12/12/2025
Récapitulatif sur le remplissage vasculaire/Transfusion
Fluid resuscitation in trauma: What you need to know
Navpreet D et Al. Journal of Trauma and Acute Care Surgery 98(1):p 20-29, January 2025.
There have been numerous changes in resuscitation strategies for severely injured patients over the last several decades. Certain strategies, such as aggressive crystalloid resuscitation, have largely been abandoned because of the high incidence of complications and worsening of trauma-induced coagulopathy. Significant emphasis has been placed on restoring a normal coagulation profile with plasma or whole blood transfusion. In addition, the importance of the lethal consequences of trauma-induced coagulopathy, such as hyperfibrinolysis, has been easily recognized by the use of viscoelastic testing, and its treatment with tranexamic acid has been extensively studied. Furthermore, the critical role of early intravenous calcium administration, even before blood transfusion administration, has been emphasized.

Other adjuncts, such as fibrinogen supplementation with fibrinogen concentrate or cryoprecipitate and prothrombin complex concentrate, are being studied and incorporated in some of the institutional massive transfusion protocols. Finally, balanced blood component transfusion (1:1:1 or 1:1:2) and whole blood have become commonplace in trauma centers in North America. This review provides a description of recent developments in resuscitation and a discussion of recent innovations and areas for future investigation.
28/03/2024
CHoc hypovolémqiue: Un nouveau venu, ? peut-être.
03/04/2023
Sang de banque sur pied: Mieux si on est entraîné
A prospective assessment of the medic autologous blood transfusion skills for field transfusion preparation
Steven G Schauer SG et Al. Transfusion. 2023 Mar 27. doi: 10.1111/trf.17325.
Background: Data demonstrate benefit from blood product administration near point-of-injury (POI). Fresh whole blood transfusion from a pre-screened donor provides a source of blood at the POI when resources are constrained. We captured transfusion skills data for medics performing autologous blood transfusion training.
Methods: We conducted a prospective, observational study of medics with varying levels of experience. Inexperienced medics were those with minimal or no reported experience learning the autologous transfusion procedures, versus reported experience among special operations medics. When available, medics were debriefed after the procedure for qualitative feedback. We followed them up to 7 days for adverse events.
Results: The median number of attempts for inexperienced and experienced medics was 1 versus 1 (interquartile range 1-1 for both, p=0.260). The inexperienced medics had a slower median time to needle venipuncture access for donation of 7.3 versus 1.5 minutes, needle removal after clamping time of 0.3 versus 0.2 minutes, time to bag preparation of 1.9 versus 1.0 minutes, time to IV access for reinfusion of 6.0 versus 3.0 minutes, time to transfusion completion of 17.3 versus 11.0 minutes, and time to IV removal of 0.9 versus 0.3 minutes (all p<0.05). We noted one administrative safety event in which allogeneic transfusion occurred. No major adverse events occurred. Qualitative data saturated around the need for quarterly training.
Conclusions: Inexperienced medics have longer procedure times when training autologous whole blood transfusion skills. This data will help establish training measures of performance for skills optimization when learning this procedure.
01/12/2022
France: Transfusion en Opex
An observational study of the blood use in combat casualties of the French Armed Forces, 2013–2021
Py N. et Al. Transfusion. 2022;1–14.
Background:
The French Armed Forces conduct asymmetric warfare in the Sahara-Sahel Strip. Casualties are treated with damage control resuscitation to the extent possible. Questions remain about the feasibility and sustainability of using blood for wider use in austere environments.
Methods:
We performed a retrospective analysis of all French military trauma patients transfused after injury in overseas military operations in Sahel-Saharan Strip, from the point of injury, until day 7, between January 11, 2013 to December 31, 2021.
Results:
Forty-five patients were transfused. Twenty-three (51%) of them required four red blood cells units (RBC) or more in the first 24H defining a severe hemorrhage. The median blood product consumption within the first 48 h, was 8 (IQR [3; 18]) units of blood products (BP) for all study population but up to 17 units (IQR [10; 27.5]) for the trauma patients with severe hemor- rhage. Transfusion started at prehospital stage for 20 patients (45%) and included several blood products: French lyophilized plasma, RBCs, and whole blood. Patients with severe hemorrhage required a median of 2 [IQR 0; 34] fur- ther units of BP from day 3 to day 7 after injury. Eight patients died in theater, 4 with severe hemorrhage and these 4 used an average of 12 products at Role 1 and 2.
Conclusion:
The transfusion needs were predominant in the first 48 h after the injury but also continued throughout the first week for the most severe trauma patients. Importantly, our study involved a low-intensity conflict, with a small number of injured combatants.
07/11/2022
Remplissage vasculaire: Quid dans la vrai vie US ?
Trends in Prehospital Blood, Crystalloid, and Colloid Administration in Accordance With Changes in Tactical Combat Casualty Care Guidelines
Clarke E E. et Al. Military Medicine, Volume 187, Issue 11-12, November-December 2022, Pages e1265–e1270,
Introduction
Hemorrhage is the leading threat to the survival of battlefield casualties. This study aims to investigate the types of fluids and blood products administered in prehospital trauma encounters to discover the effectiveness of Tactical Combat Casualty Care (TCCC) recommendations.
