29/06/2016
Afghanistan et le bilan hollandais
28/06/2016
Crico: Incisez et palpez sous la peau !
Deficiencies in locating the cricothyroid membrane by palpation: We can’t and the surgeons can’t, so what now for the emergency surgical airway ?
Law JA et Al. Can J Anesth (2016) 63:791–796
"......Certaines questions concernant la localisation de la membrane cricothyroïdienne demeurent sans réponse. Nous savons désormais que la palpation externe manque de précision, indépendamment de la spécialité du médecin évaluateur. En d’autres termes, les techniques qui s’appuient sur un accès direct à la trachée via la membrane cricothyroïdienne palpée depuis l’extérieur (par ex., les techniques percutanées de Seldinger ou réalisées à l’aide d’un trocart, un accès basé sur un scalpel à l’aide d’une coupure horizontale unique) courent toutes le risque d’un mauvais positionnement. L’alternative, lorsqu’on a recours à ces techniques de cricothyrotomie (en fait, à toutes ces techniques), est de commencer par une incision verticale médiane de 3-4 cm à travers la peau et les tissus sous-cutanés situés sur l’emplacement estimé de la membrane cricothyroïdienne.5,6 La membrane cricothyroïdienne est ensuite palpée à nouveau dans la lésion, et son emplacement devrait être bien plus facile à déterminer lorsqu’il y a considérablement moins de tissu mou entre le doigt qui palpe et la membrane cricothyroïdienne. La cricothyrotomie peut ensuite se faire à l’aide de la technique choisie et en étant absolument certain de son bon positionnement......"
| Tags : airway, coniotomie
27/06/2016
Crico: Utilisez le manche du bistouri !
Surgical Procedures in Trauma Management. New York, NY: Thieme Inc; 1986:303
| Tags : airway, coniotomie
The Trauma Manual: Trauma and Acute Care Surgery
Trauma anesthesia
Albumine 20% plutôt que fibrinogène ?
Influences of limited resuscitation with plasma or plasma protein solutions on hemostasis and survival of rabbits with noncompressible hemorrhage
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2016;81: 42–49
--------------------------------
Dans ce travail et alors que l'albumine diluée n'est pas recommandée, les auteurs évoquent la possibilité que les effets favorables d'une réanimation basée sur l'apport de plasma serait lié à l'apport de protéine et en particulier d'albumine qui aurait un effet tampon élevé, réduisant l'acidose métabolique, un des facteurs de la triade létale.
--------------------------------
BACKGROUND:
Plasma infusion with or without red blood cells is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
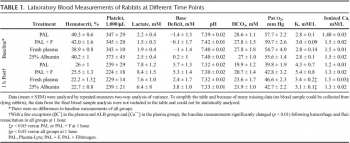
METHODS:
Anesthetized spontaneously breathing rabbits (3.3 ± 0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 minutes with Plasma-Lyte (PAL; 30 mL/kg), PAL + fibrinogen (PAL + F; 30 mL + 100 mg/kg), fresh rabbit plasma (15 mL/kg), or 25% albumin (ALB; 5 mL/kg) solution, all given in two bolus intravenous injections (15 minutes apart) to achieve a mean arterial pressure of 65 mm Hg, n = 8 to 9/group. Animals were monitored for 2 hours or until death, and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 minutes. At 60 minutes after injury, mean arterial pressure was higher with ALB than with crystalloids (PAL or PAL + F), but shock indices were not different despite the large differences in resuscitation volumes. Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein and increased survival rate to 100% (p < .05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSIONS:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate; however, its effects did not differ from those obtained with 25% ALB at one-third of the volume. The ALB advantage was consistent with our previous findings in which 5% ALB was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its ALB content rather than its coagulation proteins
| Tags : coagulopathie, remplissage
22/06/2016
AL pour intuber: A ressortir de l'oubli
The Myth of Rescue Reversal in “Can’t Intubate, Can’t Ventilate” Scenarios
Naguib N. et Al. Anesth Analg. 2016 Jul;123(1):82-92
__________________________
Ce travail met en avant l'insuffisance des démarches d'antagonisation pour restaurer une ventilation adéquate dans les situations de CICV. En ce qui concerne la gestion des voies aériennes en situation tactique, le principe de la préservation de la ventilation spontanée lors de l'accès aux voies aériennes mérite d'être rappelé. Si la réalisation d'une induction en séquence rapide reste la référence, en cas de difficulté prévisible le recours à une anesthésie locale doit être préférée (lire ce post).
