24/12/2017
AAST 2017: Utilité du TXA encore questionnée
Late TXA utilization is associated with Iincreased blood product transfusion: A secondary analysisof the pragmatic randomized optimal platelet and plasma ratios (PROPPR) study
Aravind K. et AL . Session: XIIIA: Papers 45-54: Preclincial/Translational Science Paper 52
-----------------------------------
Ce poster présenté au dernier AAST 2017 est une ré-interprétation de données de l'étude POPR. Il semblerait qu'au delà des premières heures l'administration précoce (dans la 1ère heure) de TXA n'améliore pas la survie à 24h et un mois. L'administration tardive (après la 1ère heure mais avant la 3ème) majorerait les besoins transfusionnels. Les auteurs de ce poster attirent l'attention sur la disparité des groupes comparés, ce qui peut expliquer leurs résultats.
-----------------------------------
Introduction:
Exsanguination is the leading cause of preventable death after trauma. In addition to a balanced ratio blood component strategy, tranexamic acid (TXA) is used as an adjunct in hemorrhaging patients. This secondary analysis was performed to determine the incidence of TXA utilization and outcome in patients predicted to receive a massive transfusion (MT) in level 1 trauma centers.
Methods:
Trauma patients who were predicted to require a MT and admitted to 12 level I North American trauma centers were studied. Patients were divided into those who received TXA and those who did not. We examined 3 hour, 24 hour, and 30 day mortality. We also examined incidence of thromboembolic events, blood product administration within the first 24 hours, length of stay (hospital free days), ICU free days, as well as development of complications including acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), sepsis, and multisystem organ failure (MOF). In our multivariate analysis, we controlled for Injury Severity Score (ISS), Glasgow Coma Scale (GCS), treatment group, mechanism of injury, hypotension and/or tachycardia on admission, geriatric patient (age > 65), and site as independent variables.
Results:
137 out of 680 (20.1%) patients in the PROPPR study received TXA with 130 patients receiving TXA within the first 3 hours after admission. Other adjunctive therapies administered included cryoprecipitate (25.4%), and others (6.6%). The incidence of TXA administration did not differ between the ratio groups (50.3% vs 47.4%, p=0.55), but patients receiving TXA were more severely injured with a median ISS of 34(21) vs 26(20), p<0.01 and a lower median(IQR) GCS of 9(12) vs 14(12), p<0.01. Multivariate linear regression analysis revealed no association between TXA administration and blood transfusion requirements (Table 1). Further analysis revealed that patients who received late (from >1 hour to ≤3 hours after arrival) TXA (41 patients) experienced increased blood requirements in the first 24 hours (Table 1) compared to those remaining 543 patients that did not receive TXA. There was no difference in blood product requirement in those patients who received TXA early (≤1 hour) (89 patients) versus those that did not receive TXA. In patients that receiv ed TXA, there was an increased incidence of ARDS(OR (95% CI) 1.99 (1.06,3.73), p=0.03), AKI (1.90 (1.13,3.20), p=0.01), and MOF (4.18 (1.52,11.48), p<0.01) even when controlling for the factors mentioned above. There was also a difference in adjusted 3 hour mortality (OR (95% CI) 0.22 (0.07,0.73), p=0.01) but not 24 hour (0.61 (0.30,1.24), p=0.18) or 30 day mortality (1.42 (0.78,2.59), p=0.25) for any TXA administration. There was no difference in adjusted thromboembolic events or adjusted length of stay. Subgroup analysis with additional variables that were found to have a difference between groups with a p<0.20 were added to the regression model including hematocrit, platelet count, international normalized ratio, creatinine, lactate, and R value on thrombelastography. This analysis showed an increase in PRBC transfusion with late TXA administration (16 out of 232 patients, 7.51 (0.46,14.56), p=0.04), but showed no difference in FFP or platelet administration.