Materials and Methods
This is a secondary analysis of a previously described dataset from the Department of Defense Trauma Registry with a focus on prehospital fluid and blood administration in conjunction with changes in the TCCC guidelines. We collected demographic information on each patient. We categorized receipt of each fluid type and blood product as a binary variable for each casualty and evaluated trends over 2007–2020 both unadjusted and controlling for injury severity and mechanism of injury.
Results
Our original dataset comprised 25,897 adult casualties from January 1, 2007 through March 17, 2020. Most (97.3%) of the casualties were male with a median age of 25. Most (95.5%) survived to hospital discharge, and 12.2% of the dataset received fluids of any kind. Medical personnel used crystalloids in 7.4% of encounters, packed red blood cells in 2.0%, and whole blood in 0.5% with very few receiving platelets or freeze-dried plasma. In the adjusted model, we noted significant year-to-year increases in intravenous fluid administration from 2014 to 2015 and 2018 to 2019, with significant decreases noted in 2008–2009, 2010–2012, and 2015–2016. We noted no significant increases in Hextend used, but we did note significant decreases in 2010–2012. For any blood product, we noted significant increases from 2016 to 2017, with decreases noted in 2009–2013, 2015–2016, and 2017–2018. Overall, we noted a general spike in all uses in 2011–2012 that rapidly dropped off 2012–2013. Crystalloids consistently outpaced the use of blood products. We noted a small upward trend in all blood products from 2017 to 2019.
Conclusions
Changes in TCCC guidelines did not immediately translate into changes in prehospital fluid administration practices. Crystalloid fluids continue to dominate as the most commonly administered fluid even after the 2014 TCCC guidelines changed to use of blood products over crystalloids. There should be future studies to investigate the reasons for delay in guideline implementation and efforts to improve adherence.
| Tags : remplissage, transfusion
14/02/2022
IO: Attention Embolie graisseuse ?
Intraosseous fluid resuscitation causes systemic fat emboli in a porcine hemorrhagic shock model
Kristiansen S. et Al. Scand J Trauma Resusc Emerg Med . 2021 Dec 20;29(1):172.
Background: Intraosseous cannulation can be life-saving when intravenous access cannot be readily achieved. However, it has been shown that the procedure may cause fat emboli to the lungs and brain. Fat embolization may cause serious respiratory failure and fat embolism syndrome. We investigated whether intraosseous fluid resuscitation in pigs in hemorrhagic shock caused pulmonary or systemic embolization to the heart, brain, or kidneys and if this was enhanced by open chest conditions.
Methods: We induced hemorrhagic shock in anesthetized pigs followed by fluid-resuscitation through bilaterally placed tibial (hind leg) intraosseous cannulas. The fluid-resuscitation was limited to intraosseous or i.v. fluid therapy, and did not involve cardiopulmonary resuscitation or other interventions. A subgroup underwent median sternotomy with pericardiectomy and pleurotomy before hemorrhagic shock was induced. We used invasive hemodynamic and respiratory monitoring including Swan Ganz pulmonary artery catheter and transesophageal echocardiography and obtained biopsies from the lungs, heart, brain, and left kidney postmortem.
Results: All pigs exposed to intraosseous infusion had pulmonary fat emboli in postmortem biopsies. Additionally, seven of twenty-one pigs had coronary fat emboli. None of the pigs with open chest had fat emboli in postmortem lung, heart, or kidney biopsies. During intraosseous fluid-resuscitation, three pigs developed significant ST-elevations on ECG; all of these animals had coronary fat emboli on postmortem biopsies.
Conclusions: Systemic fat embolism occurred in the form of coronary fat emboli in a third of the animals who underwent intraosseous fluid resuscitation. Open chest conditions did not increase the incidence of systemic fat embolization.
| Tags : intraosseux
20/01/2022
Fluid Resuscitation in Tactical Combat Casualty Care. Update 201
Fluid Resuscitation in Tactical Combat Casualty Care
TCCC Guidelines Change 21-01
4 November 2021
Dans ce document le mot important est choc hémorragique. Ce n'est pas parce q'un blessé saigne qu'il est en état de choc.
| Tags : choc, hémorragie, transfusion
04/12/2019
HEA 130: Protègerait le glycocalyx ?
The protective effect of hydroxyethyl starch solution on the glycocalyx layer in an acute hemorrhage mouse model.
- --------------------------------------------------------
Le recours au HEA pour le remplissage vasculaire est très décrié notamment à cause d'effets rénaux délétères observés tout particulièrement en cas de sepsis. Les HEA peuvent néanmoins être utilisés en cas de non restauration de l'hémodynamique après emploi de cristalloides isotoniques et en attendant les produits de transfusion (reco 6 de la RFE sur le choc hémorragique). Ce travail semble donc tempérer un peu le rejet des HEA pour la réanimation du choc hémorragique. Il montre une moindre élévation de syndecan-1 lors de l'emploi d'HEA 130 qu'après Salé.
--------------------------------------------------------
PURPOSE:
Fluid therapy focused on glycocalyx (GCX) protection in hemorrhagic shock is a current focus of research. Hydroxyethyl starch (HES) solution is commonly used for fluid resuscitation; however, its effects on the GCX remain unclear. The primary aim of this study was to explore the protective effect of HES130 in maintaining GCX thickness and reducing plasma syndecan-1 expression.
