30/11/2014
ATLS ? Peut être mais pas pour les seniors !
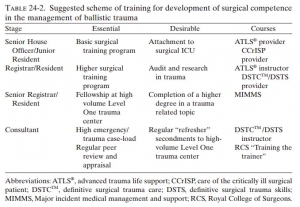
Training to Manage Ballistic Trauma
Boffard KG et Al. in Ballistic Trauma A Practical Guide
La prise en charge d'un polytraumatisé nécessite une approche très structurée et coordonnée qui fait intervenir de multiples professionnels de la médecine d'urgence. L'ATLS est un cours qui fait référence en matière de traumatologie notamment dans les pays anglo-saxons. Son apport réel est discuté notamment dans les pays qui bénéficie d'un environnement hospitalier conséquent (1, 2). L'intérêt réel de cette formation est en train de se repositionner notamment du fait de nouveaux concepts de prise en charge et l'apparition des formation en équipe par simulation en mode immersif. Le document proposé fait le point sur les démarches actuelles de formation à un tel type de prise en charge. Il présente l'ATLS comme une formation plutôt destinée aux plus jeunes, l'expertise nécessaire tant individuelle que collective devant faire appel des des enseignements beaucoup plus conséquents.
Clic sur l'image pour accéder au document
Soutien médical des interventions à risque
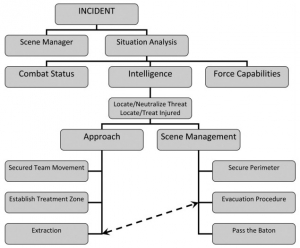
Tactical Medicine: A Joint Forces Field Algorithm
Waldman M et Al. Military Medicine, 179, 10:1056, 2014
Les forces de l'ordre interviennent de plus en plus dans un contexte de violence extrême qui impose la planification du soutien médical de ces opérations selon des principes militaires. Une telle approche est fait par les équipes israélienne. Le document proposé détaille l'algorithme proposé ci dessous.
clic sur l'image pour accéder au document
26/11/2014
Intraosseux: Pourquoi pas la mandibule ?
Intraosseous Vascular Access through the Anterior Mandible – A Cadaver Model Pilot Study
Goldschalt C. et Al. PLoS One. 2014; 9(11): e112686.
-----------------------------------------------------
L'anesthésie intraosseuse est bien connue des chirurgiens dentistes. Pour autant s'agit il d'une voie potentielle d'abord vasculaire ? Peut être, sous réserve de respecter la zone de ponction et éviter le nerf dentaire inférieur.
-----------------------------------------------------
Background
Several insertion sites have been described for intraosseous puncture in cases of emergencies when a conventional vascular access cannot be established. This pilot study has been designed to evaluate the feasibility of the mandibular bone for the use of an intraosseous vascular access in a cadaver model.
Methodology/Principal Findings
17 dentistry and 16 medical students participating in a voluntary course received a short introduction into the method and subsequently used the battery powered EZ-IO system with a 15 mm cannula for a puncture of the anterior mandible in 33 cadavers. The time needed to perform each procedure was evaluated. India ink was injected into the accesses and during the anatomy course cadavers were dissected to retrace the success or failure of the puncture. Dental students needed 25.5±18.9(mean±standard deviation)s and medical students 33±20.4 s for the procedure (p=0.18). Floor of mouth extravasation occurred in both groups in 3 cases. Success rates were 82 and 75% (p=0.93).

Conclusions/Significance
Despite floor of mouth extravasation of injected fluid into a mandibular intraosseous access might severely complicate this procedure, the anterior mandible may be helpful as an alternative to other intraosseous and intravenous insertion sites when these are not available in medical emergencies.
| Tags : intraosseux
BIG: Pas si évident !
The israeli defense force experience with intraosseous access
Nadler R.et All. Mil Med. 2014 Nov;179(11):1254-7
----------------------------------------------------------------------
La réalisation d'un abord vasculaire peut faire appel à la voie intraosseuse. Trois dispositifs sont prévus par la procédure du sauvetage au combat: le trocard de mallarmé, le BIG et l'EZ_IO. Si les études expérimentales sont en faveur de cette pratique, la réalité ne semble pas suivre notamment pour le BIG. Relativement peu de dispositifs ont eu un emploi enregistré avec un taux de succès faible. Peut être un problème de stratégie d'emploi ?
----------------------------------------------------------------------
INTRODUCTION:
Obtaining vascular access is of paramount importance in trauma care. When peripheral venous access is indicated but cannot be obtained, the intraosseous route represents an alternative. The Bone Injection Gun (BIG) is the device used for intraosseous access by the Israeli Defense Force (IDF). The purpose of this study is to assess the success rate of intraosseous access using this device.
METHOD:
The IDF Trauma Registry from 1999 to 2012 was searched for patients for whom at least 1 attempt at intraosseous access was made.
RESULTS:
37 attempts at intraosseous access were identified in 30 patients. Overall success rate was 50%. No differences in success rates were identified between different care givers. Overall mortality was 87%.