Ceci est parfaitement stipulé dans les RFE "Sédation et analgésie en structure d’urgence" dont on rappelle après la présentation de l'abstract les termes de la question N3.
__________________________
BACKGROUND:
An unanticipated difficult airway during induction of anesthesia can be a vexing problem. In the setting of can't intubate, can't ventilate (CICV), rapid recovery of spontaneous ventilation is a reasonable goal. The urgency of restoring ventilation is a function of how quickly a patient's hemoglobin oxygen saturation decreases versus how much time is required for the effects of induction drugs to dissipate, namely the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade. It has been suggested that prompt reversal of rocuronium-induced neuromuscular blockade with sugammadex will allow respiratory activity to recover before significant arterial desaturation. Using pharmacologic simulation, we compared the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade in normal, obese, and morbidly obese body sizes in this life-threatening CICV scenario. We hypothesized that although neuromuscular function could be rapidly restored with sugammadex, significant arterial desaturation will occur before the recovery from unresponsiveness and/or central ventilatory depression in obese and morbidly obese body sizes.
METHODS:
We used published models to simulate the duration of unresponsiveness and ventilatory depression using a common induction technique with predicted rates of oxygen desaturation in various size patients and explored to what degree rapid reversal of rocuronium-induced neuromuscular blockade with sugammadex might improve the return of spontaneous ventilation in CICV situations.
RESULTS:
Our simulations showed that the duration of neuromuscular blockade was longer with 1.0 mg/kg succinylcholine than with 1.2 mg/kg rocuronium followed 3 minutes later by 16 mg/kg sugammadex (10.0 vs 4.5 minutes). Once rocuronium neuromuscular blockade was completely reversed with sugammadex, the duration of hemoglobin oxygen saturation >90%, loss of responsiveness, and intolerable ventilatory depression (a respiratory rate of ≤4 breaths/min) were dependent on the body habitus and duration of oxygen administration. There is a high probability of intolerable ventilatory depression that extends well beyond the time when oxygen saturation decreases <90%, especially in obese and morbidly obese patients. If ventilatory rescue is inadequate, oxygen desaturation will persist in the latter groups, despite full reversal of neuromuscular blockade. Depending on body habitus, the duration of intolerable ventilatory depression after sugammadex reversal may be as long as 15 minutes in 5% of individuals.
CONCLUSIONS:
The clinical management of CICV should focus primarily on restoration of airway patency, oxygenation, and ventilation consistent with the American Society of Anesthesiologist's practice guidelines for management of the difficult airway. Pharmacologic intervention cannot be relied upon to rescue patients in a CICV crisis.
__________________________
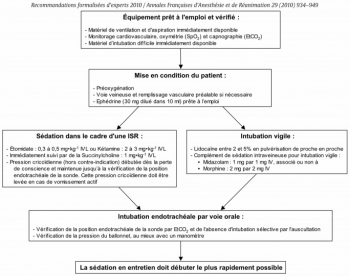
Question 3 - Intubation sous ISR et sous AL : Quelles sont les modalités de réalisation d’une sédation et/ou d’une analgésie pour l’intubation trachéale ?
Les experts recommandent d’administrer une sédation pour toutes les indications de l’intubation trachéale, excepté chez le patient en arrêt cardiaque qui ne nécessite pas de sédation. Lorsque l’intubation trachéale est présumée diffi cile, il est possible d’effectuer une anesthésie locale réalisée de proche en proche, associée ou non à une sédation légère et titrée par voie générale
L’utilisation de médicaments anesthésiques lors de l’intubation trachéale a pour but de faciliter le geste et d’assurer le confort du patient. Cette sédation doit être rapidement réversible pour restaurer une ventilation effi cace en cas de diffi culté d’intubation. Le risque d’inhalation bronchique doit être minimisé au cours de la procédure et ce d’autant que les patients sont considérés comme ayant un estomac plein.
Les experts recommandent d’utiliser les techniques d’intubation en séquence rapide (ISR) associant un hypnotique d’action rapide (étomidate ou kétamine) et un curare d’action brève (succinylcholine) ........................................................
