11/10/2014
Suis je bien dans la trachée ?
Comment vérifier la position intratrachéale d'une sonde d'intubation ?
Le débat n'est pas nouveau (1). L'intérêt de l'intubation en condition de combat est d'ouvrir les voies aériennes, de prévenir le risque d'inhalation et de permettre l'application d'une ventilation adéquate. Son indication doit être bien mesurée car elle va ajouter une dimension de complexité pour un transport préhospitalier qui n'a rien à voir avec ce qui est rencontré en métropole.
Alors quelques réflexions ne sont pas inutiles car il faut éviter tant l'intubation oesophagienne que l'intubation sélective.
1. La visualisation de la sonde entre les cordes vocales est la base que ce soit au moment de la laryngoscopie initiale ou d'un contrôle après MAIS ce n'est pas suffisant, et pas forcément toujours possible.
2. La recherche d'une auscultation symétrique des 2 champs pulmonaires et d'un silence auscultatoire épigastrique doivent être fait MAIS ce n'est pas suffisant, et parfois difficile à obtenir.
3. L'expansion thoracique symétrique et la constatation de buée sur la sonde sont observées MAIS ce n'est pas suffisant.
4. Le recours à la mesure d'une SaO2 MAIS n'est pas du tout fait pour cela.
5. Utiliser une seringue ou un bulbe spécifique MAIS n'offre pas de certitude et c'est une techniQue peu diffusée en France
6. La CERTITUDE de l'intubation est donnée par la constatation de CO2 dans le gaz expiré à condition que soient respectés des critères quantitatifs et qualitatifs. Notamment les capnogrammes doivent être visualisés sur au moins 6 cycles ventilatoires durant lesquels l’absence de décroissance du signal confirme la bonne position de la sonde. (accéder à la conférence de consensus de la SFAR). Cette analyse qualitative est importante car le CO2 observé peut provenir d'air gastrique insufflé lors de ventilation manuelle voire d'anti-acides gastriques.
Mais dans notre contexte d'emploi la capnographie, telle que l'on la connait au bloc opératoire ou en SAUV, n'est pas le plus souvent disponible. Vous disposez de capteurs chimiques qui ne donnent qu'une estimation de la capnométrie. Certains disposent d'un capnomètre portable mais qui ne donne pas d'informations qualitatives. Enfin il existe des détecteurs oesophagiens dont la performance est bonne (2), sous réserve de conditions de stockage et d'emploi conforme notamment de température ambiante, mais qui ne permettent pas une surveillance continue et surtout si ils sont fiables pour confirmer la position intra-trachéale, ils le sont beaucoup moins pour la position intra-oeosophagienne.
7. Du nouveau arrive avec l'emploi de l'échographie pour valider la position intra-trachéale de la sonde d'intubation:
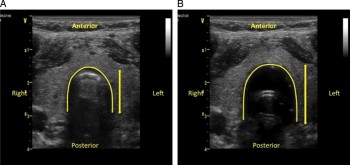
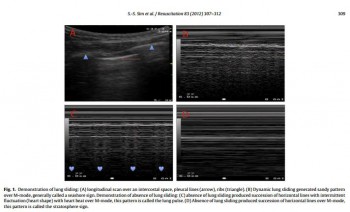
- soit par échographie cervicale (3, 4),
Kerforne T et al. Br. J. Anaesth. 2013;111:510-511
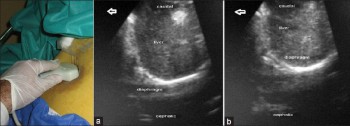
- soit par constatation de mouvements pleuraux bilatéraux (5)
- ou encore d'une mobilité diaphragmatique lors de la ventilation (6)
Int J Crit Illn Inj Sci. 2013 Apr;3(2):113-7
En contexte Militaire et en l'absence de capnographe, il faut, avant fixation de la sonde de vérification, dans le cadre la réalisation de mesures primaires de vérification de la bonne position de la sonde d'intubation ASSOCIER l'observation directe de la sonde franchissant les cordes vocales, l'expansion symétrique du thorax lors de la ventilation au ballon, la présence de buée dans la sonde, l'auscultation symétrique des deux champs pulmonaires et la présence de CO2 expiré sur le détecteur chimique. L'apport de l'échographie pourrait être d'être l'alternative à la radiographie pulmonaire pour la vérification secondaire de la bonne position de la sonde d'intubation.