METHODS:
An acute hemorrhage murine model with the dorsal skin chambers was used to measure GCX thickness and to evaluate vascular permeability. Groups of mice were treated with normal saline (NS), albumin (NS-A), HES130 (NS-V), or no exsanguination or infusion (C). We measured syndecan-1 plasma concentrations, performed blood gas analysis, and analyzed the 7-day cumulative mortality.
RESULTS:
GCX thickness in NS mice was significantly reduced compared to that in group C, but no other groups showed a difference compared to group C. The plasma concentration of syndecan-1 was significantly higher in NS mice than in group C. There were no significant differences in the fluorescence intensity of dextran in the interstitial space. HES70 leakage was suppressed in NS-V mice compared to those in other groups. HES70 was localized to the inner vessel wall in C, NS, and NS-A mice, but not in group NS-V. Blood gas analysis indicated that pH and lactate showed the greatest improvements in NS-V mice. The 7-day cumulative mortality rate was the highest in group NS.
CONCLUSION:
Resuscitation with HES130 protected the GCX and suppressed vascular permeability of HES70 during early stages of acute massive hemorrhage.
09/04/2019
Substituts au sang: Ils arrivent !
Artificial oxygen carriers- past, present and the future-a review of the most innovative and clinically relevant concepts.
--------------------------
La question du transport de l'oxygène est fondamentale pour le traumatisé sévère. La recherche de transporteurs artificiels d'oxygène sont un axe fondamental de la recherche. Il se trouve qu'une entreprise bretonne fait partie des quelques équipes travaillant sur le sujet (voir ici)
--------------------------
Blood transfusions are daily practice in hospitals. As these products are limited in availability and have various, harmful side-effects, researchers have pursued the goal to develop artificial blood components for about 40 years. Development of oxygen therapeutics and stem cells are more recent goals. Medline, clinicaltrials.gov, clinicaltrialsregister.eu and ANZCTR were searched up to November 2017 using search terms related to artificial blood products to identify new and ongoing research of the last 5 years. For already well-known products that are, however, important to the field or relevant to gain a better understanding, the reader is punctually referred to some important articles older than 5 years. This review includes not only clinically relevant substances such as heme-oxygenating carriers (HBOCs), PFOCs, stem cells and organ conservation, but also interesting pre-clinically advanced compounds depicting the pipeline of potential new products. In- depths insights into specific benefits and limitations of each substance, including the biochemical and physiological background are included. "Fancy" ideas such as Iron-based substances, O2-microbubbles, cyclodextranes or lugworms are also elucidated. To conclude, this systematic up-to-date review includes all actual achievements and ongoing clinical trials in the field of artificial blood products to pursue the dream of artificial oxygen carrier supply. Research is on the right track, but the task is demanding and challenging.
01/04/2019
Oxsealife: LE cristalloïde de demain ?
Blood transfusion is given according to haemoglobin thresholds aimed at restoration of arterial oxygen-carrying capacity. Patient survival after severe haemorrhagic shock depends on restoration of microvascular perfusion, tissue oxygen delivery, endothelial function and organ integrity. We investigated a novel crystalloid fluid designed for tissue oxygen delivery, Oxsealife® , with components that generate microvascular nitric oxide and scavenge reactive oxygen species generated during ischaemia-reperfusion injury. The amount of dissolved oxygen in blood progressively increased during step-wise in vitro haemodilution with this fluid, suggesting that the oxygen solubility coefficient of blood is dynamic, not static. We performed a pilot safety and efficacy study to compare resuscitation with this novel crystalloid vs. whole blood transfusion in a swine haemorrhagic shock model with animals bled to an arterial lactate oxygen debt target. Despite contributing no haemoglobin, viscosity nor oncotic potential, resuscitation with Oxsealife after severe haemorrhagic shock restored central haemodynamic parameters comparable to stored allogeneic blood transfusion. Tissue perfusion, oxygenation and metabolic outcomes were equivalent between treatment groups. Increased consumption of bicarbonate in animals given Oxsealife suggested greater capillary recruitment and enhanced clearance of acidic tissue metabolites. Serum markers of organ function, animal activity during recovery and histological analysis of tissue morphology and endothelial glycocalyx integrity confirmed functional recovery from haemorrhagic shock. We conclude that recovery of tissue oxygen delivery and organ function after haemorrhagic shock may not be dependent on treatments that increase haemoglobin levels. Oxsealife shows promise for treatment of severe haemorrhagic shock and may reduce the requirement for allogeneic blood products.
01/12/2017
Transfusion à l'avant: Surtout Plyo, et le sang ?
Early transfusion on battlefield before admission to role 2: A preliminary observational study during “Barkhane” operation in Sahel
Vitalys V. et Al. https://doi.org/10.1016/j.injury.2017.11.029
---------------------------------------
Ce document rapporte essentiellement l'emploi de PLyo chez des blessés de guerre avant leur prise en charge en role 2. Beaucoup est écrit sur la faisabilité d'une telle pratique. On rappelle que l'emploi du plasma lyophilisé n'est pas une nouveauté y compris en milieu précaire (1). Le plasma lyophilisé était d'emploi très courant dans les années 70 et début 80, à un tel point qu'il était pratiquement utilisé comme soluté de remplissage chez le traumatisé routier grave. Il s'agit donc d'une redécouverte et on n'est pas surpris que ceci puisse se retrouver 30 ans après avec un produit notoirement sécurisé (2).
