31/07/2016
Kétamine: Moins performant après !
Comparison of the effects of ketamine and morphine on performance of representative military tasks
Gaydos SJ et Al. J Emerg Med. 2015 Mar;48(3):313-24
BACKGROUND:
When providing care under combat or hostile conditions, it may be necessary for a casualty to remain engaged in military tasks after being wounded. Prehospital care under other remote, austere conditions may be similar, whereby an individual may be forced to continue purposeful actions despite traumatic injury. Given the adverse side-effect profile of intramuscular (i.m.) morphine, alternative analgesics and routes of administration are of interest. Ketamine may be of value in this capacity.
OBJECTIVES:
To delineate performance decrements in basic soldier tasks comparing the effects of the standard battlefield analgesic (10 mg i.m. morphine) with 25 mg i.m. ketamine.
METHODS:
Representative military skills and risk propensity were tested in 48 healthy volunteers without pain stimuli in a double-blind, placebo-controlled, crossover design.
RESULTS:
Overall, participants reported more symptoms associated with ketamine vs. morphine and placebo, chiefly dizziness, poor concentration, and feelings of happiness. Performance decrements on ketamine, when present, manifested as slower performance times rather than procedural errors.
CONCLUSIONS:
Participants were more symptomatic with ketamine, yet the soldier skills were largely resistant to performance decrements, suggesting that a trained task skill (autonomous phase) remains somewhat resilient to the drugged state at this dosage. The performance decrements with ketamine may represent the subjects' adoption of a cautious posture, as suggested by risk propensity testing whereby the subject is aware of impairment, trading speed for preservation of task accuracy. These results will help to inform the casualty care community regarding appropriate use of ketamine as an alternative or opioid-sparing battlefield analgesic.
Revue du CIMM/ICMM
30/07/2016
Gardes en SAU militaires: Utiles pour l'OPEX, pas sûr !
26/07/2016
Documentation médicale OTAN
24/07/2016
Pansement de plaie thoracique SC1
Gueules cassées: Albéric Pont, un lyonnais oublié
| Tags : maxillo
Trauma Cervico-faciaux de guerre
23/07/2016
Moins d'expérience ? Alors la conio chirurgicale
Emergency Cricothyrotomy Performed by Surgical Airway–naive Medical Personnel
Heymans F. et Al. Anesthesiology 2016; 125:295-303
BACKGROUND:
When conventional approaches to obtain effective ventilation and return of effective spontaneous breathing fail, surgical airway is the last rescue option. Most physicians have a limited lifetime experience with cricothyrotomy, and it is unclear what method should be taught for this lifesaving procedure. The aim of this study is to compare the performance of medical personnel, naive to surgical airway techniques, in establishing an emergency surgical airway in cadavers using three commonly used cricothyrotomy techniques.
METHODS:
Twenty medical students, without previous knowledge of surgical airway techniques, were randomly selected from their class. After training, they performed cricothyrotomy by three techniques (surgical, Melker, and QuickTrach II) in a random order on 60 cadavers with comparable biometrics. The time to complete the procedure, rate of success, and number of complications were recorded. A success was defined as the correct placement of the cannula within the trachea in 3 min.
RESULTS:
The success rates were 95, 55, and 50% for surgical cricothyrotomy, QuickTrach, and Melker, respectively (P = 0.025). The majority of failures were due to cannula misplacement (15 of 20). In successful procedures, the mean procedure time was 94 ± 35 s in the surgical group, 77 ± 34 in the QuickTrach II group, and 149 ± 24 in the Melker group (P < 0.001). Few significant complications were found in successful procedures. No cadaver biometric parameters were correlated with success of the procedure.
