29/06/2013
Coagulopathie du trauma: Que faire ?
Case Scenario: Management of Trauma-induced Coagulopathy in a Severe Blunt Trauma Patient
David JS et All. Anesthesiology 2013; 119:191–200
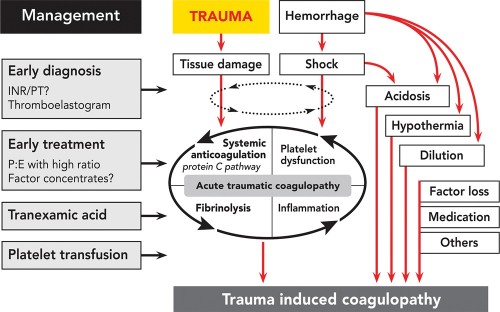
Un point très clair du problème
| Tags : coagulopathie
Pneumothorax: A partir de quel volume d'air le dépiste-t-on ?
The intrapleural volume threshold for ultrasound detection of pneumothoraces: An experimental study on porcine models
Oveland NP et All. Scand J Trauma Resusc Emerg Med. 2013; 21: 11.
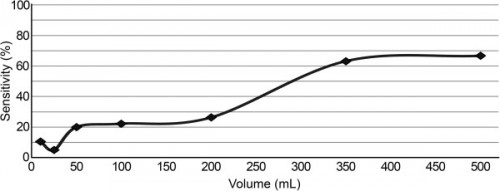
Tous les pneumothorax sont dépistés à l'échographie pour des volumes d'air de moins de 50 ml, de manière bien plus précoce que l'analyse d'une radiographie comme le montre la figure ci-dessus
| Tags : pneumothorax
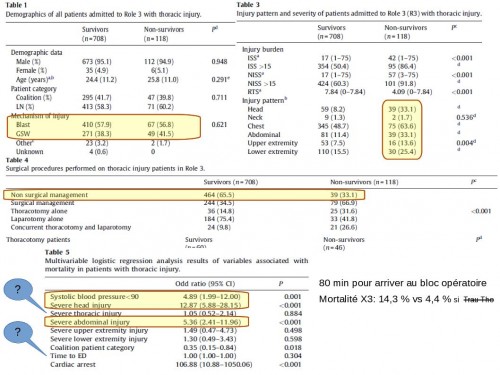
Blessés thoraciques: Données UK
The UK military experience of thoracic injury in the wars in Iraq and Afghanistan
Poon H. et All. Injury. 2013 Feb 20. pii: S0020-1383(13)00073-9.
INTRODUCTION:
Thoracic injury during warfare is associated with a high incidence of morbidity and mortality. This study examines the pattern and mortality of thoracic wounding in the counter-insurgency conflicts of Iraq and Afghanistan, and outlines the operative and decision making skills required by the modern military surgeon in the deployed hospital setting to manage these injuries.
METHODS:
The UK Joint Theatre Trauma Registry was searched between 2003 and 2011 to identify all patients who sustained battle-related thoracic injuries admitted to a UK Field Hospital (Role 3). All UK soldiers, coalition forces and local civilians were included.
RESULTS:
During the study period 7856 patients were admitted because of trauma, 826 (10.5%) of whom had thoracic injury. Thoracic injury-related mortality was 118/826 (14.3%). There were no differences in gender, age, coalition status and mechanism of injury between survivors and non-survivors. Survivors had a significantly higher GCS, Revised Trauma Score and systolic blood pressure on admission to a Role 3 facility. Multivariable regression analysis identified admission systolic blood pressure less than 90, severe head or abdominal injury and cardiac arrest as independent predictors of mortality.
CONCLUSIONS:
Blast is the main mechanism of thoracic wounding in the recent conflicts in Iraq and Afghanistan. Thoracic trauma in association with severe head or abdominal injuries are predictors of mortality, rather than thoracic injury alone. Deploying surgeons require training in thoracic surgery in order to be able to manage patients appropriately at Role 3.