Il est dommage que l'article ne détaille pas plus cet emploi au niveau des role 1 qui est le lieu de début de transfusion pour 5 des blessés transfusés sur 7, ce qui n'est pas vraiment mis en avant dans ce travail. La reconstitution du Plyo est simple, mais probablement moins aisée dans une voilure tournante que dans un Casanurse ou au sol. Cet article met également en avant l'absence de transfusion de sang total, ce qui est étonnant pour une pratique rentrée dans les moeurs chez nos collègues US et UK. Enfin on retrouve l'emploi de fibrinogène, dont l'apport suffisant ne peut être assuré par le PLyo seul, et que certains proposent en première ligne de fractions coagulantes (3). Chose intéressante deux échecs de reconstitution du Plyo ont été observées.
Un article très intéressant, dont plusieurs auteurs sont en charge du développement du PLyo, avec dans la partie discussion un bon rappel des problématiques qui se posent dans de telles circonstances. Il est dommage que le regroupement des lésions du bassin avec l'atteinte des membres ait été fait car les problématiques de contrôle des hémorragies sont différentes. De même la description des lésions observées dans le groupe transfusé (qui ne sont pas tous porteurs d'un garrot), et l'analyse spécifique du groupe présentant une hémorragie encore active aurait été méritées.
---------------------------------------
Introduction
Haemorrage is the leading cause of death after combat related injuries and bleeding management is the cornerstone of management of these casualties. French armed forces are deployed in Barkhane operatio n in the Sahel-Saharan Strip who represents an immense area. Since this constraint implies evacuation times beyond doctrinal timelines, an institutional decision has been made to deploy blood products on the battlefield and transfuse casualties before role 2 admission if indicated. The purpose of this study was to evaluate the transfusion practices on battlefield during the first year following the implementation of this policy.
Materials and methods
prospective collection of data about combat related casualties categorized alpha evacuated to a role 2. Battlefield transfusion was defined as any transfusion of blood product (red blood cells, plasma, whole blood) performed by role 1 or Medevac team before admission at a role 2. Patients’ characteristics, battlefield transfusions’ characteristics and complications were analysed.
Results
During the one year study, a total of 29 alpha casualties were included during the period study. Twenty-eight could be analysed, 7/28 (25%) being transfused on battlefield, representing a total of 22 transfusion episodes. The most frequently blood product transfused was French lyophilized plasma (FLYP). Most of transfusion episodes occurred during medevac. Compared to non-battlefield transfused casualties, battlefield transfused casualties suffered more wounded anatomical regions (median number of 3 versus 2, p = 0.04), had a higher injury severity score (median ISS of 45 versus 25, p = 0,01) and were more often transfused at role 2, received more plasma units and whole blood units. There was no difference in evacuation time to role 2 between patients transfused on battlefield and non-transfused patients. There was no complication related to battlefield transfusions. Blood products transfusion onset on battlefield ranged from 75 min to 192 min after injury.
Conclusion
Battlefield transfusion for combat-related casualties is a logistical challenge. Our study showed that such a program is feasible even in an extended area as Sahel-Saharan Strip operation theatre and reduces time to first blood product transfusion for alpha casualties. FLYP is the first line blood product on the battlefield
| Tags : transfusion
18/12/2016
Fibrinogène dès que l'Hb baisse ?
Estimation of plasma fibrinogen levels based on hemoglobin, base excess and Injury Severity Score upon emergency room admission
----------------------
Il existe un grand débat sur la manière de prendre en charge la coagulopathie traumatique des traumatisés ballistiques en contexte d'isolement (1,2).Un des sujets porte sur la manière de corriger l'hypofibrinogénémie soit par apport de Plasma soit par apport de concentrés de fibrinogène (3, 4). Le consensus européen valide les deux approches (5). Mais dans notre contexte d'intervention quels critères d'administration appliquer ? L'hémoglobinémie à la prise en charge permettrait d'indiquer l'apport de fibrinogène, en gros dès qu'elle est abaissée et surtout <10g/dl. C'est ce que peut laisser penser cette étude. Des moyens simples utilisables en contexte d'isolement permettent donc de stratifier les indications de fibrinogène apporté soit sous forme concentré soit sous forme de plasma (6).
----------------------
INTRODUCTION:
Fibrinogen plays a key role in hemostasis and is the first coagulation factor to reach critical levels in massively bleeding trauma patients. Consequently, rapid estimation of plasma fibrinogen (FIB) is essential upon emergency room (ER) admission, but is not part of routine coagulation monitoring in many centers. We investigated the predictive ability of the laboratory parameters hemoglobin (Hb) and base excess (BE) upon admission, as well as the Injury Severity Score (ISS), to estimate FIB in major trauma patients.
METHODS:
In this retrospective study, major trauma patients (ISS ≥16) with documented FIB analysis upon ER admission were eligible for inclusion. FIB was correlated with Hb, BE and ISS, alone and in combination, using regression analysis.
RESULTS:
A total of 675 patients were enrolled (median ISS 27). FIB upon admission correlated strongly with Hb, BE and ISS.