CONCLUSION:
The use of BIG in the IDF was associated with a low success rate at obtaining intraosseous access. Although inability to achieve peripheral venous access can be considered an indicator for poor prognosis, the high mortality rate for patients treated with BIG can also stand for the provider's low confidence in using this tool, making its usemaking its use a last resort. This study serves as an example to ongoing learning process that includes data collection, analysis, and improvement, constantly taking place in the IDF
| Tags : intraosseux
25/11/2014
Environnement extrême: Les reco du CIO
International Olympic Committee consensus statement on thermoregulatory and altitude challenges for high-level athletes
Bergeron MF et AL. Br J Sports Med. 2012 Sep;46(11):770-9
Clic sur l'image pour accéder au document
Dermatologie d'altitude: La connnaître
Incidence and Care of Environmental Dermatoses in the High-Altitude Region of Ladakh, India
Singh GK et All. Indian J Dermatol. 2013 Mar-Apr; 58(2): 107–112.
BACKGROUND:
Low humidity, high-velocity wind, excessive ultraviolet (UV) exposure, and extreme cold temperature are the main causes of various types of environmental dermatoses in high altitudes.
MATERIALS AND METHODS:
A retrospective study was carried out in patients visiting the lone dermatology department in Ladakh between July 2009 and June 2010. The aim was to identify the common environmental dermatoses in high altitudes so that they can be treated easily or prevented. The patients were divided into three demographic groups, namely, lowlanders, Ladakhis (native highlanders), and tourists. Data was analyzed in a tabulated fashion.
RESULTS:
A total of 1,567 patients with skin ailments were seen, of whom 965 were lowlanders, 512 native Ladakhis, and 90 were tourists. The skin disorders due to UV rays, dry skin, and papular urticaria were common among all groups. The frequency of melasma (n = 42; 49.4%), chronic actinic dermatitis (CAD) (n = 18; 81.81% of total CAD cases), and actinic cheilitis (n = 3; 100%) was much higher among the native Ladakhis. The frequency of cold-related injuries was much lesser among Ladakhis (n = 1; 1.19%) than lowlanders (n = 70; 83.33%) and tourists (n = 13; 15.47%) (P < 0.05).
CONCLUSION:
Dryness of skin, tanning, acute or chronic sunburn, polymorphic light reaction, CAD, insect bite reactions, chilblain, and frostbite are common environmental dermatoses of high altitudes. Avoidance of frequent application of soap, application of adequate and suitable emollient, use of effective sunscreen, and wearing of protective clothing are important guidelines for skin care in this region.
| Tags : altitude
24/11/2014
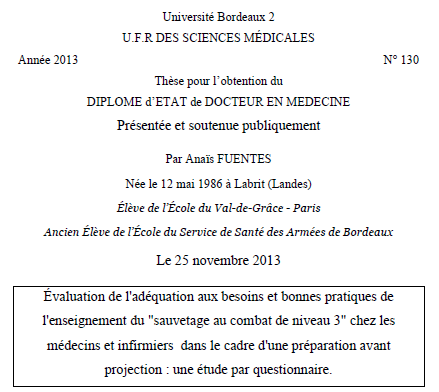
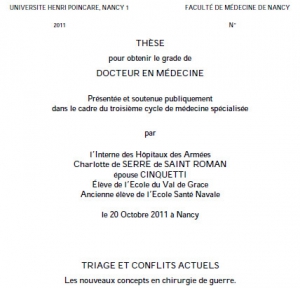
Adéquation aux besoins du SC3
Triage et conflits actuels
TRIAGE ET CONFLITS ACTUELS Les nouveaux concepts en chirurgie de guerre.
Clic sur l'image pour accéder à la thèse
Introduction :
La particularité de la chirurgie de guerre est de devoir tenir compte des impératifs militaires tactiques, du nombre des blessés, du lieu où on opère, des modalités d’évacuation. De ces contraintes, sont nés les concepts d’afflux massifs saturant et de triage. Le but de ce travail est d’analyser les conséquences des conflits actuels sur la prise en charge médico-chirurgicale du blessé de guerre d’aujourd’hui.
Méthode :
Nous commencerons par définir la doctrine classique et la notion de triage du Service de Santé des Armées français. Puis nous présenterons les particularités des nouveaux conflits dans lesquels nos armées sont engagées à partir d’une revue de la littérature internationale. Plusieurs exemples d’afflux massifs auxquels ont été confrontés des équipes du Service de Santé des Armées seront présentés. Nous analyserons le nouveau profil lésionnel du blessé de guerre et les difficultés de prise en charge qui en découlent.
Résultats :
Les conflits armés actuels sont des « conflits asymétriques » opposant des groupements plus ou moins organisés
à des institutions. Ils se déroulent sous l’égide de coalitions, dans un contexte multinational. Sur le plan médical, les lésions par explosion sont prépondérantes, l’atteinte des membres prédomine. Les conventions de Genève n’offrent plus de protection justifiant un renforcement de la formation militaire des personnels de service de santé. Par ailleurs, ces conflits surviennent dans un contexte de sur-médiatisation, qui influence l’opinion publique française concernant les pertes et l’acceptation même de la notion de triage. La judiciarisation des affaires militaires est incontournable, y compris dans la prise en charge chirurgicale. Une nouvelle catégorisation de triage a été mise au point afin d’utiliser une catégorisation compréhensible par tous en milieu multinational. En amont du triage, les aspects logistiques et militaires ont été optimisés. Une nouvelle structure hospitalière (rôle 3) est déployée, des formations adaptées au théâtre sont proposées. Enfin, la prise en charge thérapeutique du blessé de guerre s’est améliorée ; le recours aux techniques de « Damage Control », l’évacuation précoce vers la métropole et la mise en place du lot de chirurgie vitale ont permis une diminution de la morbi-mortalité de ces conflits.
