22/01/2017
Crico avec un opinel ? Possible
Bystander cricothyroidotomy with household devices - A fresh cadaveric feasibility study.
In various motion pictures, medical TV shows and internet chatrooms, non-medical devices were presented as tools for life-saving cricothyroidotomies. However, there is uncertainty about whether it is possible for a bystander to perform a cricothyroidotomy and maintain gas exchange using improvised household items. This study examines the ability of bystanders to carry out an emergency cricothyroidotomy in fresh human cadavers using only a pocket knife and a ballpoint pen.
MATERIALS AND METHODS:
Two commonly available pens and five different pocket knives were used. Ten participants with no or only basic anatomical knowledge had to choose one of the pens and one of the knives and were asked to perform a cricothyroidotomy as quickly as possible after a short introduction. Primary successful outcome was a correct placement of the pen barrel and was determined by the thoracic lifting in a mouth-to-pen resuscitation.
RESULTS:
Eight (80%) participants performed a successful approach to the upper airway with a thoracic lifting at the end. Five participants performed a cricothyroidotomy and three performed an unintentional tracheotomy. Injuries to muscles and cartilage were common, but no major vascular damage was seen in the post-procedural autopsy. However, mean time in the successful group was 243s.
CONCLUSION:
In this cadaveric model, bystanders with variable medical knowledge were able to establish an emergency cricothyroidotomy in 80% of the cases only using a pocketknife and a ballpoint pen. No major complications (particularly injuries of arterial blood vessels or the oesophagus) occurred. Although a pocket knife and ballpoint pen cricothyroidotomy seem a very extreme procedure for a bystander, the results of our study suggest that it is a feasible option in an extreme scenario. For a better outcome, the anatomical landmarks of the neck and the incision techniques should be taught in emergency courses.
| Tags : airway
Du sang qui descend du ciel
Nous ne sommes pas les seuls à avoir à faire face au contexte d'isolement. Il est particulièrement intéressant de regarder comment ces problèmes sont abordés par les pays en voie de construction. L'exemple rwandais devrait nous interpeller. Le recours à des drones de livraison en contexte militaire n'est pas une utopie car ce mode de ravitaillement a été utilisé en afghanistan.
| Tags : transfusion
21/01/2017
Coagulopathie: Fibrinogène avant PLyo, mais les 2 et + tôt ?
Despite the early uses of tourniquets and haemostatic dressings, blood loss still accounts for the vast majority of preventable deaths on the battlefield. Over the last few years, progress has been made in the management of such injuries, especially with the use of damage control resuscitation concepts. The early application of these procedures, on the field, may constitute the best opportunity to improve survival from combat injury during remote operations.
DATA SOURCES:
Currently available literature relating to trauma-induced coagulopathy treatment and far-forward transfusion was identified by searches of electronic databases. The level of evidence and methodology of the research were reviewed for each article. The appropriateness for field utilisation of each medication was then discussed to take into account the characteristics of remote military operations.
CONCLUSIONS:
In tactical situations, in association with haemostatic procedures (tourniquet, suture, etc), tranexamic acid should be the first medication used according to the current guidelines. The use of fibrinogen concentrate should also be considered for patients in haemorrhagic shock, especially if point-of-care (POC) testing of haemostasis or shock severity is available. If POC evaluation is not available, it seems reasonable to still administer this treatment after clinical assessment, particularly if the evacuation is delayed. In this situation, lyophilised plasma may also be given as a resuscitation fluid while respecting permissive hypotension. Whole blood transfusion in the field deserves special attention.