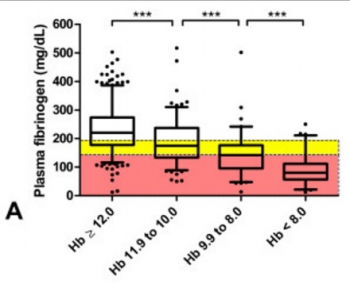
Multiple regression analysis showed that Hb and BE together predicted FIB (adjusted R2 = 0.46; loge(FIB) = 3.567 + 0.223.Hb - 0.007.Hb2 + 0.044.BE), and predictive strength increased when ISS was included (adjusted R2 = 0.51; loge(FIB) = 4.188 + 0.243.Hb - 0.008.Hb2 + 0.036.BE - 0.031.ISS + 0.0003.ISS2). Of all major trauma patients admitted with Hb <12 g/dL, 74% had low (<200 mg/dL) FIB and 54% had critical (<150 mg/dL) FIB. Of patients admitted with Hb <10 g/dL, 89% had low FIB and 73% had critical FIB. These values increased to 93% and 89%, respectively, among patients with an admission Hb <8 g/dL. Sixty-six percent of patients with only a weakly negative BE (<-2 mmol/L) showed low FIB. Of patients with BE <-6 mmol/L upon admission, 81% had low FIB and 63% had critical FIB. The corresponding values for BE <-10 mmol/L were 89% and 78%, respectively.
CONCLUSIONS:
Upon ER admission, FIB of major trauma patients shows strong correlation with rapidly obtainable, routine laboratory parameters such as Hb and BE. These two parameters might provide an insightful and rapid tool to identify major trauma patients at risk of acquired hypofibrinogenemia. Early calculation of ISS could further increase the ability to predict FIB in these patients. We propose that FIB can be estimated during the initial phase of trauma care based on bedside tests.
15/12/2016
Sang total: Pas que chaud, de banque aussi
Coagulation function of stored whole blood is preserved for 14 days in austere conditions: A ROTEM feasibility study during a Norwegian antipiracy mission and comparison to equal ratio reconstituted blood.
BACKGROUND:
Formulation of a medical preparedness plan for treating severely bleeding casualties during naval deployment is a significant challenge because of territory covered during most missions. The aim of this study was to evaluate the concept of "walking blood bank" as a supportable plan for supplying safe blood and blood products.
METHODS:
In 2013, the Royal Norwegian Navy conducted antipiracy operations from a frigate, beginning in the Gulf of Aden and ending in the Indian Ocean. Crews were on 24-hour emergency alert in preparation for an enemy assault on the frigate. Under an approved command protocol, a "walking blood bank," using crew blood donations, was established for use on board and on missions conducted in rigid-hulled inflatable boats, during which freeze-dried plasma and leukoreduced, group O low anti-A/anti-B titer, cold-stored whole blood were stored in Golden Hour Boxes. Data demonstrating the ability to collect, store, and provide whole blood were collected to establish feasibility of implementing a whole blood-focused remote damage-control resuscitation program aboard a naval vessel. In addition, ROTEM data were collected to demonstrate feasibility of performing this analysis on a large naval vessel and to also measure hemostatic efficacy of cold-stored leukoreduced whole blood (CWB) stored during a period of 14 days. ROTEM data on CWB was compared with reconstituted whole blood.
RESULTS:
Drills simulating massive transfusion activation were conducted, in which 2 U of warm fresh whole blood with platelet sparing leukoreduction were produced in 40 minutes, followed by collection of two additional units at 15-minute increments. The ROTEM machine performed well during ship-rolling, as shown by the overlapping calculated and measured mechanical piston movements measured by the ROTEM device. Error messages were recorded in 4 (1.5%) of 267 tests. CWB yielded reproducible ROTEM results demonstrating preserved fibrinogen function and platelet function for at least 3.5 weeks and 2 weeks, respectively. The frequency of ROTEM tests were as follows: EXTEM (n = 88), INTEM (n = 85), FIBTEM (n = 82), and APTEM (n = 12). CWB results were grouped. Compared with Days 0 to 2, EXTEM maximum clot firmness was significantly reduced, beginning on Days 10 to 14; however, results through that date remained within reference ranges and were comparable with the EXTEM maximum clot firmness for the reconstituted whole blood samples containing Day 5 room temperature-stored platelets.
CONCLUSION:
A "walking blood bank" can provide a balanced transfusion product to support damage-control resuscitation/remote damage-control resuscitation aboard a frigate in the absence of conventional blood bank products. ROTEM analysis is feasible to monitor damage-control resuscitation and blood product quality. ROTEM analysis was possible in challenging operational conditions.
| Tags : coagulopathie, transfusion
14/12/2016
Fibrinogène: Moins de décès
Pre-emptive administration of fibrinogen concentrate contributes to improved prognosis in patients with severe trauma
Yamamoto K, et al. Trauma Surg Acute Care Open 2016;1:1–5
---------------------------------------------------------
Bien que cela reste encore discuté, l'apport précoce de fibrinogène améliorerait la survie des traumatisés sévères. Cette publication est du moins en faveur de cette hypothèse.
---------------------------------------------------------
Background
Patients with severe trauma often present with critical coagulopathy, resulting in impaired hemostasis, massive hemorrhage, and a poor survival prognosis. The efficacy of hemostatic resuscitation in correcting coagulopathy and restoring tissue perfusion has not been studied. We assessed a novel approach of pre-emptive administration of fibrinogen concentrate to improve critical coagulopathy in patients with severe trauma.
