24/11/2013
Pratique chirurgicale de base dans les structures à moyens limités.
Garrot abdominal: Une paire de main et des bras musclés
Temporization of Penetrating Abdominal-Pelvic Trauma With Manual External Aortic Compression: A Novel Case Report
Douma M et Al. Ann Emerg Med. 2013 Oct 23. pii: S0196-0644(13)01452-2
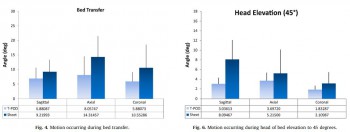
La prise en charge des traumatismes vasculaires de l'abdomen, du pelvis et des membres nécessite une intervention chirurgicale rapide. Il est dans ces cas nécessaire de tarir sinon de réduire le débit de saignement de telle sorte que le blessé arrive vivant dans la structure adaptée (1). Ceci est difficile quand les lésions ne sont pas ou difficilement garrotables notamment lors de traumatismes jonctionnels. Des équipements spécifiques ont été développé pour assurer une compression en amont des lésions et permettre de réduire ces débits de saignements. Ces dispositifs présenté par ailleurs (2, 3 , 4) n'ont pas encore fait leur preuve même si des rapports isolés en soulignent l'intérêt. Certains comme les pantalons antichocs sont considérés comme ayant peu d'indications du moins mal cernées (5) . Ces équipements sont rarement disponibles.
Pourtant la compression abdominale bi-manuelle est possible et en fait connue depuis longtemps notamment en obstétrique sous forme de compression utérine bi-manuelle (6, 7, 8).
C'est ce qu'illustre le cas clinique présenté. Il existe bien sûr des facteurs limitant comme la corpulence aussi bien du blessé que du sauveteur. Il faut en effet exercer une pression abdominale de l'ordre de 40 kg pour occlure l'aorte abdominal (9).
| Tags : hémorragie, garrot
23/11/2013
Hypothermie: Isoler étanche même mouillé est efficace !
Protection against Cold in Prehospital Care: Evaporative Heat Loss Reduction by Wet Clothing Removal or the Addition of a Vapor Barrier—A Thermal Manikin Study
Henriksson O. et Al. Prehosp Disaster Med 2012;26(6):1–6
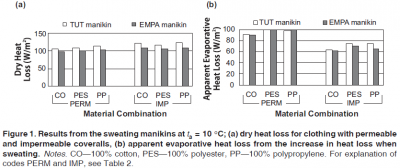
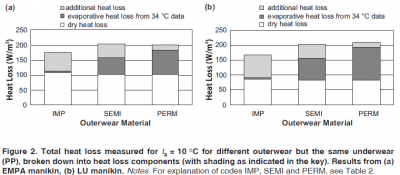
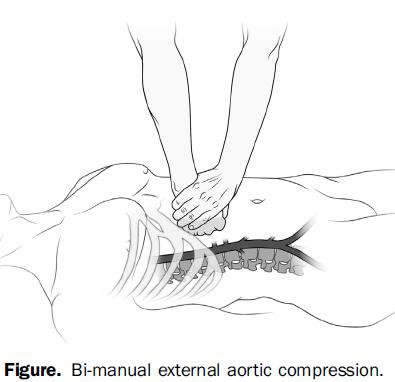
Le travail présenté met en exergue les points suivants:
1. Le fait d'envelopper un organisme dans un contenant limite les pertes thermiques par évaporation .
2 Il est meilleur de multiplier les couches d'isolation.
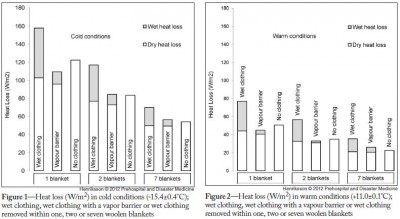
Il est fondamental que cet isolement soit parfaitement ETANCHE à l'air.
On rappelle que le principe de l'oignon (technique de hibbler)
1. La mise en place d'un écran interne au contact du blessé pour réduire les pertes thermiques par RADIATION (pertes thermiques par émission de rayonnement infrarouge, 50%des pertes) et par EVAPORATION (perte de calorie liée au changement d'état des molécules d'eau) (cutanée: 22 % des pertes et également respiratoire: 10 % des pertes) ainsi qu'en en protégeant les couches externes d'isolation de la transpiration et ou des défécations qui pourraient alors majorer les pertes par conduction. Ex: Une couverture de survie.