Conclusion :
La confrontation du service de santé des armées à ces nouveaux conflits a permis la mise en place de nouvelles méthodes thérapeutiques et d’améliorer les aspects logistiques concernant le déploiements des moyens de santé. Cette amélioration est à poursuivre dans la formation des personnels et dans le suivi épidémiologique des blessés de guerre.
| Tags : thèse
23/11/2014
Coniotomie: Quel diamètre ?
Morphometric analysis and clinical application of the working dimensions of cricothyroid membrane in south Indian adults: With special relevance to surgical cricothyroidotomy
Prithishkumar IJ et Al. Emergency Medicine Australasia (2010) 22, 13–20
-------------------------------------------------------------------
L'anatomie de la membrane cricoïdienne fait l'objet de nombreuses description. Un des intérêts de ces dernières est de préciser la taille de cette dernière et d'en déduire le diamètre de canule/sonde le plus adapté pour une insertion intratrachéale. Il existe de grandes variations selon les populations étudiées, ici indienne. On peut retenir pour notre population militaire essentiellement masculine une hauteur de 6 mm pour une largeur de 8 mm. C'est pourquoi la taille maximale des canules insérées à ce niveau ne doit excéder ces dimensions.
-------------------------------------------------------------------
Objective: To measure the working dimensions of the cricothyroid membrane in the adult south Indian population and to establish the association between the working dimensions and the appropriate endotracheal tube size for the purpose of cricothyroidotomy.
Methods: Cross-sectional evaluation of 50 fresh adult autopsy cases (35 men, 15 women) in a medical university teaching hospital in South India.
Results: Age ranged from 17.0 to 83.0 years. Working dimensions of the membrane in neutral position of neck, in men: width = 8.41 2.11 mm, height = 6.57 1.87 mm; in women: width = 6.30 1.29 mm, height = 5.80 1.56 mm. Depth of the subglottic larynx at the level of cricoid cartilage: men = 20.73 1.97 mm, women = 15.62 1.71 mm. Distance of the lower border of cricothyroid membrane from suprasternal notch in neutral position of neck, in men = 5.18 1.76 cm, women = 4.72 1.55 cm; in passively extended neck, men = 7.86 1.25 cm, women = 8.05 1.28 cm. Regression equations have been derived to determine endotracheal tube size for cricothyroidotomy, based on distance between sternal notch and chin, and height of the individual (P < 0.05).
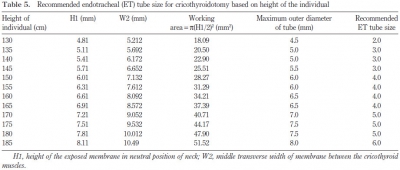
Conclusions: Working dimensions are smaller in the Indian group compared with western publications. Endotracheal tubes ranging from size 3.0 to 6.0 might be used for cricothyroidotomy in the adult south Indian population.
| Tags : coniotomie, airway
22/11/2014
Echographie en role2/3
Trauma resuscitation using echocardiography in a deployed military intensive care unit
Hutchings Sj et Al. JICS 2013:14, 120-125
Medical Aspects of Biological Warfare
- History of Biological Weapons: From Poisoned Darts to Intentional Epidemics
James W. Martin, George W. Christopher, and Edward M. Eitzen, Jr. - Food, Waterborne, and Agricultural Diseases
Zygmunt F. Dembek and Edwin L. Anderson - Epidemiology of Biowarfare and Bioterrorism
Zygmunt F. Dembek, Julie A. Pavlin, and Mark G. Kortepeter - Anthrax
Bret K. Purcell, Patricia L. Worsham, and Arthur M. Friedlander - Plague
Patricia L. Worsham, Thomas W. McGovern, Nicholas J. Vietri, and Arthur M. Friedlander - Glanders
Bridget Carr Gregory and David M. Waag - Melioidosis
Nicholas J. Vietri and David Deshazer - Tularemia
Matthew J. Hepburn, Arthur M. Friedlander, and Zygmunt F. Dembek - Brucellosis
Bret K. Purcell, David L. Hoover, and Arthur M. Friedlander - Q Fever
David M. Waag - Smallpox and Related Orthopoxviruses
Peter B. Jahrling, John W. Huggins, M. Sofi Ibrahim, James V. Lawler, and James W. Martin - Alphavirus Encephalitides
Keith E. Steele, Douglas S. Reed, Pamela J. Glass, Mary Kate Hart, George V. Ludwig, William D. Pratt, Michael D. Parker, and Jonathan F. Smith - Viral Hemorrhagic Fevers
Peter B. Jahrling, Aileen M. Marty, and Thomas W. Geisbert - Staphylococcal Enterotoxin B and Related Toxins
Robert G. Ulrich, Catherine L. Wilhelmsen, and Teresa Krakauer - Ricin
Mark A. Poli, Chad Roy, Kermit D. Huebner, David R. Franz, and Nancy K. Jaax - Botulinum Toxin
Zygmunt F. Dembek, Leonard A. Smith, and Janice M. Rusnak - Additional Toxins of Clinical Concern
Kermit D. Huebner, Robert W. Wannemacher, Jr., Bradley G. Stiles, Michel R. Popoff, and Mark A. Poli - Laboratory Identification of Biological Threats
