03/08/2015
Accès veineux: Vision israélienne
Intravenous access in the prehospital settings: What can be learned from point-of-injury experience
Nadler R et Al. J Trauma Acute Care Surg. 2015;79: 221-226
-----------------------------------
La réalisation d'un abord vasculaire est un des gestes le plus souvent pratiqué. On rappelle qu'il s'agit là de pouvoir injecter certains médicaments (morphine, adrénaline, TXA, antibiotiques), d'initier un remplissage vasculaire raisonné voire d'administrer des dérives sanguins ou fractions coagulantes. Un document intéressant qui émane de l'armée israélienne fait le point sur cette pratique. Dans cette dernière (qui on le rappelle est assez spécifique compte tenu de la grande proximité des zones de combat et des structures hospitalières), il apparaît qu'il ne faille pas aller au delà de deux tentatives de pose de VVP au risque de retarder la prise en charge chirurgicale des blessés. Par ailleurs les taux de succès des médecins, combat medics et paramédics (pour nous nos infirmiers) soit superposable. Enfin la médiocre performance de l'accès intra-osseux doit interpeller.
-----------------------------------
BACKGROUND:
Intravenous (IV) access has an essential role in the care provided for trauma patients, allowing for transfusion of blood products, fluids, and drugs. Decisions should be made regarding the necessity of IV access while considering cost-benefit of the procedure in terms of delayed evacuation times.
METHODS:
A retrospective review of all trauma patients in whom at least one attempt at IVaccess was performed were reviewed. Data were abstracted from the Israeli Defense Force Trauma Registry.
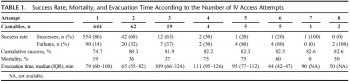
RESULTS:
Of 7,476 patients, 1,082 patients who had at least one documented attempt at IV access between January 1997 and April 2013 were included in this study. Overall cumulative success rate at IV access was 82%. Success rates for IVaccess were 86%, 68%, 63%, 50%, 20% for the first, second, third, fourth, and fifth attempts, respectively. The first and second attempts accounted for 96% of the successful procedures. Mortality in patients for whom IV access was successful was 13%; mortality in patients for whom IV access was not successful was 35%.
CONCLUSION:
The success rate of IV access declined with each subsequent attempt. There was minimal improvement of overall success rate seen after the second attempt. Our findings suggest that the inability to obtain peripheral venous access is associated with severe injuries. These finding support a policy of limiting the number of venous access attempts to two attempts, followed by a reevaluation of need for parenteral access. Improved training of combat medics and paramedics might marginally increase the success rates of IVaccess. Point-of-injury data, used for ongoing learning and research, form the ground for improving combat casualty care and thus help saving lives.
| Tags : perfusion
31/01/2015
Cristalloïde/Colloïde ration; Plutôt 1,5 que 4
Crystalloids Versus Colloids: Exploring Differences in Fluid Requirements by Systematic Review and Meta-Regression
Orbegozo Cortés D. et Al. Anesth Analg 2015;120:389–402
-------------------------------------------------------------------
Le débat qui porte sur l'efficacité comparée des solutés de remplissage n'est pas nouveau. Cette méta-analyse porte sur l'analyse de 27 publications sélectionnées parmi 978. Elle met en évidence la très grande hétérogénéité des données publiées. Les raisons avancées portent sur la nature des populations étudiées (fuite capillaire très variable), l'administration préhospitalière de fluides à des volumes mal connu ce qui va compliquer l'analyse ultérieure, les différences de pharmacodynamie et cintétique des différents solutés employés, le fait que pour un même soluté l'efficacité en terme de remplissage puisse varier en fonction du moment de son administration, Qui qu'il en soit il semble que le ratio actuel soit plus proche de 1,5 que de 4.
On rappelle que la procédure du sauvetage au combat met en avant l'emploi de soluté salé hypertonique en première intention (250 ml en 10 minutes) suivi de 500ml de colloïdes (à défaut 250 ml de salé hypertonique) en cas de non restauration du pouls radial. Ce choix est résulte d'un compromis dans lequel le poids des solutés est pris en compte.
-------------------------------------------------------------------
BACKGROUND:
Positive fluid balance has been associated with worse outcomes, and knowledge of differences in the amounts of different types of fluid needed to achieve the same end points may have important clinical implications. Large molecules persist longer in the blood vessels than smaller molecules, such that less IV colloid may be needed to achieve similar hemodynamic end points compared with crystalloid. Recent clinical data have, however, challenged this physiological concept, with investigators reporting lower-than-expected crystalloid/colloid ratios in various populations.