Lorsque l’intubation trachéale est présumée difficile, le protocole recommandé par les experts pour une intubation vigile est le suivant : - Lidocaïne entre 2 et 5% en pulvérisation de proche en proche - Complément de sédation intraveineuse pour intubation vigile : • midazolam : 1 mg par 1 mg IV • associé ou non à de la morphine : 2 mg par 2 mg IV
17/06/2016
Protection: Hauteur du tronc plutôt que taille
Determining the dimensions of essential medical coverage required by military body armour plates utilising Computed Tomography
Breeze J et Al. http://dx.doi.org/10.1016/j.injury.2016.06.010
Plus que la taille du combattant, c'est la hauteur du thorax qui doit guider le choix des protections ballistiques du tronc
-------------------------------------------
Introduction
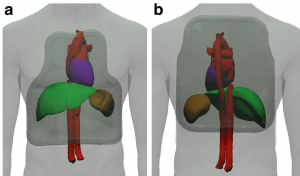
Military body armour is designed to prevent the penetration of ballistic projectiles into the most vulnerable structures within the thorax and abdomen. Currently the OSPREY and VIRTUS body armour systems issued to United Kingdom (UK) Armed Forces personnel are provided with a single size front and rear ceramic plate regardless of the individual’s body dimensions. Currently limited information exists to determine whether these plates overprotect some members of the military population, and no method exists to accurately size plates to an individual.
Method
Computed Tomography (CT) scans of 120 male Caucasian UK Armed Forces personnel were analysed to measure the dimensions of internal thoraco-abdominal anatomical structures that had been defined as requiring essential medical coverage. The boundaries of these structures were related to three potential anthropometric landmarks on the skin surface and statistical analysis was undertaken to validate the results.
Results The range of heights of each individual used in this study was comparable to previous anthropometric surveys, confirming that a representative sample had been used. The vertical dimension of essential medical coverage demonstrated good correlation to torso height (suprasternal notch to iliac crest) but not to stature (r2=0.53 versus 0.04). Horizontal coverage did not correlate to either measure of height. Surface landmarks utilised in this study were proven to be reliable surrogate markers for the boundaries of the underlying anatomical structures potentially requiring essential protection by a plate.
Front and rear Osprey shape
Potential new Shape
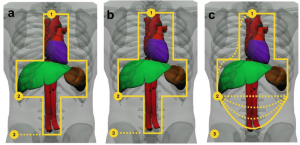
Conclusions
Providing a range of plate sizes, particularly multiple heights, should optimise the medical coverage and thus effectiveness of body armour for UK Armed Forces personnel. The results of this work provides evidence that a single width of plate if chosen correctly will provide the essential medical coverage for the entire military population, whilst recognising that it still could overprotect the smallest individuals. With regards to anthropometric measurements; it is recommended, based on this work, that torso height is used instead of stature for sizing body armour. Coverage assessments should now be undertaken for side protection as well as for other non-Caucasian populations and females, with anthropometric surveys utilising the three landmarks recommended in this study.
Comprimez à distance: Avec le genou +++
Optimization of indirect pressure in order to temporize lifethreatening haemorrhage: a simulation study
Douma MJ et Al. http://dx.doi.org/10.1016/j.injury.2016.06.010
Background
Minimizing haemorrhage using direct pressure is intuitive and widely taught. In contrast, this study examines the use of indirect-pressure, specifically external aortic compression (EAC). Indirect pressure has great potential for temporizing bleeds not amenable to direct tamponade i.e. abdominal-pelvic, junctional, and multi-site trauma. However, it is currently unclear how to optimize this technique.
Methods
We designed a model of central vessel compression using the Malbrain intraabdominal pressure monitor and digital weigh scale. Forty participants performed simulated external aortic compression on the ground, on a stretcher mattress, and with and without a backboard.
Results
The greater the rescuer’s bodyweight the greater was their mean compression (Pearson’s correlation 0.93). Using one-hand, a mean of 28% participant bodyweight (95% CI, 26% - 30%) could be transmitted at sustainable effort, waist-height, and on a stretcher. A second compressing hand increased the percentage of rescuer bodyweight transmission 10-22% regardless of other factors (i.e. presence/absence or a backboard; rescuer position) (p <0.001). Adding a backboard increased transmission of rescuer bodyweight 7%-15% (p < 0.001). Lowering the patient from waist-height backboard to the floor increased transmission of rescuer bodyweight 4%-9% (p < 0.001). Kneeling on the model was the most efficient method and transmitted 11% more weight compared to two-handed maximal compression (p < 0.001).
