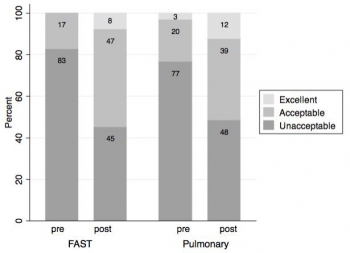
L'apprentissage de l'échographie est un impératif en médecine d'urgence. Cependant une véritable qualification ne peut être obtenue qu'au travers de formations universitaires assorties de pratiques réelles et régulières. La pratique des certains protocoles simplifiés comme le FAST serait d'acquisition plus simples. Aussi sont souvent proposées des formations de courtes durées. Ces dernières semblent en théorie très intéressantes en contexte militaire. Une analyse raisonnée de la réalité doit tempérer cet enthousiasme. Le travail présenté montre que si les connaissances théoriques des étudiants sont améliorées par une formation d'une journée, cette dernière ne permet pas l'acquisition d'une pratique suffisamment fiable. Ainsi la formation de nos personnels, qui repose souvent sur des formations de courtes durée, doit elle vue comme une découverte de cette pratique et non pas comme permettant l'acquisition d'un réel savoir faire.
Introduction:
Our objective was to evaluate the effectiveness of hands-on training at a bedside ultrasound (US) symposium (“Ultrafest”) to improve both clinical knowledge and image acquisition skills of medical students. Primary outcome measure was improvement in multiple choice questions on pulmonary or Focused Assessment with Sonography in Trauma (FAST) US knowledge. Secondary outcome was improvement in image acquisition for either pulmonary or FAST.
Methods:
Prospective cohort study of 48 volunteers at “Ultrafest,” a free symposium where students received five contact training hours. Students were evaluated before and after training for proficiency in either pulmonary US or FAST. Proficiency was assessed by clinical knowledge through written multiple-choice exam, and clinical skills through accuracy of image acquisition. We used paired sample t-tests with students as their own controls.
Results:
Pulmonary knowledge scores increased by a mean of 10.1 points (95% CI [8.9-11.3], p<0.00005), from 8.4 to a posttest average of 18.5/21 possible points. The FAST knowledge scores increased by a mean of 7.5 points (95% CI [6.3-8.7] p<0.00005), from 8.1 to a posttest average of 15.6/ 21. We analyzed clinical skills data on 32 students. The mean score was 1.7 pretest and 4.7 posttest of 12 possible points. Mean improvement was 3.0 points (p<0.00005) overall, 3.3 (p=0.0001) for FAST, and 2.6 (p=0.003) for the pulmonary US exam.
Conclusion:
This study suggests that a symposium on US can improve clinical knowledge, but is limited in achieving image acquisition for pulmonary and FAST US assessments. US training external to official medical school curriculum may augment students’ education
| Tags : échographie
21/03/2015
Eastern association for the surgery of trauma
Simulateur ou vecteur biologique ?
Randomized objective comparison of live tissue training versus simulators for emergency procedures
Hall AB. Am Surg. 2011 May;77(5):561-5.
-----------------------------------------------------------------------------------------
La simulation joue un rôle fondamental dans la foration aux gestes du sauvetage au combat. Le recours au vecteur biologique, au cadavre ou à des simulateurs artificiels reste sujet à débat. Le travail proposé montre que les simulatueurs artificiels sont aussi efficaces que les vecteurs biologiques. L'emploi de cadavres apparaît quand à lui poser le problème de leur disponibilité en nombre suffisant.