METHODS:
We performed a systematic search in MEDLINE, EMBASE, and CENTRAL up to December 18, 2013, to retrieve all studies comparing (any) crystalloid with (any) colloid in all types of patients. The crystalloid/colloid ratio was calculated for each study. Descriptive analysis was performed for all studies, and a meta-analysis was performed in those studies reporting full data (in terms of means and standard deviations) of infused fluid volumes. Studies were grouped according to study and population characteristics. A meta-regression analysis was then performed to evaluate some of the possible reasons for differences in crystalloid/colloid ratios across studies.
RESULTS:
From 976 studies, 48 were retained for the final analysis; 24 of the studies had sufficient data for meta-analysis. The crystalloid/colloid ratio across all the studies included in the meta-analysis was 1.5 (95% confidence interval, 1.36–1.65) with marked heterogeneity among studies (I2 = 94%). From the meta-regression analysis, decade of publication across all publications (P = 0.001) and concentration (tonicity) in the subgroup of albumin studies (P = 0.001) were associated with the administered crystalloid/colloid ratio. The reduction in heterogeneity among studies for all publications in the meta-regression was minimal, with the maximal decrease obtained when decade of publication was considered (R2 = 12%).
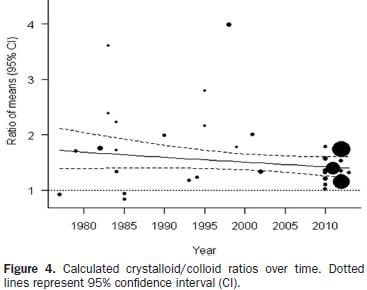
CONCLUSIONS:
Greater fluid volumes are required to meet the same targets with crystalloids than with colloids, with an estimated ratio of 1.5 (1.36–1.65), but there is marked heterogeneity among studies. The crystalloid/colloid ratio seems to have decreased over the years, and differences in ratios are correlated with the concentration of albumin solutions; however, the main reasons behind the high heterogeneity among studies remain unclear.
| Tags : remplissage, perfusion
22/06/2013
Low flow mais pas zero flow resuscitation
Hampton D. et all. J Trauma Acute Care Surg. 2013;74: S9-S15
---------------------------------------------------------------------------------------
BACKGROUND:
Delivery of intravenous crystalloid fluids (IVF) remains a tradition-based priority during prehospital resuscitation of trauma patients. Hypotensive and targeted resuscitation algorithms have been shown to improve patient outcomes. We hypothesized that receiving any prehospital IVF is associated with increased survival in trauma patients compared with receiving no prehospital IVF.
METHODS:
Prospective data from 10 Level 1 trauma centers were collected. Patient demographics, prehospital IVF volume, prehospita and emergency department vital signs, lifesaving interventions, laboratory values, outcomes, and complications were collected and analyzed. Patients who did or did not receive prehospital IVF were compared. Tests for nonparametric data wer used to assess significant differences between groups (p e 0.05). Cox regression analyses were performed to determine the independent influence of IVF on outcome and complications.
RESULTS:
The study population consisted of 1,245 trauma patients; 45 were excluded owing to incomplete data; 84% (n = 1,009) received prehospital IVF, and 16% (n = 191) did not. There was no difference between the groups with respect to sex, age, and Injury Severity Score (ISS). The on-scene systolic blood pressure was lower in the IVF group (110 mm Hg vs. 100 mm Hg, p G 0.04) and did not change significantly after IVF, measured at emergency department admission (110 mm Hg vs. 105 mm Hg, p = 0.05). Hematocrit/hemoglobin, fibrinogen, and platelets were lower (p G 0.05), and prothrombin time/ international normalized ratio and partial thromboplastin time were higher (p G 0.001) in the IVF group. The IVF group received a median fluid volume of 700 mL (interquartile range, 300Y1,300). The Cox regression revealed that prehospital fluid administration was associated with increased survival (hazard ratio, 0.84; 95% confidence interval, 0.72Y0.98; p = 0.03). Site differences in ISS and fluid volumes were demonstrated (p G 0.001).