| Surgical Technique | QuickTrach II | Melker | ||
| Success rate (%)) ) | 19 (95 | 11 (55) | 10 (50 | 0.025 |
| Failure due to time limitation (%) | 0 | 1 (5) | 4 (20) | 0.203 |
| Incorrect placement (%) | 1 (5) | 8 (40) ) | 6 (30) | 0.106 |
| Cricothyrotomy time over 3 min | 0 | 3 | 6 | 0.257 |
| Time to complete the procedure—mean (s) | 94±35 | 149±24 | < 0.001 | |
| Total complications in successful procedures | 1 | 4 | 1 | 0.018 |
| SPC: posterior tracheal wall lesion | 1 | 3 | 1 | |
| SPC: esophageal perforation 1 | 10 (50 | |||
| Total complications in failed procedures | 1 | 8 | 6 | 0.205 |
| FPC: esophageal intubation | 1 | 2 | 1 | |
| FPC: pretracheal false passage | 4 | 3 | ||
| FPC: cannula in pharynx 1 2 | 1 | 2 | ||
| FPC: broken device 1 | 1 | |||
| FPC = failed procedure complications; SPC = successful procedure complications. |
"....In conclusion, our results indicate that medical personnel naive to surgical airway techniques establish a surgical airway more efficiently using surgical cricothyroidotomy. Since the vast majority of clinicians perform emergency airway infrequently, our observation might apply to the majority of them. Whether surgical cricothyrotomy remains superior in advance-trained medical personnel requires further study......"
CONCLUSION:
Surgical airway-naive medical personnel establish emergency cricothyrotomy more efficiently and safely with the surgical procedure than with the other two commonly used techniques.
| Tags : airway
22/07/2016
De l'usage d'une chèche
Nombre de militaires l'ont adopté car elle protège du soleil, du vent du sable. Tout ceci est connu de longue date notamment des sahariens.
Mais une chèche c'est aussi ET SURTOUT ce qui permet de réaliser une stabilisation pelvienne, un garrot de fortune,un packing de plaie, une immobilisation de fortune, .....
La chèche un équipement important dans le cadre du sauvetage au combat.
Pour vous en convaincre lisez ce document
Et en plus faites une bonne action
19/07/2016
Expérience des armées de la simulation en santé de crise
| Tags : simulateurs
14/07/2016
Soleil et chaleur: plutôt gênant
Prehospital Endotracheal Intubation in Warm Climates: Caution is Required
-------------------------------------------------
Une chose bien connue et très clairement explicitée:
-------------------------------------------------
BACKGROUND:
Out-of-hospital endotracheal intubation is a frequent procedure for trauma care. Nevertheless, in warm climates, sunlight and heat can interfere with the flow of the usual procedure. They can affect the equipment and hinder the operator. There are few data on this issue. The presentation of this case highlights three common complications that may occur when intubating under a hot and bright sun.
CASE REPORT:
A 23-year-old man had a car accident in Djibouti, at 11:00 a.m., in broad sunlight. The heat was scorching. Due to a severe head trauma, with a Glasgow Coma Scale score of 8, it was decided to perform an endotracheal intubation. The operator faced three problems: the difficulty of seeing inside the mouth in the bright sunlight, the softening of the tube under the influence of the heat, and the inefficiency of colorimetric CO2 detectors in the warm atmosphere in confirming the proper endotracheal tube placement.
WHY SHOULD AN EMERGENCY PHYSICIAN BE AWARE OF THIS?:
Solutions are simple, but must be known and planned ahead, prior to beginning the procedure: Putting a jacket over his head while doing the laryngoscopy would solve the problem of dazzle; adjuncts like a stylet or gum elastic bougie have to be used at the outset to fix the softening problem; alternative methods to exhaled CO2 detection, such as the syringe aspiration technique, to confirm the proper tube placement, should be available.
Epaule luxée: Technique de Sool
The effectiveness of a newly developed reduction method of anterior shoulder dislocations; Sool's method
Park MS et Al. Am J Emerg Med. 2016 Apr 9. pii: S0735-6757(16)30036-5. doi: 10.1016/j.ajem.2016.04.01
OBJECTIVE:
Nearly a dozen reduction methods for the treatment of anterior shoulder dislocation have been reported, but the majority are painful and require patients to be in the supine or prone position.
METHODS:
This retrospective cohort study was conducted in a university-affiliated emergency department (ED). Sool's method and traditional shoulder reduction methods (TSRMs) were performed for the patient with anterior shoulder dislocation. Fifty-nine eligible patients were recruited; 35 were treated with TSRMs, wherease 24 were treated with Sool's method.