Commentaires
La plupart des traumatisés ne nécessite pas de chirurgie. Les survivants arrivent plus vite mais il ne semble pas qu'un délai un peu plus long soit associé avec une surmortalité. La gravité du traumatisme thoracique n'apparait pas être lié avec la mortalité. il existeune amélioration du pronostic rapporté à l'amélioration de la prise en charge globale.
| Tags : traumatologie, thorax
27/06/2013
DU Fosei
A partir de la rentrée universitaire 2013 et dans le cadre du projet SAMSEI , l'université de médecine proposera une formation à la simulation. Fidèle au principe d'enseignement par ilmmersion ce DU est conduit avec l'ensemble des structures universitaires lyonnaises mais aussi le service de santé des armées notamment le CITERA de l'HIA Desgenettes, Le Cefos et l'Institut de recherche du SSA.
Les modalités pratiques d'inscription à ce DU sont disponibles sur ce lien.
| Tags : simulateurs
26/06/2013
Facteurs humains: Les prendre en compte pour votre préparation
Lessons from the battlefield: human factors in defence anaesthesia
Mercer SJ et All. BJA 105 (1): 9–20 (2010)
Ce document insiste sur l'importance des factuers humains sur la performance des équipes d'anesthésistes déployés dans un environnement peu familier, des situations beaucoup plus complexes que celles rencontrées dans leur pratique habituelle. Il insiste sur les phases de préparation en amont sur des scenarii proches de ceux rencontrés en réels et sur les moyens de condurie cette préparation notamment le recours à la simulation haute fidélité.
25/06/2013
Blast TBI: Un seuil plus bas que pour le poumon
Working toward exposure thresholds for blast-induced traumatic brain injury: thoracic and acceleration mechanisms.
Courtney MW et all. Neuroimage, 2011 Jan,54 Suppl 1: S55-61