In addition to the aforementioned treatments, if the field care is prolonged, whole blood transfusion must be considered if it does not delay the evacuation
| Tags : coagulopathie, transfusion
Gelures graves: Plus tôt la thrombolyse
Severe frostbite is associated with high levels of morbidity through loss of digits or limbs. The aim of this study was to examine the salvage rate following severe frostbite injury. Frostbite patients from 2006 to 2014 were identified in the prospectively maintained database at a single urban burn and trauma center. Patients with imaging demonstrating a lack of blood flow in limbs/digits were included in the analysis (N = 73). The Hennepin Frostbite Score was used to quantify frostbite injury and salvage. This score provides a single value to assess each individual patient's salvage rate. The majority of patients with perfusion deficits were male (80%) with an average age of 42 years (range 11-83 years). Patients requiring amputation tended to be older (P = .002), have more tissue impacted by frostbite (P < .001), and experienced a longer time from rewarming to thrombolytic therapy (P = .001). A majority of patients (62%) received thrombolytic treatment. The percentage of patients requiring amputation was lower and the salvage rate was higher in patients treated with thrombolytics; however, the differences failed to reach statistical significance (P = .092 and P = .061, respectively). The rate of salvage decreases as the time from rewarming to thrombolytic therapy increases. Regression analysis demonstrates an additional 26.8% salvage loss with each hour of delayed treatment (P = .006). When the amount of tissue at risk for amputation is included in the model, each hour delay in thrombolytic treatment results in a 28.1% decrease in salvage (P = .011). This study demonstrates a significant decrease in limb/digit salvage with each hour of delayed administration of thrombolytics in patients with severe frostbite
| Tags : gelures
18/01/2017
MEDEVAC de la BSS: En gros que fait on ?
Forward medevac during Serval and Barkhane operations in Sahel: A registry study.
Carfantan C, et Al. Injury. 2017 Jan;48(1):58-63.
-----------------------------------
Une activité particulièrement sensible dont la lecture permet de comprendre toute la complexité de la prise en charge de nos soldats dans un contexte d'élongation majeure. On comprend également tous les enjeux de positionnement d'équipes sanitaires ayant la maîtrise de certaines pratiques avancées de réanimation préhospitalière.
-----------------------------------
INTRODUCTION:
The French army has been deployed in Mali since January 2013 with the Serval Operation and since July 2014 in the Sahel-Saharan Strip (SSS) with the Barkhane Operation where the distances (up to 1100km) can be very long. French Military Medical Service deploys an inclusive chain from the point of injury (POI) to hospital in France. A patient evacuation coordination cell (PECC) has been deployed since February 2013 to organise forward medical evacuation (MEDEVAC) in the area between the POI and three forward surgical units. The purpose of this work was to study the medical evacuation length and duration between the call for Medevac location accidents and forward surgical units (role 2) throughout the five million square kilometers French joint operation area.
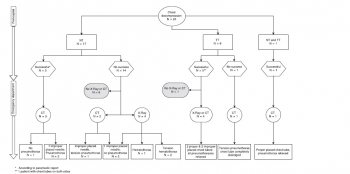
MATERIALS AND METHODS:
Our retrospective study concerns the French patients evacuated by MEDEVAC from February 2013 to July 2016. The PECC register was analysed for patients' characteristics, NATO categorisation of gravity (Alpha, Bravo or Charlie who must be respectively at hospital facility within 90min, 4h or 24h), medical motive for MEDEVAC and the time line of each MEDEVAC (from operational commander request to entrance in role 2).
RESULTS:
A total of 1273 French military were evacuated from February to 2013 to July 2016; 533 forward MEDEVAC were analysed. 12,4% were Alpha, 28,1% Bravo, 59,5% Charlie. War-related injury represented 18,2% of MEDEVAC. The median time for Alpha category MEDEVAC patients was 145min [100-251], for Bravo category patients 205min [125-273] and 310min [156-669] for Charlie. The median distance from the point of injury to role 2 was 126km [90-285] for Alpha patients, 290km [120-455] km for Bravo and 290km [105-455] for Charlie.
CONCLUSIONS:
Patient evacuation in such a large area is a logistic and human challenge. Despite this, Bravo and Charlie patients were evacuated in NATO recommended time frame. However, due to distance, Alpha patients time frame was longer than this recommended by NATO organisation. That's where French doctrine with forward medical teams embedded in the platoons is relevant to mitigate this distance and time frame challenge.
| Tags : evasan
Décompression pleurale: Dur, dur...
Failure rate of prehospital chest decompression after severe thoracic trauma.
