14/06/2017
Albumine préhospitalière: Idée qui fait son chemin
Albumin for Prehospital Fluid Resuscitation of Hemorrhagic Shock in Tactical Combat Casualty Care
----------------------------------------
Une publication récente de Kheirabadi BS et Al. (1) évoque l'intérêt potentiel de l'albumine concentrée, notammment son pouvoir tampon important, pour la prise en charge de l'hémorragie, usage qu'il ne faut pas confondre avec celui de l'albumine à 4% dont l'emploi reste controversé (2) après l'étude SAFE (3). Lire ce point (5)
----------------------------------------
Optimal fluid resuscitation on the battlefield in the absence of blood products remains unclear. Contemporary Combat medics are generally limited to hydroxyethyl starch or crystalloid solutions, both of which present significant drawbacks. Obtaining US Food and Drug Administration (FDA)-approved freeze-dried plasma (FDP) is a top casualty care research priority for the US Military. Interest in this agent reflects a desire to simultaneously expand intravascular volume and address coagulopathy. The history of FDP dates to the Second World War, when American expeditionary forces used this agent frequently. Also fielded was 25% albumin, an agent that lacks coagulation factors but offers impressive volume expansion with minimal weight to carry and requires no reconstitution in the field. The current potential value of 25% albumin is largely overlooked. Although FDP presents an attractive future option for battlefield prehospital fluid resuscitation once FDA approved, this article argues that in the interim, 25% albumin, augmented with fibrinogen concentrate and tranexamic acid to mitigate hemodilution effects on coagulation capacity, offers an effective volume resuscitation alternative that could save lives on the battlefield
| Tags : hémorragie
05/05/2017
Fractions coagulantes: Mieux que PFC ?
Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial.
-------------------------------------------------
Un travail dont les conclusions sont très claires. La prise en charge de la coagulopathie traumatique bénéficie bien plus d'une stratégie d'apports ciblés de fractions coagulantes concentrées, notamment de fibrinogène ici 50 mg/kg, qu'une stratégie classique basée sur l'apport de PFC.
-------------------------------------------------
Background
Effective treatment of trauma-induced coagulopathy is important; however, the optimal therapy is still not known. We aimed to compare the efficacy of first-line therapy using fresh frozen plasma (FFP) or coagulation factor concentrates (CFC) for the reversal of trauma-induced coagulopathy, the arising transfusion requirements, and consequently the development of multiple organ failure.
Methods
This single-centre, parallel-group, open-label, randomised trial was done at the Level 1 Trauma Center in Innsbruck Medical University Hospital (Innsbruck, Austria). Patients with trauma aged 18–80 years, with an Injury Severity Score (ISS) greater than 15, bleeding signs, and plasmatic coagulopathy identified by abnormal fibrin polymerisation or prolonged coagulation time using rotational thromboelastometry (ROTEM) were eligible. Patients with injuries that were judged incompatible with survival, cardiopulmonary resuscitation on the scene, isolated brain injury, burn injury, avalanche injury, or prehospital coagulation therapy other than tranexamic acid were excluded. We used a computer-generated randomisation list, stratification for brain injury and ISS, and closed opaque envelopes to randomly allocate patients to treatment with FFP (15 mL/kg of bodyweight) or CFC (primarily fibrinogen concentrate [50 mg/kg of bodyweight]). Bleeding management began immediately after randomisation and continued until 24 h after admission to the intensive care unit. The primary clinical endpoint was multiple organ failure in the modified intention-to-treat population (excluding patients who discontinued treatment). Reversal of coagulopathy and need for massive transfusions were important secondary efficacy endpoints that were the reason for deciding the continuation or termination of the trial. This trial is registered with ClinicalTrials.gov, number NCT01545635.
Findings
Between March 3, 2012, and Feb 20, 2016, 100 out of 292 screened patients were included and randomly allocated to FFP (n=48) and CFC (n=52). Six patients (four in the FFP group and two in the CFC group) discontinued treatment because of overlooked exclusion criteria or a major protocol deviation with loss of follow-up. 44 patients in the FFP group and 50 patients in the CFC group were included in the final interim analysis. The study was terminated early for futility and safety reasons because of the high proportion of patients in the FFP group who required rescue therapy compared with those in the CFC group (23 [52%] in the FFP group vs two [4%] in the CFC group; odds ratio [OR] 25·34 [95% CI 5·47–240·03], p<0·0001) and increased needed for massive transfusion (13 [30%] in the FFP group vs six [12%] in the CFC group; OR 3·04 [0·95–10·87], p=0·042) in the FFP group. Multiple organ failure occurred in 29 (66%) patients in the FFP group and in 25 (50%) patients in the CFC group (OR 1·92 [95% CI 0·78–4·86], p=0·15).
Interpretation
Our results underline the importance of early and effective fibrinogen supplementation for severe clotting failure in multiple trauma. The available sample size in our study appears sufficient to make some conclusions that first-line CFC is superior to FFP.
| Tags : coagulopathie
02/02/2017
Coagulopathie: Une affaire personnelle
Individual clotting factor contributions to mortality following trauma.
