19/12/2016
The 2015 Remote Damage Control Resuscitation Symposium
18/12/2016
Coagulopathie traumatique. Données actuelles
Acute traumatic coagulopathy: pathophysiology and resuscitation.
Acute Traumatic Coagulopathy occurs immediately after massive trauma when shock, hypoperfusion, and vascular damage are present. Mechanisms for this acute coagulopathy include activation of protein C, endothelial glycocalyx disruption, depletion of fibrinogen, and platelet dysfunction. Hypothermia and acidaemia amplify the endogenous coagulopathy and often accompany trauma. These multifactorial processes lead to decreased clot strength, autoheparinization, and hyperfibrinolysis. Furthermore, the effects of aggressive crystalloid administration, haemodilution from inappropriate blood product transfusion, and prolonged surgical times may worsen clinical outcomes. We review normal coagulation using the cell-based model of haemostasis and the pathophysiology of acute traumatic coagulopathy. Developed trauma systems reduce mortality, highlighting critical goals for the trauma patient in different phases of care. Once patients reach a trauma hospital, certain triggers reliably indicate when they require massive transfusion and specialized trauma care. These triggers include base deficit, international normalized radio (INR), systolic arterial pressure, haemoglobin concentration, and temperature. Early identification for massive transfusion is critically important, as exsanguination in the first few hours of trauma is a leading cause of death. To combat derangements caused by massive haemorrhage, damage control resuscitation is a technique that addresses each antagonist to normal haemostasis. Components of damage control resuscitation include damage control surgery, permissive hypotension, limited crystalloid administration, haemostatic resuscitation, and correction of hyperfibrinolysis.
Fibrinogène dès que l'Hb baisse ?
Estimation of plasma fibrinogen levels based on hemoglobin, base excess and Injury Severity Score upon emergency room admission
----------------------
Il existe un grand débat sur la manière de prendre en charge la coagulopathie traumatique des traumatisés ballistiques en contexte d'isolement (1,2).Un des sujets porte sur la manière de corriger l'hypofibrinogénémie soit par apport de Plasma soit par apport de concentrés de fibrinogène (3, 4). Le consensus européen valide les deux approches (5). Mais dans notre contexte d'intervention quels critères d'administration appliquer ? L'hémoglobinémie à la prise en charge permettrait d'indiquer l'apport de fibrinogène, en gros dès qu'elle est abaissée et surtout <10g/dl. C'est ce que peut laisser penser cette étude. Des moyens simples utilisables en contexte d'isolement permettent donc de stratifier les indications de fibrinogène apporté soit sous forme concentré soit sous forme de plasma (6).
----------------------
INTRODUCTION:
Fibrinogen plays a key role in hemostasis and is the first coagulation factor to reach critical levels in massively bleeding trauma patients. Consequently, rapid estimation of plasma fibrinogen (FIB) is essential upon emergency room (ER) admission, but is not part of routine coagulation monitoring in many centers. We investigated the predictive ability of the laboratory parameters hemoglobin (Hb) and base excess (BE) upon admission, as well as the Injury Severity Score (ISS), to estimate FIB in major trauma patients.
METHODS:
In this retrospective study, major trauma patients (ISS ≥16) with documented FIB analysis upon ER admission were eligible for inclusion. FIB was correlated with Hb, BE and ISS, alone and in combination, using regression analysis.
RESULTS:
A total of 675 patients were enrolled (median ISS 27). FIB upon admission correlated strongly with Hb, BE and ISS.