Methods
We retrospectively compared blood transfusion volumes and survival prognosis between three groups of patients with trauma, with an Injury Severity Score (ISS) ≥26 over three consecutive periods: group A, no administration of fibrinogen concentrate; group B, administration of 3 g of fibrinogen concentrate after evaluation of trauma severity and a plasma fibrinogen level <1.5 g/L; group C, pre-emptive administration of 3 g of fibrinogen concentrate immediately on patient arrival based on prehospital information, including high-severity injury or assessed
need for massive transfusion before measurement of fibrinogen.
Results
∼56% of patients with an ISS ≥26 and transfused with red blood cell concentrates ≥10 units, had hypofibrinogenemia (fibrinogen <1.5 g/L) on arrival. Patients who received fibrinogen concentrate in group C showed significantly higher fibrinogen levels after treatment with this agent than those in group B (2.41 g/L vs 1.88 g/L; p=0.01). Although no significant difference was observed in blood transfusion volumes between the groups, the 30-day survival of patients in group C (all, and those with an ISS ≥26) was significantly better than in group A ( p<0.05). The 48-hour mortality rate in patients with an ISS ≥26 was significantly lower in group C than in group A (8.6% vs 22.9%; p=0.005). Further, among patients with an ISS ≥41, the overall mortality was significantly lower in group C than in group A (20% vs 50%; p=0.02).
Conclusion
Pre-emptive administration of fibrinogen concentrate for patients with trauma with critical coagulopathy may contribute to improved survival.
| Tags : coagulopathie
11/12/2016
PEG-20k: Le graall du prolongef field care ?
Low-volume resuscitation using polyethylene glycol-20k in a preclinical porcine model of hemorrhagic shock
Plant V. et Al. J Trauma Acute Care Surg. 2016 Dec;81(6):1056-1062.
-----------------------------------
Une nouvelle approche de la prise en compte des lésions induites par l'ischémie tissulaire qui est basée sur l'expérience de l'emploi des solutés utilisés pour conserver les organes en instance de transplantation. Grosso-modo: Remplir les espaces interstitiels par des solutés ne dépendant pas de mécanismes énergétiques. Une explication ici.
-----------------------------------
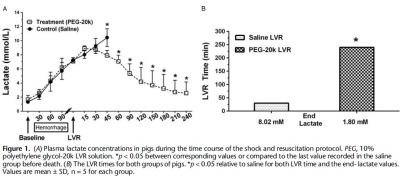
INTRODUCTION:
Polyethylene glycol-20k (PEG-20k) is highly effective for low-volume resuscitation (LVR) by increasing tolerance to the low-volume state. In our rodent shock model, PEG-20k increased survival and expanded the "golden hour" 16-fold compared to saline. The molecular mechanism is largely attributed to normalizations in cell and tissue fluid shifts after low-flow ischemia resulting in efficient microvascular exchange. The objective of this study was to evaluate PEG-20k as an LVR solution for hemorrhagic shock in a preclinical model.
METHODS:
Anesthetized male Yorkshire pigs (30-40 kg) were hemorrhaged to a mean arterial pressure (MAP) of 35 to 40 mm Hg. Once lactate reached 7 mmol/L, either saline (n = 5) or 10% PEG-20k (n = 5) was rapidly infused at 10% calculated blood volume. The primary outcome was LVR time, defined by the time from LVR administration to the time when lactate again reached 7 mmol/L. Other outcomes measured included MAP, heart rate, cardiac output, mixed venous oxygen saturation, splanchnic blood flow, and hemoglobin.
RESULTS:
Relative to saline, PEG-20k given after controlled hemorrhage increased LVR time by 16-fold, a conservative estimate given that the lactate never rose after LVR in the PEG-20k group. Survival was 80% for PEG-20k LVR compared to 0% for the saline controls (p < 0.05).
Polyethylene glycol-20k also significantly decreased heart rate after hemorrhage and increased cardiac output, MAP, splanchnic flow, and mixed venous oxygen saturation. Falling hemoglobin concentrations suggested sizable hemodilution from fluid shifts into the intravascular compartment.
CONCLUSIONS:
In a preclinical model of controlled hemorrhagic shock, PEG-20k-based LVR solution increased tolerance to the shock state 16-fold compared to saline. Polyethylene glycol-20k is a superior crystalloid for LVR that may increase safe transport times in the prehospital setting and find use in hospital emergency departments and operating rooms for patients awaiting volume replacement or normalization of cell, tissue, and compartment fluid volumes.
NaCl 7,5% ? A voir mais sans Colloïdes.
Pre-Hospital Resuscitation of Traumatic Hemorrhagic Shock with Hypertonic Solutions Worsen Hypo-Coagulation and Hyper-Fibrinolysis
Delano M. et Al. Shock. 2015 Jul;44(1):25-31
-----------------------------------------------
Le choix d'un liquide de remplissage vasculaire n'est pas simple. Au delà des contraintes d'efficacité en termes de remplissage vasculaire, de bonne tolérance notamment rénale il y a également les effets de ce dernier sur la coagulation. On sait qu'une partie importante des blessés actuellement pris en charge présentent une coagulopathie traumatique (1). Le NaCl 7.5% est le soluté recommandé par la procédure du sauvetage au combat (2) car il représente le meilleur compromis intérêt médical/logistique. Le travail ici présenté met en évidence les effets délétères des solutés hypertoniques sur la coagulation. Ce document mérite cependant d'être pondéré car il s'appuie sur une petite cohorte de patients de traumatologie civile, que le profil du remplissage vasculaire préhospitalier n'est pas clairement rapporté hormis le premier liquide, qu'il ne précise pas le niveau de calcémie plasmatique car ce dernier peut être affecté selon la nature des solutés utilisés (4), que le groupe HS a des marqueurs d'hypoperfusion tissulaire identique au groupe NS, que la comparaison se fait avec un groupe de sujets sains et non entre les groupes. Par ailleurs on sait également qu'il est mis en avant l'intérêt des solutions HS en matière de prise en charge des HTIC des plaies cranio-cérébrales (4) et la réduction de l'activation des polynucléaires neutrophiles (5). Donc il ne s'agit pas de remettre en question le choix actuel, mais de le repositionner dans le débat notamment avec l'emploi du Plama lyophylisé comme soluté de remplissage premier des blessés les plus graves (6). Une chose apparait certaine: Ne plus utiliser une association HS/Dextran type RescueFlow (7).