Un débat qui porte sur la meilleure performance comparée à la capnographie et l'auscultation du repérage échographique est même déjà ouvert (7, 8, 9).
| Tags : airway
06/10/2014
Laryngoscopie directe: Toujours la référence en 1ère intention
Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: a randomized control trial.
Trimmel H et all. Crit Care Med 2011 Mar;39(3):489-93
__________________________________________
Une étude un peu ancienne mais qui a depuis été confirmée par d'autres (1, 2) et qui met bien en avant l'importance d'un apprentissage renforcé de la gestion des voies aériennes. Une méta-analyse plus récente le confirme (3).
__________________________________________
OBJECTIVES
The optical Airtraq laryngoscope (Prodol Meditec, Vizcaya, Spain) has been shown to have advantages when compared with direct laryngoscopy in difficult airway patients. Furthermore, it has been suggested that it is easy to use and handle even for inexperienced advanced life support providers. As such, we sought to assess whether the Airtraq may be a reliable alternative to conventional intubation when used in the prehospital setting.
DESIGN, SETTING, AND PATIENTS:
Prospective, randomized control trial in emergency patients requiring endotracheal intubation provided by anesthesiologists or emergency physicians responding with an emergency medical service helicopter or ground unit associated with the Department of Anesthesiology, General Hospital, Wiener Neustadt, Austria.
MEASUREMENTS AND MAIN RESULTS:
During the 18-month study period, 212 patients were enrolled. When the Airtraq was used as first-line airway device (n=106) vs. direct laryngoscopy (n=106), success rate was 47% vs. 99%, respectively (p<.001). Reasons for failed Airtraq intubation were related to the fiber-optic characteristic of this device (i.e., impaired sight due to blood and vomitus, n=11) or to assumed handling problems (i.e., cuff damage, tube misplacement, or inappropriate visualization of the glottis, n=24). In 54 of 56 patients where Airtraq intubation failed, direct laryngoscopy was successful on the first attempt; in the remaining two and in one additional case of failed direct laryngoscopy, the airway was finally secured employing the Fastrach laryngeal mask. There was no correlation between success rates and body mass index, age, indication for airway management, emergency medical service unit, or experience of the physicians.
CONCLUSIONS:
Based on these results, the use of the Airtraq laryngoscope as a primary airway device cannot be recommended in the prehospital setting without significant clinical experience obtained in the operation room. We conclude that the clinical learning process of the Airtraq laryngoscope is much longer than reported in the anesthesia literature.
| Tags : airway
20/09/2014
Intubation face à face: Du nouveau ?
Comparison of Sitting Face-to-Face Intubation (Two-Person Technique) with Standard Oral-tracheal Intubation in Novices: A Mannequin Study
J Emerg Med. 2012 Dec;43(6):1188-95
L'intubation face au patient n'est pas une nouveauté que ce soit en préhospitalier ou au bloc opératoire. Elle est cependant très peu fréquemment mise en oeuvre. Pourtant l'apparition des vidéolaryngoscopes, notamment l'airtraq, simplifie grandement cette pratique (vidéo ici). Certains s'interrogent sur son emploi plus large. Elle serait plus aisée que la laryngoscopie directe en décubitus dorsal. C'est ce que suggère ce document. Un grand recul est cependant nécessaire. Ce travail a été fait sur mannequin.
BACKGROUND:
Few studies have evaluated the impact of the upright position on the success of oral-tracheal intubation. Yet, for patients with airway difficulties (i.e, active intraoral bleeding or morbidly obese), the upright position may both benefit the patient and facilitate intubation.
OBJECTIVES:
We compared the success rates of subjects performing standard intubation to a modified version of the sitting face-to-face oral-tracheal intubation technique on a simulation model. We also reviewed the possible advantages and limitations of the sitting face-to-face intubationtechnique.
METHODS:
Volunteer medical and paramedical students were given instruction, then tested, performing in random order both standard oral-trachealand two-person sitting face-to-face oral-tracheal intubation on full-bodied mannequins. Observers reviewed video recordings, noting the number of successful intubations and the time to completion of each procedure at 15, 20, and 30 s.