-------------------------------
Un travail intéressant qui portant sur 1463 traumatisés d'ISS médian de 16 et qui met en avant l'existence de deux profils de coagulopathie traumatique (16% des patients pris en charge). Dans 49,30 des cas, un premier est en rapport avec des anomalies des facteurs II,VII,IX,X et protéine C . Le second profil (17% des patients) exprime des anomalies sur les facteurs V et VIII. Seuls seraient liés à une motralité à 28j. LA déplétion en facteur V serait associée à une mortalité à long terme. Ce travail milite pour une approche personnalisée de la ocaguklopathie traumatique.
-------------------------------
BACKGROUND:
Acute traumatic coagulopathy affects 20% to 30% of trauma patients, but the extensive collinearity of the coagulation cascade complicates attempts to clarify global clotting factor dysfunction. This study aimed to characterize phenotypes of clotting factor dysfunction and their contributions to mortality after major trauma.
METHODS:
This prospective cohort study examines all adult trauma patients of the highest activation level presenting to San Francisco General Hospital between February 2005 and February 2015. Factors II, V, VII, VIII, IX, and X and protein C activity on admission and mortality status at 28 days were assessed. Predictors of 28-day mortality in univariate analysis were included in multiple logistic regression controlling for traumatic brain injury (TBI), acidosis, age, and mechanism of injury. Principal component analysis was utilized to identify phenotypic coagulation.
RESULTS:
Complete coagulation factor data were available for 876 (61%) of 1,429 patients. In multiple logistic regression, factors V (odds ratio [OR], 0.86; 95% confidence interval [CI], 0.76-0.97), VIII (OR, 0.97; 95% CI, 0.95-0.99), and X (OR, 0.79; 95% CI, 0.68-0.92) and protein C (OR, 1.17; 95% CI, 1.05-1.30) significantly predicted 28-day mortality after controlling for age, base deficit, mechanism of injury, and TBI. Principal component analysis identified two significant principal components (Phenotypes 1 and 2) that accounted for 66.3% of the total variance. Phenotype 1 (factors II, VII, IX, and X and protein C abnormalities) explained 49.3% and was associated with increased injury, coagulopathy, TBI, and mortality. Phenotype 2 (factors V and VIII abnormalities) explained 17.0% and was associated with increased coagulopathy, blunt injury, and mortality. Only Phenotype 2 remained significantly associated with 28-day mortality in multiple logistic regression.
CONCLUSIONS:
Principal component analysis identified two distinct phenotypes within the entirety of global clotting factor abnormalities, and these findings substantiate the crucial association of factors V and VIII on mortality following trauma. This may be the first step toward identifying unique phenotypes after injury and personalizing hemostatic resuscitation.
| Tags : hémorragie, coagulopathie
22/01/2017
Du sang qui descend du ciel
Nous ne sommes pas les seuls à avoir à faire face au contexte d'isolement. Il est particulièrement intéressant de regarder comment ces problèmes sont abordés par les pays en voie de construction. L'exemple rwandais devrait nous interpeller. Le recours à des drones de livraison en contexte militaire n'est pas une utopie car ce mode de ravitaillement a été utilisé en afghanistan.
| Tags : transfusion
21/01/2017
Coagulopathie: Fibrinogène avant PLyo, mais les 2 et + tôt ?
Despite the early uses of tourniquets and haemostatic dressings, blood loss still accounts for the vast majority of preventable deaths on the battlefield. Over the last few years, progress has been made in the management of such injuries, especially with the use of damage control resuscitation concepts. The early application of these procedures, on the field, may constitute the best opportunity to improve survival from combat injury during remote operations.
DATA SOURCES:
Currently available literature relating to trauma-induced coagulopathy treatment and far-forward transfusion was identified by searches of electronic databases. The level of evidence and methodology of the research were reviewed for each article. The appropriateness for field utilisation of each medication was then discussed to take into account the characteristics of remote military operations.
CONCLUSIONS:
In tactical situations, in association with haemostatic procedures (tourniquet, suture, etc), tranexamic acid should be the first medication used according to the current guidelines. The use of fibrinogen concentrate should also be considered for patients in haemorrhagic shock, especially if point-of-care (POC) testing of haemostasis or shock severity is available. If POC evaluation is not available, it seems reasonable to still administer this treatment after clinical assessment, particularly if the evacuation is delayed. In this situation, lyophilised plasma may also be given as a resuscitation fluid while respecting permissive hypotension. Whole blood transfusion in the field deserves special attention.
In addition to the aforementioned treatments, if the field care is prolonged, whole blood transfusion must be considered if it does not delay the evacuation
| Tags : coagulopathie, transfusion
08/01/2017
Albumine: Bon pour la coagulopathie ?
Does small-volume resuscitation with crystalloids or colloids influence hemostasis and survival of rabbits subjected to lethal uncontrolled hemorrhage?
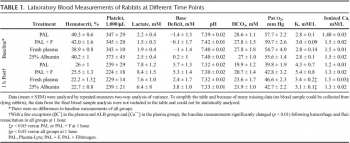
BACKGROUND:
Prehospital, small-volume resuscitation of combat casualties with a synthetic colloid (6% hydroxyethyl starch [HES] 670/0.75) has been recommended when blood or blood components are unavailable. We studied hemostatic effects of a newer synthetic colloid (6% HES, 130/0.4) compared with either a natural colloid (albumin) or to crystalloids in an uncontrolled hemorrhage model.
