12/11/2015
Et l'albumine ?
Is limited prehospital resuscitation with plasma more beneficial than using a synthetic colloid? An experimental study in rabbits with parenchymal bleeding
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2015;78: 752-759
--------------------------------------
Il existe de grands débats sur la manière optimale d'assurer le remplissage vasculaire des blessés de guerre. Pour certains le fluide de référence est un hydroxyéthylamidon, pour d'autres un cristalloïde isotonique et en ce qui nous concerne les deux avec la mise en avant du sérum salé hypertonique premier suivi d'HEA. Actuellement il existe une tendance à promouvoir une autre stratégie faisant appel pour les blessés les plus graves au plasma voire la transfusion de sang frais. L'étude proposée avait pour objectif de confirmer l'intérêt d'une démarche "plasma premier". Une des surprises a été de constater que ce n'est pas cette dernière qui permettait d'obtenir le meilleur taux de survie mais l'emploi d'albumine, et ce de loin. Ces données expérimentales certes très partielles permettent aux auteurs (?) de rediscuter les conclusions de travaux anciens notamment de l'étude SAFE (1,2). Les solutés d'albumine utilisés par cette dernière ont une osmolarité de 260 mosm/kg (versus 305 mosm/kg pour le sérum salé). Les effets délétères notamment chez le traumatisé crânien pourraient être dus non pas à l'extravasation d'albumine dans le parenchyme cérébral lésé mais à l'hypoosmolarité de l'albumex 4%, ces deux mécanismes concourrant à la plus grande fréquence d'HTIC dans le groupe albumine (3). A méditer
--------------------------------------
BACKGROUND:
Reports of survival benefits of early transfusion of plasma with red blood cells (1:1 ratio) in trauma patients suggest that plasma may be a better fluid to replace Hextend for battlefield resuscitation. We studied possible advantages of prehospital resuscitation with plasma compared with Hextend or albumin in a model of uncontrolled hemorrhage.
METHODS:
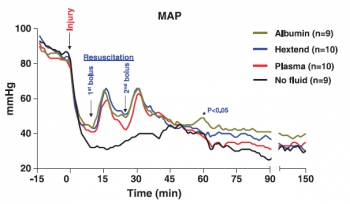
Male New Zealand white rabbits (3.3 T 0.1 kg) were anesthetized, instrumented, and subjected to a splenic injury with uncontrolled bleeding. Ten minutes after injury (mean arterial pressure [MAP] G 40 mm Hg), the rabbits received small and equal volumes (15 mL/kg) of rabbit plasma (n = 10), Hextend (n = 10), or 5% human albumin (n = 9) or no fluid. Fluids were administered in two bolus injections (20 minutes apart) and targeted to aMAP of 65 mm Hg. Animals were monitored for 2.5 hours or until death, and their blood losses were measured. Arterial blood samples were collected at different times and analyzed for ABG, CBC, and coagulation tests.
RESULTS:
There were no differences in baseline measures among groups. Splenic injury caused similar hemorrhages (9.1 T 0.4 mL/kg at 10 minutes) and decreased MAP in all subjects. Subsequent resuscitation initiated additional bleeding. At 60 minutes after injury (20 minutes after resuscitation), longer activated partial thromboplastin time and lower fibrinogen concentrations were apparent compared with baseline values with differences among groups. Thrombelastography analysis indicated faster and stronger clot formation with plasma and albumin resuscitation than with Hextend use. Shock indices were increased in all groups, but smaller changes were measured in the albumin group. Total blood loss did not differ among resuscitated rabbits but was higher (p G 0.05) than among nonresuscitated animals. Survival rates were 11% (untreated), 40% (Hextend and plasma), and 89% (albumin, p G 0.05).
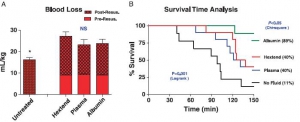
CONCLUSION:
Resuscitation with plasma or albumin better preserved coagulation function than did Hextend. However, despite these improvements, plasma resuscitation did not reduce blood loss or improve survival, while albumin administration seemed beneficial
| Tags : remplissage, coagulopathie
Lent/régulier: Mieux pour le crâne ?