Conclusions
Efficacy is maximized with larger-weight rescuers who use both hands, position themselves atop victims, and compress on hard surfaces/backboards. Knee compression is most effective and least fatiguing, thus assisting rescuers of lower weight and lesser strength, where no hard surfaces exist (i.e. no available backboard or trauma on soft ground), or when lengthy compression is required (i.e. remote locations). Our work quantifies methods to optimize indirect pressure as a temporizing measure following life-threatening haemorrhage not amenable to direct compression, and while expediting compression devices or definitive treatment.
15/06/2016
Coniotomie: Chirurgicale SVP !
Emergency Cricothyrotomy Performed by Surgical Airway–naive Medical Personnel
Heymans F. et Al. Anesthesiology 2016; 125:00-00
----------------------------------------
L'obstruction des voies aériennes est une cause rare mais évitable de décès au combat. savoir ouvrir un cou est donc un geste qui doit être maîtrisé par le médecin ou l'infirmier présent. Se pose cependant la question de la méthode: chirurgicale ou dispositif spécifique ? Ce travail apporte clairement une réponse. Des personnels de santé novice obtiennent de meilleurs résultats avec la technique chirurgicale. Même si la technique utilisée n'est pas celle promue par la procédure du sauvetage au combat (emploi d'un crochet de hook au lieu d'une pince de Monro-Kelly), ce travail conforte le choix qui est fait d'avoir recours à la technique chirurgicale.
----------------------------------------
Background: When conventional approaches to obtain effective ventilation and return of effective spontaneous breathing fail, surgical airway is the last rescue option. Most physicians have a limited lifetime experience with cricothyrotomy, and it is unclear what method should be taught for this lifesaving procedure. The aim of this study is to compare the performance of medical personnel, naive to surgical airway techniques, in establishing an emergency surgical airway in cadavers using three commonly used cricothyrotomy techniques.
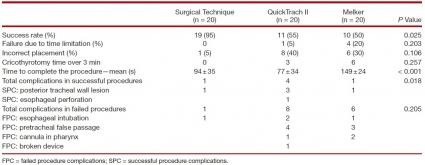
Methods: Twenty medical students, without previous knowledge of surgical airway techniques, were randomly selected from their class. After training, they performed cricothyrotomy by three techniques (surgical, Merkel, and QuickTrach II) in a random order on 60 cadavers with comparable biometrics. The time to complete the procedure, rate of success, and number of complications were recorded. A success was defined as the correct placement of the cannula within the trachea in 3min.
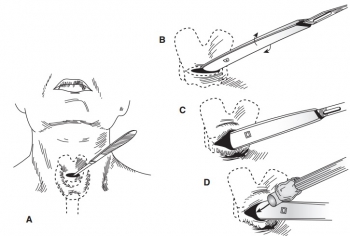
"After intact skin palpation of relevant structures (step 1), a vertical midline skin incision (step 2) is emphasized because it can be extended up or down if not correctly placed and because fewer vessels are located at the midline. Although
rarely emphasized, we recommend finger palpation through the subcutaneous tissue (step 3) and even in the trachea as a guide, as a dissector, and as a dilator; finger palpation is oblivious to bleeding and a better guide to the ligament, being the “surgeon’s eye” during cricothyrotomy. A horizontal incision of the lower aspect of the cricotracheal ligament (step 4) allows for tension release and better opening. A hook permits to maintain the skin and the tracheal opening. Caudal traction (step 5) is recommended because the cricoid cartilage is more resistant and in order to prevent laryngeal injuries. We did not use a dilator, forceps, or a retractor during this experiment. Finally, a cuffed cannula is inserted (step 6)"
Results: The success rates were 95, 55, and 50% for surgical cricothyrotomy, QuickTrach, and Merkel, respectively (P = 0.025).
The majority of failures were due to cannula misplacement (15 of 20). In successful procedures, the mean procedure time was 94± 35 s in the surgical group, 77 ± 34 in the QuickTrach II group, and 149 ±24 in the Melker group (P < 0.001). Few significant complications were found in successful procedures. No cadaver biometric parameters were correlated with success of the procedure.
Conclusion: Surgical airway–naive medical personnel establish emergency cricothyrotomy more efficiently and safely with the surgical procedure than with the other two commonly used techniques
| Tags : airway
14/06/2016
Combat Trauma. Lessons Learned from Military Operations
13/06/2016
Trauma Center: Formateur pour la guerre ?
Skill sets and competencies for the modern military surgeon: Lessons from UK military operations in Southern Afghanistan
Ramassamy A. et Al. Injury. 2010 May;41(5):453-9.
