01/05/2016
Albumine aussi bien que PFC ?
Influences of Limited Resuscitation with Plasma or Plasma Protein Solutions on Hemostasis and Survival of Rabbits with Non-Compressible Hemorrhage
J Trauma Acute Care Surg. 2016 Apr 27. Kheirabadi BS et Al.
BACKGROUND:
Plasma infusion with or without RBC is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
Anesthetized spontaneously breathing rabbits (3.3±0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 min with Plasma-Lyte (PAL; 30 ml/kg), PAL+ fibrinogen (PAL+F; 30ml+100mg/kg), fresh rabbit plasma (PLS; 15ml/kg), or 25% albumin (ALB; 5 ml/kg) solution; all given in two bolus IV injections (15 min apart) to achieve a MAP of 65 mmHg, n=8-9/group. Animals were monitored for 2 hrs or until death and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 min. At 60 min post-injury, MAP was higher with albumin than with crystalloids (PAL or PAL+F), but shock indices were not different despite the large differences in resuscitation volumes.
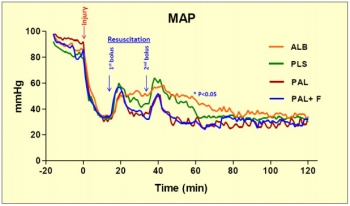
Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein, and increased survival rate to 100% (p<.05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSION:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate, however, its effects did not differ from those obtained with 25% albumin at 1/3 of the volume. The albumin advantage was consistent with our previous findings in which 5% albumin was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its albumin content rather than its coagulation proteins
| Tags : remplissage
11/04/2016
PROPPR Study: 1-1-2 aussi bien !
Damage-control resuscitation and emergency laparotomy: Findings from the PROPPR study
Undurraga VJ et AL. J Trauma Acute Care Surg. 2016 Apr;80(4):568-75
BACKGROUND:
The Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) trial has demonstrated that damage-controlresuscitation, a massive transfusion strategy targeting a balanced delivery of plasma-platelet-red blood cell in a ratio of 1:1:1, results in improved survival at 3 hours and a reduction in deaths caused by exsanguination in the first 24 hours compared with a 1:1:2 ratio. In light of these findings, we hypothesized that patients receiving 1:1:1 ratio would have improved survival after emergency laparotomy.
METHODS:
Severely injured patients predicted to receive a massive transfusion admitted to 12 Level I North American trauma centers were randomized to 1:1:1 versus 1:1:2 as described in the PROPPR trial. From these patients, the subset that underwent an emergency laparotomy, defined previously in the literature as laparotomy within 90 minutes of arrival, were identified. We compared rates and timing of emergency laparotomyas well as postsurgical survival at 24 hours and 30 days.
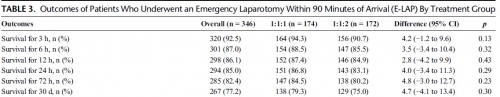
RESULTS:
Of the 680 enrolled patients, 613 underwent a surgical procedure, 397 underwent a laparotomy, and 346 underwent an emergency laparotomy. The percentages of patients undergoing emergency laparotomy were 51.5% (174 of 338) and 50.3% (172 of 342) for 1:1:1 and 1:1:2, respectively (p = 0.20). Median time to laparotomy was 28 minutes in both treatment groups. Among patients undergoing an emergency laparotomy, the proportions of patients surviving to 24 hours and 30 days were similar between treatment arms; 24-hour survival was 86.8% (151 of 174) for 1:1:1 and 83.1% (143 of 172) for 1:1:2 (p = 0.29), and 30-day survival was 79.3% (138 of 174) for 1:1:1 and 75.0% (129 of 172) for 1:1:2 (p = 0.30).
CONCLUSION:
We found no evidence that resuscitation strategy affects whether a patient requires an emergency laparotomy, time to laparotomy, or subsequent survival.
| Tags : coagulopathie, transfusion
28/01/2016
TXA: Interrogations
Les études CRASH2 et MATTERS ont mis en évidence l'intérêt de l'emploi du TXA en traumatologie grave.
Il s'agit d'un dérivé de la lysine qui agit en se liant au plasminogène bloquant ainsi l'interaction plasminogène-fibrine, donc la fibrinolyse du caillot. Le TXA franchit la barrière sang-cerveau, diffuse dans le LCR et le globe oculaire
Persistent malgré tout quelques interrogations en matière d'innocuité persistent. Si l'étude crash2 n' pas montré de risque thromboembolique majeurs, ce n'est pas le cas d' l'étude MATTERS avec environ 10 fois plus d'épisodes thrombo-emboliques en cas d'usage de TXA. Par ailleurs il est rapporté un risque d'hypotension lors de l'administration rapide de TXA et de convulsions lors de l'emploi de posologies élevées. Ceci ne remet pas en cause le recours précoce au TXA dont l'emploi ne doit pas être banalisé et respecter un certain nombre de règles: probabilité forte de coagulopathie traumatique notamment attesté par une hypotension sévère , 1ère dose le plus tôt possible (au mieux dans la première heure) et pas après 3h, deuxième dose dans les 08h00, administration lente pour éviter hypotension, pas de surdosage facteur de crises convulsives, ne pas administrer en même temps/même ligne que du PLYO.
Un certain nombre d'études complémentaires sont en cours:
1. L'étude "Pre-hospital Antifibrinolytics for Traumatic Coagulopathy and Haemorrhage" a pour objectif d'affiner notre connaissance de l'emploi du TXA.