Erik A. Henchal, George V. Ludwig, Chris A. Whitehouse, and John M. Scherer - Consequence Management: The National and Local Response
Kermit D. Huebner and James W. Martin - Medical Management of Potential Biological Casualties: A Stepwise Approach
Theodore J. Cieslak and George W. Christopher - Medical Countermeasures
Janice M. Rusnak, Ellen F. Boudreau, Matthew J. Hepburn, James W. Martin, and Sina Bavari - Biosafety
Catherine L. Wilhelmsen and Robert J. Hawley - Biosurety
Gretchen L. Demmin - Ethical and Legal Dilemmas in Biodefense Research
Jeffrey E. Stephenson and Arthur O. Anderson - Emerging Infectious Diseases and Future Threats
Chris A. Whitehouse, Alan L. Schmaljohn, and Zygmunt F. Dembek
Medical Management of Chemical Casualties
Chapter 1. Lung-Damaging Agents
Chapter 2. Cyanide
Chapter 3. Vesicants
Chapter 4. Nerve Agents
Chapter 5. Incapacitating Agents
Chapter 6. Riot-Control Agents
Chapter 7. Decontamination
Chapter 8. Casualty Management in a Contaminated Area
Chapter 9. Individual Protective Equipment
Appendices
Index
21/11/2014
Simuler 1 fois par an: Suffisant ?
Complex procedural skills are retained for a minimum of 1 yr after a single high-fidelity simulation training session
Boet S.et All. Br. J. Anaesth. (2011) 107 (4): 533-539
-----------------------------------------------------------------------------------
Certaines procédures de mise en condition de survie sont rarement réalisées en conditions réelles. Pourtant leur maîtrise par le personnel qui intervient doit être acquise. Se pose dès lors le problème de l'acquisition et du maintien de ces compétences techniques. la simulation est un moyen d'y parvenir. La coniotomie fait partie des ces gestes. Récemment il a été mis en avant que 5 réalisations simulées par des professionnels de l'urgence permettaient d'obtenir une relative maîtrise techniqe mais que cette dernière ne se maintenait pas au delà de 6 mois. (1). Le travail présenté confirme ces données.
-----------------------------------------------------------------------------------
Background. Simulation has been shown to be effective in teaching complex emergency procedural skills. However, the retention of these skills for a period of up to 1 yr has not been studied. We aimed to investigate the 6 month and 1 yr retention of the complex procedural skill of cricothyroidotomy in attending anaesthetists using a high-fidelitysimulated cannot intubate, cannot ventilate (CICV) scenario.
Methods. Thirty-eight attending anaesthetists participated individually in a high-fidelitysimulated CICV scenario (pretest) that required a cricothyroidotomy for definitive airway management. Immediately after a debriefing and structured teaching session on cricothyroidotomy insertion, subjects managed a second identical CICV scenario (posttest). Each anaesthetist was randomized to either a ‘6 month retention’ or a ‘12 month retention’ group. No further teaching occurred. At their respective retention times, each anaesthetist managed a third identical CICV scenario (retention post-test). Two blinded experts independently rated videos of all performances in a random order, using a specific checklist (CL) score, a global-rating scale (GRS) score, and procedural time (PT).
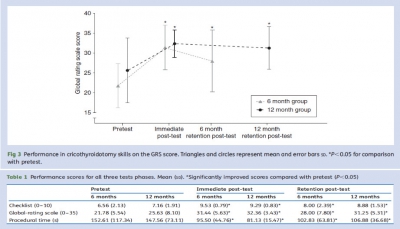
Results. Subjects from both groups improved on their cricothyroidotomy skill performances from pretest to immediate post-test and from pretest to retention post-test, irrespective of the retention interval; CL mean (SD) 8.00 (2.39) vs 8.88 (1.53), P¼0.49; GRS 28.00 (7.80) vs 31.25 (5.31), P¼0.25; PT 102.83 (63.81) s vs 106.88 (36.68) s, P¼0.73.
Conclusions. After a single simulation training session, improvements in cricothyroidotomy skills are retained for at least 1 yr. These findings suggest that high-fidelity simulation training, along with practice and feedback, can be used to maintain complex procedural skills for at least 1 yr
| Tags : simulateurs
19/11/2014
Une bougie dans la sonde: c'est mieux.
Comparison of Intubation Performance by Emergency Medicine Residents Using Gum Elastic Bougie versus Standard Stylet in Simulated Easy and Difficult Intubation Scenarios
Walsh RM et All. Emerg Med Australas - ; 26 (5); 446-9
Study Objectives: We sought to evaluate the success rate and time to endotracheal intubation by emergency medicine residents with stylet reinforced endotracheal tube (ETT-S) versus intubation with a gum elastic bougie (GEB) in simulated easy and difficult airways on a cadaveric model.