Kaserer A. et Al Am J Emerg Med. 2016 Nov 30. pii: S0735-6757(16)30892-0
-----------------------------------------------------
Une publication qui émane de nos collègues suisses et qui interpelle quelque peu. La décompression thoracique apparat être un geste dont la maîtrise est largement insuffisante y compris quand elle est réalisée au sein d'un système mature. Une raison de plus pour s'intéresser à la maîtrise effective des gestes censés participer à la mise en condition de survie des blessés. On rappelle l'intérêt de la thoracostomie au doigt (1), doigt dont la longueur est en général suffisante pour entrer dans un thorax.
-----------------------------------------------------
INTRODUCTION:
Chest decompression can be performed by different techniques, like needle thoracocentesis (NT), lateral thoracostomy (LT), or tube thoracostomy (TT). The aim of this study was to report the incidence of prehospital chest decompression and to analyse the effectiveness of these techniques.
MATERIAL AND METHODS:
In this retrospective case series study, all medical records of adult trauma patients undergoing prehospital chest decompression and admitted to the resuscitation area of a level-1 trauma center between 2009 and 2015 were reviewed and analysed. Only descriptive statistics were applied.
RESULTS:
In a 6-year period 24 of 2261 (1.1%) trauma patients had prehospital chest decompression. Seventeen patients had NT, six patients TT, one patient NT as well as TT, and no patients had LT. Prehospital successful release of a tension pneumothorax was reported by the paramedics in 83% (5/6) with TT, whereas NT was effective in 18% only (3/17). In five CT scans all thoracocentesis needles were either removed or extrapleural, one patient had a tension pneumothorax, and two patients had no pneumothorax. No NT or TT related complications were reported during hospitalization.
CONCLUSION:
Prehospital NT or TT is infrequently attempted in trauma patients. Especially NT is associated with a high failure rate of more than 80%, potentially due to an inadequate ratio between chest wall thickness and catheter length as previously published as well as a possible different pathophysiological cause of respiratory distress. Therefore, TT may be considered already in the prehospital setting to retain sufficient pleural decompression upon admission.
| Tags : pneumothorax
15/01/2017
ISR: Plutôt kétamine ?
Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia.
Lyon RM et Al. Crit Care. 2015 Apr 1;19:134
-------------------------------------------
Faut-il utiliser la kétamine ou l'étomidate ? Le travail présenté milite pour l'emploi de la kétamine, mais ceci reste controversé (voir également ici)). C'est aussi le choix présenté dans la procédure du sauvetage au combat, du fait de la polyvalence d'emploi de la kétamine tant dans ses indications que de ses voies d'administration. On rappelle quand même que si l'ISR facilite grandement les conditions de l'intubation oro-trachéale en médecine préhospitalière métropolitaine, nos conditions spécifiques d'exercice ne correspondent pas à cette dernière. Avant de réaliser une telle induction, encore faut-il être valider l'indication de l'intubation au milieu de nulle part. Par ailleurs la réalisation de ce geste sous anesthésie locale doit également être envisagée. Ceci est conforme aux recommandations sur le sujet.
-------------------------------------------
INTRODUCTION:
Rapid Sequence Induction of anaesthesia (RSI) is the recommended method to facilitate emergency tracheal intubation in trauma patients. In emergency situations, a simple and standardised RSI protocol may improve the safety and effectiveness of the procedure. A crucial component of developing a standardised protocol is the selection of induction agents. The aim of this study is to compare the safety and effectiveness of a traditional RSI protocol using etomidate and suxamethonium with a modified RSI protocol using fentanyl, ketamine and rocuronium.
METHODS:
We performed a comparative cohort study of major trauma patients undergoing pre-hospital RSI by a physician-led Helicopter Emergency Medical Service. Group 1 underwent RSI using etomidate and suxamethonium and Group 2 underwent RSI using fentanyl, ketamine and rocuronium. Apart from the induction agents, the RSI protocol was identical in both groups. Outcomes measured included laryngoscopy view, intubation success, haemodynamic response to laryngoscopy and tracheal intubation, and mortality.
RESULTS:
Compared to Group 1 (n = 116), Group 2 RSI (n = 145) produced significantly better laryngoscopy views (p = 0.013) and resulted in significantly higher first-pass intubation success (95% versus 100%; p = 0.007). A hypertensive response to laryngoscopy and tracheal intubation was less frequent following Group 2 RSI (79% versus 37%; p < 0.0001). A hypotensive response was uncommon in both groups (1% versus 6%; p = 0.05). Only one patient in each group developed true hypotension (SBP < 90 mmHg) on induction.