2.L'étude "Design of the Study of Tranexamic Acid during Air Medical Prehospital Transport (STAAMP) Trial: Addressing the Knowledge Gaps" a pour objet d'étuider la mortalité à 30 jours de traumatisés sévères pris en charge par medevac héliportées.
3. L'étude "Tranexamic Acid Mechanisms and Pharmacokinetics In Traumatic Injury (TAMPITI Trial)" vise quand à elle à confirmer un certain nombre d'hypothèses sur le mécanisme d'action.
Par ailleurs, le TXA n'est pas le seul antifibrinolyique utilisable.
| Tags : coagulopathie
21/01/2016
Le graal plaquettaire hémostatique ?
Thrombosomes: a platelet-derived hemostatic agent for control of noncompressible hemorrhage
Fitzpatrick GM et Al. Transfusion. 2013 Jan;53 Suppl 1:100S-106S
----------------
Un thrombosome est en quelque sorte une plaquette lyophilisée dans laquelle l'eau est remplacée par un sucre particulier: le trehalose. Ré exposé à une atmosphère humide, il se réhydrate pour retrouver toutes ses propriétés. Cela ne semble pas être une simple théorie car il initierait une génération de thrombine permettant la formation d'un caillot de manière satisfaisante. Des thrombosmes, du fibrinogène et du PLyo, on peut espérer !
----------------
BACKGROUND: Uncontrolled hemorrhage is responsible for ~80% of the potentially survivable deaths in combat and over 40% of early mortality in the under 65 age group in the United States. Providing an easily used infusible hemostatic agent to first responders could significantly reduce these fatalities. We report on an infusible lyophilized platelet-derived hemostatic agent stabilized with trehalose and polysucrose prior to and during lyophilization.
STUDY DESIGN AND METHODS: Characterization included determining the particle population size range, surface marker expression GPIb, GPIIbIIIa, and Annexin V binding. Function was assessed by aggregation, thromboelastography, and thrombin generation. Pharmacokinetics, biodistribution, and immunogenicity established using Indium111 labeled Thrombosomes in healthy New Zealand white rabbits (NZWRs), efficacy in thrombocytopenic NZWR, and safety in NZWRs, canines, and nonhuman primates.
RESULTS: Thrombosomes retained GPIIbIIIa expression (98.71% 0.18 of the rehydrated particles), a reduced expression of GPIb (47.77% 6.65), and Annexin V binding (86.05% 2.65). Aggregation to all agonists except thrombin in buffer (78.15% 2.5) was <50%. Thrombin generation and thromboelastography results demonstrated a concentration gradient that was consistent from lot to lot. There were no observed adverse events in any safety study and blood loss was reduced by >80% in the thrombocytopenic ear bleed model.
CONCLUSION: Our in vitro characterization studies in conjunction with preclinical animal safety and efficacy studies demonstrated lot consistency in manufacturing, maintenance of hemostatic functions of Thrombosomes, safety at high dose concentrations, and the potential to provide an effective hemostatic agent at the site of injury.
17/01/2016
Cyanokit pour l'hémorragie massive ?
A prospective, randomized trial of intravenous hydroxocobalamin versus whole blood transfusion compared to no treatment for class III hemorrhagic shock resuscitation in a prehospital swine model
Bebarta VS et Al. Acad Emerg Med.2015 Mar;22(3):321-30
--------------------------------
La prise en charge des hémorragies traumatiques en préhospitalier est basée sur la miseen oeuvre des moyens d'arrêts de ces dernières et l'initiation d'une stratégie raisonnée de remplissage vasculaire et de transfusion. L'apport équilibrée de CGR, de plasma,de fractions coagulantes et même de plaquettes fait partie de cette démarche de damage control resuscitation de même que l'apport d'acide tranexaminique pour s'opposer à une fibrinolyse précoce souvent présente. D'autres axes de recherches sont proposés. AInsi l'hydroxocobalamine, connue en tant qu'antidote de l'acide cynahydrique permettrait sur des cochons auxquels on aurait soustrait 20 ml/kg de sang de préserver la pression artérielle et la lactatémie de manière identique à celle obtenue par l'apport de sang total.
--------------------------------
OBJECTIVES:
The objective was to compare systolic blood pressure (sBP) over time in swine that have had 30% of their blood volume removed (Class III shock) and treated with intravenous (IV) whole blood or IV hydroxocobalamin, compared to nontreated control animals.
METHODS:
Thirty swine (45 to 55 kg) were anesthetized, intubated, and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged a total of 20 mL/kg over a 20-minute period. Five minutes after hemorrhage, animals were randomly assigned to receive 150 mg/kg IV hydroxocobalamin solubilized in 180 mL of saline, 500 mL of whole blood, or no treatment. Animals were monitored for 60 minutes thereafter. A sample size of 10 animals per group was determined based on a power of 80% and an alpha of 0.05 to detect an effect size of at least a 0.25 difference (>1 standard deviation) in mean sBP between groups. sBP values were analyzed using repeated-measures analysis of variance (RANOVA). Secondary outcome data were analyzed using repeated-measures multivariate analysis of variance (RMANOVA).