-----------------------------------------------
Impaired hemostasis frequently occurs after traumatic shock and resuscitation. The prehospital fluid administered can exacerbate subsequent bleeding and coagulopathy. Hypertonic solutions are recommended as first-line treatment of traumatic shock; however, their effects on coagulation are unclear. This study explores the impact of resuscitation with various hypertonic solutions on early coagulopathy after trauma. We conducted a prospective observational subgroup analysis of large clinical trial on out-of-hospital single-bolus (250 mL) hypertonic fluid resuscitation of hemorrhagic shock trauma patients (systolic blood pressure, e70 mmHg). Patients received 7.5% NaCl (HS), 7.5% NaCl/6% Dextran 70 (HSD), or 0.9% NaCl (normal saline [NS]) in the prehospital setting. Thirty-four patients were included: 9 HS, 8 HSD, 17 NS. Treatment with HS/HSD led to higher admission systolic blood pressure, sodium, chloride, and osmolarity, whereas lactate, base deficit, fluid requirement, and hemoglobin levels were similar in all groups. The HSD-resuscitated patients had higher admission international normalized ratio values and more hypocoagulable patients, 62% (vs. 55% HS, 47% NS; P G 0.05). Prothrombotic tissue factor was elevated in shock treated with NS but depressed in both HS and HSD groups. Fibrinolytic tissue plasminogen activator and antiYfibrinolytic plasminogen activator inhibitor type 1 were increased by shock but not thrombin-activatable fibrinolysis inhibitor. The HSD patients had the worst imbalance between procoagulation/anticoagulation and profibrinolysis/antifibrinolysis, resulting in more hypocoagulability and hyperfibrinolysis. We concluded that resuscitation with hypertonic solutions, particularly HSD, worsens hypocoagulability and hyperfibrinolysis after hemorrhagic shock in trauma through imbalances in both procoagulants and anticoagulants and both profibrinolytic and antifibrinolytic activities
25/08/2016
Réchauffer une perfusion: La tubulure +++
An Analysis of the Temperature Change in Warmed Intravenous Fluids during Administration in a Cold Environment at Temperatures of Less than 0
2016 Critical Care Transport Medicine Conference Scientific Forum
SIngleton W et Al. Air Medical Journal 35 (2016) 205-207
Objective: This is a non-human simulation study determining the decrease in temperature that occurred to 1L bags of Normal Saline in an austere environment. The bags were warmed to 38°C (100°F), administered through standard intravenous tubing at a set flow rate, while in an environment with ambient temperatures of less than 0°C (32°F). The goal was to determine if there was a significant decrease in fluid temperature from the IV bag through the tubing to the IV catheter administration site.
Methods/Materials: Three trials were run at four different temperatures, 0°C (32°F), -7 °C (20°F), -12°C (10°F ) and 33°C (72°F control ). Each bag of normal saline was warmed to the same temperature 38°C (100°F) utilizing the Soft Sack IV Fluid Warmer. Three of the bags were then placed in a cold austere environment (freezer) at each of the specified temperatures. The remaining bag was kept in the ambient temperature 33°C (72°F control). The fluid was administered through standard intravenous tubing (18 gauge catheter, 20 drop set, 211 cm in length) at a flow rate of 999ml/hr in temperatures less than 0°C (32°F). Fluid was collected in a glass container outside the austere environment with the temperature being recorded at 5 minute intervals.
Results: The results demonstrated a statistically significant (p> 0.05) change in temperature between the IV bag and the administration site. The most rapid change occurred within the first 5 minutes. The temperature change was more significant with the colder ambient temperatures, with an average of 50° difference at -7°C (20°F) and -12°C (10°F ). This is compared to a 27° difference at 0°C and the control temperature of 33°C (72°F control). The temperature of the fluid remaining within the IV bag also decreased an average of 15°C at the control temperature of 33°C (72°F control) and 0°C (32°F), which is statistically significant. The temperature in the bag decreased an average of 35°C at -7°C (20°F) and -12°C (10°F), which was statistically significant (p>0.05).
Conclusion: Based on these results, it appears that the most significant heat loss occurs through the IV tubing itself, the loss occurs rapidly, and is more pronounced at colder ambient air temperatures. Therefore, it may be beneficial to insulate the tubing on a trauma patient receiving warmed IV fluids in a cold environment of less than 0°C (32°F) to help prevent hypothermia.
01/05/2016
Albumine aussi bien que PFC ?
Influences of Limited Resuscitation with Plasma or Plasma Protein Solutions on Hemostasis and Survival of Rabbits with Non-Compressible Hemorrhage
J Trauma Acute Care Surg. 2016 Apr 27. Kheirabadi BS et Al.