METHODS:
Spontaneously breathing New Zealand white rabbits (3.4 ± 0.1 kg) were anesthetized, instrumented, and subjected to a splenic injury with uncontrolled bleeding. Fifteen minutes after injury, rabbits were in shock (mean arterial pressure [MAP] = 26 ± 1.3 mm Hg, and received colloids (6% HES, 130/0.4 or 5% albumin at 15 mL/kg), or crystalloids (normal saline at 30 mL/kg or 5% hypertonic saline at 7.5 mL/kg) for resuscitation in two intravenous bolus injections (15 minutes apart) to raise their MAP to 65 mm Hg, n = 9/group. Animals were monitored for 2.5 hours or until death, and blood losses were measured. Blood samples were analyzed for arterial blood gas, complete blood count, and coagulation measures.
RESULTS:
There were no differences among groups in baseline measures and initial hemorrhage volume (11.9 ± 0.6 mL/kg) at 15 minutes postinjury. Twenty minutes after fluid resuscitation (1 hour postinjury), MAP was higher, shock indices were lower, and blood pH was higher in colloids versus crystalloids groups (p < 0.05). Administration of 6% HES 130/0.4 colloid produced the largest hemodilution (54% decrease in hematocrit, p < 0.05 vs. hypertonic saline). Activated partial thromboplastin time increased approximately 35% above baseline in all groups except in 6% HES 130/0.4 group in which it doubled. Clot strength was reduced (15%) only in the 6% HES 130/0.4 group. 6% HES 130/0.4 resuscitation produced the largest blood loss and 33% survival rate that was not different than the crystalloid groups. Albumin produced the best hemostatic and survival outcomes (78%).
CONCLUSION:
Small-volume resuscitation with crystalloids appeared inadequate to treat hypovolemic shock and prevent death. 6% HES 130/0.4 was effective hemodynamically but detrimental to hemostasis. Albumin produced the best outcomes consistent with our previous observations. Further studies are needed to prove benefit of albumin solution as a possible resuscitation fluid for treating combat casualties at the point of injury.
Synopsis of the updated European trauma guideline
Management of trauma-induced coagulopathy (TIC): a synopsis of the updated European trauma guideline
Maegele M. J Res Hosp 2016;1:27
Uncontrolled hemorrhage and trauma-induced coagulopathy (TIC) are still the major causes for preventable death after trauma .
Approximately one out of four severely injured trauma patients admitted to the hospital is bleeding with variable degrees of laboratory coagulopathy. Meanwhile, TIC is recognized as an own clinical entity with substantial impact on outcome and survival after trauma. There has been speculation about the potential mechanisms underlying TIC but much of the data continues to be rather correlative than causative with robust links still lacking.
02/01/2017
Plyo: En intraosseux aussi
Pre-hospital intra-osseous freeze dried plasma transfusion: a case report
Rottenstreich et al. Disaster and Military Medicine 2015, 1:8
Background: Hemorrhage and coagulopathy are among the leading causes of death in combat and are considered the leading causes of preventable deaths. Plasma, in the form of Fresh Frozen Plasma (FFP) is considered a key component in the Damage Control Resuscitation performed within hospitals. Freeze-Dried Plasma (FDP) can be stored at room temperature and therefore is potentially useful in pre-hospital conditions. Our case report join to few cases where FDP was administered at the point of injury. It is also unique as it describes an intra- osseous administration given to pediatric patient.
Case report: M.S. otherwise healthy 13 year old girl was injured due to gunshots and grenade blast. On the first triage by the IDF medical teams she suffered from: Severe hemorrhagic shock, (Blood pressure could not be measured, Heart rate 163), superficial wounds to her face, (forehead and Rt. Eye), gunshot wounds with active bleeding from her Lt. Arm and her RT. Knee (Mangled Extremity Severity Score (MESS) 8) and open fractures of left elbow and right thigh. A peripheral intravenous catheter was established and 1 g tranexamic acid in 500 ml of Hartman fluid were administered. Due to difficulties in establishing a functioning intra-venous line, an intra-osseous catheter was established and one unit of FDP (250 ml) was given in the field. She was transferred by a military medical team to a regional civilian hospital for further treatment. Upon arrival to the hospital her blood pressure and heart rate were significantly improved. After three weeks of hospitalization M.S. was discharged and she was returned to her homeland.