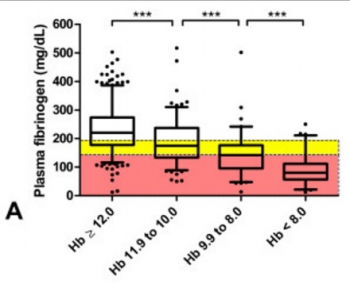
Multiple regression analysis showed that Hb and BE together predicted FIB (adjusted R2 = 0.46; loge(FIB) = 3.567 + 0.223.Hb - 0.007.Hb2 + 0.044.BE), and predictive strength increased when ISS was included (adjusted R2 = 0.51; loge(FIB) = 4.188 + 0.243.Hb - 0.008.Hb2 + 0.036.BE - 0.031.ISS + 0.0003.ISS2). Of all major trauma patients admitted with Hb <12 g/dL, 74% had low (<200 mg/dL) FIB and 54% had critical (<150 mg/dL) FIB. Of patients admitted with Hb <10 g/dL, 89% had low FIB and 73% had critical FIB. These values increased to 93% and 89%, respectively, among patients with an admission Hb <8 g/dL. Sixty-six percent of patients with only a weakly negative BE (<-2 mmol/L) showed low FIB. Of patients with BE <-6 mmol/L upon admission, 81% had low FIB and 63% had critical FIB. The corresponding values for BE <-10 mmol/L were 89% and 78%, respectively.
CONCLUSIONS:
Upon ER admission, FIB of major trauma patients shows strong correlation with rapidly obtainable, routine laboratory parameters such as Hb and BE. These two parameters might provide an insightful and rapid tool to identify major trauma patients at risk of acquired hypofibrinogenemia. Early calculation of ISS could further increase the ability to predict FIB in these patients. We propose that FIB can be estimated during the initial phase of trauma care based on bedside tests.
15/12/2016
Sang total: Pas que chaud, de banque aussi
Coagulation function of stored whole blood is preserved for 14 days in austere conditions: A ROTEM feasibility study during a Norwegian antipiracy mission and comparison to equal ratio reconstituted blood.
BACKGROUND:
Formulation of a medical preparedness plan for treating severely bleeding casualties during naval deployment is a significant challenge because of territory covered during most missions. The aim of this study was to evaluate the concept of "walking blood bank" as a supportable plan for supplying safe blood and blood products.
METHODS:
In 2013, the Royal Norwegian Navy conducted antipiracy operations from a frigate, beginning in the Gulf of Aden and ending in the Indian Ocean. Crews were on 24-hour emergency alert in preparation for an enemy assault on the frigate. Under an approved command protocol, a "walking blood bank," using crew blood donations, was established for use on board and on missions conducted in rigid-hulled inflatable boats, during which freeze-dried plasma and leukoreduced, group O low anti-A/anti-B titer, cold-stored whole blood were stored in Golden Hour Boxes. Data demonstrating the ability to collect, store, and provide whole blood were collected to establish feasibility of implementing a whole blood-focused remote damage-control resuscitation program aboard a naval vessel. In addition, ROTEM data were collected to demonstrate feasibility of performing this analysis on a large naval vessel and to also measure hemostatic efficacy of cold-stored leukoreduced whole blood (CWB) stored during a period of 14 days. ROTEM data on CWB was compared with reconstituted whole blood.
RESULTS:
Drills simulating massive transfusion activation were conducted, in which 2 U of warm fresh whole blood with platelet sparing leukoreduction were produced in 40 minutes, followed by collection of two additional units at 15-minute increments. The ROTEM machine performed well during ship-rolling, as shown by the overlapping calculated and measured mechanical piston movements measured by the ROTEM device. Error messages were recorded in 4 (1.5%) of 267 tests. CWB yielded reproducible ROTEM results demonstrating preserved fibrinogen function and platelet function for at least 3.5 weeks and 2 weeks, respectively. The frequency of ROTEM tests were as follows: EXTEM (n = 88), INTEM (n = 85), FIBTEM (n = 82), and APTEM (n = 12). CWB results were grouped. Compared with Days 0 to 2, EXTEM maximum clot firmness was significantly reduced, beginning on Days 10 to 14; however, results through that date remained within reference ranges and were comparable with the EXTEM maximum clot firmness for the reconstituted whole blood samples containing Day 5 room temperature-stored platelets.
