12/05/2016
Crico: Incisez large
The inaccuracy of using landmark techniques for cricothyroid membrane identification: a comparison of three techniques
Bair AE et Al. Acad Emerg Med 2015 Aug; 22:908
---------------------------------------------------------
Le recours à la coniotomie est rare mais il s'agit d'un geste technique à connaître pour la prise en charge des obstructions des voies aériennes. Le repérage de la membrane crio-thyroïdienne peut être difficile. Ce travail rappelle que l'identification manuelle de cette dernière est fiable dans moins de 60 % des cas. L'échographie améliorerait la fiabilité de cette localisation (Campbell M et Al. 1) mais ceci n'est pas, et c'est surprenant, retrouvé par tous (Yldiz G et Al. 2). En ce qui nous concerne, la disponibilité d'un appareil d'échographie sur le terrain est peu probable . En cas de difficulté de repérage pensez à réaliser une incision large pour repérer au doigt directement cette membrane (regardez cette vidéo)
---------------------------------------------------------
OBJECTIVES:
Successful cricothyrotomy is predicated on accurate identification of the cricothyroid membrane (CTM) by palpation of superficial anatomy. However, recent research has indicated that accuracy of the identification of the CTM can be as low as 30%, even in the hands of skilled providers. To date, there are very little data to suggest how to best identify this critical landmark. The objective was to compare three different methods of identifying the CTM.
METHODS:
A convenience sample of patients and physician volunteers who met inclusion criteria was consented. The patients were assessed by physician volunteers who were randomized to one of three methods for identifying the CTM (general palpation of landmarks vs. an approximation based on four finger widths vs. an estimation based on overlying skin creases of the neck). Volunteers would then mark the skin with an invisible but florescent pen. A single expert evaluator used ultrasound to identify the superior and inferior borders of the CTM. The variably colored florescent marks were then visualized with ultraviolet light and the accuracy of the various methods was recorded as the primary outcome. Additionally, the time it took to perform each technique was measured. Descriptive statistics and report 95% confidence intervals (CIs) are reported.
RESULTS:
Fifty adult patients were enrolled, 52% were female, and mean body mass index was 28 kg/m(2) (95% CI = 26 to 29 kg/m(2) ). The general palpation method was successful 62% of the time (95% CI = 48% to 76%) and took an average of 14 seconds to perform (range = 5 to 45 seconds). In contrast, the four-finger technique was successful 46% of the time (95% CI = 32% to 60%) and took an average of 12 seconds to perform (range = 6 to 40 seconds). Finally, the neck crease method was successful 50% of the time (95% CI = 36% to 64%) and took an average of 11 seconds to perform (range = 5 to 15 seconds).
CONCLUSIONS:
All three methods performed poorly overall. All three techniques might potentially be even less accurate in instances where the superficial anatomy is not palpable due to body habitus. These findings should alert clinicians to the significant risk of a misplaced cricothyrotomy and highlight the critical need for future research.
08/05/2016
la voie axillaire +++
Chest wall thickness and decompression failure: A systematic review and meta-analysis comparing anatomic locations in needle thoracostomy
Laan DV et Al. Injury, Int. J. Care Injured 47 (2016) 797–804
------------------------------------------
Une publication, une de plus, qui met en avant l'abord axillaire pour la décompression thoracique et qui insiste sur le peu de preuve de l'inocuité des cathéters de 8 cm. On rappelle que la thoracostomie au doigt reste la référence.
------------------------------------------
Introduction:
Current Advanced Trauma Life Support guidelines recommend decompression for thoracic tension physiology using a 5-cm angiocatheter at the second intercostal space (ICS) on the midclavicular line (MCL). High failure rates occur. Through systematic review and meta-analysis, we aimed to determine the chest wall thickness (CWT) of the 2nd ICS-MCL, the 4th/5th ICS at the anterior axillary line (AAL), the 4th/5th ICS mid axillary line (MAL) and needle thoracostomy failure rates using the currently recommended 5-cm angiocatheter.
Methods:
A comprehensive search of several databases from their inception to July 24, 2014 was conducted. The search was limited to the English language, and all study populations were included. Studies were appraised by two independent reviewers according to a priori defined PRISMA inclusion and exclusion criteria. Continuous outcomes (CWT) were evaluated using weighted mean difference and binary outcomes (failure with 5-cm needle) were assessed using incidence rate. Outcomes were pooled using the random-effects model.
Results:
The search resulted in 34,652 studies of which 15 were included for CWT analysis, 13 for NT effectiveness. Mean CWT was 42.79 mm (95% CI, 38.78–46.81) at 2nd ICS-MCL, 39.85 mm (95% CI, 28.70–51.00) at MAL, and 34.33 mm (95% CI, 28.20–40.47) at AAL (P = .08). Mean failure rate was 38% (95% CI, 24–54) at 2nd ICS-MCL, 31% (95% CI, 10–64) at MAL, and 13% (95% CI, 8–22) at AAL (P = .01).
Conclusion:
Evidence from observational studies suggests that the 4th/5th ICS-AAL has the lowest predicted failure rate of needle decompression in multiple populations.
| Tags : pneumothorax, exsufflation
01/05/2016
Albumine aussi bien que PFC ?
Influences of Limited Resuscitation with Plasma or Plasma Protein Solutions on Hemostasis and Survival of Rabbits with Non-Compressible Hemorrhage
J Trauma Acute Care Surg. 2016 Apr 27. Kheirabadi BS et Al.
BACKGROUND:
Plasma infusion with or without RBC is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
Anesthetized spontaneously breathing rabbits (3.3±0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 min with Plasma-Lyte (PAL; 30 ml/kg), PAL+ fibrinogen (PAL+F; 30ml+100mg/kg), fresh rabbit plasma (PLS; 15ml/kg), or 25% albumin (ALB; 5 ml/kg) solution; all given in two bolus IV injections (15 min apart) to achieve a MAP of 65 mmHg, n=8-9/group. Animals were monitored for 2 hrs or until death and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 min. At 60 min post-injury, MAP was higher with albumin than with crystalloids (PAL or PAL+F), but shock indices were not different despite the large differences in resuscitation volumes.
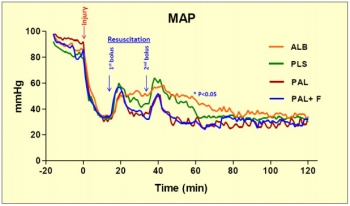
Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein, and increased survival rate to 100% (p<.05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSION:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate, however, its effects did not differ from those obtained with 25% albumin at 1/3 of the volume. The albumin advantage was consistent with our previous findings in which 5% albumin was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its albumin content rather than its coagulation proteins
| Tags : remplissage
