25/11/2023
Intubation des traumas sévères pénétrants
Prehospital and emergency department airway management of severe penetrating trauma in Sweden during the past decade
Renberg M et Al. Scand J Trauma Resusc Emerg Med. 2023 Nov 24;31(1):85
------------------------------------
On sait cet exercice difficile même entre des mains expérimentées. Cet article le confirme. N'oublions pas; ce qui compte en premier c'est d'oxygéner. Avant de procéder à une intubation, bien évaluer l'état hémodynamique car une induction et une mise sous respirateur peuvent l'altérer, voire être responsable d'un arrêt cardiaque.
------------------------------------
Background:
Prehospital tracheal intubation (TI) is associated with increased mortality in patients with penetrating trauma, and the utility of prehospital advanced airway management is debated. The increased incidence of deadly violence in Sweden warrants a comprehensive evaluation of current airway management for patients with penetrating trauma in the Swedish prehospital environment and on arrival in the emergency department (ED).
Methods:
This was an observational, multicenter study of all patients with penetrating trauma and injury severity scores (ISSs) ≥ 15 included in the Swedish national trauma register (SweTrau) between 2011 and 2019. We investigated the frequency and characteristics of prehospital and ED TI, including 30-day mortality and patient characteristics associated with TI.
Result:
Of 816 included patients, 118 (14.5%) were intubated prehospitally, and 248 (30.4%) were intubated in the ED. Patients who were intubated prehospitally had a higher ISS, 33 (interquartile range [IQR] 25, 75), than those intubated in the ED, 25 (IQR 18, 34). Prehospital TI was associated with a higher associated mortality, OR 4.26 (CI 2.57, 7.27, p < 0.001) than TI in the ED, even when adjusted for ISS (OR 2.88 [CI 1.64, 5.14, p < 0.001]). Hemodynamic collapse (≤ 40 mmHg) and low GCS score (≤ 8) were the characteristics most associated with prehospital TI. Traumatic cardiac arrests (TCAs) occurred in 154 (18.9%) patients, of whom 77 (50%) were intubated prehospitally and 56 (36.4%) were intubated in the ED. A subgroup analysis excluding TCA showed that patients with prehospital TI did not have a higher mortality rate than those with ED TI, OR 2.07 (CI 0.93, 4.51, p = 0.068), with OR 1.39 (0.56, 3.26, p = 0.5) when adjusted for ISS.
Conclusion:
Prehospital TI was associated with a higher mortality rate than those with ED TI, which was specifically related to TCA; intubation did not affect mortality in patients without cardiac arrest. Mortality was high when airway management was needed, regardless of cardiac arrest, thereby emphasizing the challenges posed when anesthesia is needed. Several interventions, including whole blood transfusions, the implementation of second-tier EMS units and measures to shorten scene times, have been initiated in Sweden to counteract these challenges. Sweden.
| Tags : intubation, airway
03/04/2023
Laryngoscopie ? McGrath +++
A multicentre randomised controlled trial of the McGrath Mac videolaryngoscope versus conventional laryngoscopy
M Kriege M et All. Anaesthesia. 2023 Mar 16. doi: 10.1111/anae.15985.
Before completion of this study, there was insufficient evidence demonstrating the superiority of videolaryngoscopy compared with direct laryngoscopy for elective tracheal intubation. We hypothesised that using videolaryngoscopy for routine tracheal intubation would result in higher first-pass tracheal intubation success compared with direct laryngoscopy. In this multicentre randomised trial, 2092 adult patients without predicted difficult airway requiring tracheal intubation for elective surgery were allocated randomly to either videolaryngoscopy with a Macintosh blade (McGrath) or direct laryngoscopy. First-pass tracheal intubation success was higher with the McGrath (987/1053, 94%), compared with direct laryngoscopy (848/1039, 82%); absolute risk reduction (95%CI) was 12.1% (10.9-13.6%). This resulted in a relative risk (95%CI) of unsuccessful tracheal intubation at first attempt of 0.34 (0.26-0.45; p < 0.001) for McGrath compared with direct laryngoscopy. Cormack and Lehane grade ≥ 3 was observed more frequently with direct laryngoscopy (84/1039, 8%) compared with McGrath (8/1053, 0.7%; p < 0.001) No significant difference in tracheal intubation-associated adverse events was observed between groups. This study demonstrates that using McGrath videolaryngoscopy compared with direct laryngoscopy improves first-pass tracheal intubation success in patients having elective surgery. Practitioners may consider using this device as first choice for tracheal intubation.
| Tags : intubation, airway
01/04/2023
Trauma des voies aériennes
Blunt and Penetrating Airway Trauma
Duggan LV et Al.. Emerg Med Clin North Am. 2023 Feb;41(1S):e1-e15.
