29/12/2014
Vidéolaryngoscopie: Un tournant ?
Techniques, Success, and Adverse Events of Emergency Department Adult Intubations
Brown CA et Al. Ann Emerg Med. 2014;-:1-9.
--------------------------------------------------------------------
Une certitude, l'emploi de vidéolaryngoscope simplifie l'abord trachéal pour les praticiens les moins expérimentés. Reste à démocratiser au plan économique ces dispositifs.
--------------------------------------------------------------------
Study objective: We describe the operators, techniques, success, and adverse event rates of adult emergency department (ED) intubation through multicenter prospective surveillance.
Methods: Eighteen EDs in the United States, Canada, and Australia recorded intubation data onto a Web-based data collection tool, with a greater than or equal to 90% reporting compliance requirement. We report proportions with binomial 95% confidence intervals (CIs) and regression, with year as the dependent variable, to model change over time.
Results: Of 18 participating centers, 5 were excluded for failing to meet compliance standards. From the remaining 13 centers, we report data on 17,583 emergency intubations of patients aged 15 years or older from 2002 to 2012. Indications were medical in 65% of patients and trauma in 31%. Rapid sequence intubation was the first method attempted in 85% of encounters.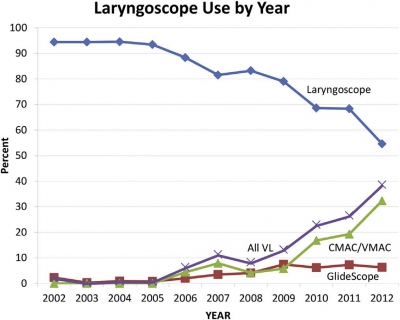 Emergency physicians managed 95% of intubations and most (79%) were physician trainees. Direct laryngoscopy was used in 84% of first attempts. Video laryngoscopy use increased from less than 1% in the first 3 years to 27% in the last 3 years (risk difference 27%; 95% CI 25% to 28%; mean odds ratio increase per year [ie, slope] 1.7; 95% CI 1.6 to 1.8). Etomidate was used in 91% and succinylcholine in 75% of rapid sequence intubations. Among rapid sequence intubations, rocuronium use increased from 8.2% in the first 3 years to 42% in the last 3 years (mean odds ratio increase per year 1.3; 95% CI 1.3 to 1.3). The first-attempt intubation success rate was 83% (95% CI 83% to 84%) and was higher in the last 3 years than in the first 3 (86% versus 80%; risk difference 6.2%; 95% CI 4.2% to 7.8%). The airway was successfully secured in 99.4% of encounters (95% CI 99.3% to 99.6%).
Emergency physicians managed 95% of intubations and most (79%) were physician trainees. Direct laryngoscopy was used in 84% of first attempts. Video laryngoscopy use increased from less than 1% in the first 3 years to 27% in the last 3 years (risk difference 27%; 95% CI 25% to 28%; mean odds ratio increase per year [ie, slope] 1.7; 95% CI 1.6 to 1.8). Etomidate was used in 91% and succinylcholine in 75% of rapid sequence intubations. Among rapid sequence intubations, rocuronium use increased from 8.2% in the first 3 years to 42% in the last 3 years (mean odds ratio increase per year 1.3; 95% CI 1.3 to 1.3). The first-attempt intubation success rate was 83% (95% CI 83% to 84%) and was higher in the last 3 years than in the first 3 (86% versus 80%; risk difference 6.2%; 95% CI 4.2% to 7.8%). The airway was successfully secured in 99.4% of encounters (95% CI 99.3% to 99.6%).
Conclusion: In the EDs we studied, emergency intubation has a high and increasing success rate. Both drug and device selection evolved significantly during the study period.
| Tags : airway, intubation
28/12/2014
Un trocard de coelio ?
Standard laparoscopic trocars for the treatment of tension pneumothorax: A superior alternative to needle decompression
Quinton H. et Al. J Trauma Acute Care Surg. 2014;77: 170-175.
-------------------------------------------------------
Le recours à un cathéter d'au moins 8 cm est prôné par certains du fait de l'épaisseur de la paroi thoracique. L'inconvénient de cette longueur est le risque non négligeable de ponction parenchymateuse surtout lors de l'emploi de la voie antérieure.
La voie latérale exposerait maoins à ce risque. Une alternative bien moins dangereuse et toute aussi efficace est la thoracostomie au doigt. Et pourquoi pas un trocard de coelio ?