RESULTS:
There were no significant differences between hemodynamic parameters of IV hydroxocobalamin versus whole blood versus control group at baseline (MANOVA; Wilks' lambda; p = 0.868) or immediately posthemorrhage (mean sBP = 47 mm Hg vs. 41 mm Hg vs. 37 mm Hg; mean arterial pressure = 39 mm Hg vs. 28 mm Hg vs. 34 mm Hg; mean serum lactate = 1.2 mmol/L vs. 1.4 mmol/L vs. 1.4 mmol/L; MANOVA; Wilks' lambda; p = 0.348). The outcome RANOVA model detected a significant difference by time between groups (p < 0.001). Specifically, 10 minutes after treatment, treated animals showed a significant increase in mean sBP compared to nontreated animals (mean sBP = 76.3 mm Hg vs. 85.7 mm Hg vs. 51.1 mm Hg; p < 0.001). RMANOVA modeling of the secondary data detected a significant difference in mean arterial pressure, heart rate, and serum lactate (p < 0.001). Similar to sBP, 10 minutes after treatment, treated animals showed a significant increase in mean arterial pressure compared to nontreated animals (mean arterial pressure = 67.7 mm Hg vs. 61.4 mm Hg vs. 40.5 mm Hg). By 10 minutes, mean heart rate was significantly slower in treated animals compared to nontreated animals (mean heart rate = 97.3 beats/min vs. 95.2 beats/min vs. 129.5 beats/min; p < 0.05). Serum lactate, an early predictor of shock, continued to rise in the control group, whereas it did not in treated animals. Thirty minutes after treatment, serum lactate values of treated animals were significantly lower compared to nontreated animals (p < 0.05). This trend continued throughout the 60-minute observation period such that 60-minute values for lactate were 1.4 mmol/L versus 1.1 mmol/L versus 3.8 mmol/L. IV hydroxocobalamin produced a statistically significant increase in systemic vascular resistance compared to control, but not whole blood, with a concomitant decrease in cardiac output.
CONCLUSIONS:
Intravenous hydroxocobalamin was more effective than no treatment and as effective as whole blood transfusion, in reversing hypotension and inhibiting rises in serum lactate in this prehospital, controlled, Class III swine hemorrhage model.
| Tags : choc
12/01/2016
Dexamethasone: Hémostatique cérébral ?
Steroid-loaded Hemostatic Nanoparticles Alleviate Injury Progression after Blast Trauma
Hubbard WD et Al.. ACS Macro Lett., 2015, 4 (4), pp 387–391
The purpose of this study was to investigate whether hemostatic dexamethasone-loaded nanoparticles (hDNP) functionalized with a peptide that binds with activated platelets could reduce cellular injury and improve functional outcomes in a model of blast trauma. Functionalized nanoparticles, or synthetic platelets, offer a wide variety of benefits and advantages compared to alternatives, such as increased biocompatibility and targeting of the injury site (DePalma, 2005). Blood loss is the primary cause of death at acute time points post injury in both civilian and battlefield traumas. Currently, there is a shortage in treatments for internal bleeding, especially for rapid administration in open field combat. In a recent U.K. study, less than fifty percent of soldiers diagnosed with primary blast lung injury (PBLI), the most common fatal blast injury, survived to reach a medical facility (Smith, 2011). This study examines potential therapeutic effects of hDNP on subacute recovery in brain pathology and behavior after blast polytrauma. An established polytrauma model that simulates severe injury, including PBLI and blast-induced neurotrauma (BINT), can be used to evaluate life-saving therapeutics (Hubbard, 2014). Poly(lactic-co-glycolic acid)-based nanoparticles with poly(ethylene glycol) arms and the arginine-glycine-aspartic acid (RGD) peptide to target activated platelets were fabricated. A blast-induced polytrauma rodent model was used to evaluate the functionalized nanoparticles at an acute stage. After anesthesia, Male Sprague Dawley rats were exposed to a single, representative “free field” blast wave from an Advanced Blast Simulator at Virginia Tech at a peak overpressure of 28 psi for 2.5 ms duration, operating above 50% lethality risk, in a sidethorax orientation (Hubbard, 2014). After injury, animals were immediately injected intravenously with hDNP, control dexamethasone-loaded nanoparticles (cDNP), or lactated ringers (LR) and physiological parameters were monitored. Sham animals were not injected or exposed to the blast wave. Open field assays were performed on surviving animals to measure levels of anxiety. At one week post-blast, brains were extracted and sections from the amygdala were obtained for immunofluorescent staining using glial fibrillary acidic protein (GFAP; activated astrocytes), cleaved caspase-3 (apoptosis), and SMI-71 (blood-brain barrier). According to physiological monitoring immediately after blast, oxygen saturation was significantly decreased in the control and LR groups compared to the active and sham groups. Using the open field test, elevated anxiety parameters were found in the control and LR groups compared to the hDNP group. GFAP was significantly elevated in the control group compared to the hDNP and sham groups in the amygdala. Caspase-3 was also significantly elevated in the control group compared to the hDNP group. SMI-71 was significantly reduced in the LR group compared to the sham group. hDNP treatment has the potential to assist recovery after internal hemorrhage. Immediate intervention to assuage hemorrhage, one source for injury pathology, is crucial to mitigate debilitating injury mechanisms that lead to cognitive and emotional deficits (Shetty, 2014).
It is possible that through prevention of microhemorrhaging of the blood-brain barrier (BBB), hDNP was able to mitigate cellular injury and improve cognitive outcomes. Future studies will evaluate the effect on inflammatory and hypoxia-related proteins after hDNP administration post-trauma.
| Tags : blast, hémorragie
25/12/2015
Transfusion de CGR: Les + graves seulement
Red Blood Cell Transfusion and Mortality in Trauma Patients: Risk-Stratified Analysis of an Observational Study
Perel P et Al. PLoS Med. 2014 Jun 17;11(6):e1001664
-------------------------------------
Les données qui suivent sont extraites de la cohorte des patients inclus dans l'étude CRASH2. Cette réinterprétation des données a pour objectif d'analyser le lien entre la mortalité à 28 jours et la transfusion de CGR. Les auteurs retrouvent un effet délétère de la transfusion de CGR pour les patients les moins à risque de mortalité. Ceci est en faveur des démarches de stratégies transfusionnelles sinon restrictives du moins raisonnées en fonction du contexte notamment préhospitalier où cette pratique associée à l'apport de fractions coagulantes semble être d'un grand intérêt(1).