Resuscitation speed affects brain injury in a large animal model of traumatic brain injury and shock
Sillesen M et Al. Scand J Trauma Resusc Emerg Med. 2014 Aug 14;22:46
----------------------------------------
En matière de remplissage vasculaire, on s'intéresse souvent à la nature des solutés et aux quantités perfusées. On s'intéresse moins aux vitesses de perfusion. Pourtant cette dernière a son importance. Le travail présenté est intéressant car il rapport qu'outre la nature du soluté importante mais aussi sa vitesse d'administration. Ainsi il semblerait que dans un modèle expérimental de traumatisme crânien l'emploi de solutés cristalloïdes de sérum salé isotonique soit responsable d'une augmentation de l'oedeme cérébal et du volume des lésions intracraniennes quel que soit le régime d'administration. Ce travail retrouve par ailleurs l'intérêt sur la maîtrise de l'oedeème cérébral de l'apport de fraction coagulantes de manière procédurée par rapport au bolus. Si l'on replace ce document dans le contexte d'isolement et de maintien en survie de nos blessés notamment cranio-cérébraux en état de choc, cela implique une formation spécifique des équipes qui devront par ailleurs pouvoir disposer d'équipements adaptés comme celui_ci (1)
----------------------------------------
BACKGROUND:
Optimal fluid resuscitation strategy following combined traumatic brain injury (TBI) and hemorrhagic shock (HS) remain controversial and the effect of resuscitation infusion speed on outcome is not well known. We have previously reported that bolus infusion of fresh frozen plasma (FFP) protects the brain compared with bolus infusion of 0.9% normal saline (NS). We now hypothesize reducing resuscitationinfusion speed through a stepwise infusion speed increment protocol using either FFP or NS would provide neuroprotection compared with a highspeed resuscitation protocol.
METHODS:
23 Yorkshire swine underwent a protocol of computer controlled TBI and 40% hemorrhage. Animals were left in shock (mean arterial pressure of 35 mmHg) for two hours prior to resuscitation with bolus FFP (n = 5, 50 ml/min) or stepwise infusion speed increment FFP (n = 6), bolus NS (n = 5, 165 ml/min) or stepwise infusion speed increment NS (n = 7). Hemodynamic variables over a 6-hour observation phase were recorded. Following euthanasia, brains were harvested and lesion size as well as brain swelling was measured.
RESULTS:
Bolus FFP resuscitation resulted in greater brain swelling (22.36 ± 1.03% vs. 15.58 ± 2.52%, p = 0.04), but similar lesion size compared with stepwise resuscitation. This was associated with a lower cardiac output (CO: 4.81 ± 1.50 l/min vs. 5.45 ± 1.14 l/min, p = 0.03). In the NS groups, bolus infusion resulted in both increased brain swelling (37.24 ± 1.63% vs. 26.74 ± 1.33%, p = 0.05) as well as lesion size (3285.44 ± 130.81 mm(3) vs. 2509.41 ± 297.44 mm3, p = 0.04). This was also associated with decreased cardiac output (NS: 4.37 ± 0.12 l/min vs. 6.35 ± 0.10 l/min, p < 0.01).
CONCLUSIONS:
In this clinically relevant model of combined TBI and HS, stepwise resuscitation protected the brain compared with bolusresuscitation.

| Tags : tbi, remplissage
03/07/2015
Fibrinogène avec le TXA ?: Plutôt oui
Association of Cryoprecipitate and Tranexamic Acid With Improved Survival Following Wartime Injury: Findings From the MATTERs II Study
Morrison JJ et Al. JAMA Surg. 2013;148(3):218-225.
Objective To quantify the impact of fibrinogen-containing cryoprecipitate in addition to the antifibrinolytic tranexamic acid on survival in combat injured.
Design Retrospective observational study comparing the mortality of 4 groups: tranexamic acid only, cryoprecipitate only, tranexamic acid and cryoprecipitate, and neither tranexamic acid nor cryoprecipitate. To balance comparisons, propensity scores were developed and added as covariates to logistic regression models predicting mortality.
Setting A Role 3 Combat Surgical Hospital in southern Afghanistan.
Patients A total of 1332 patients were identified from prospectively collected UK and US trauma registries who required 1 U or more of packed red blood cells and composed the following groups: tranexamic acid (n = 148), cryoprecipitate (n = 168), tranexamic acid/cryoprecipitate (n = 258), and no tranexamic acid/cryoprecipitate (n = 758).
Main Outcome Measure In-hospital mortality.
Results Injury Severity Scores were highest in the cryoprecipitate (mean [SD], 28.3 [15.7]) and tranexamic acid/cryoprecipitate (mean [SD], 26 [14.9]) groups compared with the tranexamic acid (mean [SD], 23.0 [19.2]) and no tranexamic acid/cryoprecipitate (mean [SD], 21.2 [18.5]) (P < .001) groups. Despite greater Injury Severity Scores and packed red blood cell requirements, mortality was lowest in the tranexamic acid/cryoprecipitate (11.6%) and tranexamic acid (18.2%) groups compared with the cryoprecipitate (21.4%) and no tranexamic acid/cryoprecipitate (23.6%) groups. Tranexamic acid and cryoprecipitate were independently associated with a similarly reduced mortality (odds ratio, 0.61; 95% CI, 0.42-0.89; P = .01 and odds ratio, 0.61; 95% CI, 0.40-0.94; P = .02, respectively). The combined tranexamic acid and cryoprecipitate effect vs neither in a synergy model had an odds ratio of 0.34 (95% CI, 0.20-0.58; P < .001), reflecting nonsignificant interaction (P = .21).