-------------------------------------------------------
BACKGROUND: Needle thoracostomy (NT) is a commonly taught intervention for tension pneumothorax (tPTX) but has a high failure rate. We hypothesize that standard 5-mm laparoscopic trocars may be a safe and more effective alternative.
METHODS: Thirty episodes of tPTX and 27 episodes of tension-induced pulseless electrical activity (PEA) were induced in five adult swine using thoracic CO2 insufflation via balloon trocar. Tension was defined as a 50% decrease in cardiac output. Chest decompression was performed with 5-mm laparoscopic trocars for the treatment of both tPTX with hemodynamic compromise and tension-induced PEA. The lungs and heart were inspected and graded at necropsy for trocar-related injury. Results were also compared with success rates with NT in the same model.
RESULTS: The placement of a 5-mm trocar rapidly and immediately relieved tension physiology in 100% of the cases. Mean arterial pressure, cardiac output, central venous pressure, and pulmonary capillary wedge pressure all returned to baseline within 1 minute of trocar placement. Adequate perfusion was restored in 100% of tension-induced PEA cases within 30 seconds of trocar placement. There was no evidence of trocar-related heart or lung damage in any of the experimental animals at necropsy (mean injury scores, 0 for both). Fivemillimeter trocars significantly outperformed standard NT for both tPTX and tension-induced PEA arrest.
CONCLUSION: tPTX and tension-induced PEA can be safely and effectively treated with chest decompression using 5-mm laparoscopic trocars. This technique may serve as a more rapid and reliable alternative to needle decompression.
| Tags : pneumothorax
22/12/2014
Plus d'auscultation mais une Echo ?
Point of care ultrasound for orotracheal tube placement assessment in out-of hospital setting.
Zadel S et AL. Resuscitation. 2014 Nov 20;87C:1-6
-----------------------------------------------
A lire cet article, on comprend pourquoi l'engouement actuel pour l'échographie des voies aériennes. A coup sûr une technique à maîtriser en préhospitalier.
-----------------------------------------------
AIM OF THE STUDY:
The percentage of unrecognised orotracheal tube displacement in an out-of-hospital setting has been reported to be between 4.8% and 25%. The aim of our study was to assess the sensitivity and specificity of Point-of-Care-UltraSound (POCUS) for confirming the propertube position after an urgent orotracheal intubation in an out-of-hospital setting and the time needed for POCUS.
METHODS:
Our single-centred prospective study included all patients who needed out-of-hospital orotracheal intubation. After the intubation, bilateral chest auscultation and assessment of bilateral lung sliding and diaphragm excursion within POCUS were done. Spectrographic quantitative capnography was used as the reference standard to confirm a proper tube position.
RESULTS:
We enrolled 124 patients. For auscultation, sensitivity and negative predicted value were 100%, specificity was 90% and positive predicted value 30% (95% confidence interval).
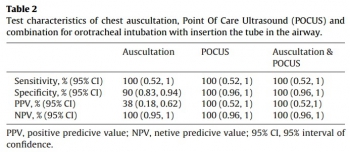
Sensitivity, specificity, positive predicted value, and negative predicted value for POCUS alone and for a combination of auscultation and POCUS were 100% (95% confidence interval). In three patients, we detected endobronchial tube displacement with auscultation and POCUS. Capnography failed to detect displacement in all three cases. The median time needed for POCUS was 30s.
CONCLUSION:
Results of our study support POCUS as an accurate and reliable method for confirming the proper orotracheal tube placement in trachea and it is feasible for out-of-hospital setting implementation. POCUS also seems to be time saving method but to make definitive conclusion more studies should be done.
| Tags : airway, intubation, échographie
20/12/2014
Simulation: Oui bien sûr, mais ?
The Role of Simulation in Continuing Medical Education for Acute Care Physicians: A Systematic Review
Khanduja PK et Al. Crit Care Med. 2015 Jan;43(1):186-93.