-------------------------------------
Background:
Haemorrhage is a common cause of death in trauma patients. Although transfusions are extensively used in the care of bleeding trauma patients, there is uncertainty about the balance of risks and benefits and how this balance depends on the baseline risk of death. Our objective was to evaluate the association of red blood cell (RBC) transfusion with mortality according to the predicted risk of death.
Methods and Findings:
A secondary analysis of the CRASH-2 trial (which originally evaluated the effect of tranexamic acid on mortality in trauma patients) was conducted. The trial included 20,127 trauma patients with significant bleeding from 274 hospitals in 40 countries. We evaluated the association of RBC transfusion with mortality in four strata of predicted risk of death: ,6%, 6%–20%, 21%–50%, and .50%. For this analysis the exposure considered was RBC transfusion, and the main outcome was death from all causes at 28 days. A total of 10,227 patients (50.8%) received at least one transfusion. We found strong evidence that the association of transfusion with all-cause mortality varied according to the predicted risk of death (p-value for interaction ,0.0001). Transfusion was associated with an increase in all-cause mortality among patients with , 6% and 6%–20% predicted risk of death (odds ratio [OR] 5.40, 95% CI 4.08–7.13, p,0.0001, and OR 2.31, 95% CI 1.96–2.73, p,0.0001, respectively), but with a decrease in all-cause mortality in patients with .50% predicted risk of death (OR 0.59, 95% CI 0.47–0.74, p,0.0001). Transfusion was associated with an increase in fatal and non-fatal vascular events (OR 2.58, 95% CI 2.05–3.24, p,0.0001). The risk associated with RBC transfusion was significantly increased for all the predicted risk of death categories, but the relative increase was higher for those with the lowest (,6%) predicted risk of death (p-value for interaction ,0.0001). As this was an observational study, the results could have been affected by different types of confounding. In addition, we could not consider haemoglobin in our analysis. In sensitivity analyses, excluding patients who died early; conducting propensity score analysis adjusting by use of platelets, fresh frozen plasma, and cryoprecipitate; and adjusting for country produced results that were similar.
Conclusions:
The association of transfusion with all-cause mortality appears to vary according to the predicted risk of death. Transfusion may reduce mortality in patients at high risk of death but increase mortality in those at low risk. The effect of transfusion in low-risk patients should be further tested in a randomised trial.
| Tags : hémorragie
20/12/2015
Coagulopathie: Du fibrinogène avant tout
Trauma-induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs
Nardi G et al. Critical Care (2015) 19:83
------------------------------------
Le damage control resuscitation fait largement appel à l'apport de plasma, concentrés de globules rouges et de plaquettes dans un rapport de 1/1/1 (1). Malgré la relative correction de la coagulopathie la survie à long terme ne semble pas être améliorée (2). Aussi certains proposent d'avoir plutôt recours à l'administration précoce de fibrinogène plutôt que l'administration de plasma. Le travail suivant qui propose l'apport précoce de 2g de fibrinogène est en faveur d'une telle démarche.
------------------------------------
INTRODUCTION:
Hemorrhage is the principal cause of death in the first few hours following severe injury. Coagulopathy is a frequent complication of critical bleeding. A network of Italian trauma centers recently developed a protocol to prevent and treat trauma-induced coagulopathy. A pre-post cohort multicenter study was conducted to assess the impact of the early coagulation support (ECS) protocol on blood products consumption,mortality and treatment costs.
METHODS:
We prospectively collected data from all severely injured patients (Injury Severity Score (ISS) >15) admitted to two trauma centers in 2013 and compared these findings with the data for 2011. Patients transfused with at least 3 units of packed red blood cells (PRBCs) within 24 hours of an accident were included in the study. In 2011, patients with significant hemorrhaging were treated with early administration of plasma with the aim of achieving a high (≥1:2) plasma-to-PRBC ratio. In 2013, the ECS protocol was the treatment strategy. Outcome data, blood product consumption and treatment costs were compared between the two periods.
RESULTS:
The two groups were well matched for demographics, injury severity (ISS: 32.9 in 2011 versus 33.6 in 2013) and clinical and laboratory data on admission. In 2013, a 40% overall reduction in PRBCs was observed, together with a 65% reduction in plasma and a 52% reduction in platelets. Patients in the ECS group received fewer blood products: 6.51 units of PRBCs versus 8.14 units. Plasma transfusions decreased from 8.98 units to 4.21 units (P <0.05), and platelets fell from 4.14 units to 2.53 units (P <0.05). Mortality in 2013 was 13.5% versus 20% in 2011 (13 versus 26 hospital deaths, respectively) (nonsignificant). When costs for blood components, factors and point-of-care tests were compared, a €76,340 saving in 2013 versus 2011 (23%) was recorded.
CONCLUSIONS:
The introduction of the ECS protocol in two Italian trauma centers was associated with a marked reduction in blood product consumption, reaching statistical significance for plasma and platelets, and with a non-significant trend toward a reduction in early and 28-daymortality. The overall costs for transfusion and coagulation support (including point-of-care tests) decreased by 23% between 2011 and 2013.
| Tags : coagulopathie
12/11/2015
Et l'albumine ?