Conclusion: Early TXA use was not associated with improved outcomes. Late TXA use was associated with increased blood product resuscitation. TXA administration in general was associated with improved 3 hour mortality. This did not translate to an improvement in mortality at 24 hours or 30 days. There was a significant increase in the incidence of ARDS, AKI, and MOF in patients who received TXA but this analysis is limited by the differences in the 2 populations despite attempts to control for them
23/12/2017
Cricothyrotomie sans repères de surface
| Tags : airway
Le glycoalyx: Une cible thérapeutique
-----------------------------------
La correction précoce de la coagulopathie traumatique est un des objectifs fondamentaux de la prise en charge du traumatisé sévère et en particulier des blessés de guerre. L'emploi de plasma lyophilisé / fibrinogène / fractions coagulantes concentrées et la transfusion de sang frais se fait selon des stratégies diverses visant à compenser les déficits observés (1) . La restauration d'une perméabilité capillaire est également une voie possible. On peut considérer que l'efficacité du plasma est en +/- grande partie liée à sa capacité à restaurer le glycocalyx endothélial (2). Le travail présenté est en faveur de l'emploi, à l'instar de l'acide tranexaminique pour la fibrinolyse, d'ajuvants pharmacologiques aux solutés de remplissage pour limiter l'atteinte du glycoclayx.
Allez sur le forum coagulopathie/transfusion
Mieux comprende le concept de perméabilité capillaire
-----------------------------------
INTRODUCTION:
There is interest in the small-volume therapeutic use of adjunct drugs for treating hemorrhagic shock (HS). However, critical information is only partially available on mechanisms of action of promising compounds such as adenosine-lidocaine-magnesium (ALM), beta-hydroxybutyrate plus melatonin (BHB/M), and poloxamer 188 (P-188). Therefore, we tested the hypothesis that these adjuncts would reverse HS-induced damage to microvascular endothelial glycocalyx and hemodynamics.
METHODS:
After baseline, 40% of total blood volume was removed from 44 anesthetized Sprague-Dawley male rats. One hour after hemorrhage, animals were resuscitated using ALM, BHB/M, or P-188 followed by lactated Ringer's (LR, 15 mL/kg). Control animals were not treated (SHAM) or received LR alone. Sampled blood was used to quantify shed syndecan-1 in plasma; multiple systemic physiological parameters were recorded. In vivo glycocalyx thickness, microvascular permeability, and microhemodynamics were evaluated in >200 cremaster venules using intravital videomicroscopy.
RESULTS:
Compared with baseline, resuscitation using adjuncts was associated with glycocalyx restoration of 97 ± 9% (ALM), 75 ± 8% (BHB/M), and 85 ± 5% (P-188): significantly higher than LR-only (56 ± 4%). Significantly better permeability, similar to SHAM values, was measured after ALM and P-188, and low plasma syndecan-1 levels were measured after resuscitation with all adjuncts. Microhemodynamic changes were relatively small while systemic parameters such as mean arterial pressure and lactate improved but remained below or above the baseline, respectively, as expected from this hypotensive resuscitation model.
CONCLUSION:
The drugs ALM, BHB/M, and P-188 provide beneficial effects as adjuncts to hypotensive resuscitation in this HS model by mechanisms involving changes at the microvascular level including the glycocalyx.
| Tags : coagulopathie, transfusion
21/12/2017
Préparateur sportif et trauma sévère: Une évidence !
Cocks M et Al. J Surg Educ. 2014 Mar-Apr;71(2):262-9
BACKGROUND:
Mental practice has been successfully applied in professional sports for skills acquisition and performance enhancement. The goals of this review are to describe the literature on mental practice within sport psychology and surgery and to explore how the specific principles of mental practice can be applied to the improvement of surgical performance-both in novice and expert surgeons.
METHOD:
The authors reviewed the sports psychology, education, and surgery literatures through Medline, PubMed, PsycINFO, and Embase.
RESULTS:
In sports, mental practice is a valuable tool for optimizing existing motor skill sets once core competencies have been mastered. These techniques have been shown to be more advantageous when used by elite athletes. Within surgery, mental practice studies have focused on skill acquisition among novices with little study of how expert surgeons use it to optimize surgical preparation.
