09/10/2018
Voies aériennes et choc hémorragique, que faire ?
Airway and ventilation management strategies for hemorrhagic shock. To tube, or not to tube, that is the question!
Hudson AJ et Al. J Trauma Acute Care Surg. 2018 Jun;84(6S Suppl 1):S77-S82
------------------------------
Primum non nocere. Souvent ne pas faire parce que c'est le plus prudent ET NON PAS PARCE QU'ON N'A PAS APPRIS ET QU'ON NE SAIT DONC PAS FAIRE.
------------------------------
Many standard trauma management guidelines advocate the early use of endotracheal intubation (ETI) and positive pressure ventilation as key treatment interventions in hemorrhagic shock. The evidence for using these airway and ventilation strategies to manage a circulation problem is unclear. The potentially harmful effects of drug-assisted intubation and positive pressure ventilation include reduced cardiac output, apnea, hypoxia, hypocapnea (due to inadvertent hyperventilation), and unnecessarily prolonged on-scene times. Conversely, the beneficial effects of spontaneous negative pressure ventilation on cardiac output are well described. Few studies, however, have attempted to explore the potential advantages of a strategy of delayed intubation and ventilation (together with a policy of aggressive volume replacement) in shocked trauma patients. Given the lack of evidence, the decision making around how, when, and where to subject shocked trauma patients to intubation and positive pressure ventilation remains complex. If providers choose to delay intubation, they must have the appropriate skills to safely manage the airway and recognize the need for subsequent intervention. If they decide to perform intubation and positive pressure ventilation, they must understand the potential risks and how best to minimize them. We suggest that for patients with hemorrhagic shock who do not have a compromised airway and who are able to maintain adequate oxygen saturation (or mentation if monitoring is unreliable), a strategy of delayed intubation should be strongly encouraged.
| Tags : choc
30/09/2018
US: Mieux que la main pour la conio
A multicentre prospective cohort study of the accuracy of conventional landmark technique for cricoid localisation using ultrasound scanning
Cricoid pressure is employed during rapid sequence induction to reduce the risk of pulmonary aspiration. Correct application of cricoid pressure depends on knowledge of neck anatomy and precise identification of surface landmarks. Inaccurate localisation of the cricoid cartilage during rapid sequence induction risks incomplete oesophageal occlusion, with potential for pulmonary aspiration of gastric contents. It may also compromise the laryngeal view for the anaesthetist. Accurate localisation of the cricoid cartilage therefore has relevance for the safe conduct of rapid sequence induction.
We conducted a multicentre, prospective cohort study to determine the accuracy of cricoid cartilage identification in 100 patients. The cranio‐caudal midpoint of the cricoid cartilage was identified by a qualified anaesthetic assistant using the conventional landmark technique and marked. While maintaining the patient in the same position, a second mark was made by identifying the midpoint of the cricoid cartilage using ultrasound scanning.
The mean (SD) distance between the two marks was 2.07 (8.49) mm. In 41% of patients the midpoint was incorrectly identified by a margin greater than 5 mm. This error was uniformly distributed both above and below the midpoint of the cricoid cartilage. The Pearson correlation coefficient of this error with respect to body mass index was 0.062 (p = 0.539) and with age was −0.020 (p = 0.843). There were also no significant differences in error between male and female patients.
Identification of cricoid position using a landmark technique has a high degree of variability and has little correlation with age, sex or body mass index. These findings have significant implications for the safe application of cricoid pressure in the context of rapid sequence induction.
| Tags : airway, coniotomie
23/09/2018
ISR par des non médecins: Oui possible
Prehospital Rapid Sequence Intubation by Intensive Care Flight Paramedics.
OBJECTIVE:
Rapid sequence intubation (RSI) is an advanced airway procedure for critically ill or injured patients. Paramedic-performed RSI in the prehospital setting remains controversial, as unsuccessful or poorly conducted RSI is known to result in significant complications. In Victoria, intensive care flight paramedics (ICFPs) have a broad scope of practice including RSI in both the adult and pediatric population. We sought to describe the success rates and characteristics of patients undergoing RSI by ICFPs in Victoria, Australia.
METHODS:
A retrospective data review was conducted of adult (≥ 16 years) patients who underwent RSI by an ICFP between January 1, 2011, and December 31, 2016. Data were sourced from the Ambulance Victoria data warehouse.
RESULTS:
A total of 795 cases were included in analyses, with a mean age of 45 (standard deviation = 19.6) years. The majority of cases involved trauma (71.7%), and most patients were male (70.1%). Neurological pathologies were the most common clinical indication for RSI (68.3%). The first pass success rate of intubation was 89.4%, and the overall success rate was 99.4%. Of the 5 failed intubations (0.6%), all patients were safely returned to spontaneous respiration. Two patients were returned via bag/valve/mask (BVM) support alone, two with BVM and oropharyngeal airway, and one via supraglottic airway. No surgical airways were required. Overall, we observed transient cases of hypotension (5.2%), hypoxemia (1.3%), or both (0.1%) in 6.6% of cases during the RSI procedure.