-----------------------------------------------------------------------------------------
There is a lack of objective analysis comparing live tissue and simulator training. This article aims to objectively determine the difference in outcomes. Twenty-four Air Force volunteers without prior experience performing emergency procedures were randomly assigned to receive training in tube thoracostomy (chest tube) and cricothyroidotomy training on either a pig model (Sus scrofa domestica) or on the TraumaMan simulator. One week posttraining, students were tested on human cadavers with objective and subjective results recorded. Average completion time for tube thoracostomy in the animal model group was 2 minutes 4 seconds and 1 minute 51 seconds in the simulator group with a mean difference of 12 seconds (P = 0.74). Average completion time for cricothyroidotomy in the animal model group was 2 minutes 35 seconds and 3 minutes 29 seconds in the simulator group with a mean difference of 53 seconds (P = 0.32). Overall confidence was 9 per cent higher in the animal trained group (P = 0.42). Success rate of cricothyroidotomy was 75 per cent in the animal model group and 58 per cent in the simulator-trained group (P = 0.67). Success rate of chest tube placement was 92 per cent in the animal group and 83 per cent in the simulator group (P = 1.00). There was no statistically significant difference in chest tube and cricothyroidotomy outcomes or confidence in the groups trained with live animal models or simulators at the 95 per cent confidence interval. Trends suggest a possible difference, but the number of cadavers required to reach greater than 95 per cent statistical confidence prohibited continuation of the study.
| Tags : simulateurs
Tourniquet: Efficace, uniquement si serré fort
Forward Assessment of 79 Prehospital Battlefield Tourniquet Use in the Current War
King DR et Al. J Spec Oper Med. 2012 Winter;12(4):33-8.
----------------------------------------------------------------------
La pose libérale d'un garrot est présentée comme étant un facteur essentiel de survie des blessés des membres. Encore faut il que ces derniers soient posés de manière correcte. Le document présenté laisse planer un gros doute. En effet il met en évidence qu'un garrot est mis en place 3 fois sur 4 alors qu'il n'y a pas de lésion vasculaire notable et que la plupart des garrots posés ne sont pas suffisamment serrés et sont en fait des garrots veineux. Pire seuls 1/3 des blessés ayant des lésions artérielles se voient appliquer un garrot artériel. C'est dire qu'une attention particulière doit être portée sur l'abolition du pouls artériel distal. Il s'agit là d'un enjeu pédagogique majeur.
----------------------------------------------------------------------
Introduction:
Battlefield tourniquet use can be lifesaving, but most reports are from hospitals with knowledge gaps remaining at the forward surgical team (FST). The quality of tourniquet applications in forward settings remain unknown. The purpose of this case series is to describe observations of tourniquet use at an FST in order to improve clinical performance.
Methods:
War casualties with tourniquet use presenting to an FST in Afghanistan in 2011 were observed. We identified appliers by training, device effectiveness, injury pattern, and clinical opportunities for improvement. Feedback was given to treating medics.
Results:
Tourniquet applications (79) were performed by special operations combat medics (47, 59%), flight medics (17, 22%), combat medics (12, 15%), and general surgeons (3, 4%). Most tourniquets were Combat Application Tourniquets (71/79, 90%). With tourniquets in place upon arrival at the FST, most limbs (83%, 54/65) had palpable distal pulses present; 17% were pulseless (11/65). Of all tourniquets, the use was venous in 83% and arterial in 17%. In total, there were 14 arterial injuries, but only 5 had effective arterial tourniquets applied.
Discussion:
Tourniquets are liberally applied to extremity injuries on the battlefield. 17% were arterial and 83% were venous tourniquets. When ongoing bleeding or distal pulses were appreciated, medics tightened tourniquets under surgeon supervision until distal pulses stopped. Medics were generally surprised at how tight a tourniquet must be to stop arterial flow–convert a venous tourniquet into an arterial tourniquet. Implications for sustainment training should be considered with regard to this life-saving skill.
| Tags : tourniquet, garrot, hémorragie
20/03/2015
Guidelines for field management of combat related head trauma
17/03/2015
Extraction dentaire improvisée
Sellick: Mieux vaut être formé pour faire.