Conclusion: We have described the successful use of FDP for pre hospital resuscitation of a 13 year old girl suffering from severe hemorrhagic shock as a result of gunshots and grenade blast. This case report demonstrates that intra-osseous FDP administration for as part pre hospital resuscitation of children has a favorable outcome.
| Tags : intraosseux
Coagulopathy/ Eléments de compréhension
Advances in the understanding of trauma-induced coagulopathy
Chang R. et al Blood. 2016;128(8):1043-1049
Ten percent of deaths worldwide are due to trauma, and it is the third most common cause of death in the United States. Despite a profound upregulation in procoagulant mechanisms, one-quarter of trauma patients present with laboratorybased evidence of trauma-induced coagulopathy (TIC), which is associated with poorer outcomes including increased mortality. The most common causes of death after trauma are hemorrhage and traumatic brain injury (TBI). The management of TIC has significant implications in both because many hemorrhagic deaths could be preventable, and TIC is associated with progression of intracranial injury after TBI. This review covers the most recent evidence and advances in our understanding of TIC, including the role of platelet dysfunction, endothelial activation, and fibrinolysis. Trauma induces a plethora of biochemical and physiologic changes, and despite numerous studies reporting differences in coagulation parameters between trauma patients and uninjured controls, it is unclear whether some of these differences may be “normal” after trauma. Comparisons between trauma patients with differing outcomes and use of animal studies have shed some light on this issue, but much of the data continue to be correlative with causative links lacking. In particular, there are little data linking the laboratory-based abnormalities with true clinically evident coagulopathic bleeding. For these reasons, TIC continues to be a significant diagnostic and therapeutic challenge.
| Tags : coagulopathie
19/12/2016
The 2015 Remote Damage Control Resuscitation Symposium
18/12/2016
Coagulopathie traumatique. Données actuelles
Acute traumatic coagulopathy: pathophysiology and resuscitation.
Acute Traumatic Coagulopathy occurs immediately after massive trauma when shock, hypoperfusion, and vascular damage are present. Mechanisms for this acute coagulopathy include activation of protein C, endothelial glycocalyx disruption, depletion of fibrinogen, and platelet dysfunction. Hypothermia and acidaemia amplify the endogenous coagulopathy and often accompany trauma. These multifactorial processes lead to decreased clot strength, autoheparinization, and hyperfibrinolysis. Furthermore, the effects of aggressive crystalloid administration, haemodilution from inappropriate blood product transfusion, and prolonged surgical times may worsen clinical outcomes. We review normal coagulation using the cell-based model of haemostasis and the pathophysiology of acute traumatic coagulopathy. Developed trauma systems reduce mortality, highlighting critical goals for the trauma patient in different phases of care. Once patients reach a trauma hospital, certain triggers reliably indicate when they require massive transfusion and specialized trauma care. These triggers include base deficit, international normalized radio (INR), systolic arterial pressure, haemoglobin concentration, and temperature. Early identification for massive transfusion is critically important, as exsanguination in the first few hours of trauma is a leading cause of death. To combat derangements caused by massive haemorrhage, damage control resuscitation is a technique that addresses each antagonist to normal haemostasis. Components of damage control resuscitation include damage control surgery, permissive hypotension, limited crystalloid administration, haemostatic resuscitation, and correction of hyperfibrinolysis.
Fibrinogène dès que l'Hb baisse ?
Estimation of plasma fibrinogen levels based on hemoglobin, base excess and Injury Severity Score upon emergency room admission
----------------------
Il existe un grand débat sur la manière de prendre en charge la coagulopathie traumatique des traumatisés ballistiques en contexte d'isolement (1,2).Un des sujets porte sur la manière de corriger l'hypofibrinogénémie soit par apport de Plasma soit par apport de concentrés de fibrinogène (3, 4). Le consensus européen valide les deux approches (5). Mais dans notre contexte d'intervention quels critères d'administration appliquer ? L'hémoglobinémie à la prise en charge permettrait d'indiquer l'apport de fibrinogène, en gros dès qu'elle est abaissée et surtout <10g/dl. C'est ce que peut laisser penser cette étude. Des moyens simples utilisables en contexte d'isolement permettent donc de stratifier les indications de fibrinogène apporté soit sous forme concentré soit sous forme de plasma (6).
----------------------
INTRODUCTION:
Fibrinogen plays a key role in hemostasis and is the first coagulation factor to reach critical levels in massively bleeding trauma patients. Consequently, rapid estimation of plasma fibrinogen (FIB) is essential upon emergency room (ER) admission, but is not part of routine coagulation monitoring in many centers. We investigated the predictive ability of the laboratory parameters hemoglobin (Hb) and base excess (BE) upon admission, as well as the Injury Severity Score (ISS), to estimate FIB in major trauma patients.
METHODS:
In this retrospective study, major trauma patients (ISS ≥16) with documented FIB analysis upon ER admission were eligible for inclusion. FIB was correlated with Hb, BE and ISS, alone and in combination, using regression analysis.
RESULTS:
A total of 675 patients were enrolled (median ISS 27). FIB upon admission correlated strongly with Hb, BE and ISS.