CONCLUSION:
A very high RSI procedural success rate was observed across the study period. This supports the growing recognition that appropriately trained paramedics can perform RSI safely in the prehospital environment.
| Tags : airway
22/09/2018
Echo pour l'intubation
Integration of Point-of-care Ultrasound during Rapid Sequence Intubation in Trauma Resuscitation.
Introduction:
Airway and breathing management play critical role in trauma resuscitation. Early identification of esophageal intubation and detection of fatal events is critical. Authors studied the utility of integration of point-of-care ultrasound (POCUS) during different phases of rapid sequence intubation (RSI) in trauma resuscitation.
Methods:
It was prospective, randomized single-centered study conducted at the Emergency Department of a level one trauma center. Patients were divided into ultrasonography (USG) and clinical examination (CE) arm. The objectives were to study the utility of POCUS in endotracheal tube placement and confirmations and identification of potentially fatal conditions as tracheal injury, midline vessels, paratracheal hematoma, vocal cord pathology, pneumothorax, and others during RSI. Patient >1 year of age were included. Time taken for procedure, number of incorrect intubations, and pathologies detected were noted. The data were collected in Microsoft Excel spread sheets and analyzed using Stata (version 11.2, Stata Corp, Texas, U. S. A) software.
Results:
One hundred and six patients were recruited. The mean time for primary survey USG versus CE arm was (20 ± 10.01 vs. 18 ± 11.03) seconds. USG detected four pneumothorax, one tracheal injury, and one paratracheal hematoma. The mean procedure time USG versus CE arm was (37.3 ± 21.92 vs. 58 ± 32.04) seconds. Eight esophageal intubations were identified in USG arm by POCUS and two in CE arm by EtCO2 values.
Conclusion:
Integration of POCUS was useful in all three phases of RSI. It identified paratracheal hematoma, tracheal injury, and pneumothorax. It also identified esophageal intubation and confirmed main stem tracheal intubation in less time compared to five-point auscultation and capnography.
| Tags : airway
21/09/2018
Airway Ultrasound
| Tags : airway
16/09/2018
Airway, pour être au RDV: S'entraîner
A Continuous Quality Improvement Airway Program Results in Sustained Increases in Intubation Success.
INTRODUCTION:
Airway management is a critical skill for air medical providers, including the use of rapid sequence intubation (RSI) medications. Mediocre success rates and a high incidence of complications has challenged air medical providers to improve training and performance improvement efforts to improve clinical performance.
OBJECTIVES:
The aim of this research was to describe the experience with a novel, integrated advanced airway management program across a large air medical company and explore the impact of the program on improvement in RSI success.
METHODS:
The Helicopter Advanced Resuscitation Training (HeART) program was implemented across 160 bases in 2015. The HeART program includes a novel conceptual framework based on thorough understanding of physiology, critical thinking using a novel algorithm, difficult airway predictive tools, training in the optimal use of specific airway techniques and devices, and integrated performance improvement efforts to address opportunities for improvement. The C-MAC video/direct laryngoscope and high-fidelity human patient simulation laboratories were implemented during the study period. Chi-square test for trend was used to evaluate for improvements in airway management and RSI success (overall intubation success, first-attempt success, first-attempt success without desaturation) over the 25-month study period following HeART implementation.
RESULTS:
A total of 5,132 patients underwent RSI during the study period. Improvements in first-attempt intubation success (85% to 95%, p < 0.01) and first-attempt success without desaturation (84% to 94%, p < 0.01) were observed. Overall intubation success increased from 95% to 99% over the study period, but the trend was not statistically significant (p = 0.311).
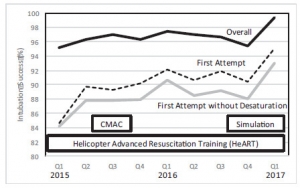
CONCLUSIONS:
An integrated advanced airway management program was successful in improving RSI intubation performance in a large air medical company.
| Tags : airway
01/06/2018
Curare pour intuber: Oui, mais aussi !
Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review.
Il est communément admis que l'emploi de curares facilite l'intubation et réduit les complications liées à ce geste. C'est bien ce que confirme cette publication. Mais cette dernière conclue également à l'importance de peser le risque bénéfice risque. Dans les conditions extrêmes d'isolement et de prise en charge de trauma maxillo-faciaux/cranien ballistique l'objectif principal doit rester l'oxygénation des blessés/accidentés. Si l'induction en séquence rapide reste la référence, l'éventualité d'une intubation sans curare sous anesthésie locale doit être évoquée en cas de risque d'impossibilité de ventilation manuelle ou spontanée et de difficulté d'intubation. Dans tous les cas il reste nécessaire de pouvoir réaliser un abord chirurgical des voies aériennes.