CONCLUSION:
A "walking blood bank" can provide a balanced transfusion product to support damage-control resuscitation/remote damage-control resuscitation aboard a frigate in the absence of conventional blood bank products. ROTEM analysis is feasible to monitor damage-control resuscitation and blood product quality. ROTEM analysis was possible in challenging operational conditions.
| Tags : coagulopathie, transfusion
14/12/2016
Fibrinogène: Moins de décès
Pre-emptive administration of fibrinogen concentrate contributes to improved prognosis in patients with severe trauma
Yamamoto K, et al. Trauma Surg Acute Care Open 2016;1:1–5
---------------------------------------------------------
Bien que cela reste encore discuté, l'apport précoce de fibrinogène améliorerait la survie des traumatisés sévères. Cette publication est du moins en faveur de cette hypothèse.
---------------------------------------------------------
Background
Patients with severe trauma often present with critical coagulopathy, resulting in impaired hemostasis, massive hemorrhage, and a poor survival prognosis. The efficacy of hemostatic resuscitation in correcting coagulopathy and restoring tissue perfusion has not been studied. We assessed a novel approach of pre-emptive administration of fibrinogen concentrate to improve critical coagulopathy in patients with severe trauma.
Methods
We retrospectively compared blood transfusion volumes and survival prognosis between three groups of patients with trauma, with an Injury Severity Score (ISS) ≥26 over three consecutive periods: group A, no administration of fibrinogen concentrate; group B, administration of 3 g of fibrinogen concentrate after evaluation of trauma severity and a plasma fibrinogen level <1.5 g/L; group C, pre-emptive administration of 3 g of fibrinogen concentrate immediately on patient arrival based on prehospital information, including high-severity injury or assessed
need for massive transfusion before measurement of fibrinogen.
Results
∼56% of patients with an ISS ≥26 and transfused with red blood cell concentrates ≥10 units, had hypofibrinogenemia (fibrinogen <1.5 g/L) on arrival. Patients who received fibrinogen concentrate in group C showed significantly higher fibrinogen levels after treatment with this agent than those in group B (2.41 g/L vs 1.88 g/L; p=0.01). Although no significant difference was observed in blood transfusion volumes between the groups, the 30-day survival of patients in group C (all, and those with an ISS ≥26) was significantly better than in group A ( p<0.05). The 48-hour mortality rate in patients with an ISS ≥26 was significantly lower in group C than in group A (8.6% vs 22.9%; p=0.005). Further, among patients with an ISS ≥41, the overall mortality was significantly lower in group C than in group A (20% vs 50%; p=0.02).
Conclusion
Pre-emptive administration of fibrinogen concentrate for patients with trauma with critical coagulopathy may contribute to improved survival.
| Tags : coagulopathie
11/12/2016
Suppression métabolique ?
Inducing metabolic suppression in severe hemorrhagic shock: Pilot study results from the Biochronicity Project.
BACKGROUND:
Suspended animation-like states have been achieved in small animal models, but not in larger species. Inducing metabolic suppression and temporary oxygen independence could enhance survivability of massive injury. Based on prior analyses of key pathways, we hypothesized that phosphoinositol-3-kinase inhibition would produce metabolic suppression without worsening organ injury or systemic physiology.
METHODS:
Twenty swine were studied using LY294002 (LY), a nonselective phosphoinositol-3-kinase inhibitor. Animals were assigned to trauma only (TO, n = 3); dimethyl sulfoxide only (DMSO, n = 4), LY drug only (LYO, n = 3), and drug + trauma (LY + T, n = 10) groups. Both trauma groups underwent laparotomy, 35% hemorrhage, severe ischemia/reperfusion injury, and protocolized resuscitation. Laboratory, physiologic, cytokine, and metabolic cart data were obtained. Histology of key end organs was also compared.
RESULTS:
Baseline values were similar among the groups. Compared with the TO group, the LYO group had reversible decreases in heart rate, mean arterial pressure, cardiac output, oxygen consumption, and carbon dioxide production. Compared with TO, LY + T showed sustained decreases in heart rate (113 vs. 76, p = 0.03), mean arterial pressure (40 vs. 31 mm Hg, p = 0.02), and cardiac output (3.8 vs. 1.9 L/min, p = 0.05) at 6 hours. Metabolic parameters showed profound suppression in the LY + T group. Oxygen consumption in LY + T was lower than both TO (119 vs. 229 mL/min, p = 0.012) and LYO (119 vs. 225 mL/min, p = 0.014) at 6 hours. Similarly, carbon dioxide production was decreased at 6 hours in LY + T when compared with TO (114 vs. 191 mL/min, p = 0.043) and LYO (114 vs. 195 mL/min, p = 0.034) groups. There was no worsening of acidosis (lactate 6.4 vs. 8.3 mmol/L, p = 0.4) or other endpoints. Interleukin 6 (IL-6) showed a significant increase in LY + T when compared with TO at 6 hours (60.5 vs. 2.47, p = 0.043). Tumor necrosis factor α and IL-1β were decreased, and IL-10 increased in TO and LY + T at 6 hours. Markers of liver and kidney injury were no different between TO and LY + T groups at 6 hours.