Conclusions Cryoprecipitate may independently add to the survival benefit of tranexamic acid in the seriously injured requiring transfusion. Additional study is necessary to define the role of fibrinogen in resuscitation from hemorrhagic shock.
| Tags : coagulopathie
27/03/2015
Hypersalé: Mieux avec de la lidocaïne , du magnésium et de l'adénosine ?
Correction of acute traumatic coagulopathy with small-volume 7.5% NaCl adenosine, lidocaine, and Mg2+ occurs within 5 minutes: A ROTEM analysis
Hayley L. et Al. J Trauma Acute Care Surg. 2015;78: 773-783
------------------------------------------------------------------------------------------------
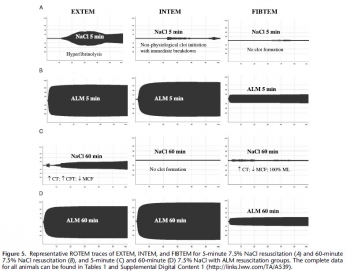
La prévention/correction de la coagulopathie traumatique est un axe essentiel de la réanimation du traumatisé grave. Le choix du soluté a son importance. L'adjonction de lidocaïne, de magnésium et d'adénosine au NaCl7,5% serait bénéfique. On observerait une fibrinolyse beaucoup moins importante qu'avec le salé hypertonique seul.
------------------------------------------------------------------------------------------------
BACKGROUND: Acute traumatic coagulopathy is a major contributor to mortality and morbidity following hemorrhagic shock. Our aim was to examine the effect of small-volume 7.5% NaCl with adenosine, lidocaine, and Mg2+ (ALM) resuscitation on the timing of correction of coagulopathy in the rat model of severe hemorrhagic shock using ROTEM.
METHODS: Male rats (300Y450 g, n = 64) were randomly assigned to (1) baseline, (2) sham, (3) bleed, (4) shock, (5) 7.5% NaCl for 5 minutes, (6) 7.5% NaCl with ALM for 5 minutes, (7) 7.5% NaCl for 60 minutes, or (8) 7.5% NaCl with ALM for 60 minutes (all n = 8). For resuscitation, 0.3-mL intravenous bolus of 7.5% NaCl was administered with and without ALM (n = 8 each group). Hemodynamics and coagulopathy were assessed.
RESULTS: After hemorrhage, prothrombin time (PT) and activated partial thromboplastin time (aPTT) increased approximately four to six times, and ROTEM indicated hypocoagulopathy. After 60-minute shock, no sustainable clots could form. 7.5% NaCl increased mean arterial pressure (MAP) to 46 T 2 mm Hg at 5 minutes and generated a weak clot in EXTEM with hyperfibrinolysis in all tests. At 60 minutes, 7.5% NaCl failed to sustain MAP (43 T 5 mm Hg) and generate a viable clot. In direct contrast, 7.5% NaCl with ALM at 5 minutes resuscitatedMAP to 64 T 3 mm Hg, corrected PT and aPTT, and generated fully formed EXTEM and FIBTEM clots. At 60 minutes, MAP was 69 T 5 mm Hg, PT and aPTT were fully corrected, and > angle, clot amplitudes (A10, A30), as well as clot firmness and elasticity were not significantly different from baseline. ALM clot lysis at 60 minutes was significantly less than bleed, shock, or 7.5% NaCl, indicating protection against hyperfibrinolysis.
CONCLUSION: Small-volume 7.5% NaCl failed to resuscitate and correct coagulopathy. In contrast, 7.5% NaCl with ALM resuscitated MAP and corrected coagulopathy at 5 minutes, with further improvements at 60 minutes in clot kinetics, propagation, and firmness. ALM fully reversed hyperfibrinolysis to baseline. The possible mechanisms are discussed. (J Trauma Acute Care Surg. 2015;78:
| Tags : remplissage, coagulopathie
Salé, HEA, Plasma ou albumine ?
Is limited prehospital resuscitation with plasma more beneficial than using a synthetic colloid? An experimental study in rabbits with parenchymal bleeding
Kheirabadi BS et Al. J Trauma Acute Care Surg. 2015;78: 752-759
----------------------------------------------------------
La recherche de la meilleure stratégie de remplissage vasculaire pour la prise en charge d'un traumatisé sévère relève de la quête du saint-Graal. L'article proposé rapporte un travail expérimental qui semble trouver in intérêt réel à l'emploi d'albumine 4%.