-------------------------------------------------------------------
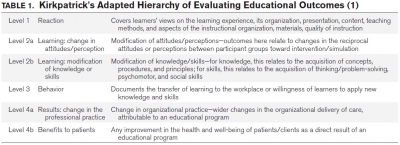
Une revue de littérature qui pointe le caractère positif RESSENTI par les participants à un programme de formation continue par simulation. Cette revue de littérature peine à confirmer que ce ressenti se traduit par une réelle amélioration de la prise en charge de nos patients. Les auteurs ne retrouvent en effet qu'une seule étude atteignant les stades 4a et b de Kirkpatrick, c'est à dire des niveaux où sont observés des changements de pratique et un bénéfice objectif pour les patients. Une des difficultés tient au fait que nombre de travaux portent sur l'anesthésie et tout particulièrement en milieu universitaire. Ils concluent néanmoins à l'intérêt de cette méthode d'enseignement.
-------------------------------------------------------------------
OBJECTIVES:
We systematically reviewed the effectiveness of simulation-based education, targeting independently practicing qualified physicians inacute care specialties. We also describe how simulation is used for performance assessment in this population.
DATA SOURCES:
Data source included: DataMEDLINE, Embase, Cochrane Database of Systematic Reviews, Cochrane CENTRAL Database of Controlled Trials, and National Health Service Economic Evaluation Database. The last date of search was January 31, 2013.
STUDY SELECTION:
All original research describing simulation-based education for independently practicing physicians in anesthesiology, criticalcare, and emergency medicine was reviewed.
DATA EXTRACTION:
Data analysis was performed in duplicate with further review by a third author in cases of disagreement until consensus was reached. Data extraction was focused on effectiveness according to Kirkpatrick's model. For simulation-based performance assessment, tool characteristics and sources of validity evidence were also collated.
DATA SYNTHESIS:
Of 39 studies identified, 30 studies focused on the effectiveness of simulation-based education and nine studies evaluated the validity of simulation-based assessment. Thirteen studies (30%) targeted the lower levels of Kirkpatrick's hierarchy with reliance on self-reporting.
CONCLUSIONS:
Simulation is perceived as a positive learning experience with limited evidence to support improved learning. Future research should focus on the optimal modality and frequency of exposure, quality of assessment tools and on the impact of simulation-based education beyond the individuals toward improved patient care.
La NAC: Intéressante en role 1: Probable ?
La N-acétylcystéine ou acétylcystéine ou NAC est un acide aminé non essentiel, qui stimule la production de glutathion, un antioxydant. Elle est surtout connue comme agent mucolytique. En médecine d'urgence son emploi lors d'intoxication au paracétamol est parfaitement validé. Moins connues sont les emplois de cet agent antioxydant dans deux types d'indication qui nous intéressent.
La première est le traumatisme sonore aigu notamment après explosion (1) ou tir (2) où il semblerait que la démarche classique [repos auditif, corticothérapie+/- vasodilatateurs] (3, 4) évoluerait vers une statégie associant le repos, la corticothérapie et unhe stratégie antioxydante précoce incluant le recours précoce à la N Acétyl Cystéine(5, 6).
La seconde porte sur la réduction des séquelles neurologiques après blast cérébral (7). Cet intérêt pour les effets anti-oxydants ne sont pas nouveaux et les effets «protecteurs» sont mis en avant également au niveau pulmonaire (8), rénale (9) et hépatique (10).
Si tout ceci reste à valider (11, 12), il semble que l'intégration de cette molécule ancienne soit d'un intérêt réel pour la prise en charge du combattant blasté ou exposéà un TSA à condition que l'administration soit précoce (<1h) (13) et donc que la N Acétyl Cystéine soit disponible en rôle 1
15/12/2014
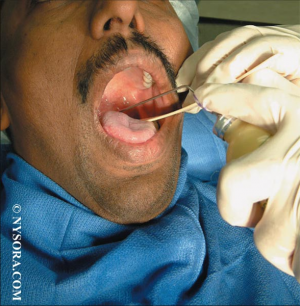
Anesthésie locale/régionale pour intubation
Regional and Topical Anesthesia for Endotracheal Intubation
En cas d'intubation difficile, il est important de préserver la ventilation spontanée. Il existe pour cela plusieurs techniques qui vous sont présentées en quelques images. Ces techniques permettent de faciliter l'intubation en évitant 3 réflexes du tronc particuliers: le gag reflexe (réflexe nauséeux) médié par le nerf glossopharyngé, le réflexe de fermeture glottique médié par les nerfs récurrents et laryngés supérieurs et le réflexe de toux médié par le vague.