CONCLUSIONS:
Phosphoinositol-3-kinase inhibition produced metabolic suppression in healthy and injured swine without increasing end-organ injury or systemic physiologic markers and demonstrated prolonged efficacy in injured animals. Further study may lead to targeted therapies to prolong tolerance to hemorrhage and extend the "golden hour" for injured patients.
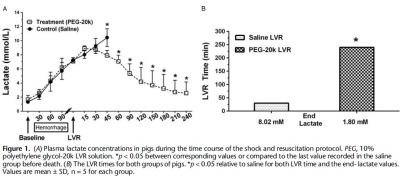
PEG-20k: Le graall du prolongef field care ?
Low-volume resuscitation using polyethylene glycol-20k in a preclinical porcine model of hemorrhagic shock
Plant V. et Al. J Trauma Acute Care Surg. 2016 Dec;81(6):1056-1062.
-----------------------------------
Une nouvelle approche de la prise en compte des lésions induites par l'ischémie tissulaire qui est basée sur l'expérience de l'emploi des solutés utilisés pour conserver les organes en instance de transplantation. Grosso-modo: Remplir les espaces interstitiels par des solutés ne dépendant pas de mécanismes énergétiques. Une explication ici.
-----------------------------------
INTRODUCTION:
Polyethylene glycol-20k (PEG-20k) is highly effective for low-volume resuscitation (LVR) by increasing tolerance to the low-volume state. In our rodent shock model, PEG-20k increased survival and expanded the "golden hour" 16-fold compared to saline. The molecular mechanism is largely attributed to normalizations in cell and tissue fluid shifts after low-flow ischemia resulting in efficient microvascular exchange. The objective of this study was to evaluate PEG-20k as an LVR solution for hemorrhagic shock in a preclinical model.
METHODS:
Anesthetized male Yorkshire pigs (30-40 kg) were hemorrhaged to a mean arterial pressure (MAP) of 35 to 40 mm Hg. Once lactate reached 7 mmol/L, either saline (n = 5) or 10% PEG-20k (n = 5) was rapidly infused at 10% calculated blood volume. The primary outcome was LVR time, defined by the time from LVR administration to the time when lactate again reached 7 mmol/L. Other outcomes measured included MAP, heart rate, cardiac output, mixed venous oxygen saturation, splanchnic blood flow, and hemoglobin.
RESULTS:
Relative to saline, PEG-20k given after controlled hemorrhage increased LVR time by 16-fold, a conservative estimate given that the lactate never rose after LVR in the PEG-20k group. Survival was 80% for PEG-20k LVR compared to 0% for the saline controls (p < 0.05).
Polyethylene glycol-20k also significantly decreased heart rate after hemorrhage and increased cardiac output, MAP, splanchnic flow, and mixed venous oxygen saturation. Falling hemoglobin concentrations suggested sizable hemodilution from fluid shifts into the intravascular compartment.
CONCLUSIONS:
In a preclinical model of controlled hemorrhagic shock, PEG-20k-based LVR solution increased tolerance to the shock state 16-fold compared to saline. Polyethylene glycol-20k is a superior crystalloid for LVR that may increase safe transport times in the prehospital setting and find use in hospital emergency departments and operating rooms for patients awaiting volume replacement or normalization of cell, tissue, and compartment fluid volumes.
NaCl 7,5% ? A voir mais sans Colloïdes.