-----------------------------
C'est une chose compliquée, pas simple surtout en condition de combat et qui justifie la maîtrise d'un abord chirurgical du cou. Ce document est, je trouve, excellent.
-----------------------------
Airway injury, be that penetrating or blunt, is a high-stakes high-stress management challenge for any airway manager and their team. Penetrating and blunt airway injury vary in injury patterns requiring prepracticed skills and protocols coordinating care between specialties. Variables including patient cooperation, coexisting injuries, cardiorespiratory stability, care location (remote vs tertiary care center), and anticipated course of airway injury (eg, oxygenating well and comfortable vs increasing subcutaneous emphysema) all play a role in determining airway if and when airway management is required. Direct airway trauma is relatively infrequent, but its presence should be accompanied by in-person or virtual otolaryngology support.
| Tags : airway
04/10/2022
NAEMSP Prehospital Airway Position Papers
The National Association of EMS Physicians Compendium of Airway Management Position Statements and Resource Documents
Clic sur le titre pour accéder à la page de présentation des documents
| Tags : airway
26/09/2020
Le doigt plutôt qu'un guide
Front-of-neck airway rescue with impalpable anatomy during a simulated cannot intubate, cannot oxygenate scenario: scalpel-finger-cannula versus scalpel-finger-bougie in a sheep model
Heard A. et All. Br J Anaesth. 2020 Aug;125(2):184-191.----------------
Une situation au final rare mais c'est pour ce genre d'évènements qu'un médecin ENTRAÎNE est sur place. C'est clair.
Background: Front-of-neck airway rescue in a cannot intubate, cannot oxygenate (CICO) scenario with impalpable anatomy is particularly challenging. Several techniques have been described based on a midline vertical neck incision with subsequent finger dissection, followed by either a cannula or scalpel puncture of the now palpated airway. We explored whether the speed of rescue oxygenation differs between these techniques.
Methods: In a high-fidelity simulation of a CICO scenario in anaesthetised Merino sheep with impalpable front-of-neck anatomy, 35 consecutive eligible participants undergoing airway training performed scalpel-finger-cannula and scalpel-finger-bougie in a random order. The primary outcome was time from airway palpation to first oxygen delivery. Data, were analysed with Cox proportional hazards.
Results: Scalpel-finger-cannula was associated with shorter time to first oxygen delivery on univariate (hazard ratio [HR]=11.37; 95% confidence interval [CI], 5.14-25.13; P<0.001) and multivariate (HR=8.87; 95% CI, 4.31-18.18; P<0.001) analyses. In the multivariable model, consultant grade was also associated with quicker first oxygen delivery compared with registrar grade (HR=3.28; 95% CI, 1.36-7.95; P=0.008).
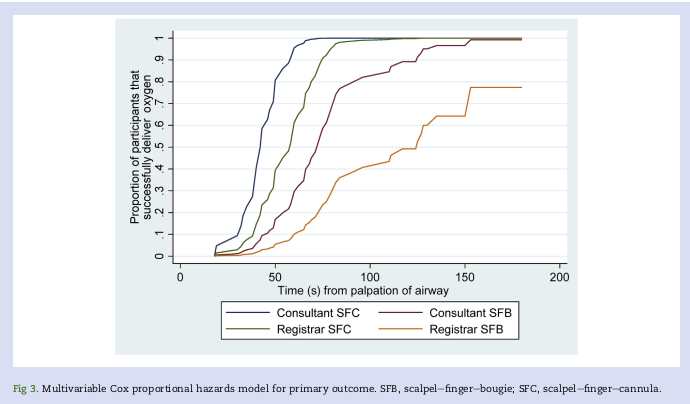
With scalpel-finger-cannula, successful oxygen delivery within 3 min of CICO declaration and ≤2 attempts was more frequent; 97% vs 63%, P<0.001. In analyses of successful cases only, scalpel-finger-cannula resulted in earlier improvement in arterial oxygen saturations (-25 s; 95% CI, -35 to -15; P<0.001), but a longer time to first capnography reading (+89 s; 95% CI, 69 to 110; P<0.001). No major complications occurred in either arm.