2. L'emballage par au moins 2 couches d'isolation interne pour permettre d'emmagasiner de la châleur. Ex: un sac de couchage ou des couvertures.
3. La mise en place de chaufferettes sans contact direct avec la peau pour permettre un réchauffement externe sans occasionner de brûlures cutanées.
4. Une couche externe étanche à la vapeur réduit les pertes par EVAPORATION en protégeant les couches internes d'isolation de l'eau externe (pluie, neige, humidité du sol) et réduit les pertes par CONVECTION (15 % des pertes, liée au vent. Ex une couverture de survie.
5. L'isolation du sol réduit les pertes par CONDUCTION (transfert de calories par contact direct entre deux corps, 3% des pertes ). Ex: un tapis de sol.
| Tags : hypothermie
21/11/2013
Le plasma lyophilisé: Bon pour le cerveau du traumatisé qui saigne
Early treatment with lyophilized plasma protects the brain in a large animal model of combined traumatic brain injury and hemorrhagic shock
Imam AM et Al. J Trauma Acute Care Surg. 2013;75: 976-983
accéder aux abstracts de la WTA publiés dans J trauma Acute care
_____________________________________
Bien sûr une étude animale, mais une de plus qui milite pour un emploi précoce du plasma lyophylisé.
_____________________________________
BACKGROUND: Combination of traumatic brain injury (TBI) and hemorrhagic shock (HS) can result in significant morbidity and mortality. We have previously shown that early administration of fresh frozen plasma (FFP) in a large animal model of TBI and HS reduces the size of the brain lesion as well as the associated edema. However, FFP is a perishable product that is not well suited for use in the austere prehospital settings. In this study, we tested whether a shelf-stable, low-volume, lyophilized plasma (LSP) product was as effective as FFP.
METHODS:
Yorkshire swine (42-50 kg) were instrumented to measure hemodynamic parameters, intracranial pressure, and brain tissue oxygenation. A prototype, computerized, cortical impact device was used to create TBI through a 20-mm craniotomy: 15-mm cylindrical tipimpactor at 4 m/s velocity, 100-millisecond dwell time, and 12-mm penetration depth. Volume-controlled hemorrhage was induced(40-45% total blood volume) concurrent with the TBI. After 2 hours of shock, animals were treated with (1) normal saline (NS, n = 5), (2) FFP (n = 5), and (3) LSP (n = 5). The volume of FFP and LSP matched the shed blood volume, whereas NS was 3 times the volume. Six hours after resuscitation, brains were sectioned and stained with TTC (2, 3, 5-Triphenyltetrazolium chloride), and lesion size (mm3) and swelling (percent change in volume compared with the contralateral, uninjured side) were measured.
RESULTS:
This protocol resulted in a highly reproducible brain injury, with clinically relevant changes in blood pressure, cardiac output, tissue hypoperfusion, intracranial pressure, and brain tissue oxygenation. Compared with NS, treatment with LSP significantly ( p G 0.05) decreased brain lesion size and swelling (51% and 54%, respectively).
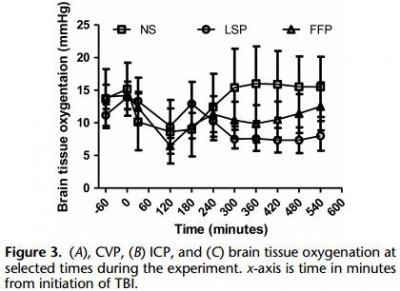
CONCLUSION: In a clinically realistic combined TBI + HS model, early administration of plasma products decreases brain lesion size and edema. LSP is as effective as FFP, while offering many logistic advantages.
| Tags : tbi, coagulopathie
18/11/2013
Hypothermie et vêtements humides
Dry and wet heat transfert through clothing dependent on the clothing properties under cold conditions
Richards GM et Al. Int J Occup Saf Ergon. 2008;14(1):69-76.
Il est recommandé lors de la prise en charge de blessés hypothermes de remplacer leurs vêtements humides par de vêtements secs. Ceci permettrait d'éviter l'aggravation de l'hypothermie secondaire à un transfert accru de châleur par conduction et par évaporation. Ceci est loin d'être toujours réalisable. Il convient dès lors de réaliser un isolement particulier du blessé basé sur latechnique de Hibler et dont la couche externe doit être ETANCHE à l'air. Ceci est connu depuis longtemps (ref ici). Le document proposé explique cela.