Lire ici les recommandations de la SFAR: Intubation difficile en anesthésie, en réanimation
---------------------------------------------
Cohort studies have indicated that avoidance of neuromuscular blocking agents (NMBA) is a risk factor for difficult tracheal intubation. However, the impact of avoiding NMBA on tracheal intubation, possible adverse effects, and postoperative discomfort has not been evaluated in a systematic review of randomised trials. We searched several databases for trials published until January 2017. We included randomised controlled trials comparing the effect of avoiding vs using NMBA. Two independent authors assessed risk of bias and extracted data. The risk of random errors was assessed by trial sequential analysis (TSA). We included 34 trials (3565 participants). In the four trials judged to have low risk of bias, there was an increased risk of difficult tracheal intubation with no use of NMBA [random-effects model, risk ratio (RR) 13.27, 95% confidence interval (CI) 8.19-21.49, P<0.00001, TSA-adjusted CI 1.85-95.04]. The result was confirmed when including all trials, (RR 5.00, 95% CI 3.49-7.15, P<0.00001, TSA-adjusted CI 1.20-20.77). There was a significant risk of upper airway discomfort or injury by avoiding NMBA (RR=1.37, 95% CI 1.09-1.74, P=0.008, TSA-adjusted CI 1.00-1.86). None of the trials reported mortality. Avoiding NMBA was significantly associated with difficult laryngoscopy, (RR 2.54, 95% CI 1.53-4.21, P=0.0003, TSA-adjusted CI 0.27-21.75). In a clinical context, one must balance arguments for using NMBA when performing tracheal intubation.
12/03/2018
Voies aériennes: L'expérience US OIF/OEF
BACKGROUND:
Airway management is of critical importance in combat trauma patients. Airway compromise is the second leading cause of potentially survivable death on the battlefield and accounts for approximately 1 in 10 preventable deaths. Reports from the Iraq and Afghanistan wars indicate 4-7% incidence of airway interventions on casualties transported to combat hospitals. The goal of this study was to describe airway management in the prehospital combat setting and document airway devices used on the battlefield.
METHODS:
This study is a retrospective review of casualties that required a prehospital life-saving airway intervention during combat operations in Afghanistan. We obtained data from the Prehospital Trauma Registry (PHTR) that was linked to the Department of Defense Trauma Registry (DoDTR) for outcome data for the time period between January 2013 and September 2014.
RESULTS:
705 total trauma patients were included, 16.9% required a prehospital airway management procedure. There were 132 total airway procedures performed, including 83 (63.4%) endotracheal intubations and 26 (19.8%) nasopharyngeal airway placements. Combat medics were involved in 48 (36.4%) of airway cases and medical officers in 73 (55.3%). Most (94.2%) patients underwent airway procedures due to battle injuries caused by explosion or gunshot wounds.
Casualties requiring airway management were more severely injured and less likely to survive as indicated by injury severity score, responsiveness level, Glascow coma score, and outcome.
CONCLUSIONS:
Percentages of airway interventions more than tripled from previous reports from the wars in Afghanistan and Iraq. These changes are significant and further study is needed to determine the causes. Casualties requiring airway interventions sustained more severe injuries and experienced lower survival than patients who did not undergo an airway procedure, findings suggested in previous reports.
11/02/2018
Airway: Prévention des complications
| Tags : airway
17/01/2018
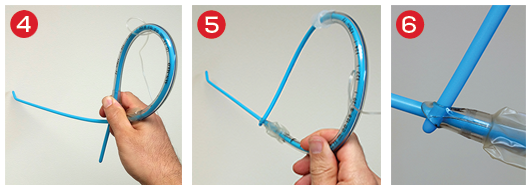
Histoire de mandrin
Il n'est parfois pas simple de bien maintenir un mandrin d'intubation dans le bon axe. Vous sont proposé en 3,4 et 5 plusieurs manières de s'en sortir.
17/12/2017
Réfllexions sur la balance Airway/complications
Strategies for the prevention of airway complications - a narrative review.
Despite being infrequent, complications of airway management remain an important contributor to morbidity and mortality during anaesthesia and care of the critically ill. Developments in the last three decades have made anaesthesia safer, and this has been mirrored in the equipment and techniques available for airway management. Modern technology including novel oxygenation modalities, widespread availability of capnography, second-generation supraglottic airway devices and videolaryngoscopy provide the tools to make airway management safer still. However, technology will only take safety so far, and non-technical aspects of airway management are critically important for communication and decision making during airway crises, acknowledging a 'cannot intubate, cannot oxygenate' situation and transitioning to emergency front of neck airway. Randomised controlled trials provide little useful information about safety in this setting, and data from registries and databases are likely to be of more value. This narrative review focuses on recent evidence in this area.
15/01/2017
ISR: Plutôt kétamine ?
Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia.
Lyon RM et Al. Crit Care. 2015 Apr 1;19:134
-------------------------------------------
Faut-il utiliser la kétamine ou l'étomidate ? Le travail présenté milite pour l'emploi de la kétamine, mais ceci reste controversé (voir également ici)). C'est aussi le choix présenté dans la procédure du sauvetage au combat, du fait de la polyvalence d'emploi de la kétamine tant dans ses indications que de ses voies d'administration. On rappelle quand même que si l'ISR facilite grandement les conditions de l'intubation oro-trachéale en médecine préhospitalière métropolitaine, nos conditions spécifiques d'exercice ne correspondent pas à cette dernière. Avant de réaliser une telle induction, encore faut-il être valider l'indication de l'intubation au milieu de nulle part. Par ailleurs la réalisation de ce geste sous anesthésie locale doit également être envisagée. Ceci est conforme aux recommandations sur le sujet.