Conclusions: The scalpel-finger-cannula technique was associated with superior oxygen delivery performance during a simulated CICO scenario in sheep with impalpable front-of-neck anatomy.
| Tags : airway
24/10/2019
Trauma airways: Une revue
Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment.
Prokakis C et Al. J Cardiothorac Surg. 2014 Jun 30;9:117.
Airway injuries are life threatening conditions. A very little number of patients suffering air injuries are transferred live at the hospital. The diagnosis requires a high index of suspicion based on the presence of non-specific for these injuries symptoms and signs and a thorough knowledge of the mechanisms of injury. Bronchoscopy and chest computed tomography with MPR and 3D reconstruction of the airway represent the procedures of choice for the definitive diagnosis. Endotracheal intubation under bronchoscopic guidance is the key point to gain airway control and appropriate ventilation. Primary repair with direct suture or resection and an end to end anastomosis is the treatment of choice for patients suffering from tracheobronchial injuries (TBI). The surgical approach to the injured airway depends on its location. Selected patients, mainly with iatrogenic injuries, can be treated conservatively as long as the injury is small (<2 cm), a secure and patent airway and adequate ventilation are achieved, and there are no signs of sepsis. Patients with delayed presentation airway injuries should be referred for surgical treatment. Intraoperative evaluation of the viability of the lung parenchyma beyond the site of stenosis/obstruction is mandatory to avoid unnecessary lung resection.
| Tags : airway
25/04/2019
Anesthésie PréHosp: Recos scandinave
| Tags : airway
16/04/2019
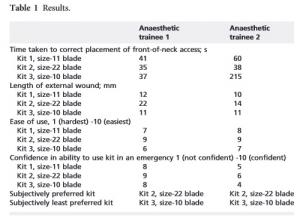
Coniotomie: Plutôt une lame de 22
Front-of-neck access technique and scalpels
Clic sur l'image pour accéder au document
| Tags : airway
07/04/2019
ControlCric: Plutôt à éviter
Necessity to depict difficult neck anatomy for training of cricothyroidotomy: A pilot study evaluating two surgical devices on a new hybrid training model.
BACKGROUND:
Everyone dealing with airway emergencies must be able to accomplish cricothyroidotomy, which cannot be trained in real patients. Training models are necessary.
OBJECTIVE:
To evaluate the suitability of a hybrid training model combining synthetic and porcine parts to depict variable neck anatomy.
DESIGN:
Model-based comparative trial.
SETTING:
Armed Forces Hospital Ulm, Germany, August 2018.
INTERVENTION:
On four anatomical neck variations (long slim/long obese/short slim/short obese) we performed two surgicalrapproaches to cricothyroidotomy (SurgiCric II vs. ControlCric).
PARTICIPANTS:
Forty-eight volunteers divided into two groups based on their personal skill level: beginners group and proficient performers group.
MAIN OUTCOME MEASURES:
Time to completion was recorded for each procedure. Once the operator had indicated completion, the correct anatomical tube placement was confirmed by dissection and structures were inspected for complications. Primary outcomes were successful tracheal placement of an airway tube and time needed to achieve a patent airway. Secondary outcome was assessment of complications.
RESULTS:
Overall, 384 procedures were performed. Median time to completion was 74 s. In total, 284 procedures (74%) resulted in successful ventilation. Time to completion was longer in short obese than in long slim and the risk of unsuccessful procedures was increased in short obese compared with long slim. Even if ControlCric resulted in faster completion of the procedure, its use was less successful and had an increased risk of complications compared with SurgiCric II. Proficient performers group performed faster but had an increased risk of injuring the tracheal wall compared with beginners group.
CONCLUSION:
Participants had difficulties in performing cricothyroidotomy in obese models, but various and difficult anatomical situations must be expected in airway management and therefore must be taught. A new hybrid model combining porcine and synthetic materials offers the necessary conditions for the next step in training of surgical airway procedures.
| Tags : airway
27/03/2019
Management of tracheal intubation in critically ill adults
| Tags : airway
03/03/2019
Crico: Simulation classique = Haute fidélité
A high-fidelity simulator for needle cricothyroidotomy training is not associated with increased proficiency compared with conventional simulators: A randomized controlled study.