Pre-Hospital Resuscitation of Traumatic Hemorrhagic Shock with Hypertonic Solutions Worsen Hypo-Coagulation and Hyper-Fibrinolysis
Delano M. et Al. Shock. 2015 Jul;44(1):25-31
-----------------------------------------------
Le choix d'un liquide de remplissage vasculaire n'est pas simple. Au delà des contraintes d'efficacité en termes de remplissage vasculaire, de bonne tolérance notamment rénale il y a également les effets de ce dernier sur la coagulation. On sait qu'une partie importante des blessés actuellement pris en charge présentent une coagulopathie traumatique (1). Le NaCl 7.5% est le soluté recommandé par la procédure du sauvetage au combat (2) car il représente le meilleur compromis intérêt médical/logistique. Le travail ici présenté met en évidence les effets délétères des solutés hypertoniques sur la coagulation. Ce document mérite cependant d'être pondéré car il s'appuie sur une petite cohorte de patients de traumatologie civile, que le profil du remplissage vasculaire préhospitalier n'est pas clairement rapporté hormis le premier liquide, qu'il ne précise pas le niveau de calcémie plasmatique car ce dernier peut être affecté selon la nature des solutés utilisés (4), que le groupe HS a des marqueurs d'hypoperfusion tissulaire identique au groupe NS, que la comparaison se fait avec un groupe de sujets sains et non entre les groupes. Par ailleurs on sait également qu'il est mis en avant l'intérêt des solutions HS en matière de prise en charge des HTIC des plaies cranio-cérébrales (4) et la réduction de l'activation des polynucléaires neutrophiles (5). Donc il ne s'agit pas de remettre en question le choix actuel, mais de le repositionner dans le débat notamment avec l'emploi du Plama lyophylisé comme soluté de remplissage premier des blessés les plus graves (6). Une chose apparait certaine: Ne plus utiliser une association HS/Dextran type RescueFlow (7).
-----------------------------------------------
Impaired hemostasis frequently occurs after traumatic shock and resuscitation. The prehospital fluid administered can exacerbate subsequent bleeding and coagulopathy. Hypertonic solutions are recommended as first-line treatment of traumatic shock; however, their effects on coagulation are unclear. This study explores the impact of resuscitation with various hypertonic solutions on early coagulopathy after trauma. We conducted a prospective observational subgroup analysis of large clinical trial on out-of-hospital single-bolus (250 mL) hypertonic fluid resuscitation of hemorrhagic shock trauma patients (systolic blood pressure, e70 mmHg). Patients received 7.5% NaCl (HS), 7.5% NaCl/6% Dextran 70 (HSD), or 0.9% NaCl (normal saline [NS]) in the prehospital setting. Thirty-four patients were included: 9 HS, 8 HSD, 17 NS. Treatment with HS/HSD led to higher admission systolic blood pressure, sodium, chloride, and osmolarity, whereas lactate, base deficit, fluid requirement, and hemoglobin levels were similar in all groups. The HSD-resuscitated patients had higher admission international normalized ratio values and more hypocoagulable patients, 62% (vs. 55% HS, 47% NS; P G 0.05). Prothrombotic tissue factor was elevated in shock treated with NS but depressed in both HS and HSD groups. Fibrinolytic tissue plasminogen activator and antiYfibrinolytic plasminogen activator inhibitor type 1 were increased by shock but not thrombin-activatable fibrinolysis inhibitor. The HSD patients had the worst imbalance between procoagulation/anticoagulation and profibrinolysis/antifibrinolysis, resulting in more hypocoagulability and hyperfibrinolysis. We concluded that resuscitation with hypertonic solutions, particularly HSD, worsens hypocoagulability and hyperfibrinolysis after hemorrhagic shock in trauma through imbalances in both procoagulants and anticoagulants and both profibrinolytic and antifibrinolytic activities
10/12/2016
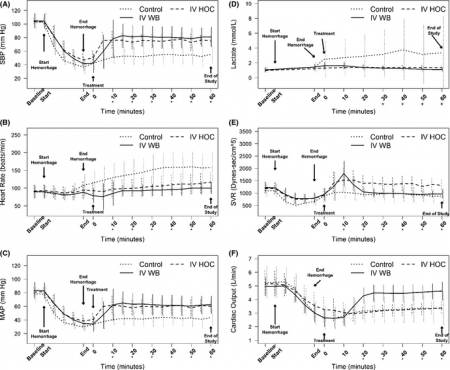
Maintenir la pression: Hydroxocobalamine ou adré ?