-------------------------------------------
INTRODUCTION:
Rapid Sequence Induction of anaesthesia (RSI) is the recommended method to facilitate emergency tracheal intubation in trauma patients. In emergency situations, a simple and standardised RSI protocol may improve the safety and effectiveness of the procedure. A crucial component of developing a standardised protocol is the selection of induction agents. The aim of this study is to compare the safety and effectiveness of a traditional RSI protocol using etomidate and suxamethonium with a modified RSI protocol using fentanyl, ketamine and rocuronium.
METHODS:
We performed a comparative cohort study of major trauma patients undergoing pre-hospital RSI by a physician-led Helicopter Emergency Medical Service. Group 1 underwent RSI using etomidate and suxamethonium and Group 2 underwent RSI using fentanyl, ketamine and rocuronium. Apart from the induction agents, the RSI protocol was identical in both groups. Outcomes measured included laryngoscopy view, intubation success, haemodynamic response to laryngoscopy and tracheal intubation, and mortality.
RESULTS:
Compared to Group 1 (n = 116), Group 2 RSI (n = 145) produced significantly better laryngoscopy views (p = 0.013) and resulted in significantly higher first-pass intubation success (95% versus 100%; p = 0.007). A hypertensive response to laryngoscopy and tracheal intubation was less frequent following Group 2 RSI (79% versus 37%; p < 0.0001). A hypotensive response was uncommon in both groups (1% versus 6%; p = 0.05). Only one patient in each group developed true hypotension (SBP < 90 mmHg) on induction.
CONCLUSIONS:
In a comparative, cohort study, pre-hospital RSI using fentanyl, ketamine and rocuronium produced superior intubating conditions and a more favourable haemodynamic response to laryngoscopy and tracheal intubation. An RSI protocol using fixed ratios of these agents delivers effective pre-hospital trauma anaesthesia.
07/09/2016
Airway: S'y pencher avec sérieux
Emergency airway management – by whom and how ?
Sollid SJ et Al. Acta Anaesthesiol Scand. 2016 Oct;60(9):1185-7
---------------------------------------
Encore une publication qui insiste sur la formation à la gestion des voies aériennes et au maintien de ses compétences. Ceci n'est pas innée et s'impose tout d'abord non seulement aux praticiens peu confrontés à cette exercice, en première ligne les médecins urgentistes, mais aussi aux médecins anesthésistes compte tenu de l'essor de l'anesthésie loco-régionale et l'emploi de dispositifs supra-glottique. A lire et relire, ainsi que les références.
---------------------------------------
Procedures for advanced airway management are important for maintaining basic life functions in the unconscious patient, and can be lifesaving in critically ill or injured patients. In Acta Anaesthesiologica Scandinavica, a working group from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (SSAI) presents updated clinical guidelines on pre-hospital airway management.[1] The recommendations from the working group are important statements in the long-lasting quest to ensure that advanced airway management is managed safely pre-hospital at the right level of competence.
Technically, many of the procedures for advanced airway management of the average patient in controlled situations are easy to learn. Yet, a German study found that at least 200 intubation attempts were required to reach a 95% success rate.[2] The challenge, however, lies in assessing and managing the difficult airway cases. Emergency physicians with anaesthesiology background seem to be better at predicting difficult intubations than emergency physicians with other backgrounds, in addition to having significantly lower incidence of intubation problems and more experience in decisions on whether to intubate.[3]
Data from the UK show that the majority of complications in airway management occur in the emergency department and the intensive care unit. One of the reasons is the relatively low exposure to such procedures in these settings.[4] Studies on pre-hospital airway management also indicate that the rate of complications in this setting is high, and also that it is greatly dependent on the competence of the provider.[5] There is sufficient evidence to support that pre-hospital advanced airway management in the hands of trained anaesthesiologists is a safe procedure.[6-8] However, as other authors have pointed out, being a proficient provider of airway management is not equivalent with being an anaesthesiologist.[9] The combination of competencies to assess the situation, practical skills and ability to manage complications are more important than the name of the provider's speciality. In a physician-staffed helicopter emergency medical service in the UK, where doctors are a mix of anaesthesiologists and emergency physicians, the success rates are still high and complications are low.[10] This is probably related to the strict training and highly standardised operating procedures that all doctors must adhere to.
Based on this, advanced airway management seems to be safe if the providers have a large volume of clinical experience (anaesthesiologists) or alternatively, operate under strict clinical guidance and protocol rule (non-anaesthesiologists). Intuitively, a combination of both could probably improve safety further and would be useful in clinical environments, and particularly when airway management occurs as unplanned events with little or no time for individual planning and screening of the patient.
The most recent consensus-based European Guidelines for Postgraduate Training in Anaesthesiology recommend the change from duration of training and number of procedures into competence-based training.[11] These competences include advanced airway management skills. Some of this training can be done in simulation settings, but simulation cannot replace real-life situations.[12, 13] Once learnt, competences must be maintained. That requires regular exposure to the procedure. As the use of laryngeal masks and regional blocks increases at the expense of anaesthesia procedures including endotracheal intubation, the training opportunities for all providers, including anaesthesia personnel is being reduced. That is one of the reasons why the Section and Board of Anaesthesiology of the European Union of Medical Specialists recommended a multispecialty approach to emergency medicine.[14] Like the Scandinavian Society of Anaesthesiology and Intensive Care recommended in 2010,[15] the European Society of Anaesthesiology is increasingly using the term ‘Critical Emergency Medicine’ for the part of the anaesthesiology speciality that all anaesthesiologists should command.