BACKGROUND:
Plasma infusion with or without RBC is the current military standard of care for prehospital resuscitation of combat casualties. We examined possible advantages of early and limited resuscitation with fresh plasma compared with a single plasma protein or crystalloid solutions in an uncontrolled hemorrhage model in rabbits.
METHODS:
Anesthetized spontaneously breathing rabbits (3.3±0.1 kg) were instrumented and subjected to a splenic uncontrolled hemorrhage. Rabbits in shock were resuscitated at 15 min with Plasma-Lyte (PAL; 30 ml/kg), PAL+ fibrinogen (PAL+F; 30ml+100mg/kg), fresh rabbit plasma (PLS; 15ml/kg), or 25% albumin (ALB; 5 ml/kg) solution; all given in two bolus IV injections (15 min apart) to achieve a MAP of 65 mmHg, n=8-9/group. Animals were monitored for 2 hrs or until death and blood loss was measured. Blood samples and tissues were collected and analyzed.
RESULTS:
There were no differences among groups in baseline measures and their initial bleeding volume at 15 min. At 60 min post-injury, MAP was higher with albumin than with crystalloids (PAL or PAL+F), but shock indices were not different despite the large differences in resuscitation volumes.
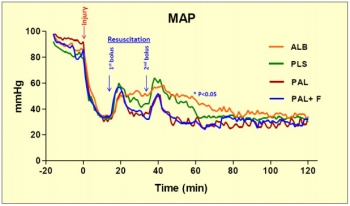
Fibrinogen addition to PAL only increased clot strength. Plasma resuscitation increased survival rate (75%) without significant improvement in coagulation measures. Albumin administration replenished total plasma protein, and increased survival rate to 100% (p<.05 vs. crystalloids). No histological adverse events were identified in the vital organs.
CONCLUSION:
Fibrinogen administration added to a compatible crystalloid did not improve hemostatic outcomes. Plasma resuscitation increased survival rate, however, its effects did not differ from those obtained with 25% albumin at 1/3 of the volume. The albumin advantage was consistent with our previous findings in which 5% albumin was used at a volume equal to plasma. The benefit of plasma for resuscitation may be mostly due to its albumin content rather than its coagulation proteins
| Tags : remplissage
09/01/2016
HES et hémorragie: Pas bon ménage ?
Effects of different types of fluid resuscitation for hemorrhagic shock on splanchnic organ microcirculation and renal reactive oxygen species formation
Wu et al. Critical Care (2015) 19:434
----------------------------------
Un travail de plus qui doit rendre raisonné sur l'emploi des colloïdes synthétiques qui si ils semblent préserver la circulation splanchnique seraient responsables de lésions oxydatives secondaires. CEla serait moins le cas avce le salé hypertonique.
----------------------------------
Introduction: Fluid resuscitation is an indispensable procedure in the acute management of hemorrhagic shock for restoring tissue perfusion, particularly microcirculation in splanchnic organs. Resuscitation fluids include crystalloids, hypertonic saline (HTS), and synthetic colloids, and their selection affects the recovery of microcirculatory blood flow and reactive oxygen species (ROS) formation, which is often evident in the kidney, following reperfusion. In this study, the effects of acute resuscitation with 0.9 % saline (NS), 3 % HTS, 4 % succinylated gelatin (GEL), and 6 % hydroxyethyl starch (HES) 130/0.4 were compared in a hemorrhagic shock rat model to analyze restoration of microcirculation among various splanchnic organs and the gracilis muscle and reperfusion-induced renal ROS formation.
Methods: A total of 96 male Wistar rats were subjected to sham operation (sham group), hemorrhagic shock (control group), and resuscitation with NS, HTS, GEL and HES. Two hours after resuscitation, changes in the mean arterial pressure (MAP), serum lactate level and the microcirculatory blood flow among various splanchnic organs, namely the liver, kidney, and intestine (mucosa, serosal muscular layer, and Peyer’s patch), and the gracilis muscle, were compared using laser speckle contrast imaging. Renal ROS formation after reperfusion was investigated using an enhanced in vivo chemiluminescence (CL) method.
Results: Microcirculatory blood flow was less severely affected by hemorrhaging in the liver and gracilis muscle. Impairment of microcirculation in the kidney was restored in all resuscitation groups. Resuscitation in the NS group failed to restore intestinal microcirculation. Resuscitation in the HTS, GEL, and HES groups restored intestinal microcirculatory blood flow. By comparison, fluid resuscitation restored hemorrhagic shock-induced hypotension and decreased lactatemia in all resuscitation groups. Reperfusion-induced in vivo renal ROS formation was significantly higher in the GEL and HES groups than in the other groups.
Conclusion: Although fluid resuscitation with NS restored the MAP and decreased lactatemia following hemorrhagic shock, intestinal microcirculation was restored only by other volume expanders, namely 3 % HTS, GEL, and HES. However, reperfusion-induced renal ROS formation was significantly higher when synthetic colloids were used.
| Tags : remplissage
19/11/2015
Stratégie Low Flow: Encore confirmée
Efficacy of limited fluid resuscitation in patients with hemorrhagic shock: a meta-analysis
Duan C. et Al. Int J Clin Exp Med. 2015; 8(7): 11645–11656.

| Tags : remplissage, choc, hémorragie