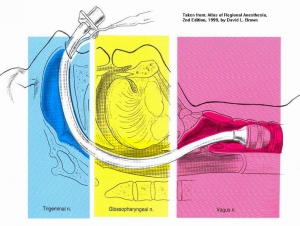
1. L'anesthésie locale de glotte de proche en proche
2. La nébulisation d'anesthésique local
3. Les blocs tronculaires
- a) Le bloc glossopharyngé
Anesthésie de l'oropharynx, de la portion postérieure de la langue et de la face antérieure de l'épiglotte
- b) Le bloc du nerf laryngé supérieur
Anesthésie de la base de la langue, de la surface postérieure de l'épiglotte, des replis aryépiglottiques et des aryténoïdes
-c) Le bloc transtrachéal des nerfs laryngés récurrents
anesthésie des cordes vocales et de la tachée
EN PRATIQUE solution 1 ou solution 2 ou association de 3b + 3c
Lire également:
Regional and Topical Anaesthesia of Upper Airways
Pani M et Al. Indian J Anaesth. Dec 2009; 53(6): 641–648.
14/12/2014
Sellick: Que disent les autres ?
La manoeuvre de Sellick
- Que disent les recommandations et RFE de nos sociétés savantes ?:
Cette manoeuvre est citée dans le document de la SFAR portant sur la "Prise en charge des voies aériennes en anesthésie adulte, à l'exception de l'intubation difficile". Il y est dit qu'elle "peut gêner l’exposition glottique au cours d’une laryngoscopie directe". Elle l'est également dans le document portant sur l'intubation difficile ("Dans le cadre de l’urgence, l’ISR avec manoeuvre de Sellick est la technique de référence"). Dans la recommandation portant sur l'abord trachéal pour la ventilation mécanique des malades de réanimation il est indiqué qu'une "séquence d'induction anesthésique rapide (préoxygénation, administration IV d'un agent anesthésique et d'un curare d'action rapide, compression cricoïdienne) permet d'obtenir de bonnes conditions d'intubation et une protection des voies aériennes". Cette manoeuve est également recommandée dans le document portant sur la sédation et analgésie en structure d’urgence : "La pression cricoïdienne (hors contre-indication) débutée dès la perte de conscience et maintenu jusqu’à la vérification de la position de la sonde endotrachéale. Cette pression cricoïdienne doit être levée en cas de vomissement"
- L'intérêt de la manoeuvre de Sellick n'est cependant plus le même qu'il y a quelques années (1, 2, 3).
- Que lit on dans les recommandations étrangères ?
1. Chez les Sud Africains
Is cricoid pressure necessary ? [Rapid sequence intubation. Emergenc medicine society of South Africa EM015 EM015B]
" We don’t know – the evidence supporting the use of cricoid pressure is fairly limited and there is more and more evidence emerging about the damaging effects of this manoeuvre. It is acceptable to omit the use of cricoid pressure in RSI. It is also acceptable to use cricoid pressure, as long as it is released if it interferes with bag-mask ventilation or laryngoscopy. .
........ The use of cricoid pressure during RSI in the EC is controversial. The consensus of expert opinion at this point in time is that cricoid pressure should be applied after the patient has lost consciousness after the administration of the induction agent and continuously maintained until the cuff has been inflated and the position of the ETT has been confirmed to be correct. This guideline is subject to the following provisos:
• Cricoid pressure should not be used if the assistant is not trained and experienced with the procedure. EMSSA Practice Guidelines provide advice on recommended practice for emergency centres, emergency personnel and emergency care activities. The information within these papers statements is advice only. EMSSA will not be held liable for clinical outcomes related to these Guidelines
• Cricoid pressure should immediately be released and not reapplied if: o There is any difficulty in bag-mask ventilation. o A supraglottic airway device is inserted. o There is any difficulty with laryngoscopy, including if external laryngeal manipulation is required (which cannot be performed while maintaining effective cricoid pressure). o The patient vomits.
• The doctor may also elect not to make use of cricoid pressure at all during the RSI."
2. En Europe du nord
Pre-hospital airway management: Scandinavian Society for Anaesthesiology and Intensive Care Medicine
Ils n'en parlent pas
3. Pour les suédois
Scandinavian clinical practice guidelines on general anaesthesia for emergency situations.
Jensenn AG et Al. Acta Anaesthesiol Scand 2010; 54: 922–950
"The use of cricoid pressure to reduce regurgitation is not based on scientific evidence. Therefore, its use cannot be recommended on the basis of scientific evidence. Anaesthesiologists can use the technique on individual judgement, but the anaesthesiologist must be ready to release the pressure if necessary. Cricoid pressure has been shown to limit the glottic view during laryngoscopy, and it should be releasedif such problems occur."