CONCLUSIONS:
In a comparative, cohort study, pre-hospital RSI using fentanyl, ketamine and rocuronium produced superior intubating conditions and a more favourable haemodynamic response to laryngoscopy and tracheal intubation. An RSI protocol using fixed ratios of these agents delivers effective pre-hospital trauma anaesthesia.
08/01/2017
Albumine: Bon pour la coagulopathie ?
Does small-volume resuscitation with crystalloids or colloids influence hemostasis and survival of rabbits subjected to lethal uncontrolled hemorrhage?
BACKGROUND:
Prehospital, small-volume resuscitation of combat casualties with a synthetic colloid (6% hydroxyethyl starch [HES] 670/0.75) has been recommended when blood or blood components are unavailable. We studied hemostatic effects of a newer synthetic colloid (6% HES, 130/0.4) compared with either a natural colloid (albumin) or to crystalloids in an uncontrolled hemorrhage model.
METHODS:
Spontaneously breathing New Zealand white rabbits (3.4 ± 0.1 kg) were anesthetized, instrumented, and subjected to a splenic injury with uncontrolled bleeding. Fifteen minutes after injury, rabbits were in shock (mean arterial pressure [MAP] = 26 ± 1.3 mm Hg, and received colloids (6% HES, 130/0.4 or 5% albumin at 15 mL/kg), or crystalloids (normal saline at 30 mL/kg or 5% hypertonic saline at 7.5 mL/kg) for resuscitation in two intravenous bolus injections (15 minutes apart) to raise their MAP to 65 mm Hg, n = 9/group. Animals were monitored for 2.5 hours or until death, and blood losses were measured. Blood samples were analyzed for arterial blood gas, complete blood count, and coagulation measures.
RESULTS:
There were no differences among groups in baseline measures and initial hemorrhage volume (11.9 ± 0.6 mL/kg) at 15 minutes postinjury. Twenty minutes after fluid resuscitation (1 hour postinjury), MAP was higher, shock indices were lower, and blood pH was higher in colloids versus crystalloids groups (p < 0.05). Administration of 6% HES 130/0.4 colloid produced the largest hemodilution (54% decrease in hematocrit, p < 0.05 vs. hypertonic saline). Activated partial thromboplastin time increased approximately 35% above baseline in all groups except in 6% HES 130/0.4 group in which it doubled. Clot strength was reduced (15%) only in the 6% HES 130/0.4 group. 6% HES 130/0.4 resuscitation produced the largest blood loss and 33% survival rate that was not different than the crystalloid groups. Albumin produced the best hemostatic and survival outcomes (78%).
CONCLUSION:
Small-volume resuscitation with crystalloids appeared inadequate to treat hypovolemic shock and prevent death. 6% HES 130/0.4 was effective hemodynamically but detrimental to hemostasis. Albumin produced the best outcomes consistent with our previous observations. Further studies are needed to prove benefit of albumin solution as a possible resuscitation fluid for treating combat casualties at the point of injury.
Synopsis of the updated European trauma guideline
Management of trauma-induced coagulopathy (TIC): a synopsis of the updated European trauma guideline
Maegele M. J Res Hosp 2016;1:27
Uncontrolled hemorrhage and trauma-induced coagulopathy (TIC) are still the major causes for preventable death after trauma .
Approximately one out of four severely injured trauma patients admitted to the hospital is bleeding with variable degrees of laboratory coagulopathy. Meanwhile, TIC is recognized as an own clinical entity with substantial impact on outcome and survival after trauma. There has been speculation about the potential mechanisms underlying TIC but much of the data continues to be rather correlative than causative with robust links still lacking.
02/01/2017
Plyo au point de blessure: Stratégique ?
Freeze-dried plasma at the point of injury: from concept to doctrine.