Methods: The study was a prospective cross-over design using a single study cohort of 29 emergency medicine residents. A fresh frozen cadaver was used in either standard positioning to facilitate a Cormack Lehane Grade 1 laryngoscopy, or with a hard cervical collar applied a Cormack Lehane Grade 3 laryngoscopy. Each participant then intubated the cadaver in each setting (Grade 1 ETT-S, Grade 1 GEB, Grade 3 ETT-S, Grade 3 GEB). The primary end-point of our investigation was the time to intubation. Secondary endpoints were: success rate of intubation, mean ratings by study participants of perceived ease of intubation for each intubation technique in each simulated degree of difficulty, and overall preference of intubation technique in each simulated degree of difficulty. To assess the effect of intubation type (GEB vs ETT-S) and difficulty on time to successful intubation and perceived ease of intubation, repeated measures ANOVAs were conducted. To examine whether success of intubation differed across the GEB and ETT-S groups we used a McNemar’s test. To examine the effect of previous experience on time to intubation, we used a mixed model ANOVA incorporating intubation type and difficulty of intubation.
Results: Mean time to intubation in all scenarios ranged from 28.8 – 116.6 seconds. Year of residency training trended toward significance but was not significant when comparing post-graduate year to time to intubation (p¼ 0.07). Time to intubation was significantly different only when comparing Grade 3 ETTS to Grade 3 GEB (p¼ 0.006). Of the 116 intubations performed in this study, a total of 36 were failed attempts. There was no significant difference in success rate when comparing Grade 1 ETT-S to Grade 1 GEB nor Grade 3 ETT-S to Grade 3 GEB (p ¼ >0.05). Across all year groups, participants perceived the Grade 1 scenario to be easier than the Grade 3 scenario. At the conclusions of the study, 55% of participants preferred using the GEB in all settings. When broken down by scenario, 41% preferred the GEB in the Grade 1 scenario while 76% preferred the GEB in the Grade 3 scenario.
Conclusions: Time to intubation in a simulated grade 3 view was significantly longer in the GEB group versus the ETT-S group. Although the differences in success rates were not statistically significant, there was a trend toward more successful intubations with the GEB in the simulated grade 3 view. This is important because in the emergency department when difficult airways can be high stress and life threatening, although the GEB group took more time, the success rates were higher.
| Tags : intubation
18/11/2014
Carum 2014 blessé cervico-maxillo-facial
CARUM 2014 BlesséCervicoMaxilloFacial.pdf
La communication de l'IHA Thill C de l'HIA Clermont Tonnerre
17/11/2014
Pneumothorax et vol en altitude : Possible ?
Cleared for takeoff: The effects of hypobaric conditions on traumatic pneumothoraces
Majercik S. et All. J Trauma Acute Care Surg. 2014;77: 729-733
| Tags : pneumothorax
Doctrine du soutien médical aux engagements opérationnels
| Tags : doctrine
13/11/2014
Drain thoracique: Confirmation, pas si simple
An audit of the complications of intercostal chest drain insertion in a high volume trauma service in South Africa.
Kong V. et All. Ann R Coll Surg Engl. 2014 Nov;96(8):609-13
Intercostal chest drain (ICD) insertion is a commonly performed procedure in trauma and may be associated with significant morbidity.
METHODS:
This was a retrospective review of ICD complications in a major trauma service in South Africa over a four-year period from January 2010 to December 2013.
RESULTS:
clic sur l'image pour accéder au document SAMU 69
A total of 1,050 ICDs were inserted in 1,006 patients, of which 91% were male. The median patient age was 24 years (interquartile range [IQR]: 20-29 years). There were 962 patients with unilateral ICDs and 44 with bilateral ICDs. Seventy-five per cent (758/1,006) sustained penetrating trauma and the remaining 25% (248/1006) sustained blunt trauma. Indications for ICD insertion were: haemopneumothorax (n=338), haemothorax (n=314), simple pneumothorax (n=265), tension pneumothorax (n=79) and open pneumothorax (n=54). Overall, 203 ICDs (19%) were associated with complications: 18% (36/203) were kinked, 18% (36/203) were inserted subcutaneously, 13% (27/203) were too shallow and in 7% (14/203) there was inadequate fixation resulting in dislodgement. Four patients (2%) sustained visceral injuries and two sustained vascular injuries. Forty-one per cent (83/203) were inserted outside the 'triangle of safety' but without visceral or vascular injuries. One patient had the ICD inserted on the wrong side. Junior doctors inserted 798 ICDs (76%) while senior doctors inserted 252 (24%). Junior doctors had a significantly higher complication rate (24%) compared with senior doctors (5%) (p<0.001). There was no mortality as a direct result of ICD insertion. </sec> Conclusions ICD insertion is associated with a high rate of complications. These complications are significantly higher when junior doctors perform the procedure. A multifaceted quality improvement programme is needed to improve the situation.