CONCLUSION:
Prehospital IVF volumes commonly used by PRospective Observational Multicenter Massive Transfusion Study (PROMMTT) investigators do not result in increased systolic blood pressure but are associated with decreased in-hospital mortality in trauma patients compared with patients who did not receive prehospital IVF
---------------------------------------------------------------------------------------
C'est du moins ce que conclue ce travail qui porte sur l'administration préhospitalière de cristalloïdes dans le cadre de conditionnements qui apparaissent assez proche de notre pratique. Ces résultats interpellent cependant car prenant apparemment le contrepied d'une autre publication récente lisible ici.
Comme dans tout restons mesurés comme proposé par ce consensus US
1. Patients porteur de plaies supérficielles: Pas d'abord veineux immédiat
2. Patient cohérent avec pouls radial: Verrou salé
3. Patient incohérent ou pas e pouls radial: Abord veineux et apport d'un volume de 500 ml
[ATTENTION AUX HEA AU SUJET DESQUELS LA CONTROVERSE S'ACCENTUE]
4. Répéter l'administration si pas d'effet
5. Si trauma cranien obtenir une PAS > 90 mmHg
L'objectif n'est pas de restaurer une pression artérielle normale mais de maintenir une pression de perfusion compatible avec la survie jusqu'à la prise en charge par une équipe chirurgicale.
| Tags : remplissage, perfusion
02/03/2013
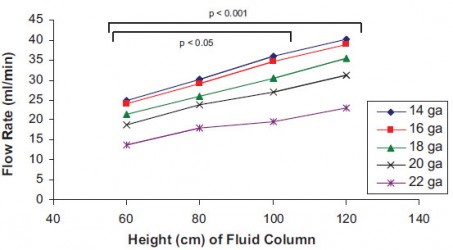
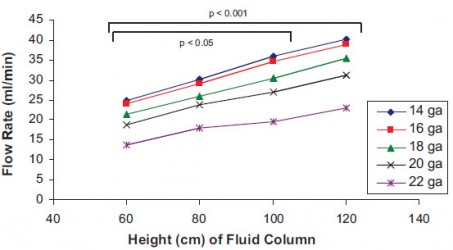
Diamètre de KT: 16 G est un bon compromis
Medication and Volume Delivery by Gravity-Driven Micro-Drip Intravenous Infusion: Potential Variations During “Wide-Open” Flow
Pierce E. et all Anesth Analg 2013;116:614–18
Ce travail porte sur l'intérêt d'administrer une perfusion par pompe plutôt que par gravité. Cependant ces deux figures relativisent l'intérêt de la pose de cathéter de 14g comparé à des cathéters de 16g dont les performances sont somme toute assez proches et qui restent bien plus simples à poser.
08/09/2012
Moins remplir: Mieux ? Oui, MAIS
Restrictive fluid resuscitation in combination with damage control resuscitation: Time for adaptation.
Marquinn D et all. J Trauma Acute Care Surg. 2012;73: 674-678.
-------------------------------------------------------------------------------------------------------------
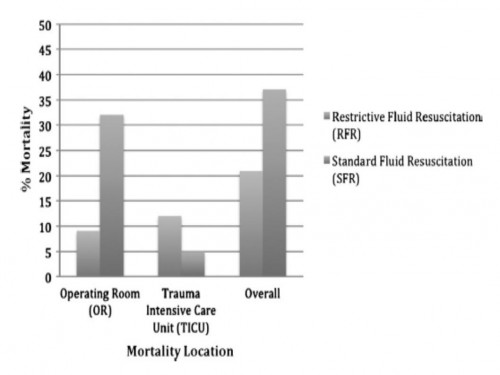
Ce travail confirme l'intérêt d'une stratégie de remplissage vasculaire parcimonieuse dès lors qu'une réanimation et une chirurgie spécialisée moderne sont accessibles. Le collectif des patients est ici celui de traumatisés thoraciques sévères arrivant dans une structure spécialisée dans des délais très courts. De telles conditions ne sont pas forcément celles de la prise en charge de blessés de guerre pour qui les délais d'évacuation sont souvent plus élevés. Il n'en demeure pas moins que cette publication milite pour une politique de remplissage vasculaire raisonnée. On rappelle que la procédure du sauvetage au combat donne pour objectif la perception d'un pouls radial perceptible.
-------------------------------------------------------------------------------------------------------------
BACKGROUND:
Damage control resuscitation (DCR) conveys a survival advantage in patients with severe hemorrhage. The role of restrictive fluid resuscitation (RFR) when used in combination with DCR has not been elucidated. We hypothesize that RFR, when used with DCR, conveys an overall survival benefit for patients with severe hemorrhage.