While early plasma transfusion for the treatment of patients with ongoing major hemorrhage is widely accepted as part of the standard of care in the hospital setting, logistic constraints have limited its use in the out-of-hospital setting. Freeze-dried plasma (FDP), which can be stored at ambient temperatures, enables early treatment in the out-of-hospital setting. Point-of-injury plasma transfusion entails several significant advantages over currently used resuscitation fluids, including the avoidance of dilutional coagulopathy, by minimizing the need for crystalloid infusion, beneficial effects on endothelial function, physiological pH level, and better maintenance of intravascular volume compared with crystalloid-based solutions. The Israel Defense Forces Medical Corps policy is that plasma is the resuscitation fluid of choice for selected, severely wounded patients and has thus included FDP as part of its armamentarium for use at the point of injury by advanced life savers, across the entire military. We describe the clinical rationale behind the use of FDP at the point-of-injury, the drafting of the administration protocol now being used by Israel Defense Forces advanced life support providers, the process of procurement and distribution, and preliminary data describing the first casualties treated with FDP at the point of injury. It is our hope that others will be able to learn from our experience, thus improving trauma casualty care around the world.
Plyo: En intraosseux aussi
Pre-hospital intra-osseous freeze dried plasma transfusion: a case report
Rottenstreich et al. Disaster and Military Medicine 2015, 1:8
Background: Hemorrhage and coagulopathy are among the leading causes of death in combat and are considered the leading causes of preventable deaths. Plasma, in the form of Fresh Frozen Plasma (FFP) is considered a key component in the Damage Control Resuscitation performed within hospitals. Freeze-Dried Plasma (FDP) can be stored at room temperature and therefore is potentially useful in pre-hospital conditions. Our case report join to few cases where FDP was administered at the point of injury. It is also unique as it describes an intra- osseous administration given to pediatric patient.
Case report: M.S. otherwise healthy 13 year old girl was injured due to gunshots and grenade blast. On the first triage by the IDF medical teams she suffered from: Severe hemorrhagic shock, (Blood pressure could not be measured, Heart rate 163), superficial wounds to her face, (forehead and Rt. Eye), gunshot wounds with active bleeding from her Lt. Arm and her RT. Knee (Mangled Extremity Severity Score (MESS) 8) and open fractures of left elbow and right thigh. A peripheral intravenous catheter was established and 1 g tranexamic acid in 500 ml of Hartman fluid were administered. Due to difficulties in establishing a functioning intra-venous line, an intra-osseous catheter was established and one unit of FDP (250 ml) was given in the field. She was transferred by a military medical team to a regional civilian hospital for further treatment. Upon arrival to the hospital her blood pressure and heart rate were significantly improved. After three weeks of hospitalization M.S. was discharged and she was returned to her homeland.
Conclusion: We have described the successful use of FDP for pre hospital resuscitation of a 13 year old girl suffering from severe hemorrhagic shock as a result of gunshots and grenade blast. This case report demonstrates that intra-osseous FDP administration for as part pre hospital resuscitation of children has a favorable outcome.
| Tags : intraosseux
Coagulopathy/ Eléments de compréhension
Advances in the understanding of trauma-induced coagulopathy
Chang R. et al Blood. 2016;128(8):1043-1049
Ten percent of deaths worldwide are due to trauma, and it is the third most common cause of death in the United States. Despite a profound upregulation in procoagulant mechanisms, one-quarter of trauma patients present with laboratorybased evidence of trauma-induced coagulopathy (TIC), which is associated with poorer outcomes including increased mortality. The most common causes of death after trauma are hemorrhage and traumatic brain injury (TBI). The management of TIC has significant implications in both because many hemorrhagic deaths could be preventable, and TIC is associated with progression of intracranial injury after TBI. This review covers the most recent evidence and advances in our understanding of TIC, including the role of platelet dysfunction, endothelial activation, and fibrinolysis. Trauma induces a plethora of biochemical and physiologic changes, and despite numerous studies reporting differences in coagulation parameters between trauma patients and uninjured controls, it is unclear whether some of these differences may be “normal” after trauma. Comparisons between trauma patients with differing outcomes and use of animal studies have shed some light on this issue, but much of the data continue to be correlative with causative links lacking. In particular, there are little data linking the laboratory-based abnormalities with true clinically evident coagulopathic bleeding. For these reasons, TIC continues to be a significant diagnostic and therapeutic challenge.
| Tags : coagulopathie