A Nordic working group published a literature review in 2008 on pre-hospital airway management, and proposed an evidence-based guideline.[16] This position paper concludes unanimously that pre-hospital emergency airway management in the appropriate patient groups should be achieved by rapid sequence induction and endotracheal intubation, provided the physician is an anaesthesiologist. Other providers should treat the same patient group in the lateral trauma recovery position and if necessary, provide assisted bag-valve-mask ventilation. Supraglottic airway devices were recommended for non-anaesthesiologists in cardiac arrest with a need for supine positioning of the patient, and as a backup device for anaesthesiologists. These findings have been reaffirmed in the new SSAI clinical practice guideline published in August issue.[1]
A similar paper concerning Scandinavian clinical practice guidelines on general anaesthesia for emergency situations underlines the dangers associated with administering anaesthesia outside the operating theatre. They too advocate that anaesthesia for emergency patients should be given by, or under very close supervision by, experienced anaesthesiologists, and stress that problems with the airway are to be anticipated.[17]
Emergency airway management outside the operating theatres carries a high risk of difficult intubation, in a recent study 10.3%, and these patients have a high risk of complications.[18] This demonstrate the need for particular vigilance in and training for these settings, and provides another argument for using supraglottic approaches for those patients in the hands of non-anaesthesiologists. A recent report from the Johns Hopkins Hospital describes a successful attempt to mitigate difficult airway situations arising within this highly specialised hospital. By the formation of a difficult airway response team, the researchers conquered difficult airway situations which until the intervention ranked among the top five adverse events in Maryland.[19]
In conclusion, emergency airway management carries a high risk of patient injury, even among highly trained and skilled anaesthesiologists. Airway management can be learned, and emergency airway handling can be performed with maintained safety also by non-anaesthesiologists, provided they operate in a highly supervised and algorithm-based environment.[9] In this light, the emerging new emergency medical specialty in the Scandinavian countries is of concern, if these acute or emergency physicians are supposed to perform emergency airway procedures independent of their anaesthesiologist colleagues. Whoever manages the compromised airway in the pre-hospital setting is required to do so with the highest level of quality, attainable through a combination of clinical experience and clinical governance. It is difficult to see how this can be achieved and maintained outside the specialty of anaesthesiology. In the end, this is a matter of patient safety, not competition for airways.
| Tags : airway
31/08/2016
Echo et voies aériennes: Mais oui, à maîtriser
The Role of Airway and Endobronchial Ultrasound in Perioperative Medicine
Vortrua J et Al. Biomed Res Int. 2015; 2015: 754626
-------------------------------
Certainement UN APPORT IMPORTANT à la gestion des voies aériennes et de la ventilation non seulement dans les blocs opératoires mais dans les situations critiques y compris hors de l'hôpital.
-------------------------------
Recent years have witnessed an increased use of ultrasound in evaluation of the airway and the lower parts of the respiratory system. Ultrasound examination is fast and reliable and can be performed at the bedside and does not carry the risk of exposure to ionizing radiation. Apart from use in diagnostics it may also provide safe guidance for invasive and semi-invasive procedures. Ultrasound examination of the oral cavity structures, epiglottis, vocal cords, and subglottic space may help in the prediction of difficult intubation. Preoperative ultrasound may diagnose vocal cord palsy or deviation or stenosis of the trachea. Ultrasonography can also be used for confirmation of endotracheal tube, double-lumen tube, or laryngeal mask placement. This can be achieved by direct examination of the tube inside the trachea or by indirect methods evaluating lung movements. Postoperative airway ultrasound may reveal laryngeal pathology or subglottic oedema. Conventional ultrasound is a reliable real-time navigational tool for emergency cricothyrotomy or percutaneous dilational tracheostomy. Endobronchial ultrasound is a combination of bronchoscopy and ultrasonography and is used for preoperative examination of lung cancer and solitary pulmonary nodules. The method is also useful for real-time navigated biopsies of such pathological structures.
| Tags : airway
29/08/2016
Echographie: Un outil pour la gestion des VAS
Role of upper airway ultrasound in airway management
Osman A. et Al. Osman and Sum Journal of Intensive Care (2016) 4:52
Upper airway ultrasound is a valuable, non-invasive, simple, and portable point of care ultrasound (POCUS) for evaluation of airway management even in anatomy distorted by pathology or trauma. Ultrasound enables us to identify important sonoanatomy of the upper airway such as thyroid cartilage, epiglottis, cricoid cartilage, cricothyroid membrane, tracheal cartilages, and esophagus. Understanding this applied sonoanatomy facilitates clinician to use ultrasound in assessment of airway anatomy for difficult intubation, ETT and LMA placement and depth, assessment of airway size, ultrasound-guided invasive procedures such as percutaneous needle cricothyroidotomy and tracheostomy, prediction of postextubation stridor and left double-lumen bronchial tube size, and detecting upper airway pathologies. Widespread POCUS awareness, better technological advancements, portability, and availability of ultrasound in most critical areas facilitate upper airway ultrasound to become the potential first-line non-invasive airway assessment tool in the future.