A prospective, randomized trial of intravenous hydroxocobalamin versus whole blood transfusion compared to no treatment for Class III hemorrhagic shock resuscitation in a prehospital swine model.
OBJECTIVES:
The objective was to compare systolic blood pressure (sBP) over time in swine that have had 30% of their blood volume removed (Class III shock) and treated with intravenous (IV) whole blood or IV hydroxocobalamin, compared to nontreated controlanimals.
METHODS:
Thirty swine (45 to 55 kg) were anesthetized, intubated, and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged a total of 20 mL/kg over a 20-minute period. Five minutes after hemorrhage, animals were randomly assigned to receive 150 mg/kg IV hydroxocobalamin solubilized in 180 mL of saline, 500 mL of whole blood, or no treatment. Animals were monitored for 60 minutes thereafter. A sample size of 10 animals per group was determined based on a power of 80% and an alpha of 0.05 to detect an effect size of at least a 0.25 difference (>1 standard deviation) in mean sBP between groups. sBP values were analyzed using repeated-measures analysis of variance (RANOVA). Secondary outcome data were analyzed using repeated-measures multivariate analysis of variance (RMANOVA).
RESULTS:
There were no significant differences between hemodynamic parameters of IV hydroxocobalamin versus whole blood versus control group at baseline (MANOVA; Wilks' lambda; p = 0.868) or immediately posthemorrhage (mean sBP = 47 mm Hg vs. 41 mm Hg vs. 37 mm Hg; mean arterial pressure = 39 mm Hg vs. 28 mm Hg vs. 34 mm Hg; mean serum lactate = 1.2 mmol/L vs. 1.4 mmol/L vs. 1.4 mmol/L; MANOVA; Wilks' lambda; p = 0.348). The outcome RANOVA model detected a significant difference by time between groups (p < 0.001). Specifically, 10 minutes after treatment, treated animals showed a significant increase in mean sBP compared to nontreated animals (mean sBP = 76.3 mm Hg vs. 85.7 mm Hg vs. 51.1 mm Hg; p < 0.001). RMANOVA modeling of the secondary data detected a significant difference in mean arterial pressure, heart rate, and serum lactate (p < 0.001). Similar to sBP, 10 minutes after treatment, treated animals showed a significant increase in mean arterial pressure compared to nontreated animals (mean arterial pressure = 67.7 mm Hg vs. 61.4 mm Hg vs. 40.5 mm Hg). By 10 minutes, mean heart rate was significantly slower in treated animals compared to nontreated animals (mean heart rate = 97.3 beats/min vs. 95.2 beats/min vs. 129.5 beats/min; p < 0.05). Serum lactate, an early predictor of shock, continued to rise in the control group, whereas it did not in treated animals. Thirty minutes after treatment, serum lactate values of treated animals were significantly lower compared to nontreated animals (p < 0.05). This trend continued throughout the 60-minute observation period such that 60-minute values for lactate were 1.4 mmol/L versus 1.1 mmol/L versus 3.8 mmol/L. IV hydroxocobalamin produced a statistically significant increase in systemic vascular resistance compared to control, but not whole blood, with a concomitant decrease in cardiac output.
CONCLUSIONS:
Intravenous hydroxocobalamin was more effective than no treatment and as effective as whole blood transfusion, in reversing hypotension and inhibiting rises in serum lactate in this prehospital, controlled, Class III swine hemorrhage model.
| Tags : choc
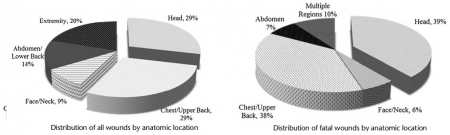
Tueries massives par armes à feu: Penser différemment !
The profile of wounding in civilian public mass shooting fatalities.