Introduction:
British military forces remain heavily committed on combat operations overseas.UK military operations in Afghanistan (Operation HERRICK) are currently supported by a surgical facility at Camp Bastion, in Helmand Province,in the south of the country. There have been no large published series of surgical workload on Operation HERRICK. The aim of this study is to evaluate this information in order to determine the appropriate skill set for the modern military surgical team.
Method:
A retrospective analysis of operating theatre records between 1st May 2006 and 1st May 2008 was performed. Data was collated on a monthly basis and included patient demographics, operation type and time of operation.
Results:
During the study period 1668 cases required 2210 procedures. Thirty-two per cent were coalition forces (ISAF),27% were Afghan security forces (ANSF)and 39% were civilians. Paediatric casualties accounted for 14.7% of all cases. Ninety-three per cent of cases were secondary to battle injury and of these 51.3% were emergencies. The breakdown of procedures,by specialty, was 66% (1463) orthopaedic, 21% (465) general surgery, 6% (139) head and neck, 5% (104) burns surgery and a further (50) non-battle, non-emergency procedures. There was an almost twofold increase in surgical workload in the second year (1103 cases) compared to the first year of the deployment (565 caps e<s ,0.05).
Discussion:
Surgical workload over the study period has clearly increased markedly since the initial deployment of ISAF forces to Helmand Province. A 6-week deployment to Helmand Province currently provides an equivalent exposure to penetrating trauma as 3 years trauma experience in the UK NHS. The spectrum of injuries seen and the requisite skill set that the military surgeon must possess is outside that usually employed within the NHS. A number of different strategies; including the deployment of trainee specialist registrars to combat hospitals, more focused pre-deploymentmilitary surgery training courses, and wet-laboratory work are proposed to prepare for future generations of surgeons operating in conflict environments
Can J Surg: Numéro spécial 2015
Foreword
Avant-Propos
Introduction
Commentaries
Review
Research
- Correction in:
- Can J Surg. 2015 Oct; 58(5): 317.
Discussions in Surgery
05/06/2016
40 years of terrorist bombings
40 years of terrorist bombings – A meta-analysis of the casualty and injury profile
Ewards DS et Al. Injury, Int. J. Care Injured 47 (2016) 646–652
Introduction: Terrorists have used the explosive device successfully globally, with their effects extending beyond the resulting injuries. Suicide bombings, in particular, are being increasingly deployed due to the devastating effect of a combination of high lethality and target accuracy. The aim of this study was to identify trends and analyse the demographics and casualty figures of terrorist bombings worldwide.
Methods: Analysis of the Global Terrorism Database (GTD) and a PubMed/Embase literature search (keywords ‘‘terrorist’’, and/or ‘‘suicide’’, and/or ‘‘bombing’’) from 1970 to 2014 was performed.
Results: 58,095 terrorist explosions worldwide were identified in the GTD. 5.08% were suicide bombings. Incidents per year are increasing (P < 0.01). Mean casualty statistics per incidents was 1.14 deaths and 3.45 wounded from non-suicide incidents, and 10.16 and 24.16 from suicide bombings (p < 0.05). The kill:wounded ratio was statistically higher in suicide attacks than non-suicide attacks, 1:1.3 and 1:1.24 respectively (p < 0.05). The Middle East witnessed the most incidents (26.9%), with Europe (13.2%) ranked 4th. The literature search identified 41 publications reporting 167 incidents of which 3.9% detailed building collapse (BC), 60.8% confined space (CS), 23.5% open space (OS) and 11.8% semiconfined space (SC) attacks. 60.4% reported on suicide terrorist attacks. Overall 32 deaths and 180 injuries per incident were seen, however significantly more deaths occurred in explosions associated with a BC. Comparing OS and CS no difference in the deaths per incident was seen, 14.2(SD 17.828) and 15.63 (SD 10.071) respectively. However OS explosions resulted in significantly more injuries, 192.7 (SD 141.147), compared to CS, 79.20 (SD 59.8). Extremity related wounds were the commonest injuries seen (32%).
Discussion/Conclusion: Terrorist bombings continue to be a threat and are increasing particularly in the Middle East. Initial reports, generated immediately at the scene by experienced coordination, on the type of detonation (suicide versus non-suicide), the environment of detonation (confined, open, building collapse) and the number of fatalities, and utilising the Kill:Wounded ratios found in this meta-analysis, can be used to predict the number of casualties and their likely injury profile of survivors to guide the immediate response by the medical services and the workload in the coming days.