4. Pour les australiens
Emergency Airway Management in the Trauma Patient
"In conscious patients the cricoid cartilage is palpated between the thumb and middle finger, with the index finger above. The cricoid cartilage is located just below the prominent thyroid cartilage (Adam’s apple). As anaesthesia is induced the pressure is increased in a vertical plane onto the vertebral body of C5. The amount of pressure needs to approximate to 30 Newtons, comparable to the pressure that would feel uncomfortable if applied to the bridge of the nose. Removal of cricoid pressure should only follow securing of the airway and the request of the person performing intubation."
5. Pour les anglais
"Cricoid force: 10N awake 30N anaesthetise. If poor view: Reduce cricoid force. If Failed intubation: Maintain 30N cricoid force. Consider reducing cricoid force if ventilation difficult. If failed oxygenation: Reduce cricoid force during insertion of the LMA"
6. Pour les canadiens
"As cricoid pressure is likely to have potential benefits, its continued use seems prudent during rapid sequence intubation in the patient at high risk of aspiration (Strong recommendation for, level of evidence C). However, if difficulty is encountered with face mask ventilation or tracheal intubation, or if SGD insertion is needed, progressive or complete release of cricoid pressure is justified."
7. Chez les US
Drug-Assisted Intubation in the Prehospital Setting (NAEMSP Position Statement)
"While we recommend the application of cricoid pressure, we note that there are presently no data to support the effectiveness of this technique during prehospital airway management."
| Tags : airway
13/12/2014
Quikclot: Un bon choix, mais les autres aussi
Comparison of novel hemostatic dressings with QuikClot combat gauze in a standardized swine model of uncontrolled hemorrhage.
Rall JM et AL. J Trauma Acute Care Surg. 2013 Aug;75(2 Suppl 2):S150-6
L'emploi des pansements hémostatiques en médecine de l'avant est devenue une pratique courante, même si cette dernière s'appuie sur relativement peu d'arguments avérés. Leur efficacité repose sur leur application au contact de la lésion qui saigne et une compression initiale. Hors ces deux critères de performance sont pas toujours remplis en condition de combat. C'est ce qui explique que certains soient relativement critiques par rapport à leur intérêt réel en condition de combat et on insiste beaucoup actuellement sur la notion de pansement compressif et de packing de plaie. Il n'en demeure pas moins indispensable de connaître ce que propose l'industrie en la matière. Le document proposé fait le point sur le différents produits utilisables. Il utilise pour cela un modèle expérimental de plaie artérielle. Sont comparés trois produits le Quikclot, le Celox et le Chitogauze. 5 versions au total sont analysées car le Quikclot et le Celox sont proposés en deux versions qui diffèrent par leur masse.
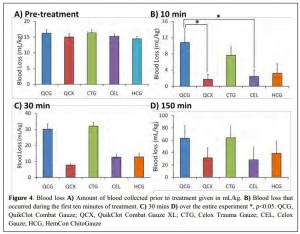

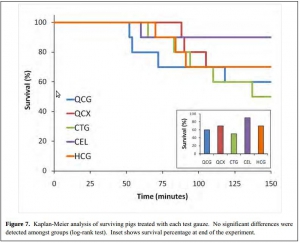
Très globalement plus la masse de produit est grande et plus l'efficacité est au rendez vous (Le Quikclot XL et le Celox, masse de 50 g de pansement) . Parmi les présentations qui proposent une masse de pansement de l'ordre de 20g l'Hemcon Chitogauze apparaît être immédiatement le plus efficace malheureusement est observé un pourcentage de resaignement élevé. Finalement de ce document on peut retenir que l'Hemcon Chitogauze, le CeloxTrauma gauze et le Quikclot Gauze ont des performances similaires. On remarque que pour le Quikclot Gauze la survie à 150 min est la plus élevée pour les pansements de 20 g, même si ceci n'est pas significatif au plan statistique. Ce dernier reste donc un très bon choix. Il est en dotation dans l'armée française .
On rappelle que ce dernier existe en deux version la version rolled et la version Z folded qui est plus particulièrement mise en avant par le fabricant pour les applications militaires.