Les mécanismes du blast cérébral associent la tansmission de la surpression via le thorax, l'impact direct sur la boite crânienne et les phénomènes d'accélaration de l'extrémité céphalique. Ce document explore la première voie et exprime bien que les seuils lésionnels de lésions cérébrales (courbes de Ono) sont plus bas que les seuils pulmonaires(courbes de Bowden).
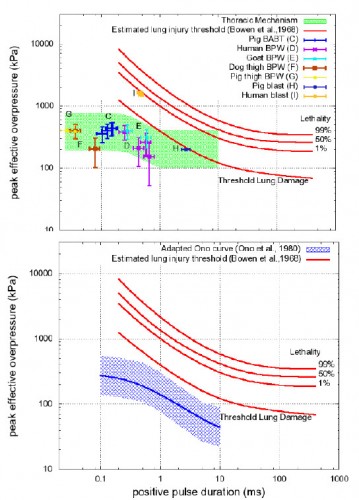
| Tags : balistique, tbi
24/06/2013
Pneumothorax: Echographie
Husain LF et All. Sonographic diagnosis of pneumothorax.
J Emerg Trauma Shock 2012;5:76-81
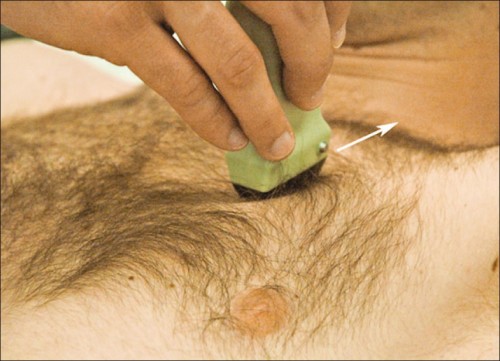
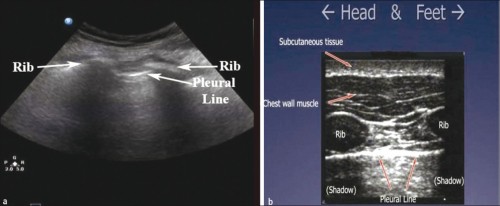
Position de la sonde
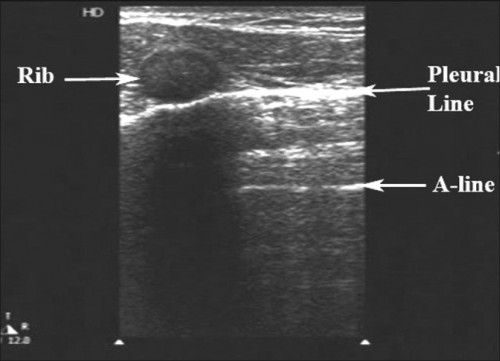
Images normales
Le glissement pleural Vidéo
La chauve-souris
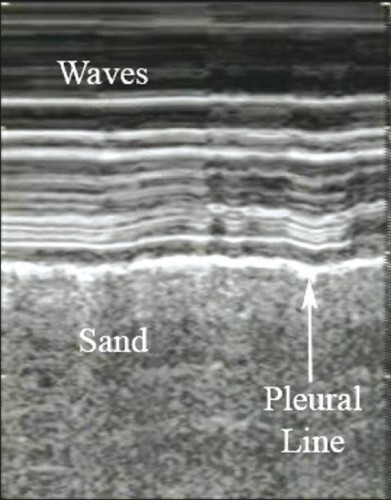
Le bord de plage
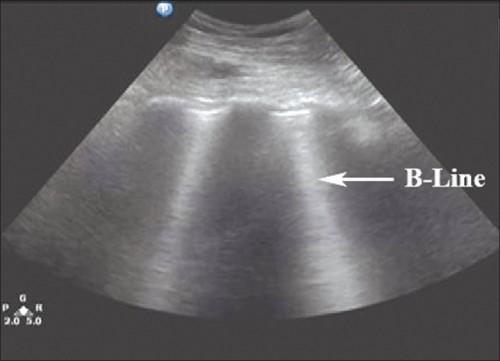
Les lignes B
Images Anormales attestant du pneumothorax
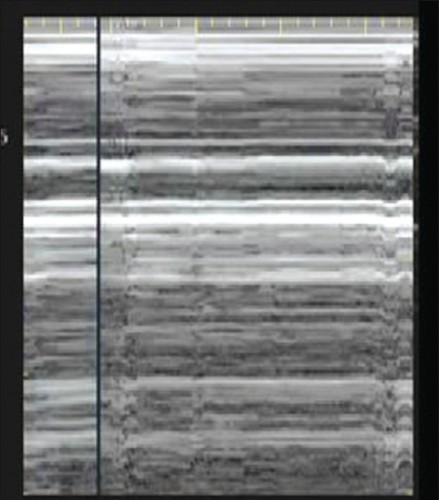
Pas de glissement Vidéo
Le signe du Barcode
Les lignes A
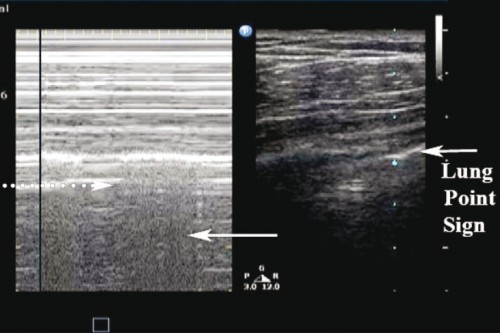
Le point poumon
Le pouls pulmonaire

Pour aller plus loin:
| Tags : pneumothorax, échographie
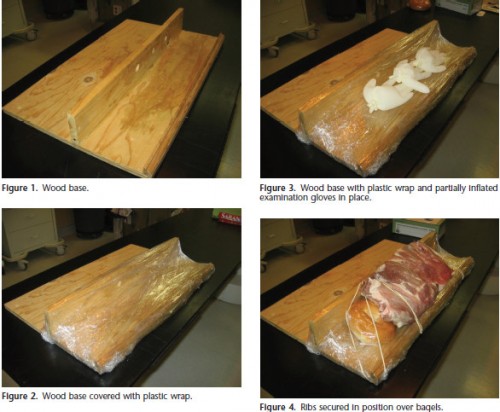
Simulateur de geste: Pour drainer le thorax
23/06/2013
Tranches de vie de nos collègues US
| Tags : retex
22/06/2013
QMS: Eclairage de l'extrême
Low flow mais pas zero flow resuscitation
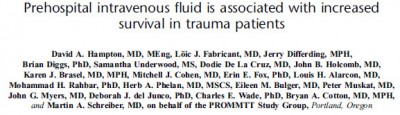
Hampton D. et all. J Trauma Acute Care Surg. 2013;74: S9-S15
---------------------------------------------------------------------------------------
BACKGROUND:
Delivery of intravenous crystalloid fluids (IVF) remains a tradition-based priority during prehospital resuscitation of trauma patients. Hypotensive and targeted resuscitation algorithms have been shown to improve patient outcomes. We hypothesized that receiving any prehospital IVF is associated with increased survival in trauma patients compared with receiving no prehospital IVF.