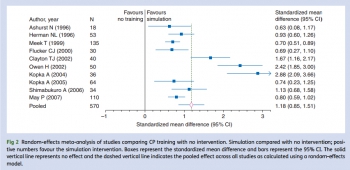
Cricoid pressure training using simulation: a systematic review and meta-analysis
Johnson RL et AL. Br J Anaesth. 2013 Sep;111(3):338-46
Le recours à la manoeuvre de Sellick est très controversé (1). Quelle que soit son efficacité réelle, une chose est certaine c'est qu'elle doit être correctement réalisée (2). L'application d'une pression cricoïdienne de 20N dès le début de l'induction pour atteindre 40N à la perte de conscience est requise (3). Le travail présenté met en évidence l'importance de la formation pour la maîtrrise de ce geste.
Clic sur l'image pour accéder au document
| Tags : airway
13/03/2015
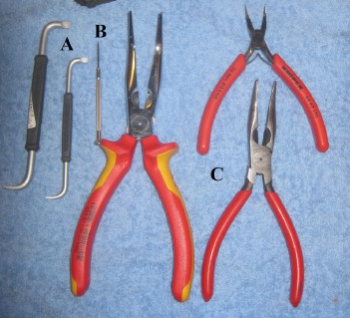
Simulation, simple est possible: La coniotomie
Il existe de nombreux simulateurs de coniotomie commerciaux. Ils sont onéreux tant à l'achat que dans leur entretien. Faire simple et peu onéreux est possible.
Premier exemple:
| Tags : coniotomie
Simulateur de crico: Un modèle animal facile
An Innovative and Inexpensive Model for Teaching Cricothyrotomy
Wang E. et Al Simul Healthc. 2007 Spring;2(1):25-9
Une trachée animale: Ici de boeuf
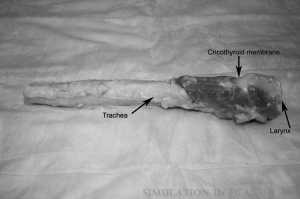
On couvre avec un emballage souple

On s'entraîne

| Tags : coniotomie
12/03/2015
Simulateur de crico: Pas cher, c'est possible
Every Surgical Resident Should Know How to Perform a Cricothyrotomy: An Inexpensive Cricothyrotomy Task Trainer for Teaching and Assessing Surgical Trainees.
Aho JM et Al. J Surg Educ. 2015 Feb 18. pii: S1931-7204(14)00346-8
OBJECTIVE:
Emergency cricothyrotomy is a rare but potentially lifesaving procedure. Training opportunities for surgical residents to learn this skill are limited, and many graduating residents have never performed one during their training. We aimed to develop and validate a novel and inexpensive cricothyrotomy task trainer that can be constructed from household items.
DESIGN:
A model was constructed using a toilet paper roll (trachea and larynx), Styrofoam (soft tissue), cardboard (thyroid cartilage), zip tie (cricoid), and fabric (skin). Participants were asked to complete a simulated cricothyrotomy procedure using the model. They were then evaluated using a 10-point checklist (5 points total) devised by 6 general surgeons. Participants were also asked to complete an anonymous survey rating the educational value and the degree of enjoyment regarding the model.

SETTING:
A tertiary care teaching hospital.
PARTICIPANTS:
A total of 54 students and general surgery residents (11 medical students, 32 interns, and 11 postgraduate year 3 residents).
RESULTS:
All 54 participants completed the training and assessment. The scores ranged from 0 to 5. The mean (range) scores were 1.8 (1-4) for medical students, 3.5 (1-5) for junior residents, and 4.9 (4-5) for senior-level residents. Medical students were significantly outperformed by junior- and senior-level residents (p < 0.001). Trainees felt that the model was educational (4.5) and enjoyable (4.0).
CONCLUSIONS:
A low-fidelity, low-cost cricothyrotomy simulator distinguished the performance of emergency cricothyrotomy between medical students and junior- and senior-level general surgery residents. This task trainer may be ideally suited to providing basic skills to all physicians in training, especially in settings with limited resources and clinical opportunities.
| Tags : coniotomie, matériel