Une couche externe ETANCHE réduit les pertes thermiques évaporatives.
| Tags : hypothermie
16/11/2013
NAC après une explosion: Bon pour le neurone.
Amelioration of Acute Sequelae of Blast Induced Mild Traumatic Brain Injury by N-Acetyl Cysteine: A Double- Blind, Placebo Controlled Study
Hoffer ME et Al. PLoS One. 2013;8(1):e54163. doi: 10.1371/journal.pone.0054163. Epub 2013 Jan 23.
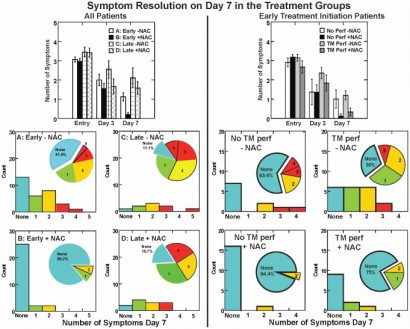
Background: Mild traumatic brain injury (mTBI) secondary to blast exposure is the most common battlefield injury in Southwest Asia. There has been little prospective work in the combat setting to test the efficacy of new countermeasures. The goal of this study was to compare the efficacy of N-acetyl cysteine (NAC) versus placebo on the symptoms associated with blast exposure mTBI in a combat setting.
Methods: This study was a randomized double blind, placebo-controlled study that was conducted on active duty service members at a forward deployed field hospital in Iraq. All symptomatic U.S. service members who were exposed to significant ordnance blast and who met the criteria for mTBI were offered participation in the study and 81 individuals agreed to participate. Individuals underwent a baseline evaluation and then were randomly assigned to receive either N- acetyl cysteine (NAC) or placebo for seven days.
4 g per os puis 18-24h après 2X2 g jusqu'à J4 puis 1,5 g X2 jusqu'à J7
Each subject was re-evaluated at 3 and 7 days. Outcome measures were the presence of the following sequelae of mTBI: dizziness, hearing loss, headache, memory loss, sleep disturbances, and neurocognitive dysfunction. The resolution of these symptoms seven days after the blast exposure was the main outcome measure in this study. Logistic regression on the outcome of ‘no day 7 symptoms’ indicated that NAC treatment was significantly better than placebo (OR = 3.6, p = 0.006). Secondary analysis revealed subjects receiving NAC within 24 hours of blast had an 86% chance of symptom resolution with no reported side effects versus 42% for those seen early who received placebo.
Conclusion: This study, conducted in an active theatre of war, demonstrates that NAC, a safe pharmaceutical countermeasure, has beneficial effects on the severity and resolution of sequelae of blast induced mTBI. This is the first demonstration of an effective short term countermeasure for mTBI. Further work on long term outcomes and the potential use of NAC in civilian mTBI is warranted
| Tags : blast
Retex US 2013: Le rapport du TCCC comitee
06/11/2013
Pansement compressif: Un nouveau venu
Il existe une grande variété de pansements compressifs. L'armée française utilise le pansement dit israélien de la société Persys Medical et le pansement Olaes modular bandage de la société TacMed Solutions. En plus des bandes de compression, d'autres dispositifs on fait leur apparition visant à contrôler les hémorragies par une compression plus proximale (le CROC, le tourniquet abdominal, le SAMTourniquet, le Junctional emergency treatment tool). Ces dispositifs ont recours à des dispositifs de compression. L'Aiwrap est un pansement compressif proche des pansements en dotation auquel est adjoint une vessie qui une fois gonflée va majorer de manière importante la compression sous le pansement. Son positionnement dans une gamme de produit reste à préciser.
| Tags : hémorragie, pansement
Oxygénation transtrachéale de sauvetage
Viable oxygenation with cannula-overneedle cricothyrotomy for asphyxial airway occlusion
Kofke WA et Al. Br. J. Anaesth. (2011) 107 (4): 642-643.
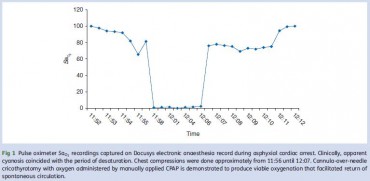
Le recours à un cathéter veineux et une seringue pour la réalisation d'une coniotomie est souvent présenté comme un simple gadget.