BACKGROUND:
A high-fidelity task simulator for cricothyroidotomy was created using data from a 3-dimensional (3D) computed tomography scan using a 3D printer. We hypothesized that this high-fidelity cricothyroidotomy simulator results in increased proficiency for needle cricothyroidotomy compared with conventional simulators.
METHODS:
Cricothyroidotomy-naive residents were recruited and randomly assigned to 2 groups, including simulation training with a conventional simulator (Group C) and with a high-fidelity simulator (Group 3D). After simulation training, participants performed cricothyroidotomy using an ex vivo porcine larynx fitted with an endoscope to record the procedure. The primary outcomes were success rate and procedure time. The secondary outcome was a subjective measure of the similarity of the simulator to the porcine larynx.
RESULTS:
Fifty-two residents participated in the study (Group C: n = 27, Group 3D: n = 25). There was no significant difference in the success rate or procedure time between the 2 groups (success rate: P = .24, procedure time: P = .34). There was no significant difference in the similarity of the simulators to the porcine larynx (P = .81).
CONCLUSION:
We developed a high-fidelity simulator for cricothyroidotomy from 3D computed tomography data using a 3D printer. This anatomically high-fidelity simulator did not have any advantages compared with conventional dry simulators.
| Tags : airway, coniotomie
05/12/2018
Crico: Manque d'expérience/Entraînement
Emergency front-of-neck airway by ENT surgeons and residents: A dutch national survey
----------------------------
Ce travail hollandais met en avant le caractère non anecdotique des accès chirurgicaux aux voies aériennes. Pour les chirurgiens ORL hollandais, il s'agit essentiellement de trachéotomies. Le faible recours à la coniotomie s'explique surtout par le manque d'entraînement et d'équipements spécifiques. L'article souligne l'importance des démarches d'acquisition et de maintien des compétences, ce qui ne doit pas nous étonner. Comme pour les chirurgiens ORL le besoin d'un programme structuré de formations à l'accès aux voies aériennes en condition de combat est un impératif.
----------------------------
Objectives:
ENT surgeons and anesthesiologists work closely together in managing challenging airway cases. Sharing knowledge, experiences, and expectations interdisciplinary is essential in order to facilitate decision-making and adequate management in emergency front-of-neck airway cases.
Methods:
A survey was performed, to analyze level of experience, technique of preference, training, knowledge of material and protocols, and self-efficacy scores of Dutch ENT surgeons and residents in performing an urgent or emergency front-of-neck airway.
Results:
Within one year (January 2014-2015), 25.7% of the 257 respondents had performed an urgent or emergency front-of-neck airway. Of all reported emergency front-of-neck airways (N = 30), 80% were managed by tracheotomy. In future emergency front-of-neck airway cases, 74% stated cricothyrotomy would be their technique of preference. The majority would choose an uncuffed large-bore cannula technique. Post-academic hands-on training was attended by 42% of respondents. Self-efficacy scores were highest for surgical tracheotomy, and higher when trained or experienced. In case of an emergency scenario, 8.6% would not perform a front-of-neck airway themselves.


The main reasons for reluctance to start in general were lack of experience and lack of training. Reported items for improvement were mainly the development of a protocol and training.
Conclusion:
The chance of encountering an airway emergency scenario requiring front-of-neck airway is realistic. There is inconsistency between advised technique, technique of preference and technique actually performed by ENT surgeons. This study shows that there is both a need and desire for improvement in training and organization of care. Interdisciplinary guidelines and education is needed and could eventually safe lives.
| Tags : airway
02/12/2018
Crico: Incisez VERTICAL et LARGE
Emergency cricothyroidotomy: an observational study to estimate optimal incision position and length
Background
A vertical incision is recommended for cricothyroidotomy when the anatomy is impalpable, but no evidence-based guideline exists regarding optimum site or length. The Difficult Airway Society guidelines, which are based on expert opinion, recommend an 80–100 mm vertical caudad to cephalad incision in the extended neck position. However, the guidelines do not advise the incision commencement point. We sought to determine the minimum incision length and commencement point above the suprasternal notch required to ensure that the cricothyroid membrane would be accessible within its margins.
