30/08/2011
Exacyl: Bon aussi pour le blessé de guerre !
Une étude à paraître conduite par une équipe US a mis en évidence l'intérêt de l'acide tranexaminique.
----------------
Tranexamic acid decreases mortality following wartime injury: the Military Application of Tranexamic acid in Trauma Emergency Resuscitation Study (MATTERS) MAJ Jonathan J. Morrison, MB ChB, MRCS, RAMC(V), LT COL (sel) Joseph J. Dubose, MD, USAF MC, COL Todd E. Rasmussen, MD, USAF MC, SURG CAPT Mark Midwinter, BMedSci, MD FRCS RN
http://archsurg.ama-assn.org/cgi/content/short/archsurg.2...
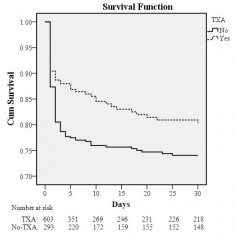
A recent registry-based study of combat injured troops receiving blood in Afghanistan (January 2009 - December 2010) at the Bastion Role 3 facility has demonstrated findings supportive of TXA use in this population. In a review of 896 combat casualties treated at Bastion over this time frame, 32.7% (N=293) received TXA (mean ± SD dose: 2.3 ± 1.3g) while 67.2% (N=603) did not receive TXA. In the overall cohort, the TXA group was more severely injured (ISS: 25.2±16.6 vs. 22.5±18.5; p<0.001), required more blood (11.8±12.1 vs. 9.8±13.1 pRBC units; p<0.001), and had a lower Glasgow Coma Score (7.3±5.5 vs. 10.5±5.5; p<0.001) and initial systolic blood pressure (112±29.1 vs. 122.5±30.3 mmHg), but also had a lower unadjusted mortality than the no-TXA group (17.4% vs. 23.9%; p=0.028). In the massive transfusion cohort (N=321; 24 hour transfusion: 21.9±14.7 pRBC; 19.1±13.3 FFP and 3.5±3.2 apheresis platelet units), mortality was also lower in the TXA (mean ± SD dose: 2.4 ± 1.4g) compared to the no-TXA group (14.4% vs. 28.1%; p=0.004). In a multivariate regression model, TXA use in the massive transfusion cohort was independently associated with survival (odds ratio: 7.28; 95% confidence interval: 3.02-17.32. For all patients requiring at least one unit of blood after combat injury, patients receiving TXA had higher rates of DVT (2.4% vs. 0.2%, p = 0.001) and PE (2.7% vs. 0.3%, p =0.001), but were also more likely to have injury patterns associated with higher risk of thromboembolic events ; including higher mean ISS (25 vs 23, p < 0.001), more severe extremity injuries (extremity AIS >=3 66.6% in TXA group, 47.3% non-TXA, p < 0.001), and more commonly GCS < or = 8 (63.3% vs. 35.6%, p < 0.001). These survival benefit findings associated with TXA use support the hypothesis that the use of this adjunct, in conjunction with component-based resuscitation following combat injury, is associated with improved survival. This association is most prominent in those requiring massive transfusion.
----------------
Exacyl 1g IV au mieux dans l'heure et pas après 3 heures après la blessure

Les commentaires sont fermés.