12/12/2014
HEA: Possible pour les trauma ouverts
Differences between blunt and penetrating trauma after resuscitation with hydroxyethyl starch
Casey JA et Al. J Trauma Acute Care Surg. 2014;77: 859-864
----------------------------------------------------------------
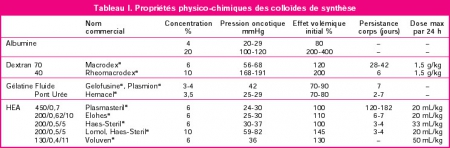
Ce travail effectué avec un HEA ancien (450/07: Hetastarch®, Hextent®) suggère que l'emploi des HEA lors de la prise en charge de trauma ouvert n'est pas associé à un risque accru de décès ou d'insuffisance rénale. On rappelle qu'il ne s'agit pas de la même classe d'HEA que celle que nous avons l'habitude d'utiliser (130/0.4: Voluven)
 ----------------------------------------------------------------
----------------------------------------------------------------
BACKGROUND: The purpose of this study was to test the hypothesis that a single bolus of 6% hydroxyethyl starch (HES 450/0.7 in lactated electrolyte injection) during initial resuscitation has a differential effect in blunt and penetrating trauma patients.
METHODS: Consecutive admissions to the trauma service were reviewed. Patients who died within 24 hours were excluded. Multivariate analysis defined individual predictors for the primary outcomes, acute kidney injury (AKI) and mortality within 90 days. Data were expressed as mean T SD, and significance was assessed at p G 0.05.
RESULTS: Therewere 1,410 patients (76% male; mean T SD, age 43 T 18 years; 68% blunt trauma; mean T SD Injury Severity Score [ISS] 14 T 11; AKI, 4.4%; and mortality, 3.4%). HES (0.5-1.5 L) was administered to 216 patients (15.3%). After multiple logistic regression, HES remained a significant independent predictor of AKI after blunt trauma (odds ratio [OR], 2.54; 95% confidence interval [CI], 1.24-5.19; area under the receiver operating characteristic curve [AUROC], 0.809) but not penetrating
trauma (OR, 0.90; 95% CI, 0.23-3.60; AUROC, 0.849). In separate logistic regression models, HES was a significant predictor of mortality after blunt trauma (OR, 3.77; 95% CI, 0.91-0.97; AUROC, 0.921) but not penetrating trauma (OR, 0.72; 95% CI, 0.13-3.94; AUROC, 0.904).
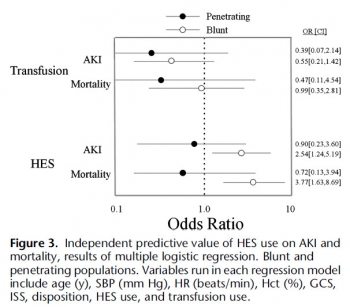
CONCLUSION: HES is an independent risk factor for AKI and death after blunt, but not penetrating, trauma, which underscores a fundamental difference between these two injury types.
| Tags : remplissage
Prehospital management of chest injuries
The prehospital management of chest injuries: a consensus statement. Faculty of Pre-hospital Care, Royal College of Surgeons of Edinburgh
Lee C. et AL. Emerg Med J 2007;24:220–224
---------------------------------------------------------------------------
Un document un peu ancien des nos confrères britanniques mais qui reste d'actualité.
---------------------------------------------------------------------------
This paper provides a guideline for the management of prehospital chest injuries after a consensus meeting held by the
Faculty of Prehospital Care, Royal College of Surgeons of Edinburgh, Edinburgh, UK, in January 2005. An overview of
the prehospital assessment, diagnosis and interventions for life threatening chest injury are discussed, with the application of
skills depending on the training, experience and competence of the individual practitioner
| Tags : thorax
10/12/2014
Echographie: 10 bonnes raisons POUR
Ten good reasons to practice ultrasound in critical care
Lichtenstein D. et AL Anaesthesiol Intensive Ther. 2014 Nov-Dec;46(5):323-35
-----------------------------------------------------------------
Le document proposé est une réflexion faite par un des promoteurs mondial de l'échographie pulmonaire. Il s'agit donc d'un document référence à lire en cliquant sur le lien proposé dans le titre.