RESULTS:
All of the sitting face-to-face intubations were successful, 53/53 (100%, 95% confidence interval [CI] 93-100%); whereas of the 53 subjects who performed standard intubation, 48 were successful (91%, 95% CI 80-96%). The difference between successful intubations using thestandard vs. sitting face-to-face technique was 9% (95% CI 1.3-9.4%, p=0.025). At times 15 and 20 s, medical student subjects who successfully performed both techniques were less successful at completing the procedure when performing the standard technique as compared to the sittingface-to-face technique (p=0.016). A post-procedural survey found that the majority of subjects preferred the sitting technique.
CONCLUSION:
Subjects were significantly more successful at performing and preferred the sitting face-to-face intubation when compared to standardintubation.
| Tags : airway
06/09/2014
Coniotomie: Comment en situation isolée ?
| Tags : airway, coniotomie
30/08/2014
Que font les israéliens en role 1
Role I trauma experience of the Israeli Defense Forces on the Syrian border
Benov A. et All. J Trauma Acute Care Surg. 2014 Sep;77(3 Suppl 2):S71-6
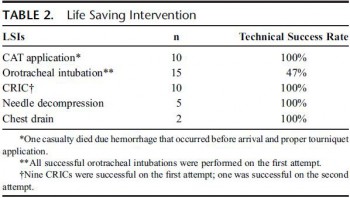
Une des particularités des actions conduites en role 1 par les équipes israéliennes est la maîtrise par leurs personnels des gestes de contrôle des voies aériennes, qu'il s'agisse de médecins ou de paramédic EMT-P. Cette publication l'illistre et confirme l'importance actuelle de ce savoir faire qui est donc ESSENTIEL pour une médicalisation réelle de l'avant.
---------------------------------------------------------------------------------------------------------------------
" Two-hundred fifty-eight casualties arrived at the border, 60 of whom were evaluated and returned to Syria. Of those, 15 received basic care and did not require any additional intervention, 39 experienced chronic conditions with no immediate need for medical attention, and 6 were dead on arrival. ......................Data from all echelons including prehospital information were available for 178 (90%) of the 198 patients, and this group constituted the study cohort. The extent of medical evacuation among the 178 casualtiesis as follows: 8 (4%) required only Role I care (debridement of wounds, removal of fragments, or death despite resuscitation attempts); 65 (36%) were evacuated to a Role 2+ facility and were later discharged; and 84 (47%) were evacuated to Role 3 civilian hospitals. ................................Eighteen patients underwent advanced airway procedures. Of 14 patients with a documented oxygen saturation of less than 90%, 5 improved following oxygen supplementation and did not require airway intervention. Of the 18 patients undergoing definitive airway management, head and face injury was present in two thirds (n = 11) of these, whereas a quarter (n = 4) had thoracic injury. The procedures were endotracheal intubation (ETI) (n = n = 15) and cricothyroidotomy (CRIC) (n = 10). Seven of eight casualties underwent CRI following failed initial attempt at ETI, and one patient was able to have mask ventilation following failed ETI. In three cases, CRIC was the first choice of airway management, two patients experiencing severe maxillofacial injury and one with severe laryngeal edema. There were no cases of preventable death due to airway obstruction and no complications from airway interventions. Forty-three casualties experienced thoracic injuries, five underwent chest decompression at a Role I facility by either needle decompression (n = 3) or insertion of a chest drain (n = 2).
| Tags : airway
03/07/2014
Dispositifs laryngés préhospitalier: Prudence !
Prehospital airway management using the laryngeal tube : An emergency department point of view.
Bernardht M. et Al Anaesthesist. 2014 Jul 2. [Epub ahead of print]
Il est proposé d'avoir recours à des dispositifs supra glottique pour la maîtrise de l'abord des voies aériennes en préhospitalier. Si ces dispositifs présentent des avantages avec notamment celui supposé d'une insertion plus simple que l'intubation ces derniers ont également des limites. AInsi l'engouement actuel doit il être tempéré par des inconvénients qui commencent à être décrits. C'est ce que rapporte l'article.
Parmi ceux ci, il y a les mauvais placement avec pour conséquence un défaut de ventilation du patient, un oedème obstructif de langue malgré des temps de pose court inférieur à 45 min et une situation d'intubation difficile, des problèmes d'étanchéité avec dans un cas une insufflation gastrique importante responsable d'un gêne à la ventilation contrôlée, un défaut de protection des voies aériennes avec inhalation du contenu gastrique.