| Tags : drainage thorax
12/11/2014
Prevention and Treatment of Acute Altitude Illness
Wilderness Medical Society Consensus Guidelines for the Prevention and Treatment of Acute Altitude Illness
Luks AM et All. Wilderness Environ Med. 2010 Jun;21(2):146-55
To provide guidance to clinicians about best practices, the Wilderness Medical Society (WMS) convened an expert panel to develop evidence-based guidelines for the prevention and treatment of acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high altitude pulmonary edema (HAPE). These guidelines present the main prophylactic and therapeutic modalities for each disorder and provide recommendations for their roles in disease management. Recommendations are graded based on the quality of supporting evidence and balance between the benefits and risks/burdens according to criteria put forth by the American College of Chest Physicians. The guidelines also provide suggested approaches to the prevention and management of each disorder that incorporate these recommendations.
| Tags : altitude
Hypothermie accidentelle: Guidelines 2014 de la WMS
Wilderness Medical Society Practice Guidelines for the Out-of-Hospital Evaluation and Treatment of Accidental Hypothermia
Zaphren K. et All. Wilderness Environ Med. 2014 in press
----------------------------------------------------
Doit être remarqué la recommandation de ne pas mobiliser le blessé hypotherme pendant au moins 30 min après la mise en oeuvre des techniques de réchauffement. Ceci a pour objet de limiter les effets de l'afterdrop, mécanisme par lequel le réchauffement peut transitoirement aggraver l'hypothermie centrale par un mécanisme de recirculation de sang froid.
----------------------------------------------------

1. The key factors to guide treatment are level of consciousness, shivering intensity, and cardiovascular stability, based on blood pressure and cardiac rhythm Core temperature can provide additional helpful information (panel consensus).
2. A patient who is shivering but able to function well and to care for himself or herself is unlikely to be hypothermic. A patient who is shivering, becoming incapacitated, and having difficulty caring for himself or herself is likely to be hypothermic. If there is any doubt, assume that the patient is hypothermic (panel consensus).
3. Because the temperature ranges to which the HT grades are meant to correspond are the same as the standard classification, rescuers should refer to mild, moderate, severe, and profound hypothermia (<24°C) on the basis of their clinical observations, remembering that shivering can occur below 32°C, usually with altered mental status, and that patients can have detectable vital signs with core temperatures below 24°C (panel consensus).
4. Clinicians should consider causes other than hypothermia to explain altered mental status or lack of shivering that does not correlate with the measured core temperature or by a history of minimal cold exposure (panel consensus).
5. In a patient whose airway has been secured with an endotracheal tube or with a supraglottic airway that has a port for placing a gastric tube, use esophageal temperature monitoring with the esophageal temperature probe inserted into the lower third of the esophagus (1C).
6. Use an epitympanic thermometer designed for field conditions with an isolating ear cap in a patient whose airway has not been secured by endotracheal intubation or a supraglottic airway or in a patient with a secured airway if an esophageal probe is not available (1C)
7. Rectal temperature should not be measured in the field until the patient is in a warm environment (1C).
8.Use oral temperature measurement with a thermometer (electronic or liquid-filled) that can read below 35°C only to rule out hypothermia (1A).
9. Monitor rectal or bladder temperature during rewarming of an unconscious patient only if an esophageal or epitympanic probe is not available. If rectal or bladder temperature is used for monitoring during rewarming, allow for inaccuracy owing to the time lag behind core temperature changes (1A).
10. Do not use a temporal artery thermometer in a possibly hypothermic patient (1C)
11. The decision to rescue or to resuscitate a potentially severely hypothermic patient should only be made after the scene is secure and safe for the rescuers to enter and make an evaluation (1A). After safety of rescuers has been assured, the priorities in out-of-hospital treatment of a hypothermic patient who is not in cardiac arrest are to avoid causing cardiovascular collapse during rescue, to prevent a further decrease in core temperature (afterdrop), and to rewarm the patient in a safe manner. If a hypothermic patient is in cardiac arrest, rescuers should initiate resuscitation, if indicated.
12. Rescuers should keep a hypothermic patient horizontal, especially during rescue from water or from a crevasse (1B) and should limit physical effort by the patient during rescue (1B). A conscious patient should be encouraged to be vigilant and focus on survival (1C).
13. Handle a hypothermic patient gently and continue to keep the patient horizontal (1B). Avoid any disturbance, especially movement of the extremities that might precipitate VF (1B). Once the patient is in a warm environment, clothes should be cut off rather than removed manually (1B)
14. Protect from further cooling by using insulation and a vapor barrier until the patient has reached a warm environment, such as the interior of an ambulance. Remove wet clothes, preferably by cutting them off, only when the patient has been protected from the cold (1C). Take special care to insulate the patient from the ground (eg, with sleeping pads) to protect from conductive heat loss and also to protect the head and neck by closing the area around the face as effectively as possible (1C).
15. Use an outer windproof layer to protect the patient from wind and especially from rotor wash when loading or unloading from a helicopter (1C).
16. Shivering is an effective method of rewarming a patient who is cold but not hypothermic or who is mildly hypothermic. The patient must have sufficient energy reserves to sustain shivering and must be adequately insulated from the environment to retain the heat that is generated (1A)
17. An alert patient who is shivering, and who is not at risk for aspiration, should receive high-carbohydrate liquids and food. Liquids and food may be warmed but should not be hot enough to cause burns (1C).