CONCLUSIONS:
We propose that performance optimization and skills acquisition should be viewed as 2 separate domains of mentalpractice. Further understanding of this phenomenon has implications for changing how we teach and train not only novice surgeons but also how experienced surgeons continue to maintain their skills, acquire new ones, and excel in surgery.
| Tags : top
Pour du sang à l'avant: Le drone !
L'emploi du sang se heurte à de nombreux problèmes. Le recours à des drones n'est pas une utopie. Tout ceci est très étudié par les pays dont le maillage hospitaliers et les infrastructures sont peu développés.
Les drones font partie du futur (1) et leur autonomie est un atout précieux pour qu’ils puissent devenir un moyen de porter rapidement secours aux individus. Ainsi, les aéronefs sont dès à présent envisagés comme une alternative pour livrer des équipements médicaux dans des lieux qui pourraient s’avérer plus compliqués à traverser pour l’être humain (2)
« Les drones pourraient être le meilleur système de livraison des équipements médicaux du vingt-et-unième siècle "
Diverses technologies de drone peuvent être employées. Un modèle tanzanien parait bien opérant (3) et commence à être utilisé en routine au rwanda pour la délivrance de sang (4) . Certains ont démontré leur capacité à oeuvrer dans un rayon de 260 km (5, lire cette publication US).
| Tags : drone
17/12/2017
Réfllexions sur la balance Airway/complications
Strategies for the prevention of airway complications - a narrative review.
Despite being infrequent, complications of airway management remain an important contributor to morbidity and mortality during anaesthesia and care of the critically ill. Developments in the last three decades have made anaesthesia safer, and this has been mirrored in the equipment and techniques available for airway management. Modern technology including novel oxygenation modalities, widespread availability of capnography, second-generation supraglottic airway devices and videolaryngoscopy provide the tools to make airway management safer still. However, technology will only take safety so far, and non-technical aspects of airway management are critically important for communication and decision making during airway crises, acknowledging a 'cannot intubate, cannot oxygenate' situation and transitioning to emergency front of neck airway. Randomised controlled trials provide little useful information about safety in this setting, and data from registries and databases are likely to be of more value. This narrative review focuses on recent evidence in this area.
09/12/2017
Vladimir Oppel: Précurseur des trauma System
03/12/2017
Garrot: Pas si simple sans formation
The Tourniquet Gap: A Pilot Study of the Intuitive Placement of Three Tourniquet Types by Laypersons
Ross EM et Al. http://dx.doi.org/10.1016/j.jemermed.2017.09.011
--------------------------
La pose de garrot par l'intervenant le plus proche d'une victime blessé semble être une évidence. Pourtant ce travail met en évidence un taux relativement important d'échec. Ceci milite pour la conduite de campagne de formation avant toute mise à disposition de garrot industriel
--------------------------
Objectives
The objective of this pilot study was to determine which tourniquet type was the most intuitive for a layperson to apply correctly.
Methods
This project is a randomized study derived from a “Stop the Bleed” education initiative conducted between September 2016 and March 2017. Novice tourniquet users were randomized to apply one of three commercially available tourniquets (Combat Action Tourniquet [CAT; North American Rescue, LLC, Greer, SC], Ratcheting Medical Tourniquet [RMT; m2 Inc., Winooski, VT], or Stretch Wrap and Tuck Tourniquet [SWAT-T; TEMS Solutions, LLC, Salida, CO]) in a controlled setting. Individuals with formal medical certification, prior military service, or prior training with tourniquets were excluded. The primary outcome of this study was successful tourniquet placement.
Results
Of 236 possible participants, 198 met the eligibility criteria. Demographics were similar across groups. The rates of successful tourniquet application for the CAT, RMT, and SWAT-T were 16.9%, 23.4%, and 10.6%, respectively ( p = 0.149). The most common causes of application failure were: inadequate tightness (74.1%), improper placement technique (44.4%), and incorrect positioning (16.7%).