METHODS:
This is a retrospective analysis from January 2007 to May 2011 at a Level I trauma center. Inclusion criteria included penetrating torso injuries, systolic blood pressure less than or equal to 90 mm Hg, and managed with DCR and damage control surgery (DCS). There were two groups according to the quantity of fluid before DCS: (1) standard fluid resuscitation (SFR)greater than or equal to 150 mL of crystalloid; (2) RFR less than 150 mL of crystalloid. Demographics and outcomes were analyzed.
RESULTS:
Three hundred seven patients were included. Before DCS, 132 (43%) received less than 150 mL of crystalloids, grouped under RFR; and 175 (57%) received greater than or equal to 150 mL of crystalloids, grouped under SFR. Demographics and initial clinical characteristicswere similar between the study groups. Compared with the SFR group, RFR patients received less fluid preoperatively (129 mL vs. 2,757 mL; p G 0.001), exhibited a lower intraoperative mortality (9% vs. 32%; p G 0.001), and had a shorter hospital length of stay (13 vs. 18 days; p = 0.02). Patients in the SFR group had a lower trauma intensive care unit mortality (5 vs. 12%; p = 0.03) but exhibited a higher overall mortality. Patients receiving RFR demonstrated a survival benefit, with an odds ratio for mortality of 0.69 (95% confidence interval, 0.37Y0.91).
CONCLUSION:
To the best of our knowledge, this is the first civilian study that analyzes the impact of RFR in patients managed with DCR. Its use in conjunction with DCR for hypotensive trauma patients with penetrating injuries to the torso conveys an overall and early intraoperative survival benefit.
| Tags : remplissage, choc, hémorragie, perfusion
11/02/2012
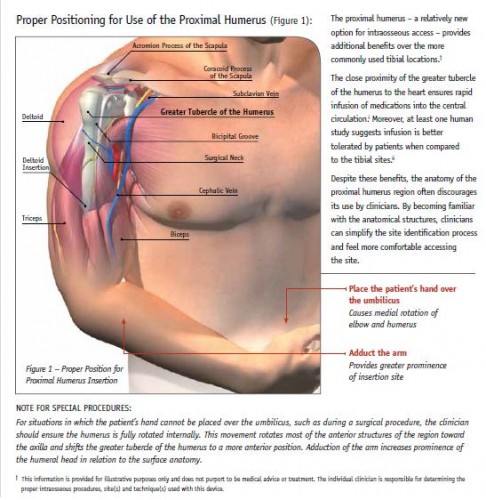
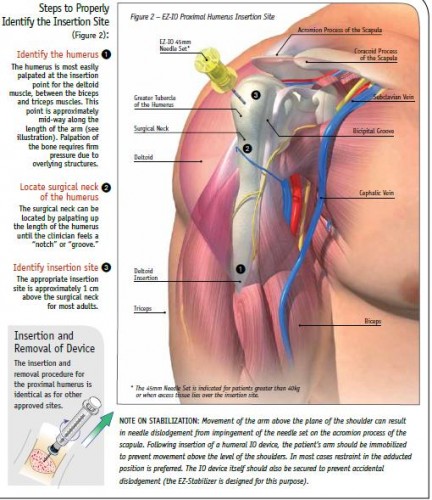
Accès intraosseux: La voie humérale
| Tags : intraosseux, perfusion
Accès intraosseux: Revue
| Tags : intraosseux, perfusion
24/12/2011
HEA, vraiment sûrs ?: Réponse début 2012 ?
Fluid Resuscitation with 6% Hydroxyethyl Starch (130/0.4) in Acutely Ill Patients: An Updated Systematic Review and Meta-Analysis
Gattas DJ et all. Anesth Analg 2012; 114:159–69
Une autre méta-analyse sur l'inocuité ou pas des solutions d'HEA 130 000/0,4 (Voluven]. Rien ne permet de conclure pour ou pas. Les auteurs estiment nécessaire de s'assurer de l'inocuité réele de ces produits par des travaux conduits de manière indépendante de l'industrie et sur une population plus large que celle de réanimation habituellement incluse. Ils mettent par ailleurs en avant le retrait récent de plusieurs publications portant sur la sécurité de ce type d'HEA. Il cite une étude intitulée Crystalloid versus Hydroxyethyl Starch Trial (CHEST) réalisée en australie portant sur l'analyse de la mortalité à 90 jours en comparant ce type de solutés à du salé isotonique qui devrait voir ses premiers résultats produits début 2012.
| Tags : remplissage, perfusion, choc