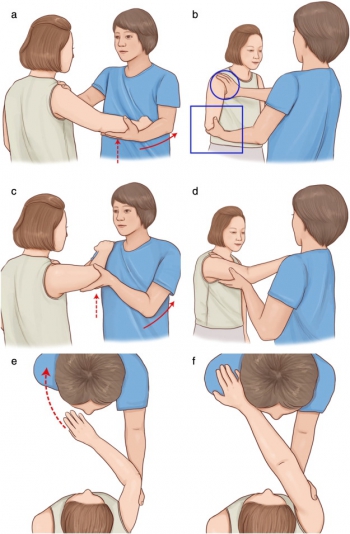
clic sur l'image pour voir une vidéo
RESULTS:
The rate of successful reduction was 80% (26/35) in the TSRM group and 75% (18/24) in the Sool's method group (P=.75). The length of stay in the ED was 72.3minutes in the Sool's method group and 98.4minutes in the TSRM group (P=.037). No significant difference was observed between the neurovascular deficit before and after reduction in either group. The procedural time of successfully reduced cases in patients treated by Sool's method was shorter than that of the failed cases (P=.015).
CONCLUSIONS:
Sool's method was as successful as other methods at reducing shoulder dislocation and has demonstrated encouraging results, including significant reduction in length of stay in the ED and unnecessary use of sedation. Sool's method is technically easy and requires only a place to sit and a single operator.
09/07/2016
Intubation préhospitalière: Oui, mais mieux vaut être pratiquant
Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians
Lockey D. et Al. British Journal of Anaesthesia 113 (2): 220–5 (2014)
-------------------------------
L'idée globale de cet article est que concernant la gestion des voies aériennes en préhospitalier, plus on est pratiquant et plus les situations de gestion difficile sont moins fréquentes, mais que le recours à un abord chirurgical reste une éventualité à laquelle se préparer. Dans ce travail, ce recours est particulièrement fréquent dans les traumas de la face et chez les brûlés.
-------------------------------
Background. Effective airway management is a priority in early trauma management. Data on physician pre-hospital tracheal intubation are limited; this study was performed to establish the success rate for tracheal intubation in a physician-led system and examine the management of failed intubation and emergency surgical cricothyroidotomy in pre-hospital trauma patients. Failed intubation rates for anaesthetists and non-anaesthetists were compared.
Methods. A retrospective database review was conducted to identify trauma patients undergoing pre-hospital advanced airway management between September 1991 and December 2012. The success rate of tracheal intubation and the use and success of rescue techniques were established. Success rates of tracheal intubation by individuals and by speciality were recorded.
Results. The doctor–paramedic team attended 28 939 patients; 7256 (25.1%) required advanced airway management. A surgical airway was performed immediately, without attempted laryngoscopy, in 46 patients (0.6%). Tracheal intubation was successful in 7158 patients (99.3%). Rescue surgical airways were performed in 42 patients, seven had successful insertion of supraglottic devices, and two patients had supraglottic device insertion and a surgical airway. One patient breathed spontaneously with bag-valve-mask support during transfer. All rescue techniques were successful. Non-anaesthetists performed 4394 intubations and failed to intubate in 41 cases (0.9%); anaesthetists performed 2587 intubations and failed in 11 (0.4%) (P¼0.02).
Conclusions. This is the largest series of physician pre-hospital tracheal intubation; the success rate of 99.3% is consistent with other reported data. All rescue airways were successful. Non-anaesthetists were twice as likely to have to perform a rescue airway intervention than anaesthetists. Surgical airway rates reported here (0.7%) are lower than most other physician-led series (median 3.1%, range 0.1–7.7%).
08/07/2016
Coniotomie: Plaidoyer UK pour la chirurgie
The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective
Tyle T et Al. J R Army Med Corps. 2016 Jun 6. pii: jramc-2016-000637. doi: 10.1136/jramc-2016-000637
-----------------------------------------------
Un geste peu fréquent: 86 blessés sur une période de 8 ans et pourtant un geste essentiel à maîtriser. Faire simple est mieux. Pour cela pas besoin d'être chirurgien, urgentiste ou anesthésiste-réanimateur.