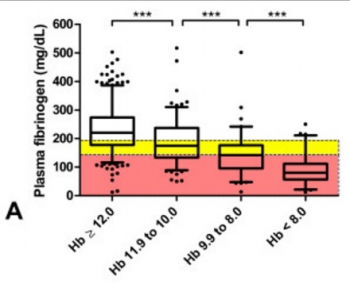
Multiple regression analysis showed that Hb and BE together predicted FIB (adjusted R2 = 0.46; loge(FIB) = 3.567 + 0.223.Hb - 0.007.Hb2 + 0.044.BE), and predictive strength increased when ISS was included (adjusted R2 = 0.51; loge(FIB) = 4.188 + 0.243.Hb - 0.008.Hb2 + 0.036.BE - 0.031.ISS + 0.0003.ISS2). Of all major trauma patients admitted with Hb <12 g/dL, 74% had low (<200 mg/dL) FIB and 54% had critical (<150 mg/dL) FIB. Of patients admitted with Hb <10 g/dL, 89% had low FIB and 73% had critical FIB. These values increased to 93% and 89%, respectively, among patients with an admission Hb <8 g/dL. Sixty-six percent of patients with only a weakly negative BE (<-2 mmol/L) showed low FIB. Of patients with BE <-6 mmol/L upon admission, 81% had low FIB and 63% had critical FIB. The corresponding values for BE <-10 mmol/L were 89% and 78%, respectively.
CONCLUSIONS:
Upon ER admission, FIB of major trauma patients shows strong correlation with rapidly obtainable, routine laboratory parameters such as Hb and BE. These two parameters might provide an insightful and rapid tool to identify major trauma patients at risk of acquired hypofibrinogenemia. Early calculation of ISS could further increase the ability to predict FIB in these patients. We propose that FIB can be estimated during the initial phase of trauma care based on bedside tests.
14/12/2016
Fibrinogène: Moins de décès
Pre-emptive administration of fibrinogen concentrate contributes to improved prognosis in patients with severe trauma
Yamamoto K, et al. Trauma Surg Acute Care Open 2016;1:1–5
---------------------------------------------------------
Bien que cela reste encore discuté, l'apport précoce de fibrinogène améliorerait la survie des traumatisés sévères. Cette publication est du moins en faveur de cette hypothèse.
---------------------------------------------------------
Background
Patients with severe trauma often present with critical coagulopathy, resulting in impaired hemostasis, massive hemorrhage, and a poor survival prognosis. The efficacy of hemostatic resuscitation in correcting coagulopathy and restoring tissue perfusion has not been studied. We assessed a novel approach of pre-emptive administration of fibrinogen concentrate to improve critical coagulopathy in patients with severe trauma.
Methods
We retrospectively compared blood transfusion volumes and survival prognosis between three groups of patients with trauma, with an Injury Severity Score (ISS) ≥26 over three consecutive periods: group A, no administration of fibrinogen concentrate; group B, administration of 3 g of fibrinogen concentrate after evaluation of trauma severity and a plasma fibrinogen level <1.5 g/L; group C, pre-emptive administration of 3 g of fibrinogen concentrate immediately on patient arrival based on prehospital information, including high-severity injury or assessed
need for massive transfusion before measurement of fibrinogen.
Results
∼56% of patients with an ISS ≥26 and transfused with red blood cell concentrates ≥10 units, had hypofibrinogenemia (fibrinogen <1.5 g/L) on arrival. Patients who received fibrinogen concentrate in group C showed significantly higher fibrinogen levels after treatment with this agent than those in group B (2.41 g/L vs 1.88 g/L; p=0.01). Although no significant difference was observed in blood transfusion volumes between the groups, the 30-day survival of patients in group C (all, and those with an ISS ≥26) was significantly better than in group A ( p<0.05). The 48-hour mortality rate in patients with an ISS ≥26 was significantly lower in group C than in group A (8.6% vs 22.9%; p=0.005). Further, among patients with an ISS ≥41, the overall mortality was significantly lower in group C than in group A (20% vs 50%; p=0.02).
Conclusion
Pre-emptive administration of fibrinogen concentrate for patients with trauma with critical coagulopathy may contribute to improved survival.
| Tags : coagulopathie
11/12/2016
NaCl 7,5% ? A voir mais sans Colloïdes.
Pre-Hospital Resuscitation of Traumatic Hemorrhagic Shock with Hypertonic Solutions Worsen Hypo-Coagulation and Hyper-Fibrinolysis
Delano M. et Al. Shock. 2015 Jul;44(1):25-31
-----------------------------------------------
Le choix d'un liquide de remplissage vasculaire n'est pas simple. Au delà des contraintes d'efficacité en termes de remplissage vasculaire, de bonne tolérance notamment rénale il y a également les effets de ce dernier sur la coagulation. On sait qu'une partie importante des blessés actuellement pris en charge présentent une coagulopathie traumatique (1). Le NaCl 7.5% est le soluté recommandé par la procédure du sauvetage au combat (2) car il représente le meilleur compromis intérêt médical/logistique. Le travail ici présenté met en évidence les effets délétères des solutés hypertoniques sur la coagulation. Ce document mérite cependant d'être pondéré car il s'appuie sur une petite cohorte de patients de traumatologie civile, que le profil du remplissage vasculaire préhospitalier n'est pas clairement rapporté hormis le premier liquide, qu'il ne précise pas le niveau de calcémie plasmatique car ce dernier peut être affecté selon la nature des solutés utilisés (4), que le groupe HS a des marqueurs d'hypoperfusion tissulaire identique au groupe NS, que la comparaison se fait avec un groupe de sujets sains et non entre les groupes. Par ailleurs on sait également qu'il est mis en avant l'intérêt des solutions HS en matière de prise en charge des HTIC des plaies cranio-cérébrales (4) et la réduction de l'activation des polynucléaires neutrophiles (5). Donc il ne s'agit pas de remettre en question le choix actuel, mais de le repositionner dans le débat notamment avec l'emploi du Plama lyophylisé comme soluté de remplissage premier des blessés les plus graves (6). Une chose apparait certaine: Ne plus utiliser une association HS/Dextran type RescueFlow (7).