Is limited prehospital resuscitation with plasma more beneficial than using a synthetic colloid? An experimental study in rabbits with parenchymal bleeding
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2015;78: 752-759
--------------------------------------
Il existe de grands débats sur la manière optimale d'assurer le remplissage vasculaire des blessés de guerre. Pour certains le fluide de référence est un hydroxyéthylamidon, pour d'autres un cristalloïde isotonique et en ce qui nous concerne les deux avec la mise en avant du sérum salé hypertonique premier suivi d'HEA. Actuellement il existe une tendance à promouvoir une autre stratégie faisant appel pour les blessés les plus graves au plasma voire la transfusion de sang frais. L'étude proposée avait pour objectif de confirmer l'intérêt d'une démarche "plasma premier". Une des surprises a été de constater que ce n'est pas cette dernière qui permettait d'obtenir le meilleur taux de survie mais l'emploi d'albumine, et ce de loin. Ces données expérimentales certes très partielles permettent aux auteurs (?) de rediscuter les conclusions de travaux anciens notamment de l'étude SAFE (1,2). Les solutés d'albumine utilisés par cette dernière ont une osmolarité de 260 mosm/kg (versus 305 mosm/kg pour le sérum salé). Les effets délétères notamment chez le traumatisé crânien pourraient être dus non pas à l'extravasation d'albumine dans le parenchyme cérébral lésé mais à l'hypoosmolarité de l'albumex 4%, ces deux mécanismes concourrant à la plus grande fréquence d'HTIC dans le groupe albumine (3). A méditer
--------------------------------------
BACKGROUND:
Reports of survival benefits of early transfusion of plasma with red blood cells (1:1 ratio) in trauma patients suggest that plasma may be a better fluid to replace Hextend for battlefield resuscitation. We studied possible advantages of prehospital resuscitation with plasma compared with Hextend or albumin in a model of uncontrolled hemorrhage.
METHODS:
Male New Zealand white rabbits (3.3 T 0.1 kg) were anesthetized, instrumented, and subjected to a splenic injury with uncontrolled bleeding. Ten minutes after injury (mean arterial pressure [MAP] G 40 mm Hg), the rabbits received small and equal volumes (15 mL/kg) of rabbit plasma (n = 10), Hextend (n = 10), or 5% human albumin (n = 9) or no fluid. Fluids were administered in two bolus injections (20 minutes apart) and targeted to aMAP of 65 mm Hg. Animals were monitored for 2.5 hours or until death, and their blood losses were measured. Arterial blood samples were collected at different times and analyzed for ABG, CBC, and coagulation tests.
RESULTS:
There were no differences in baseline measures among groups. Splenic injury caused similar hemorrhages (9.1 T 0.4 mL/kg at 10 minutes) and decreased MAP in all subjects. Subsequent resuscitation initiated additional bleeding. At 60 minutes after injury (20 minutes after resuscitation), longer activated partial thromboplastin time and lower fibrinogen concentrations were apparent compared with baseline values with differences among groups. Thrombelastography analysis indicated faster and stronger clot formation with plasma and albumin resuscitation than with Hextend use. Shock indices were increased in all groups, but smaller changes were measured in the albumin group. Total blood loss did not differ among resuscitated rabbits but was higher (p G 0.05) than among nonresuscitated animals. Survival rates were 11% (untreated), 40% (Hextend and plasma), and 89% (albumin, p G 0.05).
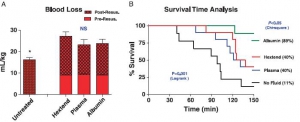
CONCLUSION:
Resuscitation with plasma or albumin better preserved coagulation function than did Hextend. However, despite these improvements, plasma resuscitation did not reduce blood loss or improve survival, while albumin administration seemed beneficial
| Tags : remplissage, coagulopathie
10/11/2015
Dépakine chez le blessé cranien en choc ?
Treatment with a histone deacetylase inhibitor, valproic acid, is associated with increased platelet activation in alarge animal model of traumatic brain injury and hemorrhagic shock
Dekker SE et Al. J Surg Res. 2014 Jul;190(1):312-8
---------------------------
Le concept du damaged control resuscitation fait appel en partie à de nouvelles modalités transfusionnelles et d'emploi de fractions coagulantes. D'autres approches sont possibles comme celles visant à restuarer la fonction plaquettaire. C'est ce que permettrait l'adminsitration de médicaments appartenant à la classe des inhibiteurs des histone deacetylase et dont les effets neuroprotecteurs pourraient ainsi être mis à profit. Le document proposé semble conforter cette approche.
---------------------------
BACKGROUND:
We have previously shown that resuscitation with fresh frozen plasma (FFP) in a large animal model of traumatic brain injury (TBI) and hemorrhagic shock (HS) decreases the size of the brain lesion, and that addition of a histone deacetylase inhibitor, valproic acid (VPA), provides synergistic benefits. In this study, we hypothesized that VPA administration would be associated with a conservation of platelet function as measured by increased platelet activation after resuscitation.
MATERIALS AND METHODS:
Ten swine (42-50 kg) were subjected to TBI and HS (40% blood loss). Animals were left in shock for 2 h before resuscitation with either FFP or FFP+VPA (300 mg/kg). Serum levels of platelet activation markers transforming growth factor beta, CD40 L, P-selectin, and platelet endothelial cell adhesion molecule (PECAM) 1 were measured at baseline, postresuscitation, and after a 6-h observation period. Platelet activation markers were also measured in the brain whole cell lysates and immunohistochemistry.