Methods
We measured using ultrasound, in 80 subjects (40 males and 40 females) without airway pathology, the distance between the suprasternal notch and the cricothyroid membrane, in the neutral and extended neck positions. We assessed the inclusion of the cricothyroid membrane within theoretical incisions of 0–100 mm in length made at 10 mm intervals above the suprasternal notch.
Results
In 80 subjects (40 males and 40 females), the distance ranged from 27 to 105 mm. Movement of the cricothyroid membrane on transition from the neutral to extended neck position varied from 15 mm caudad to 27 mm cephalad.
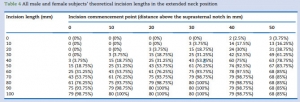
The minimum incision required in the extended position was 70 mm in males and 80 mm in females, commencing 30 mm above the suprasternal notch.
Conclusions
An 80 mm incision commencing 30 mm above the suprasternal notch would include all cricothyroid membrane locations in the extended position in patients without airway pathology, which is in keeping with the Difficult Airway Society guidelines recommended incision length.
| Tags : airway
05/10/2018
Conio: Echo, cela se confirme
Ultrasound Is Superior to Palpation in Identifying the Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical Trial.
BACKGROUND: Success of a cricothyrotomy is dependent on accurate identification of the cricothyroid membrane. The objective of this study was to compare the accuracy of ultrasonography versus external palpation in localizing the cricothyroid membrane.
METHODS:
In total, 223 subjects with abnormal neck anatomy who were scheduled for neck computed-tomography scan at University Health Network hospitals in Toronto, Canada, were randomized into two groups: external palpation and ultrasound. The localization points of the cricothyroid membrane determined by ultrasonography or external palpation were compared to the reference midpoint (computed-tomography point) of the cricothyroid membrane by a radiologist who was blinded to group allocation. Primary outcome was the accuracy in identification of the cricothyroid membrane, which was measured by digital ruler in millimeters from the computed-tomography point to the ultrasound point or external-palpation point. Success was defined as the proportion of accurate attempts within a 5-mm distance from the computed-tomography point to the ultrasound point or external-palpation point.
RESULTS:
The percentage of accurate attempts was 10-fold greater in the ultrasound than external-palpation group (81% vs. 8%; 95% CI, 63.6 to 81.3%; P < 0.0001). The mean (SD) distance measured from the external-palpation to computed-tomography point was five-fold greater than the ultrasound to the computed-tomography point (16.6 ± 7.5 vs. 3.4 ± 3.3 mm; 95% CI, 11.67 to 14.70; P < 0.0001).
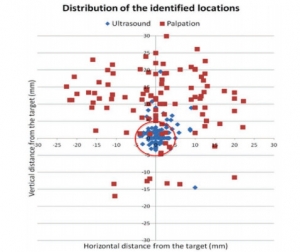
Analysis demonstrated that the risk ratio of inaccurate localization of the cricothyroid membrane was 9.14-fold greater with the external palpation than with the ultrasound (P < 0.0001). There were no adverse events observed.
CONCLUSIONS:
In subjects with poorly defined neck landmarks, ultrasonography is more accurate than external palpation in localizing the cricothyroid membrane.
| Tags : airway, coniotomie
30/09/2018
US: Mieux que la main pour la conio
A multicentre prospective cohort study of the accuracy of conventional landmark technique for cricoid localisation using ultrasound scanning
Cricoid pressure is employed during rapid sequence induction to reduce the risk of pulmonary aspiration. Correct application of cricoid pressure depends on knowledge of neck anatomy and precise identification of surface landmarks. Inaccurate localisation of the cricoid cartilage during rapid sequence induction risks incomplete oesophageal occlusion, with potential for pulmonary aspiration of gastric contents. It may also compromise the laryngeal view for the anaesthetist. Accurate localisation of the cricoid cartilage therefore has relevance for the safe conduct of rapid sequence induction.
We conducted a multicentre, prospective cohort study to determine the accuracy of cricoid cartilage identification in 100 patients. The cranio‐caudal midpoint of the cricoid cartilage was identified by a qualified anaesthetic assistant using the conventional landmark technique and marked. While maintaining the patient in the same position, a second mark was made by identifying the midpoint of the cricoid cartilage using ultrasound scanning.
The mean (SD) distance between the two marks was 2.07 (8.49) mm. In 41% of patients the midpoint was incorrectly identified by a margin greater than 5 mm. This error was uniformly distributed both above and below the midpoint of the cricoid cartilage. The Pearson correlation coefficient of this error with respect to body mass index was 0.062 (p = 0.539) and with age was −0.020 (p = 0.843). There were also no significant differences in error between male and female patients.