-----------------------------------------------------------------
Over the past decade, critical care ultrasound has gained its place in the armamentarium of monitoring tools. A greater understanding of lung, abdominal, and vascular ultrasound plus easier access to portable machines have revolutionised he bedside assessment of our ICU patients. Because ultrasound is not only a diagnostic test, but can also be seen as a component of the physical exam, it has the potential to become the stethoscope of the 21st century. Critical care ultrasound is a combination of simple protocols, with lung ultrasound being a basic application, allowing assessment of urgent diagnoses in combination with therapeutic decisions. The LUCI (Lung Ultrasound in the Critically Ill) consists of the identification of ten signs: the bat sign (pleural line); lung sliding (seashore sign); the A-lines (horizontal artefact); the quad sign and sinusoid sign indicating pleural effusion; the fractal and tissue-like sign indicating lung consolidation; the B-lines and lung rockets indicating interstitial syndromes; abolished lung sliding with the stratosphere sign suggesting pneumothorax; and the lung point indicating pneumothorax. Two more signs, the lung pulse and the dynamic air bronchogram, are used to distinguish atelectasis from pneumonia. The BLUE protocol (Bedside Lung Ultrasound in Emergency) is a fast protocol (< 3 minutes), also including a vascular (venous) analysis allowing differential diagnosis in patients with acute respiratory failure. With this protocol, it becomes possible to differentiate between pulmonary oedema, pulmonary embolism, pneumonia, chronic obstructive pulmonary disease, asthma, and pneumothorax, each showing specific ultrasound patterns and profiles. The FALLS protocol (Fluid Administration Limited by Lung Sonography) adapts the BLUE protocol to be used in patients with acute circulatory failure. It makes a sequential search for obstructive, cardiogenic, hypovolemic, and distributive shock using simple real-time echocardiography in combination with lung ultrasound, with the appearance of B-lines considered to be the endpoint for fluid therapy. An advantage of lung ultrasound is that the patient is not exposed to radiation, and so the LUCI-FLR project (LUCI favouring limitation of radiation) can be unfolded in trauma patients. Although it has been practiced for 25 years, critical care ultrasound is a relatively young but expanding discipline and can be seen as the stethoscope of the modern intensivist. In this review, the usefulness and advantages of ultrasound in the critical care setting are discussed in ten points. The emphasis is on a holistic approach, with a central role for lung ultrasound.
| Tags : échographie
07/12/2014
Echographe et situation isolée: Quid en 2013 ?
Ultrasound in the Austere Environment: A Review of the History, Indications, and Specifications
Russel TC et AL. Military Medicine, 178, 1:21, 2013
----------------------------------------------------------------------------------
L'échographie s'est très largement démocratisée et du fait des améliorations technologiques continues est en passe de devenir un outil incontournable non seulement en médecine d'urgence (1) mais tout simplement en médecine générale. La maîtrise de cette pratique est donc incontournable pour tout médecin militaire projeté. Cependant connaître une technique et la maîtriser sont deux choses différentes, c'est dire l'importance non seulement de la nature des formations initiales et surtout des modalités de maintien des compétences (2). Intégrer cet outil dans son raisonnement clinique impose une réflexion personnelle sur son niveau d'expertise comme celui de pouvoir réaliser de manière fiable l'acquisition de toutes les coupes d'une FAST Echo en 5 min. D'autres indications plus médicales sont bien réelles voire même plus fréquentes. Très certainement, le recours à des outils de simulation trouvera très rapidement une place (3)
----------------------------------------------------------------------------------
In the last 10 years, the use of ultrasound has expanded because of its portability, safety, real-time image display, and rapid data collection. Simultaneously, more people are going into the backcountry for enjoyment and employment. Increased deployment for the military and demand for remote medicine services have led to innovative use and study of ultrasound in extreme and austere environments. Ultrasound is effective to rapidly assess patients during triage and evacuation decision making. It is clinically useful for assessment of pneumothorax, pericardial effusion, blunt abdominal trauma, musculoskeletal trauma, high-altitude pulmonary edema, ocular injury, and obstetrics, whereas acute mountain sickness and stroke are perhaps still best evaluated on clinical grounds. Ultrasound performs well in the diverse environments of space, swamp, jungle, mountain, and desert. Although some training is necessary to capture and interpret images, real-time evaluation with video streaming is expected to get easier and cheaper as global communications improve. Although ultrasound is not useful in every situation, it can be a worthwhile tool in the austere or deployed environment.
| Tags : échographie
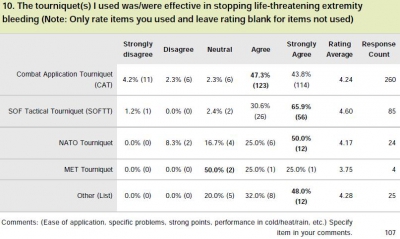
Tourniquet: Que disent les utilisateurs ?