RESULTS:
Circulating P-selectin levels were significantly higher in the FFP+VPA group compared with the FFP alone group (70.85±4.70 versus 48.44±7.28 ng/mL; P<0.01). Likewise, immunohistochemistry data showed elevated P-selectin in the VPA treatment group (22.30±10.39% versus 8.125±3.94%, P<0.01). Serum sCD40L levels were also higher in the FFP+VPA group (3.21±0.124 versus 2.38±0.124 ng/mL; P<0.01), as was brainsCD40L levels (1.41±0.15 versus 1.22±0.12 ng/mL; P=0.05). Circulating transforming growth factor beta levels were elevated in the FFP+VPA group, but this did not reach statistical significance (11.20±1.46 versus 8.09±1.41 ng/mL; P=0.17). Brain platelet endothelial cell adhesion molecule 1 levels were significantly lower in the FFP+VPA group compared with the FFP group (5.22±2.00 pg/mL versus 7.99±1.13 pg/mL; P=0.03).
CONCLUSIONS:
In this clinically relevant large animal model of combined TBI+HS, the addition of VPA to FFP resuscitation results in an early upregulation of platelet activation in the circulation and the brain. The previously observed neuroprotective effects of VPA may be due to a conservation of platelet function as measured by a higher platelet activation response after resuscitation.
| Tags : tbi, coagulopathie
09/11/2015
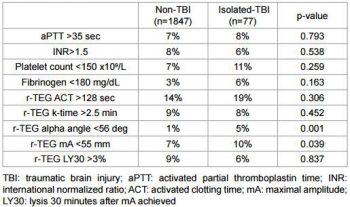
Plaie cérébrale et coagulopathie
Quelques faits
1. Elle est fréquente voire très fréquente: Greuters et al. Critical Care 2011 15:R2 doi:10.1186/cc9399

2. Elle est + fréquente en cas d'hypoTA: Wafaisade Neurocrit Care. 2010 Apr;12(2):211-9
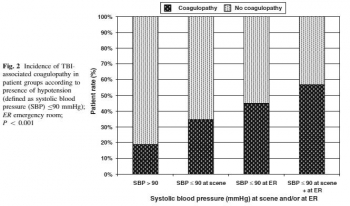
3. Elle est de mauvais pronostic: J Emerg Trauma Shock. 2013 Jul-Sep; 6(3): 180–185

4. Elle est mise en évidence plutôt par thromboélastographie (r TEG) : Sixta al., J Neurol Neurophysiol 2014, 6:5
| Tags : coagulopathie
08/11/2015
Damage Control: Vraiment bénéfique
Changing Patterns of In-Hospital Deaths Following Implementation of Damage Control Resuscitation Practices in US Forward Military Treatment Facilities
Langan NR et Al. JAMA Surg. 2014;149(9):904-912
Importance
Analysis of combat deaths provides invaluable epidemiologic and quality-improvement data for trauma centers and is particularly important under rapidly evolving battlefield conditions.
Objective
To analyze the evolution of injury patterns, early care, and resuscitation among patients who subsequently died in the hospital, before and after implementation of damage control resuscitation (DCR) policies.
Design, Setting, and participants
In a review of the Joint Theater Trauma Registry (2002-2011) of US forward combat hospitals, cohorts of patients with vital signs at presentation and subsequent in-hospital death were grouped into 2 time periods: pre-DCR (before 2006) and DCR (2006-2011).
Main outcomes and measures
Injury types and Injury Severity Scores (ISSs), timing and location of death, and initial (24-hour) and total volume of blood products and fluid administered.
Results
Of 57 179 soldiers admitted to a forward combat hospital, 2565 (4.5%) subsequently died in the hospital. The majority of patients (74%) were severely injured (ISS > 15), and 80% died within 24 hours of admission. Damage control resuscitation policies were widely implemented by 2006 and resulted in a decrease in mean 24-hour crystalloid infusion volume (6.1-3.2 L) and increased fresh frozen plasma use (3.2-10.1 U) (both P < .05) in this population. The mean packed red blood cells to fresh frozen plasma ratio changed from 2.6:1 during the pre-DCR period to 1.4:1 during the DCR period (P < .01). There was a significant increase in mean ISS between cohorts (pre-DCR ISS = 23 vs DCR ISS = 27; P < .05) and a marked shift in injury patterns favoring more severe head trauma in the DCR cohort.
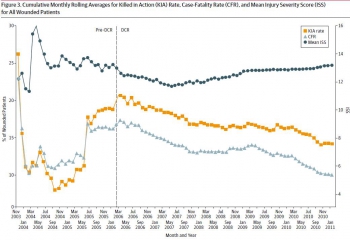
Conclusions and relevance
There has been a significant shift in resuscitation practices in forward combat hospitals indicating widespread military adoption of DCR. Patients who died in a hospital during the DCR period were more likely to be severely injured and have a severe brain injury, consistent with a decrease in deaths among potentially salvageable patients
| Tags : remplissage
02/11/2015
Mg++: Médicament de la coagulopathie ?