-----------------------------------------------
Impaired hemostasis frequently occurs after traumatic shock and resuscitation. The prehospital fluid administered can exacerbate subsequent bleeding and coagulopathy. Hypertonic solutions are recommended as first-line treatment of traumatic shock; however, their effects on coagulation are unclear. This study explores the impact of resuscitation with various hypertonic solutions on early coagulopathy after trauma. We conducted a prospective observational subgroup analysis of large clinical trial on out-of-hospital single-bolus (250 mL) hypertonic fluid resuscitation of hemorrhagic shock trauma patients (systolic blood pressure, e70 mmHg). Patients received 7.5% NaCl (HS), 7.5% NaCl/6% Dextran 70 (HSD), or 0.9% NaCl (normal saline [NS]) in the prehospital setting. Thirty-four patients were included: 9 HS, 8 HSD, 17 NS. Treatment with HS/HSD led to higher admission systolic blood pressure, sodium, chloride, and osmolarity, whereas lactate, base deficit, fluid requirement, and hemoglobin levels were similar in all groups. The HSD-resuscitated patients had higher admission international normalized ratio values and more hypocoagulable patients, 62% (vs. 55% HS, 47% NS; P G 0.05). Prothrombotic tissue factor was elevated in shock treated with NS but depressed in both HS and HSD groups. Fibrinolytic tissue plasminogen activator and antiYfibrinolytic plasminogen activator inhibitor type 1 were increased by shock but not thrombin-activatable fibrinolysis inhibitor. The HSD patients had the worst imbalance between procoagulation/anticoagulation and profibrinolysis/antifibrinolysis, resulting in more hypocoagulability and hyperfibrinolysis. We concluded that resuscitation with hypertonic solutions, particularly HSD, worsens hypocoagulability and hyperfibrinolysis after hemorrhagic shock in trauma through imbalances in both procoagulants and anticoagulants and both profibrinolytic and antifibrinolytic activities
24/09/2016
Transfusion en vol: Sécurité assurée
Risk Management Analysis of Air Ambulance Blood Product Administration in Combat Operations
BACKGROUND:
Between June-October 2012, 61 flight-medic-directed transfusions took place aboard U.S. Army Medical Evacuation (medevac) helicopters in Afghanistan. This represents the initial experience for pre-hospital blood product transfusion by U.S. Army flight medics.
METHODS:
We performed a retrospective review of clinical records, operating guidelines, after-action reviews, decision and information briefs, bimonthly medical conferences, and medevac-related medical records.
RESULTS:
A successful program was administered at 10 locations across Afghanistan. Adherence to protocol transfusion indications was 97%. There were 61 casualties who were transfused without any known instance of adverse reaction or local blood product wastage. Shock index (heart rate/systolic blood pressure) improved significantly en route, with a median shock index of 1.6 (IQR 1.2-2.0) pre-transfusion and 1.1 (IQR 1.0-1.5) post-transfusion (P < 0.0001). Blood resupply, training, and clinical procedures were standardized across each of the 10 areas of medevacoperations.
DISCUSSION:
Potential risks of medical complications, reverse propaganda, adherence to protocol, and diversion and/or wastage of limited resources were important considerations in the development of the pilot program. Aviation-specific risk mitigation strategies were important to ensure mission success in terms of wastage prevention, standardized operations at multiple locations, and prevention of adverse clinical outcomes. Consideration of aviation risk mitigation strategies may help enable other helicopter emergency medical systems to develop remote pre-hospital transfusion capability. This pilot program provides preliminary evidence that blood product administration by medevac is safe.