Cette technique a été mise en oeuvre dans le cadre de la prise en charge d'un arrêt circulatoire dans un bloc opéatoire. L'usage d'un cathéter de 14g, d'une seringue de 3ml associé à l'application continue doxygène à une pression de 35 à 4O mmHg a permis la restauration d'une oxygénation suffisante contribuant ainsi au succès des manoeuvres de prise en charge de l'arrêt circulatoires.
Le fait d'avoir à disposition une machine d'anesthésie permettant de générer une pression d'insufflation continue et élevée est certainement un élément essentiel à prendre en compte. Il n'est pas certain que ceci puisse être réalisé avec un BAVU sauf à bien obturer la valve notamment celle de surpression si elle existe.
| Tags : airway, coniotomie
Coniotomie: Chirurgicale avec un mandrin
Comparison of a percutaneous device and the bougie-assisted surgical technique for emergency cricothyrotomy: an experimental study on a porcine model performed by air ambulance anaesthesiologists
Nakstad et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2013, 21:59
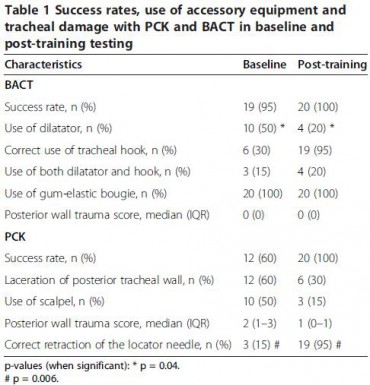
Background: A large number of techniques and devices for cricothyroidotomy have been developed. In this study, the Portex™ Cricothyroidotomy Kit (PCK, Smiths Medical Ltd, Hythe, UK) was compared with the bougie assisted emergency surgical cricothyrotomy technique (BACT).
Methods: Twenty air ambulance anaesthesiologists performed emergency cricothyrotomy on a cadaveric porcine airway model using both PCK and BACT. Baseline performance and performance after the intensive training package were recorded. Success rate, time to secured airway and tracheal damage were the primary endpoints, and confidence rating was a secondary endpoint.
Results: During baseline testing, success rates for PCK and BACT were 60% and 95%, respectively. Tracheal injury rate with PCK was 60% while no such injury was found in BACT. A lecture was given and skills were trained until the participants were able to perform five consecutive successful procedures with both techniques. In the posttraining test, all participants were successful with either technique. The mean time to successful insertion was reduced by 15.7 seconds (from 36.3 seconds to 20.6 seconds, p< 0.001) for PCK and by 7.8 seconds (from 44.9 seconds to 37.1 seconds, p=0.021) for BACT. In the post-training scenario, securing the airway with PCK was significantly faster than with BACT (p<0.001). Post-training tracheal laceration occurred in six (30%) of the PCK procedures and in none of the BACT procedures (p=0.028). The self-evaluated confidence level was measured both pre- and post-training using a confidence scale with 10 indicating maximum amount of confidence. The median values increased from 4 to 8 for PCK and from 6.5 to 9.5 for BACT. All participants reported that BACT was their preferred technique.
Conclusions: Testing the base-line PCK skills of prehospital anaesthesiologists revealed low confidence, sub-optimal performance and a very high failure rate. The BACT technique demonstrated a significantly higher success rate and no tracheal damage. In spite of PCK being a significantly faster technique in the post-training test, the anaesthesiologists still reported a higher confidence in BACT. Limitations of the cadaveric porcine airway may have influenced this study because the airway did not challenge the clinicians with realistic tissue bleeding.
| Tags : airway, coniotomie
Coniotomie: On fait le point
Emergency cricothyrotomy - A systematic review
Langvad F. et Al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2013 21:43
Une revue exhaustive de ce qui est publié sur le sujet. Il en ressort qu'il n'existe pas vraiment d'avantages d'une technique sur une autre, qu'en condition extrême une technique chirurgicale semble préférable. Le point clé est l'expérience et l'entraînement de celui qui la réalise.
----------------------------
Background: An emergency cricothyrotomy is the last-resort in most airway management protocols and is performed when it is not possible to intubate or ventilate a patient. This situation can rapidly prove fatal, making it important to identify the best method to establish a secure airway. We conducted a systematic review to identify whether there exists superiority between available commercial kits versus traditional surgical and needle techniques.
Methods: Medline, EMBASE and other databases were searched for pertinent studies. The inclusion criteria included manikin, animal and human studies and there were no restrictions regarding the professional background of the person performing the procedure.