BACKGROUND:
The incidence and severity of civilian public mass shootings (CPMS) continue to r.ise. Initiatives predicated on lessons learned from military woundings have placed strong emphasis on hemorrhage control, especially via use of tourniquets, as means to improve survival. We hypothesize that both the overall wounding pattern and the specific fatal wounds in CPMS events are different from those in military combat fatalities and thus may require a new management strategy.
METHODS:
A retrospective study of autopsy reports for all victims involved in 12 CPMS events was performed. Civilian public mass shootings was defined using the FBI and the Congressional Research Service definition. The site of injury, probable site of fatal injury, and presence of potentially survivable injury (defined as survival if prehospital care is provided within 10 minutes and trauma center care within 60 minutes of injury) was determined independently by each author.
RESULTS:
A total 139 fatalities consisting of 371 wounds from 12 CPMS events were reviewed. All wounds were due to gunshots. Victims had an average of 2.7 gunshots. Relative to military reports, the case fatality rate was significantly higher, and incidence of potentially survivable injuries was significantly lower. Overall, 58% of victims had gunshots to the head and chest, and only 20% had extremity wounds. The probable site of fatal wounding was the head or chest in 77% of cases.
Only 7% of victims had potentially survivable wounds. The most common site of potentially survivable injury was the chest (89%). No head injury was potentially survivable. There were no deaths due to exsanguination from an extremity.
CONCLUSION:
The overall and fatal wounding patterns following CPMS are different from those resulting from combat operations. Given that no deaths were due to extremity hemorrhage, a treatment strategy that goes beyond use of tourniquets is needed to rescue the few victims with potentially survivable injuries.
03/12/2016
Voies aériennes: Objectifs de formation CHIFFRE
A n'en pas douter: Il faut un minimum de pratique pour pouvoir prétendre jouer un rôle. Le caractère obligatoire de quotas de geste est en route.
Clic sur l'image pour accéder à la RFE
Intubation/Extubation en REA
Combat MEDEVAC: Par qui ?
Combat MEDEVAC: A comparison of care by provider type for en route trauma care in theater and 30-day patient outcomes.
---------------------------------------------
L'intérêt e la présence d'un personnel à bord d'un vecteur d'évacuation est l'objet de débats passionnés. Le travail présenté ici rapporte l'analyse de MEDEVAC conduites sur le territoire afghan par nos alliés américains. Il ne met pas en évidence d'apport significatif d'équipes disposant de pratiques avancés en traumatologie, y compris pour les blessés les plus sévères. Il confirme le nombre limité de procédures mises en oeuvre (1). Il met même en évidence le moindre recours à des pratiques transfusionnelles dans ce groupe de personnels par rapport au groupe Paramedic, alors que plus d'abord vasculaire et d'apport de liquide de remplissage est conduit. On peut légitimement s'étonner de ces résultats car d'autres publications mettent en avant l'apport de la présence de praticiens disposant de connaissances avancées dans ce domaine (2). la composition de ce groupe de personnels aux pratiques avancées interpelle quand même car il contient des infirmiers des médecins et des assistants médecins dont l'expertise réelle en matière de prise en charge de traumatisés reste non décrite. On peut se poser la question d'une expertise moindre que celle des Paramedics dont le cursus de formation est d'excellente qualité (3). Une autre explication peut être trouvée par la spécificité du territoire afghan où les temps de transport étaient au final assez brefs, sans commune mesure avec celui d'autres théâtres d'intervention, notamment africains (4). Les conditions actuelles de soutien médical nous montre bien que la mise en oeuvre de pratiques avancées par du personnel non seulement PRATIQUANT mais aussi EXPERT doit rester l'objectif essentiel. Un vrai challenge pour les années à venir.
BACKGROUND:
Medical evacuation (MEDEVAC) is the movement and en route care of injured and medically compromised patients by medical care providers via helicopter. Military MEDEVAC platforms provide lifesaving interventions that improve survival in combat. There is limited evidence to support decision making related to en route care and allocation of resources. The association between provider type and en route care is not well understood. Our objective was to describe MEDEVAC providers and identify associations between provider type, procedures performed, and outcomes.