Ce travail illustre donc que le recours aux dispositifs supraglottique ne doit pas être pensé comme une alternative à l'intubation qui permettrait à des opérateurs moins formés de pouvoir réaliser un geste de contrôle des voies aériennes. Il ne remet pas en cause l'intérêt de certains masques notamment les masques laryngés d'intubation qui on toute leur place dans la stratégie de gestion de l'intubation difficile. Enfin en condition de combat on rappelle que les 3 techniques dont la maîtrise doit être parfaite sont la ventilation manuelle, l'intubation oro-trachéale avec ISR et la coniotomie. Ceci est également le positionnement de l'armée israélienne. On retrouve là, comme avec l'exsufflation des pneumothorax avec des aiguilles de 8 cm en lieu et place des cathéters courants, outre la prudence nécessaire à avoir face à des avantages apparents sans analyses des inconvénients associés.
BACKGROUND:
Competence in airway management and maintenance of oxygenation and ventilation represent fundamental skills in emergency medicine. The successful use of laryngeal tubes (LT, LT-D, LTS II) to secure the airway in the prehospital setting has been published in the past. However, some complications can be associated with the use of a laryngeal tube.
METHODS:
In a nonconsecutive case series, problems and complications associated with the use of the laryngeal tube in prehospital emergency medicine as seen by independent observers in the emergency room are presented.
RESULTS:
Various problems and possible complications associated with the use of a laryngeal tube in eight case reports are reported: incorrect placement of the laryngeal tube in the trachea, displacement and/or incorrect placement of the laryngeal tube in the pharynx, tongue and pharyngeal swelling with subsequently difficult laryngoscopy, and inadequate ventilation due to unrecognized airway obstruction and tension pneumothorax.
CONCLUSION:
Although the laryngeal tube is considered to be an effective, safe, and rapidly appropriable supraglottic airway device, it is also associated with adverse effects. In order to prevent tongue swelling, after initial prehospital or in-hospital placement of laryngeal tube and cuff inflation, it is important to adjust and monitor the cuff pressure.
| Tags : airway
13/06/2014
Airway Cam Portal
| Tags : airway
05/06/2014
Réflexions US sur l'accès aux voies aériennes
Advances in prehospital airway management
Jacobs PE et all. Int J Crit Illn Inj Sci. 2014 Jan-Mar; 4(1): 57–64.
Prehospital airway management is a key component of emergency responders and remains an important task of Emergency Medical Service (EMS) systems worldwide. The most advanced airway management techniques involving placement of oropharyngeal airways such as the Laryngeal Mask Airway or endotracheal tube. Endotracheal tube placement success is a common measure of out-of-hospital airway management quality. Regional variation in regard to training, education, and procedural exposure may be the major contributor to the findings in success and patient outcome. In studies demonstrating poor outcomes related to prehospital-attempted endotracheal intubation (ETI), both training and skill level of the provider are usually often low. Research supports a relationship between the number of intubation experiences and ETI success. National standards for certification of emergency medicine provider are in general too low to guarantee good success rate in emergency airway management by paramedics and physicians. Some paramedic training programs require more intense airway training above the national standard and some EMS systems in Europe staff their system with anesthesia providers instead. ETI remains the cornerstone of definitive prehospital airway management, However, ETI is not without risk and outcomes data remains controversial. Many systems may benefit from more input and guidance by the anesthesia department, which have higher volumes of airway management procedures and extensive training and experience not just with training of airway management but also with different airway management techniques and adjuncts.
| Tags : airway, intubation
27/05/2014
Maîtrise de la coniotomie en environnement austère: Une nécessité.
Optimizing Emergent Surgical Cricothyrotomy for use in Austere Environments
HessertMJ et Al. Wilderness Environ Med. 2013 Mar;24(1):53-66
" Although cricothyrotomy is becoming less common as other alternative airway devices are introduced, such as the laryngeal mask airway, King LT-D (King Systems Corp, Noblesville, IN), and other supraglottic devices, there is, and likely always will be, a role for cricothy- rotomy in a subsection of patients with difficult airways, especially in environments in which such devices are unlikely to be available. A common emergency medicine aphorism is: “If you do one cricothyrotomy, you’re a hero; if you do two, work on your airway skills.” True perhaps in a hospital, but in an austere environment many factors besides failed ET intubation lead to early cricothyrotomy. Wilderness providers must be not only technically skilled, but also adequately trained to recognize the key indications and situational decision triggers for cricothyrotomy that differ from in-hospital practice."