----------------------------------------------------------
CONCLUSION:
Resuscitation with plasma or albumin better preserved coagulation function than did Hextend. However, despite these improvements, plasma resuscitation did not reduce blood loss or improve survival, while albumin administration seemed beneficial
| Tags : remplissage
31/01/2015
Cristalloïde/Colloïde ration; Plutôt 1,5 que 4
Crystalloids Versus Colloids: Exploring Differences in Fluid Requirements by Systematic Review and Meta-Regression
Orbegozo Cortés D. et Al. Anesth Analg 2015;120:389–402
-------------------------------------------------------------------
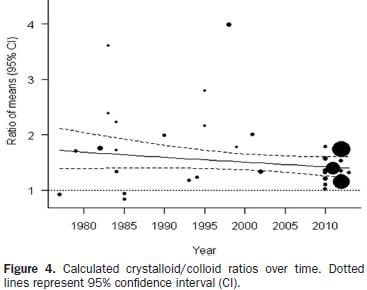
Le débat qui porte sur l'efficacité comparée des solutés de remplissage n'est pas nouveau. Cette méta-analyse porte sur l'analyse de 27 publications sélectionnées parmi 978. Elle met en évidence la très grande hétérogénéité des données publiées. Les raisons avancées portent sur la nature des populations étudiées (fuite capillaire très variable), l'administration préhospitalière de fluides à des volumes mal connu ce qui va compliquer l'analyse ultérieure, les différences de pharmacodynamie et cintétique des différents solutés employés, le fait que pour un même soluté l'efficacité en terme de remplissage puisse varier en fonction du moment de son administration, Qui qu'il en soit il semble que le ratio actuel soit plus proche de 1,5 que de 4.
On rappelle que la procédure du sauvetage au combat met en avant l'emploi de soluté salé hypertonique en première intention (250 ml en 10 minutes) suivi de 500ml de colloïdes (à défaut 250 ml de salé hypertonique) en cas de non restauration du pouls radial. Ce choix est résulte d'un compromis dans lequel le poids des solutés est pris en compte.
-------------------------------------------------------------------
BACKGROUND:
Positive fluid balance has been associated with worse outcomes, and knowledge of differences in the amounts of different types of fluid needed to achieve the same end points may have important clinical implications. Large molecules persist longer in the blood vessels than smaller molecules, such that less IV colloid may be needed to achieve similar hemodynamic end points compared with crystalloid. Recent clinical data have, however, challenged this physiological concept, with investigators reporting lower-than-expected crystalloid/colloid ratios in various populations.
METHODS:
We performed a systematic search in MEDLINE, EMBASE, and CENTRAL up to December 18, 2013, to retrieve all studies comparing (any) crystalloid with (any) colloid in all types of patients. The crystalloid/colloid ratio was calculated for each study. Descriptive analysis was performed for all studies, and a meta-analysis was performed in those studies reporting full data (in terms of means and standard deviations) of infused fluid volumes. Studies were grouped according to study and population characteristics. A meta-regression analysis was then performed to evaluate some of the possible reasons for differences in crystalloid/colloid ratios across studies.
RESULTS:
From 976 studies, 48 were retained for the final analysis; 24 of the studies had sufficient data for meta-analysis. The crystalloid/colloid ratio across all the studies included in the meta-analysis was 1.5 (95% confidence interval, 1.36–1.65) with marked heterogeneity among studies (I2 = 94%). From the meta-regression analysis, decade of publication across all publications (P = 0.001) and concentration (tonicity) in the subgroup of albumin studies (P = 0.001) were associated with the administered crystalloid/colloid ratio. The reduction in heterogeneity among studies for all publications in the meta-regression was minimal, with the maximal decrease obtained when decade of publication was considered (R2 = 12%).
CONCLUSIONS:
Greater fluid volumes are required to meet the same targets with crystalloids than with colloids, with an estimated ratio of 1.5 (1.36–1.65), but there is marked heterogeneity among studies. The crystalloid/colloid ratio seems to have decreased over the years, and differences in ratios are correlated with the concentration of albumin solutions; however, the main reasons behind the high heterogeneity among studies remain unclear.
| Tags : remplissage, perfusion
31/10/2014
HES: Du côté des belges
Hydroxyethyl Starches in the Perioperative Period. A review on the efficacy and safety of starch solutions
Ghuselings I et All. Acta Anaesth. Belg., 2014, 65, 9-22

14/09/2014
HEA: Peut être un peu de sérénité ?
Hydroxyethyl Starches: A Tale of Two Contexts: The Problem of Knowledge
Weiskopf R. Anesth Analg. 2014 Sep;119(3):509-13.