| Tags : transfusion
11/08/2016
Transfusion, Thrombosis and Bleeding Management
Special Issue: Transfusion, Thrombosis and Bleeding Management
January 2015 - Volume 70, Issue Supplement s1 - Pages 1–e41
Clic sur l'image pour accéder au numéro en ligne
Blood – the most important humour? (pages 1–e1)
C. R. Bailey, A. A. Klein and B. J. Hunt
Version of Record online: 1 DEC 2014 | DOI: 10.1111/anae.12930
Review Articles
L. Green, S. Allard and R. Cardigan
☛ CPD available at http://www.learnataagbi.org
Corrected by:
Corrigendum: Modern banking, collection, compatibility testing and storage of blood and blood components
Vol. 70, Issue 3, 373, Version of Record online: 11 FEB 2015
Evidence and triggers for the transfusion of blood and blood products (pages 10–e3)
A. Shah, S. J. Stanworth and S. McKechnie
Pre-operative anaemia (pages 20–e8)
B. Clevenger and T. Richards
The pathophysiology and consequences of red blood cell storage (pages 29–e12)
D. Orlov and K. Karkouti
Red cell transfusion and the immune system (pages 38–e16)
S. Hart, C. M. Cserti-Gazdewich and S. A. McCluskey
The current place of aprotinin in the management of bleeding (pages 46–e17)
D. Royston
The current place of tranexamic acid in the management of bleeding (pages 50–e18)
B. J. Hunt
Practical management of major blood loss (pages 54–e20)
R. Gill
Management of peri-operative anti-thrombotic therapy (pages 58–e23)
J. J. van Veen and M. Makris
Laboratory monitoring of haemostasis (pages 68–e24)
A. Fowler and D. J. Perry
Point-of-care monitoring of haemostasis (pages 73–e26)
S. V. Mallett and M. Armstrong
Haemostatic management of obstetric haemorrhage (pages 78–e28)
R. E. Collis and P. W. Collins
Haemostatic management of cardiac surgical haemorrhage (pages 87–e31)
M. W. Besser, E. Ortmann and A. A. Klein
The pathogenesis of traumatic coagulopathy (pages 96–e34)
A. Cap and B. J. Hunt
Management of traumatic haemorrhage – the European perspective (pages 102–e37)
H. Schöchl, W. Voelckel and C. J. Schlimp
Management of traumatic haemorrhage – the US perspective (pages 108–e38)
R. P. Dutton
Surgery in patients with inherited bleeding disorders (pages 112–e40)
P. K. Mensah and R. Gooding
The management of abnormal haemostasis in the ICU (pages 121–e41)
A. Retter and N. A. Barrett
27/06/2016
Albumine 20% plutôt que fibrinogène ?
Influences of limited resuscitation with plasma or plasma protein solutions on hemostasis and survival of rabbits with noncompressible hemorrhage
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2016;81: 42–49
--------------------------------
Dans ce travail et alors que l'albumine diluée n'est pas recommandée, les auteurs évoquent la possibilité que les effets favorables d'une réanimation basée sur l'apport de plasma serait lié à l'apport de protéine et en particulier d'albumine qui aurait un effet tampon élevé, réduisant l'acidose métabolique, un des facteurs de la triade létale.
--------------------------------
BACKGROUND:
Plasma infusion with or without red blood cells is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
Anesthetized spontaneously breathing rabbits (3.3 ± 0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 minutes with Plasma-Lyte (PAL; 30 mL/kg), PAL + fibrinogen (PAL + F; 30 mL + 100 mg/kg), fresh rabbit plasma (15 mL/kg), or 25% albumin (ALB; 5 mL/kg) solution, all given in two bolus intravenous injections (15 minutes apart) to achieve a mean arterial pressure of 65 mm Hg, n = 8 to 9/group. Animals were monitored for 2 hours or until death, and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 minutes. At 60 minutes after injury, mean arterial pressure was higher with ALB than with crystalloids (PAL or PAL + F), but shock indices were not different despite the large differences in resuscitation volumes. Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein and increased survival rate to 100% (p < .05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSIONS:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate; however, its effects did not differ from those obtained with 25% ALB at one-third of the volume. The ALB advantage was consistent with our previous findings in which 5% ALB was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its ALB content rather than its coagulation proteins
| Tags : coagulopathie, remplissage
04/06/2016
PLyo: Une révolution ? Pas vraiment, une redécouverte
Pusateri AE et Al. Transfusion. 2016 Apr;56 Suppl 2:S128-39
------------------------------------------
Les nouvelles modalités de transfusion mettent en avant le bénéfice de l'apport précoce de plasma. Les contraintes logistiques liées à l'emploi de plasma frais sont réelles. L'emploi de plasma lyophilisé permet de raccourcir ce délai et peut représenter dans certaines conditions d'isolement la seule source disponibles de fractions coagulantes. Le plasma lyophylisé est un vieux monsieur, mais dont la place est fondamentale. Largement utilisé notamment par l'armée française pendant la guerre d'indocchine, le SSA a maintenu sa production jusqu'à ce que l'épidémie de VIH ne survienne. Depuis les années 1980, le SSA a travaillé sans relâche pour sécuriser un produit qui retrouve la place qui lui est due dans la stratégie transfusionnelle du blessé de guerre (1) Il s'agit donc d'une redécouverte avec un emploi effectif en opération dès 1996 (2), plutôt que de révolution. Le document proposé à la lecture fait le point sur cette historique et les développements à venir. La lecture de ce document ne doit pas faire oublier la réflexion de plus en plus présente sur l'emploi en situation d'isolement de l'intérêt de la transfusion de sang total, seule source de plaquettes, associé au recours à des fractions coagulantes comme le fibrinogène et les complexes prothrombiques. Une telle association représente probablement l'avenir de la réanimation hémostatique préhospitalière (3, 4).
------------------------------------------
Historical dried plasma development Event Selected References
1930s Plasma lyophilization developed in the 1930s.