| Tags : airway, coniotomie, intubation
23/05/2014
Manoeuvre de Sellick: Questions/Réponses
Cricoid Pressure in Emergency Department Rapid Sequence Tracheal Intubations: A Risk-Benefit Analysis
Ellis DY et Al. An Emerg Med. 2007 Dec;50(6):653-65
La manœuvre de Sellick est une technique de compression du cartilage cricoïde, décrite en 1961 par Sellick BA. Lors de la réalisation d'une intubation trachéale, elle est utilisée pour prévenir le risque de régurgitation du contenu gastrique et œsophagien vers le pharynx et son inhalation bronchique et alvéolaire lors de l'induction anesthésique qui entraîne une dépression des réflexes de protection des voies aériennes, chez un patient dont l’estomac est plein.
Elle consiste à appuyer fermement sur le cartilage cricoïde qui va alors comprimer l'extrémité supérieure de l'œsophage dont les parois sont souples, contre le corps vertébral de la vertèbre cervicale sous-jacente, rigide. L'intensité de la force à exercer doit être d'environ 20 newtons (N) si le patient est conscient et de 30 N s'il est inconscient2. Cette force est suffisante pour prévenir la régurgitation (inefficace si inférieure à 10 N), n'entraîne pas de sensation nauséeuses susceptibles d'augmenter l'inhalation du contenu gastrique et met à l'abri d'une rupture œsophagienne.
Le taux d'efficacité de la manœuvre de Sellick n'est pas bien établi, techniquement simple, elle est pourtant souvent mal réalisée.
-----------------------------------------------------------------------
Cricoid pressure is considered an integral part of patient safety in rapid sequence tracheal intubation and emergency airway management. Cricoid pressure is applied to prevent the regurgitation of gastric contents into the pharynx and subsequent aspiration into the pulmonary tree. This review analyzes the published evidence supporting cricoid pressure, along with potential problems, including increased difficulty with tracheal intubation and ventilation. According to the evidence available, the universal and continuous application of cricoid pressure during emergency airway management is questioned. An awareness of the benefits and potential problems with technique allows the practitioner to better judge when cricoid pressure should be used and instances in which it should be removed.
-----------------------------------------------------------------------
Le travail présenté répond à un certain nombre d'interrogations et précise pourquoi la réalisation de cette manoeuvre est remise en question.
| Tags : airway
08/04/2014
Coniotomie au Combat: Simuler pour retenir le savoir
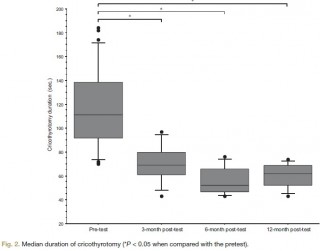
Vincent H. et Al. Anesthesiology 2014; 120:999-1008
background:
The effectiveness of simulation is rarely evaluated. The aim of this study was to assess the impact of a short training course on the ability of anesthesiology residents to comply with current difficult airway management guidelines.
METHODS:
Twenty-seven third-year anesthesiology residents were assessed on a simulator in a "can't intubate, can't ventilate" scenario before the training (the pretest) and then randomly 3, 6, or 12 months after training (the posttest). The scenario was built so that the resident was prompted to perform a cricothyrotomy. Compliance with airway management guidelines and the cricothyrotomy's duration and technical quality were assessed as a checklist score [0 to 10] and a global rating scale [7 to 35].
RESULTS:
After training, all 27 residents (100%) complied with the airway management guidelines, compared with 17 (63%) in the pretest (P < 0.005). In the pretest and the 3-, 6-, and 12-month posttests, the median [range] duration of cricothyrotomy was respectively 117 s [70 to 184], 69 s [43 to 97], 52 s [43 to 76], and 62 s [43 to 74] (P < 0.0001 vs. in the pretest), the median [range] checklist score was 3 [0 to 7], 10 [8 to 10], 9 [6 to 10], and 9 [4 to 10] (P < 0.0001 vs. in the pretest) and the median [range] global rating scale was 12 [7 to 22], 30 [20 to 35], 33 [23 to 35], and 31 [18 to 33] (P < 0.0001 vs. in the pretest). There were no significant differences between performance levels achieved in the 3-, 6-, and 12-month posttests.