Conclusion
Our pilot study on the intuitive nature of applying commercially available tourniquets found unacceptably high rates of failure. Large-scale community education efforts and manufacturer improvements of tourniquet usability by the lay public must be made before the widespread dissemination of tourniquets will have a significant public health effect.
| Tags : tourniquet
02/12/2017
Fibrinogène en PREMIER pour le trauma
BACKGROUND:
Effective treatment of trauma-induced coagulopathy is important; however, the optimal therapy is still not known. We aimed to compare the efficacy of first-line therapy using fresh frozen plasma (FFP) or coagulation factor concentrates (CFC) for the reversal of trauma-induced coagulopathy, the arising transfusion requirements, and consequently the development of multiple organ failure.
METHODS:
This single-centre, parallel-group, open-label, randomised trial was done at the Level 1 Trauma Center in Innsbruck Medical University Hospital (Innsbruck, Austria). Patients with trauma aged 18-80 years, with an Injury Severity Score (ISS) greater than 15, bleeding signs, and plasmatic coagulopathy identified by abnormal fibrin polymerisation or prolonged coagulation time using rotational thromboelastometry (ROTEM) were eligible. Patients with injuries that were judged incompatible with survival, cardiopulmonary resuscitation on the scene, isolated brain injury, burn injury, avalanche injury, or prehospital coagulation therapy other than tranexamic acid were excluded. We used a computer-generated randomisation list, stratification for brain injury and ISS, and closed opaque envelopes to randomly allocate patients to treatment with FFP (15 mL/kg of bodyweight) or CFC (primarily fibrinogen concentrate [50 mg/kg of bodyweight]). Bleeding management began immediately after randomisation and continued until 24 h after admission to the intensive care unit. The primary clinical endpoint was multiple organ failure in the modified intention-to-treat population (excluding patients who discontinued treatment). Reversal of coagulopathy and need for massive transfusions were important secondary efficacy endpoints that were the reason for deciding the continuation or termination of the trial. This trial is registered with ClinicalTrials.gov, number NCT01545635.
FINDINGS:
Between March 3, 2012, and Feb 20, 2016, 100 out of 292 screened patients were included and randomly allocated to FFP (n=48) and CFC (n=52). Six patients (four in the FFP group and two in the CFC group) discontinued treatment because of overlooked exclusion criteria or a major protocol deviation with loss of follow-up. 44 patients in the FFP group and 50 patients in the CFC group were included in the final interim analysis.
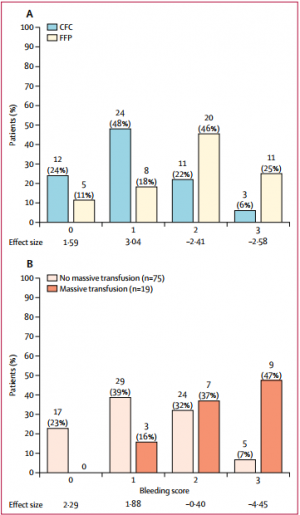

The study was terminated early for futility and safety reasons because of the high proportion of patients in the FFP group who required rescue therapy compared with those in the CFC group (23 [52%] in the FFP group vs two [4%] in the CFC group; odds ratio [OR] 25·34 [95% CI 5·47-240·03], p<0·0001) and increased needed for massive transfusion (13 [30%] in the FFP group vs six [12%] in the CFC group; OR 3·04 [0·95-10·87], p=0·042) in the FFP group. Multiple organ failure occurred in 29 (66%) patients in the FFP group and in 25 (50%) patients in the CFC group (OR 1·92 [95% CI 0·78-4·86], p=0·15).
INTERPRETATION:
Our results underline the importance of early and effective fibrinogen supplementation for severe clotting failure in multiple trauma. The available sample size in our study appears sufficient to make some conclusions that first-line CFC is superior to FFP.
01/12/2017
Transfusion à l'avant: Surtout Plyo, et le sang ?