Results: In total, 1,405 unique references were identified; 108 full text articles were retrieved; and 24 studies were included in the review. Studies comparing kits with one another or with various surgical and needle techniques were identified. The outcome measures included in this systematic review were success rate and time consumption. The investigators performing the studies had chosen unique combinations of starting and stopping points for time measurements, making comparisons between studies difficult and leading to many conflicting results. No single method was shown to be better than the others, but the size of the studies makes it impossible to draw firm conclusions.
Conclusions: The large majority of the studies were too small to demonstrate statistically significant differences, and the limited available evidence was of low or very low quality. That none of the techniques in these studies demonstrated better results than the others does not necessarily indicate that each is equally good, and these conclusions will likely change as new evidence becomes available
| Tags : coniotomie, airway
Voies aériennes: Avant tout une histoire de communication
Airway management: judgment and communication more than gadgets
Donati F. Can J Anesth/J Can Anesth (2013) 60:1035–1040
------------------------------------
Un éditorial publié à l'occasion de la sortie des nouvelles recommandations canadiennes sur l'intubation difficile (1 et 2). Plein de on sens et de pragmatisme et au final de rigueur scientifique dans ce document qui insiste sur le facteur humain et non le facteur matériel. . Les points essentiels sont
1. le maintien de l’oxygènation est proposé comme objectif ultime de toute manœuvre au niveau des voies aériennes
Non pas
"cannot intubate cannot ventilate"
mais
"cannot intubate cannot oxygenate"
2. Malgré la popularité croissante et l’utilisation répandue des dispositifs supraglottiques, l’intubation trachéale demeure l’étalon or et la méthode préférée pour une prise en charge stable des voies aériennes.
3. La vidéolaryngoscopie n’est pas présentée comme la solution universelle à tous les problèmes liés aux voies aériennes
4. Le nombre de tentatives, quelle que soit la technique d’intubation ou la position, devrait se limiter à trois même si n’existe aucune donnée probante solide appuyant un tel énoncé.
5. Même si il existe des données probantes selon lesquelles un accès chirurgical aux voies aériennes chirurgicales ne sauve pas toujours des vies, le groupe recommande d’essayer d’obtenir un accès chirurgical aux voies aériennes lorsque tous les autres types de tentative échouent.
05/11/2013
Coniotomie: Un nouveau set
A Comparison of Two Open Surgical Cricothyroidotomy Techniques by Military Medics Using a Cadaver Model
Mabry RL et All., Ann EmergMed. 2013;-:1-5
---------------------------------
Le taux d'échec observé est d'environ 33%. Aussi est on toujours à la recherche de dispositifs d'aide à la réalisation de ce geste considéré comme essentiel. L'originalité du kit présenté ici tient à son guide qui a une forme particulière censée améliorer la performance des combat medics. Relisez la fiche technique de la coniotomie en sachant que vous pouvez vous servir du mandrin d'eschmann comme guide d'insertion si vous avez recours à la technique chirurgicale ce qui est recommandé.
---------------------------------
Study objective: The CricKey is a novel surgical cricothyroidotomy device combining the functions of a tracheal hook, stylet, dilator, and bougie incorporated with a Melker airway cannula. This study compares surgical cricothyroidotomy with standard open surgical versus CricKey technique.
Methods: This was a prospective crossover study using human cadaveric models. Participants included US Army combat medics credentialed at the emergency medical technician–basic level. After a brief anatomy review and demonstration, participants performed in random order standard open surgical cricothyroidotomy and CricKey surgical cricothyroidotomy. The primary outcome was first-pass success, and the secondary outcome measure was procedural time.
Results: First-attempt success was 100% (15/15) for CricKey surgical cricothyroidotomy and 66% (10/15) for open surgical cricothyroidotomy (odds ratio 16.0; 95% confidence interval 0.8 to 326). Surgical cricothyroidotomy insertion was faster for CricKey than open technique (34 versus 65 seconds; median time difference 28 seconds; 95% confidence interval 16 to 48 seconds).
Conclusion: Compared with the standard open surgical cricothyroidotomy technique, military medics demonstrated faster insertion with the CricKey. First-pass success was not significantly different between the techniques
| Tags : coniotomie, airway
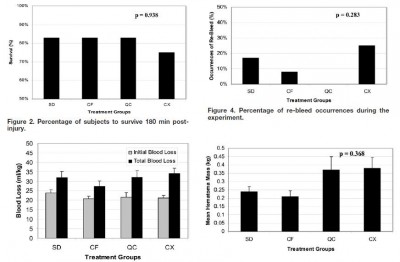
Pansement hémostatique: Utile?