-----------------------------------------------
BACKGROUND:
The insertion of a surgical airway in the presence of severe airway compromise is an uncommon occurrence in everyday civilian practice. In conflict, the requirement for insertion of a surgical airway is more common. Recent military operations in Afghanistan resulted in large numbers of severely injured patients, and a significant proportion required definitive airway management through the insertion of a surgical airway.
OBJECTIVE:
To examine the procedural success and survival rate to discharge from a military hospital over an 8-year period.
METHODS:
A retrospective database and chart review was conducted, using the UK Joint Theatre Trauma Registry and the Central Health Records Library. Patients who underwent surgical airway insertion by UK medical personnel from 2006 to 2014 were included. Procedural success, demographics, Injury Severity Score, practitioner experience and patient survival data were collected. Descriptive statistics were used for data comparison, and statistical significance was defined as p<0.05.
RESULTS:
86 patients met the inclusion criterion and were included in the final analysis. The mean patient age was 25 years, (SD 5), with a median ISS of 62.5 (IQR 42). 79 (92%) of all surgical airways were successfully inserted. 7 (8%) were either inserted incorrectly or failed to perform adequately. 80 (93%) of these procedures were performed either by combat medical technicians or General Duties Medical Officers (GDMOs) at the point of wounding or Role 1. 6 (7%) were performed by the Medical Emergency Response Team. 21 (24%) patients survived to hospital discharge.
DISCUSSION:
Surgical airways can be successfully performed in the most hostile of environments with high success rates by combat medical technicians and GDMOs. These results compare favourably with US military data published from the same conflict.
| Tags : airway, coniotomie
01/07/2016
U.K. Military Burns 2008–2013
Epidemiology of U.K. Military Burns 2008–2013
J Burn Care Res. 2016 Jun 2. [Epub ahead of print]
After sustaining burn injuries overseas, U.K. Armed Forces personnel are evacuated to the Royal Centre for Defence Medicine. The objective was to review the etiology of U.K. Military burns managed at the center between 2008 and 2013. Analysis will aid provision planning and assist in the prevention of burn injuries for future tours. The International Burn Injury Database database of all U.K. Armed Forces burn injured patients evacuated to the Queen Elizabeth University Hospital Birmingham between 2008 and 2013 were reviewed retrospectively. Analysis included patient demographics, injury mechanism, burn severity, management, and mortality. There were 65 military personnel with burn injuries requiring repatriation to the United Kingdom. Percentage of 78.5 were sustained in Afghanistan. The mean age was 25 (18–46) years. Percentage of 70.8 were considered noncombat burn injuries. Of the noncombat burns, the mechanism of injury most commonly involved burning waste and misuse of fuels and scalds.
| Combat | |
| Improvised explosive device | 10 |
| Unintentional detonation of ammunition | 3 |
| Rocket propelled grenade | 2 |
| Mini-flare fired into face | 1 |
| Explosion during training | 1 |
| Thermal injury from fired bullet | 1 |
| White phosphorus flame burn | 1 |
| Non combat | |
| Misuse of fuel | 11 |
| Burning waste | 7 |
| Cooking | 4 |
| Others | 16 |
| Total | 65 |
"...One fifth of all patients sustained associated injuries, of which 88.3% were personnel with combat burns. Associated injuries included complex fractures,
tympanic injuries, ophthalmic injury, spinal injury, lung contusions, a gunshot wound to the upper limb and a gunshot wound causing an intracranial hemorrhage. One patient required bilateral lower limb amputations. In addition, two patients sustained an associated inhalation injury..."
The mean TBSA for all patients was 6% (0.05–51%). Areas most commonly affected included arms, legs, and face. The length of hospital stay for combat vs noncombat burn injury patients was 10 vs 7 days. There were no fatalities. In conclusion, substantially fewer military personnel sustained combat burns between 2008 and 2013 than in preceding study period (19 vs 79). The number of accidental noncombat burns remained constant. The decrease in combat burns may reflect a relative decrease in military intensity and effective protective equipment and safety measures. Further education may allow for an additional decrease in preventable burn injuries.
| Tags : brûlure