Un débat moins passionné est en train de se mettre en place au sujet de la toxicité des HES. Le texte proposé en est un exemple. Il propose une relecture pertinente des études 6S, CHEST et surtout CRISTAL qui d'une certaine façon remet en question les deux précédentes. Il nous demande de prendre en compte plusieurs éléments : La diversité des HES, les différences qui peuvent exister entre une administration répétée en réanimation et une administration ponctuelle péri-opératoire. Il s'appuie sur deux écrits publiés dans le même numéro.
Raghunathan K et all. (Intravenous Starches: Is Suspension the Best Solution?) suggèrent que les solutions colloïdes sont à réserver pour les hypovolémies aiguës alors que Irwin et all. (Volume Therapy with Hydroxyethyl Starches: Are We Throwing the Anesthesia Baby Out with the Intensive Care Unit Bathwater?) estiment que le recours aux HES 130/0.4 est pleinement justifié en environnement périopératoire.
Cette démarche correspond au positionnement de la SFAR. Rappelons que la position actuelle des instances européennes est la suivante:
" Les solutions à base d’HEA peuvent être utilisées pour la réanimation des patients avec une hypovolémie causée par une perte aiguë de sang, quand les alternatives comme la perfusion de cristalloïdes seuls sont insuffisantes. Afin de limiter les risques potentiels, les solutions contenant des HEA ne devront pas être utilisées plus de 24 heures et la fonction rénale devra être monitorée après administration des HEA "
| Tags : remplissage
04/09/2014
Remplissage vasculaire: Evolution majeure du TCCC
L'emploi préhospitalier de la transfusion de globules rouges et de plasma était évoqué de manière anecdotique. Une évolution importante survient dans la procédure américaine du TCCC (1, 2). Cette pratique est en passe de devenir une recommandation protocolée de théâtre pour les blessés en état de choc (Pas de pouls radial et conscience altérée el l'absence de traumatisme crânien) hémorragique avec notons le recours au Plyo du CTSA.
" Tactical Field Care and TACEVAC Care
7. Fluid resuscitation
a. The resuscitation fluids of choice for casualties in hemorrhagic shock, listed from most to least preferred, are: whole blood*; plasma, RBCs and platelets in 1:1:1 ratio*; plasma and RBCs in 1:1 ratio; plasma or RBCs alone; Hextend; and crystalloid (Lactated Ringers or Plasma-Lyte A).
b. Assess for hemorrhagic shock (altered mental status in the absence of brain injury and/or weak or absent radial pulse).
1. If not in shock:
- No IV fluids are immediately necessary.
- Fluids by mouth are permissible if the casualty is conscious and can swallow.
2. If in shock and blood products are available under an approved command or theater blood product administration protocol:
- Resuscitate with whole blood*, or, if not available
- Plasma, RBCs and platelets in a 1:1:1 ratio*, or, if not available
- Plasma and RBCs in 1:1 ratio, or, if not available;
- Reconstituted dried plasma, liquid plasma or thawed plasma alone or RBCs alone;
- Reassess the casualty after each unit. Continue resuscitation until a palpable radial pulse, improved mental status or systolic BP of 80-90 mmHg is present.
3. If in shock and blood products are not available under an approved command or theater blood product administration protocol due to tactical or logistical constraints:
- Resuscitate with Hextend, or if not available;
- Lactated Ringers or Plasma-Lyte A;
- Reassess the casualty after each 500 mL IV bolus;
- Continue resuscitation until a palpable radial pulse, improved mental status, or systolic BP of 80-90 mmHg is present.
- Discontinue fluid administration when one or more of the
above end points has been achieved.
4. If a casualty with an altered mental status due to suspected TBI has a weak or absent peripheral pulse, resuscitate as necessary to restore and maintain a normal radial pulse. If BP monitoring is available, maintain a target systolic BP of at least 90 mmHg.
5. Reassess the casualty frequently to check for recurrence of shock. If shock recurs, recheck all external hemorrhage control measures to ensure that they are still effective and repeat the fluid resuscitation as outlined above.
* Neither whole blood nor apheresis platelets as these products are currently collected in theater are FDA-compliant. Consequently, whole blood and 1:1:1 resuscitation using apheresis platelets should be used only if all of the FDA-compliant blood products needed to support 1:1:1 resuscitation are not avalaible
| Tags : choc, coagulopathie, remplissage
07/08/2013
Plasma: En préhospitalier AUSSI +++
Point-of-injury use of reconstituted freeze dried plasma as a resuscitative fluid: A special report for prehospital trauma care
Glassberg E. et All. J J Trauma Acute Care Surg. 2013;75(Suppl 2):S111YS111.