1940—Large scale production of pooled, lyophilized plasma by both the US and British established for war time use (to meet logistical constraints of whole blood and frozen/liquid plasma).ans les années
1941—Spray dried plasma produced for the Swedish Defense Department. 21 WWII Production 20-22 British produced >500,000 U lyophilized plasma during WWII. US produced >6,000,000 U lyophilized plasma during WWII. US/British distributed world-wide. Sweden produced approximately 17,000 U spray dried plasma for Sweden and Finland.
1945—Hepatitis 23 Hepatitis as a result of plasma transfusion recognized by the end of WWII. Believed that benefits outweighed the risk.
1945-1952—Hepatitis 24 Attempts at pathogen reduction and reducing pool size not successful. Several deaths in clinical studies of ultraviolet irradiated pooled plasma.
1953
—Department of the Army (Circular 73) directed that, because of the risk of serum hepatitis, the higher cost, and the need to use it for the production of specific globulins, plasma would not be used “to support blood volume” unless dextran was not available.
—Serum albumin replaced plasma as primary resuscitative product for US Forces in Korea.
1968—National Research Council Committee on Plasma and Plasma Substitutes recommended that “the use of whole, pooled human plasma be discouraged and even discontinued unless a clear cut case can be made for its unique requirements.”
The French Military Blood Institute produced dried plasma from 1949 to 1984, and provided over 40,000 units to French military forces during the Indochina War. In 1985, production was discontinued due to risk of HIV infection.
| Tags : coagulopathie, transfusion
Acide tranexaminique systématique: La roue tournerait-elle ?
Acute Fibrinolysis Shutdown after Injury Occurs Frequently and Increases Mortality: A Multicenter Evaluation of 2,540 Severely Injured Patients
Moore HB et Al. J Am Coll Surg. 2016 Apr;222(4):347-55.
------------------------------------------------------
La recommandation n°15 de la RFE Portant sur la réanimation du choc hémorragique stipule qu' il est recommandé d'administrer de l'acide tranexamique dès que possible chez les patients traumatisés à la dose de 1 g en bolus intraveineux en 10 min suivi de 1 g perfusé sur 8 h chez les patients traumatisés. Cette administration ne doit pas être initiée au delà de la 3e heure suivant la survenue d'un traumatisme avec choc hémorragique. Si l'étude CRASH-2 a montré que l'acide tranexamique réduisait significativement la mortalité. De nouvelles données disponibles depuis alimentent la discussion (1). Trois états du système de fibrinolyse peuvent être retrouvés: normal, hyperfibrinolyse, inhibition Les deux derniers sont associés à une surmortalité mais la fréquence des états d'inhibition de l'inhibition ne plaiderait pas pour une administration systématique mais ciblée d'exacyl. En qui nous concerne il faut à nouveau insister sur la précocité de l'administration d'exacyl dans l'heure chez les blessés sévères, pour lesquels le bénéfice en terme de mortalité est le plus grand (2). Une réflexion pour un emploi optimisé est en MARCHE (3, 4)
------------------------------------------------------
BACKGROUND:
Fibrinolysis is a physiologic process that maintains microvascular patency by breaking down excessive fibrin clot. Hyperfibrinolysis is associated with a doubling of mortality. Fibrinolysis shutdown, an acute impairment of fibrinolysis, has been recognized as a risk factor for increased mortality. The purpose of this study was to assess the incidence and outcomes of fibrinolysis phenotypes in 2 urban trauma centers.
STUDY DESIGN:
Injured patients included in the analysis were admitted between 2010 and 2013, were 18 years of age or older, and had an Injury Severity Score (ISS) > 15. Admission fibrinolysis phenotypes were determined by the clot lysis at 30 minutes (LY30): shutdown ≤ 0.8%, physiologic 0.9% to 2.9%, and hyperfibrinolysis ≥ 3%. Logistic regression was used to adjust for age, arrival blood pressure, ISS, mechanism, and facility.
RESULTS:
There were 2,540 patients who met inclusion criteria. Median age was 39 years (interquartile range [IQR] 26 to 55 years) and median ISS was 25 (IQR 20 to 33), with a mortality rate of 21%. Fibrinolysis shutdown was the most common phenotype (46%) followed by physiologic (36%) and hyperfibrinolysis (18%). Hyperfibrinolysis was associated with the highest death rate (34%), followed by shutdown (22%), and physiologic (14%, p < 0.001). The risk of mortality remained increased for hyperfibrinolysis (odds ratio [OR] 3.3, 95% CI 2.4 to 4.6, p < 0.0001) and shutdown (OR 1.6, 95% CI 1.3 to 2.1, p = 0.0003) compared with physiologic when adjusting for age, ISS, mechanism, head injury, and blood pressure (area under the receiver operating characteristics curve 0.82, 95% CI 0.80 to 0.84).
CONCLUSIONS:
Fibrinolysis shutdown is the most common phenotype on admission and is associated with increased mortality. These data provide additional evidence of distinct phenotypes of coagulation impairment and that individualized hemostatic therapy may be required.
| Tags : coagulopathie
03/06/2016
The 2015 Remote Damage Control Resuscitation Symposium
| Tags : transfusion, coagulopathie


1365-2044/asset/olbannerleft.gif?v=1&s=bd83df57543a1d11ffc15f630bb1301f0be80859)