CONCLUSION: The training session significantly improved the residents' compliance with guidelines and their performance of cricothyrotomy.
| Tags : airway, intubation
07/04/2014
Airway en préhospitalier US: Plus tube que dispositif glottique
An update on out-of-hospital airway management practices in the United States
Diggs LA. et Al. Resuscitation. 2014 Mar 15. pii: S0300-9572
______________________________________________________
Ce document fait le point sur la pratique préhospitalière US. Cette dernière est faite avant tout d'intubation et la prudence est de mise concernant les performances réelles des dispositifs supra-glottiques avec lesquels (excepté le tube de king) les résultats sont moins bons.
______________________________________________________
OBJECTIVE: We characterized out-of-hospital airway management interventions, outcomes, and complications using the 2012 NEMSIS Public-Release Research Data Set containing almost 20 million Emergency Medical Services activations from 40 states and two territories. We compared the outcomes with a previous study that used 2008 NEMSIS data containing 16 states with 4 million EMS activations.
METHODS:
Patients who received airway management interventions including endotracheal intubation (ETI), alternate airways (Combitube, Laryngeal Mask Airway (LMA), King LT, Esophageal-Obturator Airway (EOA)), and cricothyroidotomy (needle and surgical) were identified. Using descriptive statistics, airway management success and complications were examined in the full cohort and key subsets including cardiac arrest, non-arrest medical, non-arrest injury, children<10 years, children 10-19 years, rapid sequence intubation (RSI), population setting, US census region, and US census division.
RESULTS:
Among 19,831,189 EMS activations, there were 74,993 ETIs, 21,990 alternate airways, and 1332 cricothyroidotomies. ETI success rates were: overall 63,956/74,993 (85.3%; 95% CI: 85.0-85.5), cardiac arrest 33,558/39,270 (85.5%), non-arrest medical 12,215/13,611 (89.7%), non-arrest injury (90.1%), children<10 years 2069/2468 (83.8%), children 10-19 years 1647/1900 (86.7%), adults>19 years 58,965/69,144 (85.3%), and rapid sequence intubation 5265/5658 (93.1%). Major complications included bleeding 677 (4.4 per 1000 interventions), vomiting 1221 (8 per 1000 interventions), esophageal intubation immediately detected 874 (5.7 per 1000 interventions), and esophageal intubations other 219 (1.4 per 1000 interventions).
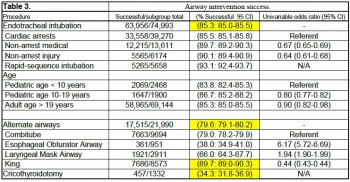
CONCLUSIONS:
Paramedics provide life-saving emergency medical care to patients in the out-of-hospital setting. Only selected emergency medical procedures have proved to be safe and effective. The safety and efficacy profile of ETI has been challenged in the last ten years. Intubation has been the standard of care in the United States for more than thirty years and is regarded as one of the most important EMS procedures. In this study, we retrospectively examined the largest aggregate of EMS data currently available and observed low out-of-hospital ETI success rates.
ETI is a complex procedure requiring skilled choreography and numerous critical decisions and actions. In the absence of qualified personnel, or if ETI proves problematic, alternate airways are commonly employed. As more EMS systems embrace alternate airway devices in lieu of ETI, it is important to have a clear appreciation of the true success rates of airway procedures using these devices across a variety of patient characteristics and clinical settings. This study examined the most commonly used alternate airway devices including the Combitube, Esophageal Obturator Airway, Laryngeal Mask Airway, King Laryngeal Tube, and cricothyroidotomy and observed very low alternate airway success rates in the largest population sample to date. Alternate airway success rates were substantially lower than ETI success rates except for the King LT.
| Tags : airway, intubation
29/01/2014
Trauma ballistique de la face: 1/3 nécessitent un airway sécurisé
Gunshot wounds and blast injuries to the face are associated with significant morbidity and mortality: Results of an 11-year multi-institutional study of 720 patients
Shackford et All. J Trauma Acute Care Surg. 2014;76: 347-352
BACKGROUND:
Gunshot wounds and blast injuries to the face (GSWBIFs) produce complex wounds requiring management by multiple surgical specialties. Previous work is limited to single institution reports with little information on processes of care or outcome. We sought to determine those factors associated with hospital complications and mortality.