La prise en charge d'hémorrragie catastrophique en phase préhospitalière est particulièrement complexe. Ces dernières années la mise en place d'un réseau structuré de prise en charge, 'application de procédures spécifiques visant à arrêter les hémorragies au plus tôt, le recours à l'acide tranexaminique, la prévention des hypothermies et l'application d'une politique raisonnée de rénaimation/chirurgie ont constitué une grande avancée. Certaines nations ont équipé leurs vecteurs d'évacuations de concentrés érythrocytaires. Le maintien d'une coagulation optimale est un enjeu majeur. Pour cela existe, entre autres, le plasma lyophilisé. Les forces armées israéliennes militent pour l'emploi de ce type de solutions en phase préhospitalière
| Tags : coagulopathie, hémorragie
16/07/2013
Colloids versus crystalloids for fluid resuscitation in critically ill patients
There is no evidence from randomised controlled trials that resuscitation using colloids compared with crystalloids reduces the risk of death in patients with trauma, burns or following surgery. The use of hydroxyethyl starch might even increase mortality. Since colloid use is not associated with improved survival and colloids are considerably more expensive than crystalloids, it is hard to see how their continued use in clinical practice can be justified.
| Tags : remplissage
Point sur les problématiques actuelles du remplissage
| Tags : remplissage
Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients
We recommend not to use HES with molecular weight C200 kDa and/or degree of substitution[0.4 in patients with severe sepsis or risk of acute kidney injury and suggest not to use 6% HES130/0.4 or gelatin in these populations. We recommend not to use colloids in patients with head injury and not to administer gelatins and HES in organ donors. We suggest not to use hyperoncotic solutions for fluid resuscitation. We conclude and recommend that any new colloid should be introduced into clinical practice only after its patient-important safety parameters are established.
| Tags : hémorragie, traumatologie
Management of bleeding and coagulopathy following major trauma: an updated European guideline
| Tags : hémorragie, traumatologie
22/06/2013
Low flow mais pas zero flow resuscitation
Hampton D. et all. J Trauma Acute Care Surg. 2013;74: S9-S15
---------------------------------------------------------------------------------------
BACKGROUND:
Delivery of intravenous crystalloid fluids (IVF) remains a tradition-based priority during prehospital resuscitation of trauma patients. Hypotensive and targeted resuscitation algorithms have been shown to improve patient outcomes. We hypothesized that receiving any prehospital IVF is associated with increased survival in trauma patients compared with receiving no prehospital IVF.
METHODS:
Prospective data from 10 Level 1 trauma centers were collected. Patient demographics, prehospital IVF volume, prehospita and emergency department vital signs, lifesaving interventions, laboratory values, outcomes, and complications were collected and analyzed. Patients who did or did not receive prehospital IVF were compared. Tests for nonparametric data wer used to assess significant differences between groups (p e 0.05). Cox regression analyses were performed to determine the independent influence of IVF on outcome and complications.
RESULTS:
The study population consisted of 1,245 trauma patients; 45 were excluded owing to incomplete data; 84% (n = 1,009) received prehospital IVF, and 16% (n = 191) did not. There was no difference between the groups with respect to sex, age, and Injury Severity Score (ISS). The on-scene systolic blood pressure was lower in the IVF group (110 mm Hg vs. 100 mm Hg, p G 0.04) and did not change significantly after IVF, measured at emergency department admission (110 mm Hg vs. 105 mm Hg, p = 0.05). Hematocrit/hemoglobin, fibrinogen, and platelets were lower (p G 0.05), and prothrombin time/ international normalized ratio and partial thromboplastin time were higher (p G 0.001) in the IVF group. The IVF group received a median fluid volume of 700 mL (interquartile range, 300Y1,300). The Cox regression revealed that prehospital fluid administration was associated with increased survival (hazard ratio, 0.84; 95% confidence interval, 0.72Y0.98; p = 0.03). Site differences in ISS and fluid volumes were demonstrated (p G 0.001).
CONCLUSION:
Prehospital IVF volumes commonly used by PRospective Observational Multicenter Massive Transfusion Study (PROMMTT) investigators do not result in increased systolic blood pressure but are associated with decreased in-hospital mortality in trauma patients compared with patients who did not receive prehospital IVF
---------------------------------------------------------------------------------------
C'est du moins ce que conclue ce travail qui porte sur l'administration préhospitalière de cristalloïdes dans le cadre de conditionnements qui apparaissent assez proche de notre pratique. Ces résultats interpellent cependant car prenant apparemment le contrepied d'une autre publication récente lisible ici.