| Tags : intubation
14/07/2016
Soleil et chaleur: plutôt gênant
Prehospital Endotracheal Intubation in Warm Climates: Caution is Required
-------------------------------------------------
Une chose bien connue et très clairement explicitée:
-------------------------------------------------
BACKGROUND:
Out-of-hospital endotracheal intubation is a frequent procedure for trauma care. Nevertheless, in warm climates, sunlight and heat can interfere with the flow of the usual procedure. They can affect the equipment and hinder the operator. There are few data on this issue. The presentation of this case highlights three common complications that may occur when intubating under a hot and bright sun.
CASE REPORT:
A 23-year-old man had a car accident in Djibouti, at 11:00 a.m., in broad sunlight. The heat was scorching. Due to a severe head trauma, with a Glasgow Coma Scale score of 8, it was decided to perform an endotracheal intubation. The operator faced three problems: the difficulty of seeing inside the mouth in the bright sunlight, the softening of the tube under the influence of the heat, and the inefficiency of colorimetric CO2 detectors in the warm atmosphere in confirming the proper endotracheal tube placement.
WHY SHOULD AN EMERGENCY PHYSICIAN BE AWARE OF THIS?:
Solutions are simple, but must be known and planned ahead, prior to beginning the procedure: Putting a jacket over his head while doing the laryngoscopy would solve the problem of dazzle; adjuncts like a stylet or gum elastic bougie have to be used at the outset to fix the softening problem; alternative methods to exhaled CO2 detection, such as the syringe aspiration technique, to confirm the proper tube placement, should be available.
22/06/2016
AL pour intuber: A ressortir de l'oubli
The Myth of Rescue Reversal in “Can’t Intubate, Can’t Ventilate” Scenarios
Naguib N. et Al. Anesth Analg. 2016 Jul;123(1):82-92
__________________________
Ce travail met en avant l'insuffisance des démarches d'antagonisation pour restaurer une ventilation adéquate dans les situations de CICV. En ce qui concerne la gestion des voies aériennes en situation tactique, le principe de la préservation de la ventilation spontanée lors de l'accès aux voies aériennes mérite d'être rappelé. Si la réalisation d'une induction en séquence rapide reste la référence, en cas de difficulté prévisible le recours à une anesthésie locale doit être préférée (lire ce post).
Ceci est parfaitement stipulé dans les RFE "Sédation et analgésie en structure d’urgence" dont on rappelle après la présentation de l'abstract les termes de la question N3.
__________________________
BACKGROUND:
An unanticipated difficult airway during induction of anesthesia can be a vexing problem. In the setting of can't intubate, can't ventilate (CICV), rapid recovery of spontaneous ventilation is a reasonable goal. The urgency of restoring ventilation is a function of how quickly a patient's hemoglobin oxygen saturation decreases versus how much time is required for the effects of induction drugs to dissipate, namely the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade. It has been suggested that prompt reversal of rocuronium-induced neuromuscular blockade with sugammadex will allow respiratory activity to recover before significant arterial desaturation. Using pharmacologic simulation, we compared the duration of unresponsiveness, ventilatory depression, and neuromuscular blockade in normal, obese, and morbidly obese body sizes in this life-threatening CICV scenario. We hypothesized that although neuromuscular function could be rapidly restored with sugammadex, significant arterial desaturation will occur before the recovery from unresponsiveness and/or central ventilatory depression in obese and morbidly obese body sizes.
METHODS:
We used published models to simulate the duration of unresponsiveness and ventilatory depression using a common induction technique with predicted rates of oxygen desaturation in various size patients and explored to what degree rapid reversal of rocuronium-induced neuromuscular blockade with sugammadex might improve the return of spontaneous ventilation in CICV situations.
RESULTS:
Our simulations showed that the duration of neuromuscular blockade was longer with 1.0 mg/kg succinylcholine than with 1.2 mg/kg rocuronium followed 3 minutes later by 16 mg/kg sugammadex (10.0 vs 4.5 minutes). Once rocuronium neuromuscular blockade was completely reversed with sugammadex, the duration of hemoglobin oxygen saturation >90%, loss of responsiveness, and intolerable ventilatory depression (a respiratory rate of ≤4 breaths/min) were dependent on the body habitus and duration of oxygen administration. There is a high probability of intolerable ventilatory depression that extends well beyond the time when oxygen saturation decreases <90%, especially in obese and morbidly obese patients. If ventilatory rescue is inadequate, oxygen desaturation will persist in the latter groups, despite full reversal of neuromuscular blockade. Depending on body habitus, the duration of intolerable ventilatory depression after sugammadex reversal may be as long as 15 minutes in 5% of individuals.
CONCLUSIONS:
The clinical management of CICV should focus primarily on restoration of airway patency, oxygenation, and ventilation consistent with the American Society of Anesthesiologist's practice guidelines for management of the difficult airway. Pharmacologic intervention cannot be relied upon to rescue patients in a CICV crisis.