Le garrot en dotation dans l'armée française est le Special Operation Tactical Tourniquet (SOFT-T) , concurrent du Combat Application Tourniquet (CAT). Il existe de nombreux travaux qui cherchent à comparer entre eux les divers produits proposés par l'industrie. Tel garrot semble plus efficace sur des modèles expériemetaux, un autre voit sa barre de torsion se briser, un autre est plus fragile que son concurrent lorsque les conditions de stockage ne sont pas optimales.

Une autre démarche consiste à demander à ceux qui les ont employé en conditions réelles. Une idée est donnée par le tableau qui suit et qui est tiré d'un questionnaire de suivi de mise en oeuvre des équipements du TCCC. Le modèle actuellement en dotation apparaît parfaitement adapté.
Clic sur l'image pour accéder au suivi des équipemens du TCCC
| Tags : tourniquet
Tourniquet: La largeur compte
Tourniquets and Occlusion: The Pressure of Design
Wall PL et AL. Military Medicine, 178, 5:578, 2013
-------------------------------------------------------------------
Cet article est intéressant car il met en évidence que d'autres garrots que les tourniquets du type du CAT sont efficaces en matière d'occlusion notamment ceux basés sur l'emploi de bandes compressives comme le SWAT-T et d'autre part que le niveau de pression d'occlusion observé avec un tourniquet classique peut être associé à un resaignment si l'on observe un relâchement musculaire
-------------------------------------------------------------------
Nerve injuries result from tourniquet pressure. The objective was to determine arterial occlusion and completion pressures with the 3.8-cm-wide windlass Combat Application Tourniquet (CAT) and the 10.4-cm-wide Stretch, Wrap, and Tuck Tourniquet (SWAT-T). Methods: Sixteen volunteers self-applied and had tourniquets applied to their thighs and arms (CAT and SWAT-T, random order, then blood pressure cuffs). Results: Occlusion (Doppler signal elimination) pressures were higher than predicted ( p < 0.0001), highest with the CAT ( p < 0.0001), and often lower than completion pressures (completion median, range: CAT 360, 147–745 mm Hg; SWAT-T 290, 136–449 mm Hg; cuff 184, 108–281 mm Hg). Three CAT thigh and 9 CAT arm completion pressures were >500 mm Hg. Pressure decreases and occlusion losses occurred over 1 minute (pressure decrease: CAT 44 ± 33 mm Hg; SWAT-T 6 ± 8 mm Hg; cuff 14 ± 19 mm Hg; p < 0.0001; loss/initially occluded: CAT 17 of 61, SWAT-T 5 of 61, cuff 40 of 64, p < 0.01). CAT pressures before turn did not have a clear relationship with turns to occlusion. Conclusions: Limb circumference/ tourniquet width occlusion pressure predictions are not good substitutes for measurements. The wider SWAT-T has lower occlusion and completion pressures than the CAT. Decreases in muscle tension lead to decreases in tourniquet pressure, especially with the nonelastic CAT, which can lead to occlusion loss
| Tags : tourniquet
Soutien psychologique durant les phases de déploiement : Guide du chef militaire
RTO-TR-HFM-081 - Stress and Psychological Support in Modern Military Operations
02/12/2014
Echo: Quels requis ?
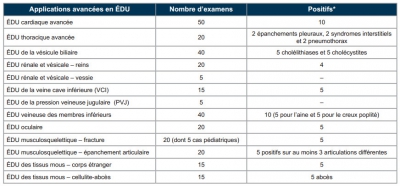
L’échographie ciblée en médecine d’urgence. Nouvelles normes et applications avancées. Position conjointe de l’Association des médecins d’urgence du Québec (AMUQ) et de l’Association des spécialistes en médecine d’urgence du Québec (ASMUQ) adoptée le 7 novembre 2012
La pratique de l'échographie aux urgences est très régulière. Si des formations courtes permettent un apprentissage rapide de techniques de débrouillage comme la FAST Echo, seule une pratique régulière encadrée permet l'acquisition d'une véritable expertise. Le tableau présenté rappelle les prérequis nécessaires à un exercice indépendant chez nos cousins québécois.
| Tags : échographie