Early transfusion on battlefield before admission to role 2: A preliminary observational study during “Barkhane” operation in Sahel
Vitalys V. et Al. https://doi.org/10.1016/j.injury.2017.11.029
---------------------------------------
Ce document rapporte essentiellement l'emploi de PLyo chez des blessés de guerre avant leur prise en charge en role 2. Beaucoup est écrit sur la faisabilité d'une telle pratique. On rappelle que l'emploi du plasma lyophilisé n'est pas une nouveauté y compris en milieu précaire (1). Le plasma lyophilisé était d'emploi très courant dans les années 70 et début 80, à un tel point qu'il était pratiquement utilisé comme soluté de remplissage chez le traumatisé routier grave. Il s'agit donc d'une redécouverte et on n'est pas surpris que ceci puisse se retrouver 30 ans après avec un produit notoirement sécurisé (2).
Il est dommage que l'article ne détaille pas plus cet emploi au niveau des role 1 qui est le lieu de début de transfusion pour 5 des blessés transfusés sur 7, ce qui n'est pas vraiment mis en avant dans ce travail. La reconstitution du Plyo est simple, mais probablement moins aisée dans une voilure tournante que dans un Casanurse ou au sol. Cet article met également en avant l'absence de transfusion de sang total, ce qui est étonnant pour une pratique rentrée dans les moeurs chez nos collègues US et UK. Enfin on retrouve l'emploi de fibrinogène, dont l'apport suffisant ne peut être assuré par le PLyo seul, et que certains proposent en première ligne de fractions coagulantes (3). Chose intéressante deux échecs de reconstitution du Plyo ont été observées.
Un article très intéressant, dont plusieurs auteurs sont en charge du développement du PLyo, avec dans la partie discussion un bon rappel des problématiques qui se posent dans de telles circonstances. Il est dommage que le regroupement des lésions du bassin avec l'atteinte des membres ait été fait car les problématiques de contrôle des hémorragies sont différentes. De même la description des lésions observées dans le groupe transfusé (qui ne sont pas tous porteurs d'un garrot), et l'analyse spécifique du groupe présentant une hémorragie encore active aurait été méritées.
---------------------------------------
Introduction
Haemorrage is the leading cause of death after combat related injuries and bleeding management is the cornerstone of management of these casualties. French armed forces are deployed in Barkhane operatio n in the Sahel-Saharan Strip who represents an immense area. Since this constraint implies evacuation times beyond doctrinal timelines, an institutional decision has been made to deploy blood products on the battlefield and transfuse casualties before role 2 admission if indicated. The purpose of this study was to evaluate the transfusion practices on battlefield during the first year following the implementation of this policy.
Materials and methods
prospective collection of data about combat related casualties categorized alpha evacuated to a role 2. Battlefield transfusion was defined as any transfusion of blood product (red blood cells, plasma, whole blood) performed by role 1 or Medevac team before admission at a role 2. Patients’ characteristics, battlefield transfusions’ characteristics and complications were analysed.
Results
During the one year study, a total of 29 alpha casualties were included during the period study. Twenty-eight could be analysed, 7/28 (25%) being transfused on battlefield, representing a total of 22 transfusion episodes. The most frequently blood product transfused was French lyophilized plasma (FLYP). Most of transfusion episodes occurred during medevac. Compared to non-battlefield transfused casualties, battlefield transfused casualties suffered more wounded anatomical regions (median number of 3 versus 2, p = 0.04), had a higher injury severity score (median ISS of 45 versus 25, p = 0,01) and were more often transfused at role 2, received more plasma units and whole blood units. There was no difference in evacuation time to role 2 between patients transfused on battlefield and non-transfused patients. There was no complication related to battlefield transfusions. Blood products transfusion onset on battlefield ranged from 75 min to 192 min after injury.
Conclusion
Battlefield transfusion for combat-related casualties is a logistical challenge. Our study showed that such a program is feasible even in an extended area as Sahel-Saharan Strip operation theatre and reduces time to first blood product transfusion for alpha casualties. FLYP is the first line blood product on the battlefield
| Tags : transfusion