__________________________
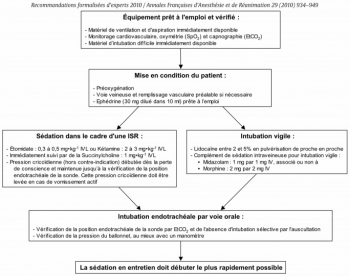
Question 3 - Intubation sous ISR et sous AL : Quelles sont les modalités de réalisation d’une sédation et/ou d’une analgésie pour l’intubation trachéale ?
Les experts recommandent d’administrer une sédation pour toutes les indications de l’intubation trachéale, excepté chez le patient en arrêt cardiaque qui ne nécessite pas de sédation. Lorsque l’intubation trachéale est présumée diffi cile, il est possible d’effectuer une anesthésie locale réalisée de proche en proche, associée ou non à une sédation légère et titrée par voie générale
L’utilisation de médicaments anesthésiques lors de l’intubation trachéale a pour but de faciliter le geste et d’assurer le confort du patient. Cette sédation doit être rapidement réversible pour restaurer une ventilation effi cace en cas de diffi culté d’intubation. Le risque d’inhalation bronchique doit être minimisé au cours de la procédure et ce d’autant que les patients sont considérés comme ayant un estomac plein.
Les experts recommandent d’utiliser les techniques d’intubation en séquence rapide (ISR) associant un hypnotique d’action rapide (étomidate ou kétamine) et un curare d’action brève (succinylcholine) ........................................................
Lorsque l’intubation trachéale est présumée difficile, le protocole recommandé par les experts pour une intubation vigile est le suivant : - Lidocaïne entre 2 et 5% en pulvérisation de proche en proche - Complément de sédation intraveineuse pour intubation vigile : • midazolam : 1 mg par 1 mg IV • associé ou non à de la morphine : 2 mg par 2 mg IV
05/06/2016
Echographie pour l'intubation: Plutôt oui.
Tracheal ultrasonography and ultrasonographic lung sliding for confirming endotracheal tube placement: Speed and Reliability
BACKGROUND:
In this study we aimed to evaluate the success of ultrasonography (USG) for confirming the tube placement and timeliness by tracheal USG and ultrasonographic lung sliding in resuscitation and rapid sequence intubation.
MATERIALS AND METHODS:
This study was a prospective, single-center, observational study conducted in the emergency department of a tertiary care hospital. Patients were prospectively enrolled in the study. Patients who went under emergency intubation because of respiratory failure, cardiac arrest or severe trauma included in the study. Patients with severe neck trauma, neck tumors, history of neck operation or tracheotomy and under 18years old were excluded from the study.
RESULTS:
A total of 115 patients included in the study. The mean age was 67.2±17.1 with age 16-95years old. Among 115 patients 30 were cardiac arrest patients other 85 patients were non-cardiac arrest patients intubated with rapid sequence intubation. The overall accuracy of the ultrasonography was 97.18% (95% CI, 90.19-99.66%), and the value of kappa was 0.869 (95% CI, 0.77-0.96), indicating a high degree of agreement between the ultrasonography and capnography. The ulrasonography took significantly less time than capnography in total.
DISCUSSION:
Ultrasonography achieved high sensitivity and specificity for confirming tube placement and results faster than end-tidal carbon dioxide. Ultrasonography is a good alternative for confirming the endotracheal tube placement. Future studies should examine the use of ultrasonography as a method for real-time assessment of endotracheal tube placement by emergency physicians with only basic ultrasonographic training.
| Tags : airway, échographie
24/01/2016
Succinylcholine et frigo: Non fondé ?