18. Initially, a hypothermic patient should not be allowed to stand or walk (1C)
19. A shivering patient who may be hypothermic should be kept as warm as possible, given calorie replacement, and observed for at least 30 minutes before exercising. The patient should be monitored closely. An alert patient may be allowed to stand. If the patient can stand without difficulty, exercise intensity should start low and increase gradually as tolerated (1C)
20. Large heat pads should be used, if available (1B). Rewarming devices should be used in conjunction with vapor barriers and insulation (1C). The HeatPac should only be used outdoors or with proper ventilation that is carefully monitored (1B).
21. Body-to-body rewarming can be used in mild hypothermia to increase patient thermal comfort if enough personnel are available and if it does not delay evacuation to definitive care (1B).
22. Apply heat sources to the axillae, chest, and back. A large heat pad or blanket should be placed over the chest and, if large enough, extended into the axillae and under the back (1B). Additional heat, if available, can be applied to the neck if precautions are taken to prevent heat loss through any neck opening (1C). Avoid applying external heat to the extremities, although it is not necessary to insulate the arms from heat applied to the torso (1B).
23. The HPMK can be used as a convenient and effective means of preventing heat loss and providing active external rewarming (1C).
24. Avoid localized pressure to cold skin. Heat should never be applied directly to the skin. A barrier should be used to prevent burning the skin when using chemical or electrical heat pads or warm water bottles (1C).
25. Do not use small chemical heat packs for rewarming a hypothermic patient (1B). Small chemical heat packs can be used to prevent local cold injury to the hands and feet during treatment and transport (1C).
26. Heated humidified oxygen can be used in combination with other rewarming methods (2C), but should not be relied on as the only rewarming method (1B).
27. Do not use a warm shower or bath for rewarming, even if a patient appears to be only mildly hypothermic (1C).
28. Distal limb warming to the elbows and knees in 421C to 451C water can be used for rewarming a patient with mild hypothermia (1C).
29. Forced-air warming should be used during air or ground transport, if available (1A). If forced-air warming is not available, use of heat pads, including the HPMK, can be continued. Care must be take to prevent CO buildup with the charcoal HeatPac in a ground ambulance; this can be done by igniting the device outside the vehicle, bringing it inside only after initial smoke production subsides, ventilating the vehicle compartment, and monitoring CO (1C). HeatPac should not be used in an aircraft (1C).
30. Patient compartments in ground and air ambulances should be heated to at least 241C, if possible, to decrease further heat loss (1C).
31. A cold-stressed patient who is not hypothermic does not need to be kept horizontal. The patient may be allowed to remove his or her own wet clothing and to put on dry clothing without shelter, if necessary. The patient may be allowed to rest in a sitting position, to eat and drink to maintain energy reserves and hydration, and may move or keep moving, if necessary (panel consensus).
32. Fixed, dilated pupils, apparent rigor mortis, and dependent lividity are not contraindications to resuscitation of a severely hypothermic patient (1A for fixed, dilated pupils and apparent rigor mortis; 2C for dependent lividity). If there are no contraindications to cardiopulmonary resuscitation (CPR), rescuers should not give up hope and should attempt resuscitation (1A).
33. Do not attempt to resuscitate a patient with obvious fatal injuries or whose chest wall is too stiff for compressions (1A).
34. Do not attempt resuscitation in an avalanche victim buried for 35 minutes or longer with an airway that is definitely obstructed by snow or ice (1A).
35. Rescuers should make every effort to move the patient to a warm setting, such as a ground or air ambulance or a medical facility where cardiac monitoring is available to guide resuscitation and to start rewarming (1C). Before starting CPR, feel for a carotid pulse for 1 minute. If there is no detectible pulse after 1 minute, start CPR, including rescue breathing (1C).
36. CPR should be started if a nonperfusing rhythm, including ventricular tachycardia (VT), VF, or asystole, is detected. If there is a cardiac rhythm with organized QRS complexes (other than VT), CPR should not be performed (1C) unless ETCO2 monitoring confirms lack of perfusion or echocardiography shows that there are no cardiac contractions corresponding to electrical activity (1B).
37. If shock is advised by the AED, attempt defibrillation and start CPR. If no shock is advised on an AED, no carotid pulse is found after palpating for at least 1 minute, normal breathing or other signs of life are not observed, and ultrasound is not available to verify cardiac activity or pulses, start CPR (1C).
38. In patients with severe or profound hypothermia, CPR can be delayed (“scoop and run”) and can be given intermittently during evacuation if it is not technically possible or safe to perform continuous CPR (1C). CPR can be given for several hours, if necessary (1B).
39. If there is no contraindication to CPR and no indication to terminate CPR, continue resuscitation attempts in a patient even if the core temperature is below 101C measured by an esophageal probe in the lower third of the esophagus (2C).
40. If a cardiac monitor is available, use maximal amplification to search for QRS complexes (1C).
41. If a monitor or defibrillator shows VT or VF or if shock is advised by an AED in a patient whose core temperature is thought to be below 301C, give a single shock at maximal power (1C).