METHODS:
Prospective data from 10 Level 1 trauma centers were collected. Patient demographics, prehospital IVF volume, prehospita and emergency department vital signs, lifesaving interventions, laboratory values, outcomes, and complications were collected and analyzed. Patients who did or did not receive prehospital IVF were compared. Tests for nonparametric data wer used to assess significant differences between groups (p e 0.05). Cox regression analyses were performed to determine the independent influence of IVF on outcome and complications.
RESULTS:
The study population consisted of 1,245 trauma patients; 45 were excluded owing to incomplete data; 84% (n = 1,009) received prehospital IVF, and 16% (n = 191) did not. There was no difference between the groups with respect to sex, age, and Injury Severity Score (ISS). The on-scene systolic blood pressure was lower in the IVF group (110 mm Hg vs. 100 mm Hg, p G 0.04) and did not change significantly after IVF, measured at emergency department admission (110 mm Hg vs. 105 mm Hg, p = 0.05). Hematocrit/hemoglobin, fibrinogen, and platelets were lower (p G 0.05), and prothrombin time/ international normalized ratio and partial thromboplastin time were higher (p G 0.001) in the IVF group. The IVF group received a median fluid volume of 700 mL (interquartile range, 300Y1,300). The Cox regression revealed that prehospital fluid administration was associated with increased survival (hazard ratio, 0.84; 95% confidence interval, 0.72Y0.98; p = 0.03). Site differences in ISS and fluid volumes were demonstrated (p G 0.001).
CONCLUSION:
Prehospital IVF volumes commonly used by PRospective Observational Multicenter Massive Transfusion Study (PROMMTT) investigators do not result in increased systolic blood pressure but are associated with decreased in-hospital mortality in trauma patients compared with patients who did not receive prehospital IVF
---------------------------------------------------------------------------------------
C'est du moins ce que conclue ce travail qui porte sur l'administration préhospitalière de cristalloïdes dans le cadre de conditionnements qui apparaissent assez proche de notre pratique. Ces résultats interpellent cependant car prenant apparemment le contrepied d'une autre publication récente lisible ici.
Comme dans tout restons mesurés comme proposé par ce consensus US
1. Patients porteur de plaies supérficielles: Pas d'abord veineux immédiat
2. Patient cohérent avec pouls radial: Verrou salé
3. Patient incohérent ou pas e pouls radial: Abord veineux et apport d'un volume de 500 ml
[ATTENTION AUX HEA AU SUJET DESQUELS LA CONTROVERSE S'ACCENTUE]
4. Répéter l'administration si pas d'effet
5. Si trauma cranien obtenir une PAS > 90 mmHg
L'objectif n'est pas de restaurer une pression artérielle normale mais de maintenir une pression de perfusion compatible avec la survie jusqu'à la prise en charge par une équipe chirurgicale.
| Tags : remplissage, perfusion
19/06/2013
HEA : Encore une publication contre
Association of Hydroxyethyl Starch Administration With Mortality and Acute Kidney Injury in Critically Ill Patients Requiring Volume ResuscitationA Systematic Review and Meta-analysis
In critically ill patients requiring acute volume resuscitation, use of hydroxyethyl starch compared with other resuscitation solutions was not associated with a decrease in mortality. Moreover, after exclusion of 7 trials performed by an investigator whose research has been retracted because of scientific misconduct, hydroxyethyl starch was associated with a significant increased risk of mortality and acute kidney injury. Clinical use of hydroxyethyl starch for acute volume resuscitation is not warranted due to serious safety concerns.
| Tags : remplissage
09/06/2013
Mise en condition de survie des blessés en opération extérieure
Mise en condition de survie des blessés en opération extérieure : Procédure et expérience à partir du terrain afghan
Conditions for the survival of combat casualties in overseas operations : procedure and experience from the Afghan out-of-hospital theater
Palmier B. Bull. Acad. Natle Méd., 2012, 196, nos 4-5, 893-907, séance du 24 avril 2012
RÉSUMÉ
Les conflits récents ont amené le service de santé des armées français à préciser la mise en condition de survie des blessés de guerre en opération extérieure. La majorité d’entre eux est victime de blessures par explosion et un contrôle précoce de l’hémorragie est le moyen principal d’améliorer la survie. Une procédure appelée « Sauvetage au Combat » est enseignée pour la mise en condition de survie de ces blessés. Elle est appliquée depuis quelques années sur le terrain afghan.