Identification of cricoid position using a landmark technique has a high degree of variability and has little correlation with age, sex or body mass index. These findings have significant implications for the safe application of cricoid pressure in the context of rapid sequence induction.
| Tags : airway, coniotomie
23/09/2018
ISR par des non médecins: Oui possible
Prehospital Rapid Sequence Intubation by Intensive Care Flight Paramedics.
OBJECTIVE:
Rapid sequence intubation (RSI) is an advanced airway procedure for critically ill or injured patients. Paramedic-performed RSI in the prehospital setting remains controversial, as unsuccessful or poorly conducted RSI is known to result in significant complications. In Victoria, intensive care flight paramedics (ICFPs) have a broad scope of practice including RSI in both the adult and pediatric population. We sought to describe the success rates and characteristics of patients undergoing RSI by ICFPs in Victoria, Australia.
METHODS:
A retrospective data review was conducted of adult (≥ 16 years) patients who underwent RSI by an ICFP between January 1, 2011, and December 31, 2016. Data were sourced from the Ambulance Victoria data warehouse.
RESULTS:
A total of 795 cases were included in analyses, with a mean age of 45 (standard deviation = 19.6) years. The majority of cases involved trauma (71.7%), and most patients were male (70.1%). Neurological pathologies were the most common clinical indication for RSI (68.3%). The first pass success rate of intubation was 89.4%, and the overall success rate was 99.4%. Of the 5 failed intubations (0.6%), all patients were safely returned to spontaneous respiration. Two patients were returned via bag/valve/mask (BVM) support alone, two with BVM and oropharyngeal airway, and one via supraglottic airway. No surgical airways were required. Overall, we observed transient cases of hypotension (5.2%), hypoxemia (1.3%), or both (0.1%) in 6.6% of cases during the RSI procedure.
CONCLUSION:
A very high RSI procedural success rate was observed across the study period. This supports the growing recognition that appropriately trained paramedics can perform RSI safely in the prehospital environment.
| Tags : airway
22/09/2018
Echo pour l'intubation
Integration of Point-of-care Ultrasound during Rapid Sequence Intubation in Trauma Resuscitation.
Introduction:
Airway and breathing management play critical role in trauma resuscitation. Early identification of esophageal intubation and detection of fatal events is critical. Authors studied the utility of integration of point-of-care ultrasound (POCUS) during different phases of rapid sequence intubation (RSI) in trauma resuscitation.
Methods:
It was prospective, randomized single-centered study conducted at the Emergency Department of a level one trauma center. Patients were divided into ultrasonography (USG) and clinical examination (CE) arm. The objectives were to study the utility of POCUS in endotracheal tube placement and confirmations and identification of potentially fatal conditions as tracheal injury, midline vessels, paratracheal hematoma, vocal cord pathology, pneumothorax, and others during RSI. Patient >1 year of age were included. Time taken for procedure, number of incorrect intubations, and pathologies detected were noted. The data were collected in Microsoft Excel spread sheets and analyzed using Stata (version 11.2, Stata Corp, Texas, U. S. A) software.
Results:
One hundred and six patients were recruited. The mean time for primary survey USG versus CE arm was (20 ± 10.01 vs. 18 ± 11.03) seconds. USG detected four pneumothorax, one tracheal injury, and one paratracheal hematoma. The mean procedure time USG versus CE arm was (37.3 ± 21.92 vs. 58 ± 32.04) seconds. Eight esophageal intubations were identified in USG arm by POCUS and two in CE arm by EtCO2 values.
Conclusion:
Integration of POCUS was useful in all three phases of RSI. It identified paratracheal hematoma, tracheal injury, and pneumothorax. It also identified esophageal intubation and confirmed main stem tracheal intubation in less time compared to five-point auscultation and capnography.
| Tags : airway
21/09/2018
Coniotomie: Control-Cric pas optimal
A Randomized Comparative Assessment of Three Surgical Cricothyrotomy Devices on Airway Mannequins.