Froid et suxaméthonium : une recommandation non fondée
Dewachter P et AL. Ann. Fr. Med. Urgence DOI 10.1007/s13341-015-0600-1
Morceaux choisis:
L’Agence nationale de sécurité du médicament et des produits de santé (ANSM) a publié en 2012 une recommandation destinée aux médecins anesthésistes-réanimateurs et urgentistes décrivant les conditions d’utilisation du chlorure de suxaméthonium. .......Cette recommandation faisait suite à une enquête rétrospective de pharmacovigilance sur les réactions allergiques induites par les curares qui mettait en évidence une augmentation des notifications de réactions allergiques attribuées au suxaméthonium........Néanmoins, l’hypothèse émise par l’ANSM ne résiste pas à l’évaluation scientifique. En effet, aucune étude n’a démontré que le suxaméthonium conservé à température ambiante favorise la survenue d’une réaction allergique, ce qui avait déjà été souligné lors de la publication de cette recommandation..........................En revanche, depuis 20 ans, plusieurs équipes européennes et nord-américaines ont confirmé la stabilité des solutions de chlorure de suxaméthonium à température ambiante ou lors de variations extrêmes de température................... La succinylcholine (50 mg/mL) préservée dans l’ampoule est stable pendant deux mois à température ambiante (25°C) [5] alors que la solution à 20 mg/mL reste stable au moins sept jours après exposition à des variations extrêmes de température (de -6°C à +54°C).......................Par ailleurs, la solution de succinylcholine (20 mg/mL) conservée dans une seringue en plastique est stable trois mois à 25°C et deux mois à 40°C . Enfin, la stabilité de la succinylcholine stockée à bord d’ambulances, respectivement pendant sept mois [8] et un an , a été évaluée après exposition aux variations climatiques auxquelles ces équipes sont exposées. La succinylcholine (20 mg/mL) est stable pendant environ trois mois quand elle est soumise à des températures moyennes variant de -9°C à +32°C [8] alors que la solution à 100 mg/mL est stable pendant un peu plus d’un mois quand elle est exposée de -8°C à +36°C. D’autres études ont également confirmé la stabilité de la succinylcholine (10 mg/ml) dans une seringue en plastique pendant sept jours [9] et pendant au moins cinq mois, quand celle-ci est conservée dans l’ampoule (20 et 50 mg/ml) ..........Plus récemment, la stabilité de la succinylcholine à température ambiante (25°C) a été confirmée par l’ANSM pour qui les résultats obtenus sont « conformes aux spécifications à péremption décrites dans le dossier d’AMM................Ce rapport de conclure que « les données relatives à la qualité ne semblent donc pas être en mesure d’expliquer l’augmentation des réactions anaphylactiques sur la période étudiée............Le turn-over prévisible de l’utilisation du suxaméthonium stocké à température ambiante rend ainsi son utilisation possible par les équipes de Samu. En effet, l’éventuelle morbidité – voire mortalité – induite par cette recommandation ne peut être occultée. Nombreux sont les patients qui devant bénéficier d’une induction à séquence rapide, ont été intubés sans curare par les équipes qui ne disposaient pas d’un réfrigérateur à bord alors que l’appréciation de la balance risque/ bénéfice penche en faveur de l’utilisation du suxaméthonium dans cette situation clinique
Gammon DL, et al (2008) Alteration in prehospital drug concentration after thermal exposure. Am J Emerg Med 26:566–73.
| Tags : intubation
23/01/2016
Maîtriser l'airway +++, entre autres
Augmentation of point of injury care: Reducing battlefield
mortality—The IDF experience
Benov A. et Al. Injury. 2015 Nov 18. pii: S0020-1383(15)00697-X. doi: 10.1016/j.injury.2015.10.078.
------------------------------
Une publication particulièrement intéressante car elle émane de collègues militaires qui interviennent dans un contexte très particulier de prise en charge de blessés tels qu'on peut les rencontrer en opérations extérieures mai dans un contexte de réseau de traumatologie civile puisque que les hôpitaux de recueil de ces blessés sont les hôpitaux civils. Les données présentées ne portent que sur la prise en charge de combattants.
Un des points analysé est la performance des équipes dans certains gestes considérés comme essentiel, notamment la gestion des voies aériennes. Comme dans l'armée française l'intubation orotrachéale et la criciothyrotomie représentent les deux procédures mises en oeuvre par des médecins. Manifestement, il existe une grande maîtrise de la coniotomie alors que celle de l'Intubation est moins évidente: 41% de succès et une moyenne de 2 tentatives. Ceci reste problématique lorsque la prise en charge des blessés se fait loin d'un trauma center et qu'il faut envisager la gestion de ces voies aériennes et l'initiation d'une ventilation pendant plusieurs heures (jours ?). Pour ces raisons et même si la probabilité d'être confronté à une telle situation est faible, ce travail rapporte les 2/3 des blessés ne sont pas urgent et que 5% seulement des nécessitent un geste sur les voies aériennes, il s'agit d'un point fondamental en matière de réduction de morts indues.
------------------------------
STUDY OBJECTIVE:
In 2012, the Israel Defense Forces Medical Corps (IDF-MC) set a goal of reducing mortality and eliminating preventable death on the battlefield. A force buildup plan entitled "My Brother's Keeper" was launched addressing: trauma medicine, training, change of Clinical Practice Guidelines (CPGs), injury prevention, data collection, global collaboration and more. The aim of this article is to examine how military medical carehas evolved due "My Brother's Keeper" between Second Lebanon War (SLW, 2006) to Operation Protective Edge (OPE, 2014).
METHODS:
Records of all casualties during OPE and SLW were extracted and analyzed from the I.D.F Trauma Registry. Noncombat injuries and civilian injuries from missile attacks were excluded from this analysis.
RESULTS:
The plans main impacts were; incorporation of a physician or paramedic as an integral part of each fighting company, implementation of new CPGs, introduction of new approaches for extremity haemorrhage control and Remote Damage Control Resuscitation at point of injury (POI) using single donor reconstituted freeze dried plasma (25 casualties) and transexamic acid (98 casualties). During OPE, 704 soldiers sustained injuries compared with 833 casualties during SLW. Fatalities were 65 and 119, respectively, cumulating to Case Fatality Rate of 9.2% and 14.3%, respectively.
CONCLUSIONS:
Significant changes in the way the IDF-MC provides combat casualty care have been made in recent years. It is the transformation from concept to doctrine and integration into a structured and Goal-Oriented Casualty Care System, especially POI care that led to the unprecedented survival rates in IDF as shown in this conflict.
| Tags : airway