METHODS:
We performed an 11-year multicenter retrospective cohort analysis of patients sustaining GSWBIF. The face, defined as the area anterior to the external auditory meatuses from the top of the forehead to the chin, was categorized into three zones: I, the chin to the base of the nose; II, the base of the nose to the eyebrows; III, above the brows. We analyzed the effect of multiple factors on outcome.
RESULTS:
From January 1, 2000, to December 31, 2010, we treated 720 patients with GSWBIF (539 males, 75%), with a median age of 29 years. The wounding agent was handgun in 41%, explosive (shotgun and blast) in 20%, rifle in 6%, and unknown in 33%. Prehospital or resuscitative phase airway was required in 236 patients (33%). Definitive care was rendered by multiple specialties in 271 patients (38%). Overall, 185 patients died (26%), 146 (79%) within 48 hours. Of the 481 patients hospitalized greater than 48 hours, 184 had at least one complication (38%). Factors significantly associated with any of a total of 207 complications were total number of operations (p < 0.001), Revised Trauma Score (RTS, p < 0.001), and head Abbreviated Injury Scale (AIS) score (p < 0.05). Factors significantly associated with mortality were RTS (p < 0.001), head AIS score (p < 0.001), total number of operations (p < 0.001), and age (p < 0.05). An injury located in Zone III was independently associated with mortality (p < 0.001).
CONCLUSION:
GSWBIFs have high mortality and are associated with significant morbidity. The multispecialty involvement required for definitive care necessitates triage to a trauma center and underscores the need for an organized approach and the development of effective guidelines.
| Tags : airway
07/12/2013
Rupture cricotrachéale: Que faire ?
Cricotracheal Separation after Gunshot to the Neck: Report of a Survivor with Recovery of Bilateral Vocal Fold Function.
Vivero RJ et Al. http://dx.doi.org/10.1016/j.jemermed.2013.08.090
Il s'agit d'une éventualité rarissime mais cette observation montre qu'en situation d'isolement extrême il peut être possible d'agir si la partie distale est visible. Encore faut il connaître l'existence de cette conduite à tenir.
------------------------------------------------------
Initial appropriate airway management is imperative to improve survival. Numerous case reports in the literature demonstrate incidental findings of airway injury after routine workup of the patient or the advent of ominous clinical findings (1,2) . At this stage in patient management, it can become difficult to adequately secure the airway, which places the patient at increased risk. A careful physical examination is therefore critical, with fiberoptic laryngoscopy used, as necessary, in the stable patient. A CT scan can be a useful adjunct in the clinical workup, but it should not be relied upon solely, as it can be inconclusive (3) . When cricotracheal separation is identified and the patient is stable, the airway should be secured surgically in the operating room or trauma bay. The proximal stump of the airway should be grasped and secured with a clamp, and then an awake tracheotomy performed (under local anesthesia if possible) distal to the injury. In the event that the patient is unstable or that intubation fails, the distal stump of the trachea should be identified either visually or by palpation. The stump of trachea should then be grasped with a clamp and pulled superficially (out of the wound toward the skin surface), and an appropriately sized endotracheal tube is placed as a temporary measure and secured. The clamp should not be removed from the airway, as the distal tracheal stump can retract into the mediastinum. The patient should then be taken to the operating room emergently for formal tracheotomy or maturation of the airway tracheostoma. In general, cricothyrotomy should not be performed, as this is usually proximal to the site of airway separation.
| Tags : airway
06/11/2013
Oxygénation transtrachéale de sauvetage
Viable oxygenation with cannula-overneedle cricothyrotomy for asphyxial airway occlusion
Kofke WA et Al. Br. J. Anaesth. (2011) 107 (4): 642-643.
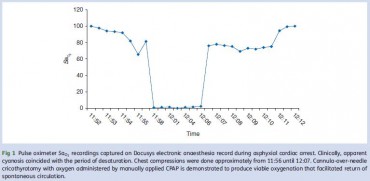
Le recours à un cathéter veineux et une seringue pour la réalisation d'une coniotomie est souvent présenté comme un simple gadget.
Cette technique a été mise en oeuvre dans le cadre de la prise en charge d'un arrêt circulatoire dans un bloc opéatoire. L'usage d'un cathéter de 14g, d'une seringue de 3ml associé à l'application continue doxygène à une pression de 35 à 4O mmHg a permis la restauration d'une oxygénation suffisante contribuant ainsi au succès des manoeuvres de prise en charge de l'arrêt circulatoires.