42. Wait until a patient has been rewarmed at least 11C to 21C or to 301C before attempting further shocks (2C). Once the core temperature reaches 301C, follow defibrillation guidelines for normothermic patients (1C).
43. For cardiac arrest in a hypothermic patient, deliver chest compressions at the same rate as in normothermic patients (1C).
44. In the absence of ETCO2 monitoring, deliver ventilations at the same rate recommended for a normothermic patient,11,17 unless an advanced airway is in place (see below) (2C).
45. gement. Recommendation. In a patient with an advanced airway, if ETCO2 monitoring is not available, deliver ventilations at half the rate recommended for a normothermic patient to avoid hyperventilation (1C).
46. If ETCO2 monitoring is available, keep ETCO2 within the normal range. In rescues at altitudes above 1200 m, ALS personnel should be aware of the normal range of ETCO2 at a given altitude (1C).
47. High-quality CPR can be performed effectively during prolonged transport using a mechanical device (1C).
48. The advantages of advanced airway management outweigh the risk of causing VF (1C). A nasogastric or orogastric tube should also be placed to decompress the stomach, after the airway is secured (1C).
49. Below a core temperature of 301C, dosages of anesthetic and neuromuscular blocking agents should be lowered and intervals extended according to the degree of hypothermia. Current data are insufficient to recommend specific protocols (1C).
50. A hypothermic patient may receive supplemental oxygen, especially at altitudes greater than 2500 m. There is potential benefit and no known harm (1C).
51. If circulatory access cannot immediately be obtained with a peripheral IV catheter, access should be obtained by the IO method (1C). Central venous access can be obtained using a femoral line if no other option is available (1C).
52. Resuscitate a hypothermic patient with normal saline warmed to 401C to 421C given IV or IO. Use caution to prevent volume overload (1B).
53. When practical, fluids should be given as boluses rather than by continuous infusion (1C). The goal of fluid administration should be to maintain systolic blood pressure at a level that provides adequate perfusion, depending on the degree of hypothermia (1C).
54. Glucose should be administered to a hypothermic patient who is hypoglycemic (1A). Insulin is not initially indicated for hyperglycemia (1B). If glucose testing is not available, IV glucose can be administered empirically to a hypothermic patient with altered mental status (1C).
55. Transcutaneous pacing may be beneficial in hypothermia in the setting of bradycardia with hypotension disproportionate to the core temperature (2C).
56. No treatment is indicated for atrial dysrhythmias in a hemodynamically stable patient during rewarming (IB).
57. A severely injured patient should be treated early and aggressively with active rewarming during all phases of out-of-hospital care to prevent hypothermia (1B).
58. To prepare a patient for transport, potential spinal injuries should be stabilized105 (1C). Fractures and dislocations should be reduced as much as possible to normal anatomic configuration (1C). Open wounds should be covered (1C).
59. An uninjured patient who is completely alert and shivering may be treated without being transported to a hospital (1B).
60. If injuries meet trauma criteria, a patient should be transported to a trauma center (1B). An asphyxiated patient should be transported to a hospital for observation (1B).
61. A patient with moderate to severe hypothermia who is hemodynamically stable can be transferred to the closest hospital or other appropriate medical facility such as a rural clinic (1C). A patient who is hemodynamically unstable or who has a core temperature less than 281C should be transferred to a hospital capable of providing critical care and ECC, if possible. If this will require significant additional time—generally more than an additional hour—of non– critical care transport the patient should first be stabilized at a closer facility (1C). A patient in cardiac arrest should be transferred to a hospital capable of providing ECC if possible. If all other factors are equal, ECMO is preferable to CPB (1B). In geographic regions where there is no hospital capable of providing ECC or when a hospital capable of providing ECC is not accessible, transport a patient in cardiac arrest to the closest hospital where serum potassium can be measured and where resuscitation methods not involving ECC can be attempted for a patient whose serum potassium is 12 mmol/L or less. (Please see following section for use of biochemical markers.) (1C).
62. If an adult hypothermic patient has a potassium greater than 12 mmol/L, CPR should be terminated (1B).
63. An avalanche victim buried 35 minutes or less or with a core temperature of at least 321C should receive standard resuscitation, including CPR if in cardiac arrest67,120 (1C). If there is ROSC, the victim should be transported to the nearest hospital that can manage any associated injuries (1C). An avalanche victim who was buried more than 35 minutes or who has a core temperature less than 321C and has detectable vital signs should be transported to the nearest hospital or rural clinic for active rewarming (1C). If there are no vital signs and the airway is patent, CPR should be started67 (1B). An avalanche victim in cardiac arrest with an airway that is definitely obstructed should not be resuscitated if burial time was greater than 35 minutes or core temperature is less than 321C67 (1C). If there is any chance that the airway was patent, a short trial of CPR is warranted (1B).
64. An avalanche victim with CPR in progress should be transported to a hospital with the capability of performing extracorporeal rewarming if possible (1B). If it is not practical for the patient to go directly to a hospital that can perform extracorporeal rewarming and serum potassium has not already been measured, the patient should be transported to a hospital or clinic capable of measuring serum potassium (1C). Resuscitation should be continued only if serum potassium is 12 mmol/L or less (1B).
| Tags : hypothermie