Comme dans tout restons mesurés comme proposé par ce consensus US
1. Patients porteur de plaies supérficielles: Pas d'abord veineux immédiat
2. Patient cohérent avec pouls radial: Verrou salé
3. Patient incohérent ou pas e pouls radial: Abord veineux et apport d'un volume de 500 ml
[ATTENTION AUX HEA AU SUJET DESQUELS LA CONTROVERSE S'ACCENTUE]
4. Répéter l'administration si pas d'effet
5. Si trauma cranien obtenir une PAS > 90 mmHg
L'objectif n'est pas de restaurer une pression artérielle normale mais de maintenir une pression de perfusion compatible avec la survie jusqu'à la prise en charge par une équipe chirurgicale.
| Tags : remplissage, perfusion
19/06/2013
HEA : Encore une publication contre
Association of Hydroxyethyl Starch Administration With Mortality and Acute Kidney Injury in Critically Ill Patients Requiring Volume ResuscitationA Systematic Review and Meta-analysis
In critically ill patients requiring acute volume resuscitation, use of hydroxyethyl starch compared with other resuscitation solutions was not associated with a decrease in mortality. Moreover, after exclusion of 7 trials performed by an investigator whose research has been retracted because of scientific misconduct, hydroxyethyl starch was associated with a significant increased risk of mortality and acute kidney injury. Clinical use of hydroxyethyl starch for acute volume resuscitation is not warranted due to serious safety concerns.
| Tags : remplissage
21/02/2013
Pour la coagulation: HEA de haut PM pas bon ?
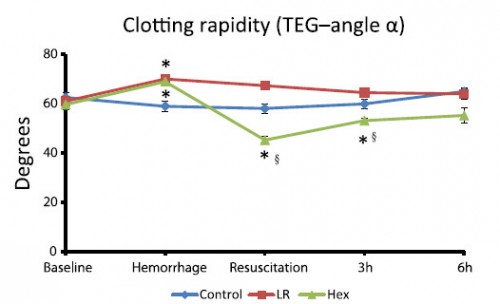
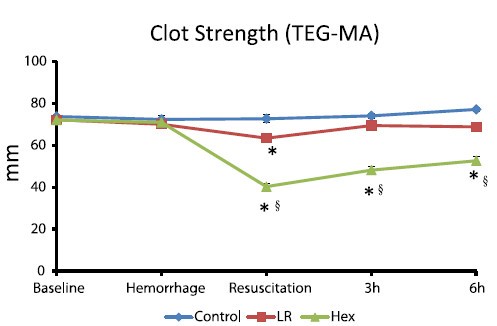
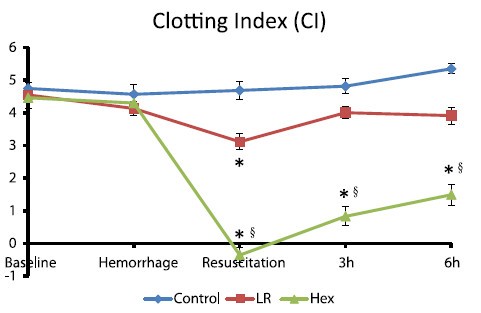
Comparisons of lactated Ringer’s and Hextend resuscitation on hemodynamics and coagulation following femur injury and severe hemorrhage in pigs
Wenjun Z et all J Trauma Acute Care Surg. 2013;74: 732-740
After traumatic hemorrhage, coagulation function was restored within 6 hours with LR resuscitation but not with Hextend. The lack of recovery after Hextend is likely caused by greater hemodilution and possible effects of starches on coagulation substrates and further documents the need to restrict the use of high-molecular-weight starch in resuscitation fluids for bleeding casualties.
On rappelle que l'Hextend est un HEA 670/0.75 et que le voluven est un HEA 130/0,4 dont les effets sur la coagulation sont réputées étant moindres.
| Tags : coagulopathie, remplissage, hémorragie
02/12/2012
Expansion volémique par F Shortgen IAR IDF
| Tags : remplissage, choc
08/09/2012
Moins remplir: Mieux ? Oui, MAIS
Restrictive fluid resuscitation in combination with damage control resuscitation: Time for adaptation.
Marquinn D et all. J Trauma Acute Care Surg. 2012;73: 674-678.
-------------------------------------------------------------------------------------------------------------
Ce travail confirme l'intérêt d'une stratégie de remplissage vasculaire parcimonieuse dès lors qu'une réanimation et une chirurgie spécialisée moderne sont accessibles. Le collectif des patients est ici celui de traumatisés thoraciques sévères arrivant dans une structure spécialisée dans des délais très courts. De telles conditions ne sont pas forcément celles de la prise en charge de blessés de guerre pour qui les délais d'évacuation sont souvent plus élevés. Il n'en demeure pas moins que cette publication milite pour une politique de remplissage vasculaire raisonnée. On rappelle que la procédure du sauvetage au combat donne pour objectif la perception d'un pouls radial perceptible.