Dorsam J et Al. Prehosp Emerg Care. 2018 Sep 1:1-30
-------------
La réalisation d'une coniotomie peut se faire par voie percutanée avec mandrin souple ou chirurgical, aidée ou pas d'une bougie. L'armée américaine recommande dans sa dernière révision du TCCC le recours à un dispositif appelé control-kit. Les données sur lesquelles reposent une telle proposition sont minces. Ce travail n'est clairement pas en sa faveur, du moins sur le modèle de moulage utilisé pour l'étude. La référence reste donc la technique chirurgicale.
-------------
BACKGROUND:
Airway obstruction is the second leading cause of preventable battlefield death, at least in part because surgical cricothyrotomy (SC) failure rates remain unacceptably high. Ideally, SC should be a rapid, simple, easily-learned, and reliably-performed procedure. Currently, Tactical Combat Casualty Care (TCCC) has approved three SC devices: The Tactical CricKit® (TCK), Control-Cric™(CC), and Bougie-assisted Technique (BAT). However, no previous studies have compared these devices in application time, application success, user ratings, and user preference.
METHODS:
United States Navy Corpsmen (N = 25) were provided 15 minutes of standardized instruction, followed by hands-on practice with each device on airway mannequins. Participants then performed SC with each of the three devices in a randomly assigned sequence. In this within-subjects design, application time, application success, participant ratings, and participant preference data were analyzed using repeated-measures ANOVA, regression, and non-parametric statistics at p < 0.05.
RESULTS:
Application time for CC (M = 184 sec, 95% CI 144-225 sec) was significantly slower than for BAT (M = 135 sec, 95% CI 113-158 sec, p < 0.03) and TCK (M = 117 sec, 95% CI 93-142 sec, p < 0.005). Success was significantly greater for BAT (76%) than for TCK (40%, p < 0.02) and trended greater than CC (48%, p = 0.07).
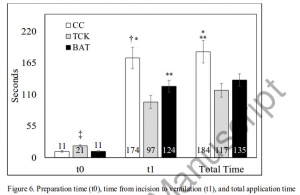
CC was rated significantly lower than TCK and BAT in ease of application, effectiveness, and reliability (each p < 0.01). User preference was significantly (p < 0.01) higher for TCK (58%) and BAT (42%) than for CC (0%). Improved CC blade design was the most common user suggestion.
CONCLUSION:
While this study was limited by the use of mannequins in a laboratory environment, present results indicate that none of these devices was ideal for performing SC. Based on slow application times, low success rates, and user feedback, the Control-Cric™ cannot be recommended until improvements are made to the blade design.
| Tags : airway
Airway Ultrasound
| Tags : airway
16/09/2018
Airway, pour être au RDV: S'entraîner
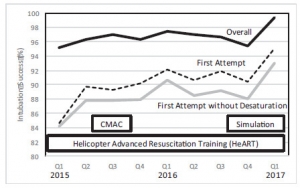
A Continuous Quality Improvement Airway Program Results in Sustained Increases in Intubation Success.
INTRODUCTION:
Airway management is a critical skill for air medical providers, including the use of rapid sequence intubation (RSI) medications. Mediocre success rates and a high incidence of complications has challenged air medical providers to improve training and performance improvement efforts to improve clinical performance.
OBJECTIVES:
The aim of this research was to describe the experience with a novel, integrated advanced airway management program across a large air medical company and explore the impact of the program on improvement in RSI success.
METHODS:
The Helicopter Advanced Resuscitation Training (HeART) program was implemented across 160 bases in 2015. The HeART program includes a novel conceptual framework based on thorough understanding of physiology, critical thinking using a novel algorithm, difficult airway predictive tools, training in the optimal use of specific airway techniques and devices, and integrated performance improvement efforts to address opportunities for improvement. The C-MAC video/direct laryngoscope and high-fidelity human patient simulation laboratories were implemented during the study period. Chi-square test for trend was used to evaluate for improvements in airway management and RSI success (overall intubation success, first-attempt success, first-attempt success without desaturation) over the 25-month study period following HeART implementation.
RESULTS:
A total of 5,132 patients underwent RSI during the study period. Improvements in first-attempt intubation success (85% to 95%, p < 0.01) and first-attempt success without desaturation (84% to 94%, p < 0.01) were observed. Overall intubation success increased from 95% to 99% over the study period, but the trend was not statistically significant (p = 0.311).
CONCLUSIONS:
An integrated advanced airway management program was successful in improving RSI intubation performance in a large air medical company.
| Tags : airway