Both acute delivery of and storage with magnesium sulfate promote cold-stored platelet aggregation and coagulation function
Meledeo MA et Al. J Trauma Acute Care Surg. 2015 Oct;79(4 Suppl 2):S139-45
----------------------------------------
Il y a quelque mois était publié un travail de recherche portant sur l'intérêt de l'administration de Adénosine/Lidocaïne/Mg2+ ALM (1, 2, 3). Une hypothèse faite par les auteurs serait que L'ALM agirait comme un antifibrinolytique en activant la voie du thrombin-activatable fibrinolysis inhibitor (TAFI) plutôt que celle de la protéine C. Cette action passerait par un mécanisme antiinflammatoire, une modification de la polarité endothéliale et une action sur la fonction plaquettaire. Le travail expérimental dont l'abstract est présenté met en avant l'intérêt de l'adminsitration de magnésium pour la restauration de la fonction plaquettaire après conservation de palquettes d'aphérèse au delà de 5 jours.
----------------------------------------
BACKGROUND:
The platelet storage lesion causes loss of function and viability over time. A new paradigm for platelet storage is desired to enable safer, more effective transfusions while reducing waste. We hypothesized that repletion of Mg, which is chelated by citrate anticoagulant, could reduce platelet storage lesion severity when given in conjunction with storage at a refrigerated temperature.
METHODS:
Apheresis platelet units were collected from healthy donors and stored at 22°C or 4°C. On Days 0, 2, 4, and 8, samples were collected for analyses of receptor-mediated aggregation, coagulation, adhesion to collagen under flow, and viability. In the first series, samples were given anacute dose of MgSO4 before testing; in the second series, storage bags were supplemented with 0-, 3-, or 6-mM MgSO4.
RESULTS:
Acutely delivered MgSO4 induced a more rapid coagulation time in apheresis platelets, further enhanced by storage at 4°C. Plateletadhesion to a collagen surface while exposed to arterial shear rates (920 s) was enhanced by MgSO4 supplementation-acute MgSO4 had a large effect on adhesion of fresh platelets, which diminished more rapidly in 22°C samples, while storage with MgSO4 showed significant benefits even out to Day 4 at both temperatures. Although 4°C storage improves the longevity of platelet aggregation responses to agonists, MgSO4 supplementation did not change those responses.
CONCLUSION:
Acute MgSO4 reduces clot time likely through the transient increase of free Ca. Limited differences between platelet function inacute delivery of and storage with MgSO4 diminish the possibility that Mg-induced metabolic inhibition of platelets synergizes with 4°C storage. Regardless, magnesium supplementation to platelets is an exciting possibility in transfusion because the adhesion response of 22°C-stored platelets on Day 4 is significantly enhanced when stored with 6-mM MgSO4
| Tags : coagulopathie
18/09/2015
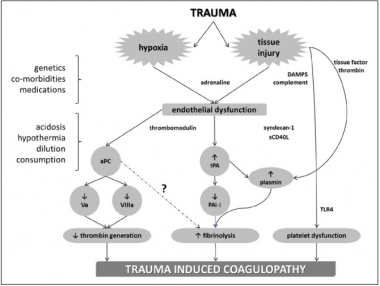
Coagulopathie traumatique: Mécanismes
Trauma-Induced Coagulopathy: An Institution's 35 Year Perspective on Practice and Research
Gonzales E. et Al. Scandinavian Journal of Surgery 103: 89–103, 2014
| Tags : coagulopathie
03/07/2015
Fibrinogène avec le TXA ?: Plutôt oui
Association of Cryoprecipitate and Tranexamic Acid With Improved Survival Following Wartime Injury: Findings From the MATTERs II Study
Morrison JJ et Al. JAMA Surg. 2013;148(3):218-225.
Objective To quantify the impact of fibrinogen-containing cryoprecipitate in addition to the antifibrinolytic tranexamic acid on survival in combat injured.
Design Retrospective observational study comparing the mortality of 4 groups: tranexamic acid only, cryoprecipitate only, tranexamic acid and cryoprecipitate, and neither tranexamic acid nor cryoprecipitate. To balance comparisons, propensity scores were developed and added as covariates to logistic regression models predicting mortality.
Setting A Role 3 Combat Surgical Hospital in southern Afghanistan.
Patients A total of 1332 patients were identified from prospectively collected UK and US trauma registries who required 1 U or more of packed red blood cells and composed the following groups: tranexamic acid (n = 148), cryoprecipitate (n = 168), tranexamic acid/cryoprecipitate (n = 258), and no tranexamic acid/cryoprecipitate (n = 758).
Main Outcome Measure In-hospital mortality.
Results Injury Severity Scores were highest in the cryoprecipitate (mean [SD], 28.3 [15.7]) and tranexamic acid/cryoprecipitate (mean [SD], 26 [14.9]) groups compared with the tranexamic acid (mean [SD], 23.0 [19.2]) and no tranexamic acid/cryoprecipitate (mean [SD], 21.2 [18.5]) (P < .001) groups. Despite greater Injury Severity Scores and packed red blood cell requirements, mortality was lowest in the tranexamic acid/cryoprecipitate (11.6%) and tranexamic acid (18.2%) groups compared with the cryoprecipitate (21.4%) and no tranexamic acid/cryoprecipitate (23.6%) groups. Tranexamic acid and cryoprecipitate were independently associated with a similarly reduced mortality (odds ratio, 0.61; 95% CI, 0.42-0.89; P = .01 and odds ratio, 0.61; 95% CI, 0.40-0.94; P = .02, respectively). The combined tranexamic acid and cryoprecipitate effect vs neither in a synergy model had an odds ratio of 0.34 (95% CI, 0.20-0.58; P < .001), reflecting nonsignificant interaction (P = .21).