Comparison of ChitoFlex®, CELOX™, and QuikClot® in control of hemorrhage
Devlin JJ et all. J Emerg Med. 2011 Sep;41(3):237-45
Un article qui complète le précédent et qui doit appeler à de la mesure sur l'emploi des pansements hémostatiques. Bien qu'il existe de nombreux travaux comparatifs prônant l'intérêt de tel ou tel dispositifs, le bien fondé de leur emploi extensif ne peut toujours pas être affirmé en condition de combat. Les messages pédagogiques doivent donc avant tout porter sur l'application correcte des pansements compressifs et le packing de plaie.
------------------------------------
BACKGROUND:
Exsanguinating extremity wounds remain the primary source of battlefield mortality. Operating forces employ three agents in Iraq: HemCon® (HemCon Medical Technologies, Inc., Portland, OR), QuikClot® (Z-Medica Corporation, Wallingford, CT), and CELOX™ (SAM Medical, Tualatin, OR). Anecdotal reports suggest that these agents are less useful on small entrance, linear-tract injuries. ChitoFlex® (HemCon Medical Technologies, Inc., Portland, OR) has been introduced but is untested.
STUDY OBJECTIVES:
To compare the equivalency of the ChitoFlex® dressing, QuikClot® ACS+™ dressing, CELOX™, and standard gauze in their effectiveness to control bleeding from non-cavitary groin wounds.
METHODS:
Forty-eight swine were randomly assigned to one of four treatment groups: standard gauze dressing (SD), ChitoFlex® dressing (CF), QuikClot® ACS+™ dressing (QC), and CELOX™ dressing (CX). A groin injury with limited vessel access was created in each animal. Subjects were resuscitated with 500 mL of hetastarch. The primary endpoint was 180-min survival. Secondary endpoints included total blood loss in mL/kg, incidence of re-bleeding, survival times among the animals that did not survive for 180 min, failure to achieve initial hemostasis, incidence of recurrent bleeding, time to initial re-bleeding, amount of re-bleeding, and mass of residual hematoma.
RESULTS:
Survival occurred in 10 of 12 SD animals, 10 of 12 CF animals, 10 of 12 QC animals, and 9 of 12 CX animals. No statistically significant difference was found.
CONCLUSION:
In our study of limited-access extremity bleeding, ChitoFlex® performed equally well in mitigating blood loss and promoting survival. The ChitoFlex® dressing is an equally effective alternative to currently available hemostatic agents. However, no agents were superior to standard gauze in our model of limited access.
| Tags : pansement
03/11/2013
The army hearing program
Heritage of army audiology and the road ahead: The Army Hearing Program
Mc Ilwain DS et all. Am J Public Health. 2008;98:2167–2172
Il n'y a pas que le PTSD qui soit considéré comme un enjeu majeur de dépistage et de traitement. La perte auditive bénéficie également d'un programme de grande ampleur au sein de l'armée américaine.
Les deux images qui suivent expliquent pourquoi:
1. La fréquence des déficits auditifs liés au combat
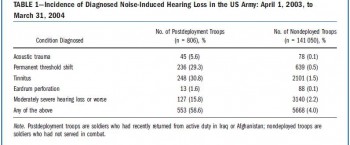
Un point détaillé récent ici
2. L'ouie est un système d'arme:
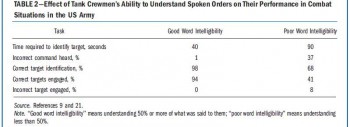
Ce document vous en décrit les grandes lignes
----------------------------------------
" Noise-induced hearing loss has been documented as early as the 16th century, when a French surgeon, Ambroise Pare´ , wrote of the treatment of injuries sustained by firearms and described acoustic trauma in great detail. Even so, the protection of hearing would not be addressed for three more centuries, when the jet engine was invented and resulted in a long overdue whirlwind of policy developmentaddressingtheprevention of hearing loss. We present a synopsis of hearing loss prevention in the US Army and describe the current Army Hearing Program, which aims to prevent noise-induced hearing loss in soldiers and to ensure their maximum combat effectiveness.............