SUMMARY
Recent conflicts have led the French Army Health Service to specify the setting condition for the survival of combat casualties in overseas operations. The majority of them are victims of explosion injuries, and an early and effective control of bleeding is the primary means of improving survival. A procedure called ‘‘ Combat Rescue ’’ is taught. This chronological procedure favours external haemostasis and led to specific equipment, in particular a tourniquet and a haemostatic bandage of high efficiency. It is applied in recent years on the Afghan out-of-hospital theatre. A very front medical presence, which is systematic during evacuations, is a feature of the French Army Health Service operations support.
03/06/2013
Garrots: Sur soi mais pas n'importe comment !
Efficacy of tourniquets exposed to the afghanistan combat environment stored in individual first aid kits versus on the exterior of plate carriers
Weppner J et all. Mil Med. 2013 Mar;178(3):334-7
Between February and May 2010, 1st Battalion, 6th Marines reported a 10% (10/92) breakage rate for tourniquets. One theory suggested was that tourniquets were weakened by exposure to the Afghan environment. Our study was designed to compare three groups of Afghanistan-exposed tourniquets to unexposed tourniquets. The three experimental arms were: (1) Afghan-exposed tourniquets worn on the plate carrier, (2) Afghan-exposed tourniquets carried in the Individual First Aid Kit (IFAK) and wrapped in manufacturer plastic wrapping, and (3) Afghan-exposed tourniquets carried in the IFAK with the manufacturer plastic wrapping removed. The outcome measures of this study were efficacy, breakage, and number of turns required to successfully stop the distal pulse. Tourniquets worn on the plate carrier had an efficacy of 57%, which was significantly lower than the control efficacy rate of 95.2%. When compared to the control arm, there were no significant differences in efficacy between the tourniquets stored in the IFAK with or without manufacturing packaging. No control tourniquets or tourniquets stored in IFAKs broke; however, 46 (12%) of the plate carrier-exposed tourniquets did break. No statistically significant differences were found between the four groups with regard to the median number of turns required to stop the distal pulse.
| Tags : tourniquet
02/06/2013
Hémorragies jonctionnelles: Comprimer le pelvis
UK Combat-Related Pelvic Junctional Vascular Injuries 2008-2011: Implications for Future Intervention.
Walker NM et All. - Bone Joint Journal (2013) vol. 95-B no. SUPP 8 13
---------------------------------------------------------------------------------------
L'arrêt d'une hémorragie jonctionnelle est un enjeu majeur. Plusieurs dispositifs ont été récemment proposés. Il semble que la grande majorité des lésions observées se situent au dessus du ligament inguinal rendant ainsi l'efficacité de dispositif comme le CRoC limité. Le tourniquet abdominal ou le sam junctionnal tourniquet paraissent ainsi au moins théoriquement un meilleur choix si toutefois ils permettent une compression suffisante.
---------------------------------------------------------------------------------------
In a recent publication, 4.6% of 6450 Coalition deaths over ten years were reported to be due to junctional bleeding. The authors suggested that some of these deaths could have been avoided with a junctional hemorrhage control device.
Prospectively collected data on all injuries sustained in Afghanistan by UK military personnel over a 2 year period were reviewed. All fatalities with significant pelvic injuries were identified and analysed, and the cause of death established.
Significant upper thigh, groin or pelvic injuries were recorded in 124 casualties, of which 92 died. Pelvic injury was the cause of death in 42; only 1 casualty was identified where death was at least in part due to a vascular injury below the inguinal ligament, not controlled by a tourniquet, representing <1% of all deaths. Twenty one deaths were due to vascular injury between the aortic bifurcation and the inguinal ligament, of which 4 survived to a medical facility.
Some potentially survivable deaths due to exsanguination may be amenable to more proximal vascular control. We cannot substantiate previous conclusions that this can be achieved through use of a groin junctional tourniquet. There may be a role for more proximal vascular control of pelvic bleeding.
| Tags : tourniquet, hémorragie, jonctionnel