Conclusions Cryoprecipitate may independently add to the survival benefit of tranexamic acid in the seriously injured requiring transfusion. Additional study is necessary to define the role of fibrinogen in resuscitation from hemorrhagic shock.
| Tags : coagulopathie
07/02/2015
RFE Choc hémorragique
| Tags : choc, hémorragie
30/10/2014
Plaquettes synthétiques: Possible ? Mais oui
Tuning Ligand Density on Intravenous Hemostatic Nanoparticles Dramatically Increases Survival Following Blunt Trauma
Proc Natl Acad Sci U S A. 2014 Jul 15;111 (28) 10293-10298
Des plaquettes synthétiques pour arrêter le saignement ? Certains l'ont fait grâce à la technologie des nanoparticules (1, 2). Un espoir qui reste à confirmer.
-----------------------------------------------------------------------------------
Explosions account for 79% of combat-related injuries, leading to multiorgan hemorrhage and uncontrolled bleeding. Uncontrolled bleeding is the leading cause of death in battlefield traumas as well as in civilian life. We need to stop the bleeding quickly to save lives, but, shockingly, there are no treatments to stop internal bleeding. A therapy that halts bleeding in a site-specific manner and is safe, stable at room temperature, and easily administered is critical for the advancement of trauma care. To address this need, we have developed hemostatic nanoparticles that are administered intravenously. When tested in a model of blast trauma with multiorgan hemorrhaging, i.v. administration of the hemostatic nanoparticles led to a significant improvement in survival over the short term (1 h postblast). No complications from this treatment were apparent out to 3 wk. This work demonstrates that these particles have the potential to save lives and fundamentally change trauma care.
-----------------------------------------------------------------------------------
| Tags : hémorragie
21/11/2013
Le plasma lyophilisé: Bon pour le cerveau du traumatisé qui saigne
Early treatment with lyophilized plasma protects the brain in a large animal model of combined traumatic brain injury and hemorrhagic shock
Imam AM et Al. J Trauma Acute Care Surg. 2013;75: 976-983
accéder aux abstracts de la WTA publiés dans J trauma Acute care
_____________________________________
Bien sûr une étude animale, mais une de plus qui milite pour un emploi précoce du plasma lyophylisé.
_____________________________________
BACKGROUND: Combination of traumatic brain injury (TBI) and hemorrhagic shock (HS) can result in significant morbidity and mortality. We have previously shown that early administration of fresh frozen plasma (FFP) in a large animal model of TBI and HS reduces the size of the brain lesion as well as the associated edema. However, FFP is a perishable product that is not well suited for use in the austere prehospital settings. In this study, we tested whether a shelf-stable, low-volume, lyophilized plasma (LSP) product was as effective as FFP.
METHODS:
Yorkshire swine (42-50 kg) were instrumented to measure hemodynamic parameters, intracranial pressure, and brain tissue oxygenation. A prototype, computerized, cortical impact device was used to create TBI through a 20-mm craniotomy: 15-mm cylindrical tipimpactor at 4 m/s velocity, 100-millisecond dwell time, and 12-mm penetration depth. Volume-controlled hemorrhage was induced(40-45% total blood volume) concurrent with the TBI. After 2 hours of shock, animals were treated with (1) normal saline (NS, n = 5), (2) FFP (n = 5), and (3) LSP (n = 5). The volume of FFP and LSP matched the shed blood volume, whereas NS was 3 times the volume. Six hours after resuscitation, brains were sectioned and stained with TTC (2, 3, 5-Triphenyltetrazolium chloride), and lesion size (mm3) and swelling (percent change in volume compared with the contralateral, uninjured side) were measured.
RESULTS:
This protocol resulted in a highly reproducible brain injury, with clinically relevant changes in blood pressure, cardiac output, tissue hypoperfusion, intracranial pressure, and brain tissue oxygenation. Compared with NS, treatment with LSP significantly ( p G 0.05) decreased brain lesion size and swelling (51% and 54%, respectively).
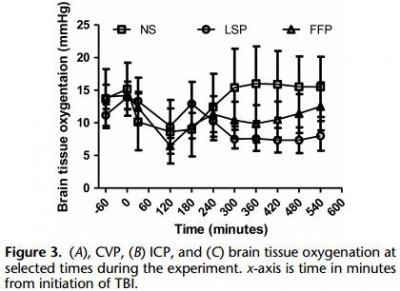
CONCLUSION: In a clinically realistic combined TBI + HS model, early administration of plasma products decreases brain lesion size and edema. LSP is as effective as FFP, while offering many logistic advantages.
| Tags : tbi, coagulopathie
07/08/2013
Plasma: En préhospitalier AUSSI +++
Point-of-injury use of reconstituted freeze dried plasma as a resuscitative fluid: A special report for prehospital trauma care
Glassberg E. et All. J J Trauma Acute Care Surg. 2013;75(Suppl 2):S111YS111.
La prise en charge d'hémorrragie catastrophique en phase préhospitalière est particulièrement complexe. Ces dernières années la mise en place d'un réseau structuré de prise en charge, 'application de procédures spécifiques visant à arrêter les hémorragies au plus tôt, le recours à l'acide tranexaminique, la prévention des hypothermies et l'application d'une politique raisonnée de rénaimation/chirurgie ont constitué une grande avancée. Certaines nations ont équipé leurs vecteurs d'évacuations de concentrés érythrocytaires. Le maintien d'une coagulation optimale est un enjeu majeur. Pour cela existe, entre autres, le plasma lyophilisé. Les forces armées israéliennes militent pour l'emploi de ce type de solutions en phase préhospitalière
| Tags : coagulopathie, hémorragie
16/07/2013
Management of bleeding and coagulopathy following major trauma: an updated European guideline
| Tags : hémorragie, traumatologie