With hearing conservation programs documenting marked initial improvements, the anticipated cost of veterans’ disability claims and payments were expected to decrease over time.10,11 However, with the start of the war in Afghanistan in 2001 and the war in Iraq in 2003, this proved not to be the case. Current data show that 51.8% of combat soldiers have moderately severe hearing loss or worse, mainly because of the loud sounds associated with combat. The implications for the army are great. When soldiers reach these levels of hearing loss, they must be evaluated for the ability to perform their duties safely and effectively. Depending on the findings, they may be given the option of changing to a job that does not put their hearing at further risk or leaving the service with a medical discharge......
."
| Tags : blast
02/11/2013
Blast et audition: Le responsable ?
Mechanisms of Hearing Loss after Blast Injury to the Ear
Cho S. et All. Plos One 8(7): e67618. doi:10.1371/journal.pone.0067618
Given the frequent use of improvised explosive devices (IEDs) around the world, the study of traumatic blast injuries is of increasing interest. The ear is the most common organ affected by blast injury because it is the body’s most sensitive pressure transducer. We fabricated a blast chamber to re-create blast profiles similar to that of IEDs and used it to develop a reproducible mouse model to study blast-induced hearing loss. The tympanic membrane was perforated in all mice after blast exposure and found to heal spontaneously. Micro-computed tomography demonstrated no evidence for middle ear or otic capsule injuries; however, the healed tympanic membrane was thickened. Auditory brainstem response and distortion product otoacoustic emission threshold shifts were found to be correlated with blast intensity. As well, these threshold shifts were larger than those found in control mice that underwent surgical perforation of their tympanic membranes, indicating cochlear trauma. Histological studies one week and three months after the blast demonstrated no disruption or damage to the intra-cochlear membranes. However, there was loss of outer hair cells (OHCs) within the basal turn of the cochlea and decreased spiral ganglion neurons (SGNs) and afferent nerve synapses. Using our mouse model that recapitulates human IED exposure, our results identify that the mechanisms underlying blast-induced hearing loss does not include gross membranous rupture as is commonly believed. Instead, there is both OHC and SGN loss that produce auditory dysfunction.
-----------------
Expérimentalement, La perte auditive n'est pas liée à l'atteinte du tympan mais plutôt à l'atteinte des cellules ciliées externes et du ganglion spiral de corti. L'image qui suit tirée d'un autre document vous présente les grandes causes d'atteinte de l'audition.
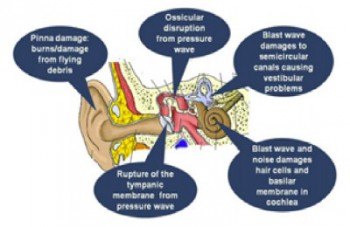
| Tags : blast
01/11/2013
Stabilisation pelvienne: Simple est efficace
Comparison of circumferential pelvic sheeting versus the T-POD on unstable pelvic injuries: A cadaveric study of stability
Prasarn ML et All. Injury. 2013 Jun 27. pii: S0020-1383(13)00256-8
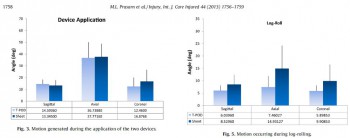
Objectives: Commercially available binder devices are commonly used in the acute treatment of pelvic fractures, while many advocate simply placing a circumferential sheet for initial stabilization of such injuries. We sought to determine whether or not the T-POD would provide more stability to an unstable pelvic injury as compared to circumferential pelvic sheeting.
Methods: Unstable pelvic injuries (OTA type 61-C-1) were surgically created in five fresh, lightly embalmed whole human cadavers. Electromagnetic sensors were placed on each hemi-pelvis. The amount of angular motion during testing was measured using a Fastrak, three-dimensional, electromagnetic motion analysis device (Polhemus Inc., Colchester, VT). Either a T-POD or circumferential sheet was applied in random order for testing. The measurements recorded in this investigation included maximum displacements for sagittal, coronal, and axial rotation during application of the device, bed transfer, log-rolling, and head of bed elevation.
Results: There were no differences in motion of the injured hemi-pelvis during application of either the T-POD or circumferential sheet. During the bed transfer, log-rolling, and head of bed elevation, there were no significant differences in displacements observed when the pelvis was immobilized with either a sheet or pelvic binder (T-POD).
Conclusions: A circumferential pelvic sheet is more readily available, costs less, is more versatile, and is equally as efficacious at immobilizing the unstable pelvis as compared to the T-POD. We advocate the use of circumferential sheeting for temporary stabilization of unstable pelvic injuries.
| Tags : pelvis