Adhérence des pansements 3 côtés: Pas tous équivalents
Adherence Evaluation of Vented Chest Seals in a Swine Skin model
Arnaud F. et Al. Injury doi:10.1016/j.injury.2016.05.041
----------------------------------
L'adhérence cutanée est une caractéristique importante des pansements 3 côtés industriels. A l'évidence il existe des différences. C'est ce que démontre ce travail particulièrement intéressant car il napporte également quelques informations sur les effets de la température de stockage sur ces dispositifs. Une remarque: la peau est celle de cochons (lire aussi ce travail non publié)
----------------------------------
Objectives
Perforation of the chest (open pneumothorax) with and without lung injury can cause air accumulation in the chest, positive intrapleural pressure and lead to tension pneumothorax if untreated. The performance of chest seals to prevent tension physiology depends partially on their ability to adhere to the skin and seal the chest wound. Novel non-occlusive vented chest seals were assessed for their adhesiveness on skin of live swine under normal and extreme environmental conditions to simulate austere battlefield conditions.
Methods
Chest seals were applied on the back of the swine on skin that was soiled by various environmental contaminants to represent battlefield situations. A peeling (horizontal rim peeling) and detachment and breaching (vertical pulling) techniques were used to quantify the adhesive performance of vented chest seals. Among eight initially selected vented seals, five (Bolin, Russell, Fast breathe, Hyfin and SAM) were further down-selected based on their superior adherence scores at ambient temperatures. The adherence of these seals was then assessed after approximately 17 h storage at extreme cold (-19.5 °C) and hot (71.5 °C) temperatures.
Results
Adherence scores for peeling (above 90%) and detachment scores (less than 25%) were comparable for four vented chest seals when tested at ambient temperature, except for the Bolin seal which had higher breaching. Under extreme storage temperatures, adherence peeling scores were comparable to those at ambient temperatures for four chest seals.
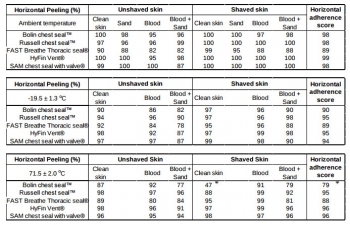
Scores were significantly lower for the Bolin seal at extreme temperatures. This seal also had the highest detachment and breaching scores. In contrast, the Russell, Fast breathe, Hyfin and SAM seals showed similar ability to stay air tight without breaching after hot storage.
Conclusion
No significant difference was found in skin adherence of the five vented chest seals at ambient temperature and the four seals (Russell, Fast breathe, Hyfin and SAM) maintained superior adherence even after exposure to extreme temperatures compared to the Bolin. To select the most effective product from the 5 selected vented chest seals, further functional evaluation of the valve of these chest seals on a chest wound with the potential for tension in the pneumothorax or hemopneumothorax is warranted.
Echographie pour l'intubation: Plutôt oui.
Tracheal ultrasonography and ultrasonographic lung sliding for confirming endotracheal tube placement: Speed and Reliability
BACKGROUND:
In this study we aimed to evaluate the success of ultrasonography (USG) for confirming the tube placement and timeliness by tracheal USG and ultrasonographic lung sliding in resuscitation and rapid sequence intubation.
MATERIALS AND METHODS:
This study was a prospective, single-center, observational study conducted in the emergency department of a tertiary care hospital. Patients were prospectively enrolled in the study. Patients who went under emergency intubation because of respiratory failure, cardiac arrest or severe trauma included in the study. Patients with severe neck trauma, neck tumors, history of neck operation or tracheotomy and under 18years old were excluded from the study.
RESULTS:
A total of 115 patients included in the study. The mean age was 67.2±17.1 with age 16-95years old. Among 115 patients 30 were cardiac arrest patients other 85 patients were non-cardiac arrest patients intubated with rapid sequence intubation. The overall accuracy of the ultrasonography was 97.18% (95% CI, 90.19-99.66%), and the value of kappa was 0.869 (95% CI, 0.77-0.96), indicating a high degree of agreement between the ultrasonography and capnography. The ulrasonography took significantly less time than capnography in total.