METHODS:
We conducted an institutional review board-approved, retrospective record review of patients traumatically injured incombat, evacuated by MEDEVAC from the point of injury, between 2011 and 2014. Data abstracted included injury description, provider type, procedures performed, medications administered, survival, and 30-day outcomes. Subjects were grouped according to provider type: medics, paramedics, and ADVs (advanced-level providers to include nurses, physician assistants, and physicians). Groups were compared. Analyses were performed using χ tests for categorical variables and analysis of variance tests (Kruskal-Wallis tests) for continuous variables; p < 0.05 was considered significant.
RESULTS:
The MEDEVAC records were reviewed, and data were abstracted from 1,237 subjects. The providers were composed of medics, 76%; paramedics, 21%; and ADVs, 4%. Patient and injury demographics were similar among groups. The ADVs were most likely to perform intubation, chest needle decompressions (p < 0.0001), and hypothermia prevention (p = 0.01). Paramedics were most likely to administer blood en route (p < 0.0001). All other procedures were similar between groups. Paramedics were most likely to administer ketamine (p < 0.0001), any analgesic (p < 0.0001), or any medication en route (p < 0.0001). Incidence rates of en route events (pain, hypoxia, abnormal hemodynamics, vital signs) were similar between provider types. In-theater and 30-day survival rates were similar between provider types.
CONCLUSION:.
Providers with higher-level training were more likely to perform more advanced procedures during en route care. .y found no.ficant .ociati. bet.ee. More evidence is needed to determine the appropriate level of MEDEVAC personnel training and skill maintenance necessary to minimize combat mortality.
| Tags : medevac
02/12/2016
Echo préhospitalière: Expertise à construire svp!
Prehospital ultrasound of the abdomen and thorax changes trauma patient management: A systematic review
O’Dochartaigh D et Al. Injury, Int. J. Care Injured 46 (2015) 2093–2102
--------------------------------------------------
L'échographie tend à prendre une place de plus en plus importante dans notre quotidien. L'existence d'appareils portables, à l'ergonomie et la performance sans cesse améliorée, procède à la généralisation de cet outil d'évaluation dont on comprend bien l'intérêt. Pour autant qu'apporte réellement ce moyen d'exploration et tout particulièrement en préhospitalier ? Et bien les choses ne sont pas si évidentes que cela. Sauf à être mis en oeuvre par des mains expertes et pour des pathologies ciblées et malgré l'engouement général l'intérêt réel reste à prouver. Ce travail n'est pas isolé (1, 2) et devrait nous pousser à une certaine pondération et surtout à des efforts de formation des praticiens ayant recours à cette technique (3).
--------------------------------------------------
Background: Ultrasound examination of trauma patients is increasingly performed in prehospital services. It is unclear if prehospital sonographic assessments change patient management: providing prehospital diagnosis and treatment, determining choice of destination hospital, or treatment at the receiving hospital.
Objective: This review aims to assess and grade the evidence that specifically examines whether prehospital ultrasound (PHUS) of the thorax and/or abdomen changes management of the trauma patient.
Methods: A systematic review was conducted of trauma patients who had an ultrasound of the thorax or abdomen performed in the prehospital setting. PubMed, MEDLINE, Web of Science (CINAHL, EMBASE, Cochrane Central Register of Controlled Trials) and the reference lists of included studies were searched. Methodological quality was checked and risk of bias analysis performed, a level of evidence grade was assigned, and descriptive data analysis performed.
Results: 992 unique citations were identified, which included eight studies that met inclusion criteria with a total of 925 patients. There are no reports of randomised controlled trials. Heterogeneity exists between the included studies which ranged from a case series to retrospective and prospective nonrandomised observational studies. Three studies achieved a 2+ Scottish Intercollegiate Guidelines Networks grade for quality of evidence and the remainder demonstrated a high risk of bias. The three best studies each provided examples of prehospital ultrasound positively changing patient management.
Conclusion: There is moderate evidence that supports prehospital physician use of ultrasound for trauma patients. For some patients, management was changed based on the results of the PHUS. The benefit of ultrasound use in non-physician services is unclear.