-------------------------------------------------------------------------------------------------------------
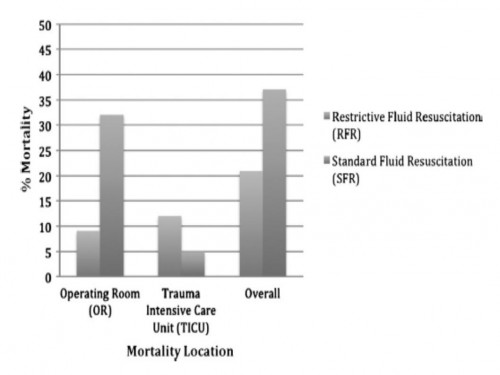
BACKGROUND:
Damage control resuscitation (DCR) conveys a survival advantage in patients with severe hemorrhage. The role of restrictive fluid resuscitation (RFR) when used in combination with DCR has not been elucidated. We hypothesize that RFR, when used with DCR, conveys an overall survival benefit for patients with severe hemorrhage.
METHODS:
This is a retrospective analysis from January 2007 to May 2011 at a Level I trauma center. Inclusion criteria included penetrating torso injuries, systolic blood pressure less than or equal to 90 mm Hg, and managed with DCR and damage control surgery (DCS). There were two groups according to the quantity of fluid before DCS: (1) standard fluid resuscitation (SFR)greater than or equal to 150 mL of crystalloid; (2) RFR less than 150 mL of crystalloid. Demographics and outcomes were analyzed.
RESULTS:
Three hundred seven patients were included. Before DCS, 132 (43%) received less than 150 mL of crystalloids, grouped under RFR; and 175 (57%) received greater than or equal to 150 mL of crystalloids, grouped under SFR. Demographics and initial clinical characteristicswere similar between the study groups. Compared with the SFR group, RFR patients received less fluid preoperatively (129 mL vs. 2,757 mL; p G 0.001), exhibited a lower intraoperative mortality (9% vs. 32%; p G 0.001), and had a shorter hospital length of stay (13 vs. 18 days; p = 0.02). Patients in the SFR group had a lower trauma intensive care unit mortality (5 vs. 12%; p = 0.03) but exhibited a higher overall mortality. Patients receiving RFR demonstrated a survival benefit, with an odds ratio for mortality of 0.69 (95% confidence interval, 0.37Y0.91).
CONCLUSION:
To the best of our knowledge, this is the first civilian study that analyzes the impact of RFR in patients managed with DCR. Its use in conjunction with DCR for hypotensive trauma patients with penetrating injuries to the torso conveys an overall and early intraoperative survival benefit.
| Tags : remplissage, choc, hémorragie, perfusion
17/04/2012
HEA pas bon en cas de sepsis sévère: Si l'on en croit le "6S trial"
Le choc hémorragique n'est pas le choc septique, mais on peut s'interroger
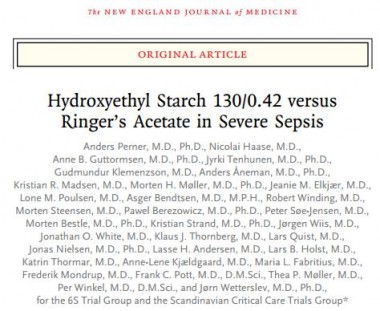
Background
Hydroxyethyl starch (HES) is widely used for fluid resuscitation in intensive care units (ICUs), but its safety and efficacy have not been established in patients with severe sepsis.
Methods
In this multicenter, parallel-group, blinded trial, we randomly assigned patients with severe sepsis to fluid resuscitation in the ICU with either 6% HES 130/0.42 (Tetraspan) or Ringer’s acetate at a dose of up to 33 ml per kilogram of ideal body weight per day. The primary outcome measure was either death or end-stage kidney failure (dependence on dialysis) at 90 days after randomization.
Results
Of the 804 patients who underwent randomization, 798 were included in the modified intention-to-treat population. The two intervention groups had similar baseline characteristics. At 90 days after randomization, 201 of 398 patients (51%) assigned to HES 130/0.42 had died, as compared with 172 of 400 patients (43%) assigned to Ringer’s acetate (relative risk, 1.17; 95% confidence interval [CI], 1.01 to 1.36; P=0.03); 1 patient in each group had end-stage kidney failure. In the 90-day period, 87 patients (22%) assigned to HES 130/0.42 were treated with renal-replacement therapy versus 65 patients (16%) assigned to Ringer’s acetate (relative risk, 1.35; 95% CI, 1.01 to 1.80; P=0.04), and 38 patients (10%) and 25 patients (6%), respectively, had severe bleeding (relative risk, 1.52; 95% CI, 0.94 to 2.48; P=0.09). The results were supported by multivariate analyses, with adjustment for known risk factors for death or acute kidney injury at baseline.
Conclusions
Patients with severe sepsis assigned to fluid resuscitation with HES 130/0.42 had an increased risk of death at day 90 and were more likely to require renal-replacement therapy, as compared with those receiving Ringer’s acetate.
(Funded by the Danish Research Council and others; 6S ClinicalTrials.gov number, NCT00962156.)