DISCUSSION:
Ultrasonography achieved high sensitivity and specificity for confirming tube placement and results faster than end-tidal carbon dioxide. Ultrasonography is a good alternative for confirming the endotracheal tube placement. Future studies should examine the use of ultrasonography as a method for real-time assessment of endotracheal tube placement by emergency physicians with only basic ultrasonographic training.
| Tags : airway, échographie
04/06/2016
European guideline on management of major bleeding / Trauma
The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition
Rossaint et al. Critical Care (2016) 20:100
Background: Severe trauma continues to represent a global public health issue and mortality and morbidity in trauma patients remains substantial. A number of initiatives have aimed to provide guidance on the management of trauma patients. This document focuses on the management of major bleeding and coagulopathy following trauma and encourages adaptation of the guiding principles to each local situation and implementation within each institution.
Methods: The pan-European, multidisciplinary Task Force for Advanced Bleeding Care in Trauma was founded in 2004 and included representatives of six relevant European professional societies. The group used a structured, evidence-based consensus approach to address scientific queries that served as the basis for each recommendation and supporting rationale. Expert opinion and current clinical practice were also considered, particularly in areas in which randomised clinical trials have not or cannot be performed. Existing recommendations were reconsidered and revised based on new scientific evidence and observed shifts in clinical practice; new recommendations were formulated to reflect current clinical concerns and areas in which new research data have been generated. This guideline represents the fourth edition of a document first published in 2007 and updated in 2010 and 2013.
Results: The guideline now recommends that patients be transferred directly to an appropriate trauma treatment centre and encourages use of a restricted volume replacement strategy during initial resuscitation. Best-practice use of blood products during further resuscitation continues to evolve and should be guided by a goal-directed strategy. The identification and management of patients pre-treated with anticoagulant agents continues to pose a real challenge, despite accumulating experience and awareness. The present guideline should be viewed as an educational aid to improve and standardise the care of the bleeding trauma patients across Europe and beyond. This document may also serve as a basis for local implementation. Furthermore, local quality and safety management systems need to be established to specifically assess key measures of bleeding control and outcome.
Conclusions: A multidisciplinary approach and adherence to evidence-based guidance are key to improving patient outcomes. The implementation of locally
PLyo: Une révolution ? Pas vraiment, une redécouverte
Pusateri AE et Al. Transfusion. 2016 Apr;56 Suppl 2:S128-39
------------------------------------------
Les nouvelles modalités de transfusion mettent en avant le bénéfice de l'apport précoce de plasma. Les contraintes logistiques liées à l'emploi de plasma frais sont réelles. L'emploi de plasma lyophilisé permet de raccourcir ce délai et peut représenter dans certaines conditions d'isolement la seule source disponibles de fractions coagulantes. Le plasma lyophylisé est un vieux monsieur, mais dont la place est fondamentale. Largement utilisé notamment par l'armée française pendant la guerre d'indocchine, le SSA a maintenu sa production jusqu'à ce que l'épidémie de VIH ne survienne. Depuis les années 1980, le SSA a travaillé sans relâche pour sécuriser un produit qui retrouve la place qui lui est due dans la stratégie transfusionnelle du blessé de guerre (1) Il s'agit donc d'une redécouverte avec un emploi effectif en opération dès 1996 (2), plutôt que de révolution. Le document proposé à la lecture fait le point sur cette historique et les développements à venir. La lecture de ce document ne doit pas faire oublier la réflexion de plus en plus présente sur l'emploi en situation d'isolement de l'intérêt de la transfusion de sang total, seule source de plaquettes, associé au recours à des fractions coagulantes comme le fibrinogène et les complexes prothrombiques. Une telle association représente probablement l'avenir de la réanimation hémostatique préhospitalière (3, 4).
------------------------------------------
Historical dried plasma development Event Selected References
1930s Plasma lyophilization developed in the 1930s.
1940—Large scale production of pooled, lyophilized plasma by both the US and British established for war time use (to meet logistical constraints of whole blood and frozen/liquid plasma).ans les années
1941—Spray dried plasma produced for the Swedish Defense Department. 21 WWII Production 20-22 British produced >500,000 U lyophilized plasma during WWII. US produced >6,000,000 U lyophilized plasma during WWII. US/British distributed world-wide. Sweden produced approximately 17,000 U spray dried plasma for Sweden and Finland.
1945—Hepatitis 23 Hepatitis as a result of plasma transfusion recognized by the end of WWII. Believed that benefits outweighed the risk.
1945-1952—Hepatitis 24 Attempts at pathogen reduction and reducing pool size not successful. Several deaths in clinical studies of ultraviolet irradiated pooled plasma.
1953
—Department of the Army (Circular 73) directed that, because of the risk of serum hepatitis, the higher cost, and the need to use it for the production of specific globulins, plasma would not be used “to support blood volume” unless dextran was not available.
—Serum albumin replaced plasma as primary resuscitative product for US Forces in Korea.
1968—National Research Council Committee on Plasma and Plasma Substitutes recommended that “the use of whole, pooled human plasma be discouraged and even discontinued unless a clear cut case can be made for its unique requirements.”
The French Military Blood Institute produced dried plasma from 1949 to 1984, and provided over 40,000 units to French military forces during the Indochina War. In 1985, production was discontinued due to risk of HIV infection.
| Tags : coagulopathie, transfusion
Acide tranexaminique systématique: La roue tournerait-elle ?
Acute Fibrinolysis Shutdown after Injury Occurs Frequently and Increases Mortality: A Multicenter Evaluation of 2,540 Severely Injured Patients
Moore HB et Al. J Am Coll Surg. 2016 Apr;222(4):347-55.
------------------------------------------------------
La recommandation n°15 de la RFE Portant sur la réanimation du choc hémorragique stipule qu' il est recommandé d'administrer de l'acide tranexamique dès que possible chez les patients traumatisés à la dose de 1 g en bolus intraveineux en 10 min suivi de 1 g perfusé sur 8 h chez les patients traumatisés. Cette administration ne doit pas être initiée au delà de la 3e heure suivant la survenue d'un traumatisme avec choc hémorragique. Si l'étude CRASH-2 a montré que l'acide tranexamique réduisait significativement la mortalité. De nouvelles données disponibles depuis alimentent la discussion (1). Trois états du système de fibrinolyse peuvent être retrouvés: normal, hyperfibrinolyse, inhibition Les deux derniers sont associés à une surmortalité mais la fréquence des états d'inhibition de l'inhibition ne plaiderait pas pour une administration systématique mais ciblée d'exacyl. En qui nous concerne il faut à nouveau insister sur la précocité de l'administration d'exacyl dans l'heure chez les blessés sévères, pour lesquels le bénéfice en terme de mortalité est le plus grand (2). Une réflexion pour un emploi optimisé est en MARCHE (3, 4)
------------------------------------------------------
BACKGROUND:
Fibrinolysis is a physiologic process that maintains microvascular patency by breaking down excessive fibrin clot. Hyperfibrinolysis is associated with a doubling of mortality. Fibrinolysis shutdown, an acute impairment of fibrinolysis, has been recognized as a risk factor for increased mortality. The purpose of this study was to assess the incidence and outcomes of fibrinolysis phenotypes in 2 urban trauma centers.
STUDY DESIGN:
Injured patients included in the analysis were admitted between 2010 and 2013, were 18 years of age or older, and had an Injury Severity Score (ISS) > 15. Admission fibrinolysis phenotypes were determined by the clot lysis at 30 minutes (LY30): shutdown ≤ 0.8%, physiologic 0.9% to 2.9%, and hyperfibrinolysis ≥ 3%. Logistic regression was used to adjust for age, arrival blood pressure, ISS, mechanism, and facility.
RESULTS:
There were 2,540 patients who met inclusion criteria. Median age was 39 years (interquartile range [IQR] 26 to 55 years) and median ISS was 25 (IQR 20 to 33), with a mortality rate of 21%. Fibrinolysis shutdown was the most common phenotype (46%) followed by physiologic (36%) and hyperfibrinolysis (18%). Hyperfibrinolysis was associated with the highest death rate (34%), followed by shutdown (22%), and physiologic (14%, p < 0.001). The risk of mortality remained increased for hyperfibrinolysis (odds ratio [OR] 3.3, 95% CI 2.4 to 4.6, p < 0.0001) and shutdown (OR 1.6, 95% CI 1.3 to 2.1, p = 0.0003) compared with physiologic when adjusting for age, ISS, mechanism, head injury, and blood pressure (area under the receiver operating characteristics curve 0.82, 95% CI 0.80 to 0.84).
CONCLUSIONS:
Fibrinolysis shutdown is the most common phenotype on admission and is associated with increased mortality. These data provide additional evidence of distinct phenotypes of coagulation impairment and that individualized hemostatic therapy may be required.
| Tags : coagulopathie
03/06/2016
The 2015 Remote Damage Control Resuscitation Symposium
| Tags : transfusion, coagulopathie