Le fait d'avoir à disposition une machine d'anesthésie permettant de générer une pression d'insufflation continue et élevée est certainement un élément essentiel à prendre en compte. Il n'est pas certain que ceci puisse être réalisé avec un BAVU sauf à bien obturer la valve notamment celle de surpression si elle existe.
| Tags : airway, coniotomie
Coniotomie: Chirurgicale avec un mandrin
Comparison of a percutaneous device and the bougie-assisted surgical technique for emergency cricothyrotomy: an experimental study on a porcine model performed by air ambulance anaesthesiologists
Nakstad et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2013, 21:59
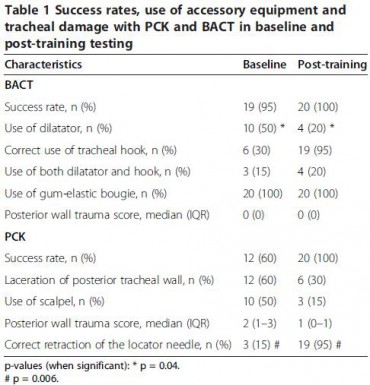
Background: A large number of techniques and devices for cricothyroidotomy have been developed. In this study, the Portex™ Cricothyroidotomy Kit (PCK, Smiths Medical Ltd, Hythe, UK) was compared with the bougie assisted emergency surgical cricothyrotomy technique (BACT).
Methods: Twenty air ambulance anaesthesiologists performed emergency cricothyrotomy on a cadaveric porcine airway model using both PCK and BACT. Baseline performance and performance after the intensive training package were recorded. Success rate, time to secured airway and tracheal damage were the primary endpoints, and confidence rating was a secondary endpoint.
Results: During baseline testing, success rates for PCK and BACT were 60% and 95%, respectively. Tracheal injury rate with PCK was 60% while no such injury was found in BACT. A lecture was given and skills were trained until the participants were able to perform five consecutive successful procedures with both techniques. In the posttraining test, all participants were successful with either technique. The mean time to successful insertion was reduced by 15.7 seconds (from 36.3 seconds to 20.6 seconds, p< 0.001) for PCK and by 7.8 seconds (from 44.9 seconds to 37.1 seconds, p=0.021) for BACT. In the post-training scenario, securing the airway with PCK was significantly faster than with BACT (p<0.001). Post-training tracheal laceration occurred in six (30%) of the PCK procedures and in none of the BACT procedures (p=0.028). The self-evaluated confidence level was measured both pre- and post-training using a confidence scale with 10 indicating maximum amount of confidence. The median values increased from 4 to 8 for PCK and from 6.5 to 9.5 for BACT. All participants reported that BACT was their preferred technique.
Conclusions: Testing the base-line PCK skills of prehospital anaesthesiologists revealed low confidence, sub-optimal performance and a very high failure rate. The BACT technique demonstrated a significantly higher success rate and no tracheal damage. In spite of PCK being a significantly faster technique in the post-training test, the anaesthesiologists still reported a higher confidence in BACT. Limitations of the cadaveric porcine airway may have influenced this study because the airway did not challenge the clinicians with realistic tissue bleeding.
| Tags : airway, coniotomie
Coniotomie: On fait le point
Emergency cricothyrotomy - A systematic review
Langvad F. et Al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2013 21:43
Une revue exhaustive de ce qui est publié sur le sujet. Il en ressort qu'il n'existe pas vraiment d'avantages d'une technique sur une autre, qu'en condition extrême une technique chirurgicale semble préférable. Le point clé est l'expérience et l'entraînement de celui qui la réalise.
----------------------------
Background: An emergency cricothyrotomy is the last-resort in most airway management protocols and is performed when it is not possible to intubate or ventilate a patient. This situation can rapidly prove fatal, making it important to identify the best method to establish a secure airway. We conducted a systematic review to identify whether there exists superiority between available commercial kits versus traditional surgical and needle techniques.
Methods: Medline, EMBASE and other databases were searched for pertinent studies. The inclusion criteria included manikin, animal and human studies and there were no restrictions regarding the professional background of the person performing the procedure.
Results: In total, 1,405 unique references were identified; 108 full text articles were retrieved; and 24 studies were included in the review. Studies comparing kits with one another or with various surgical and needle techniques were identified. The outcome measures included in this systematic review were success rate and time consumption. The investigators performing the studies had chosen unique combinations of starting and stopping points for time measurements, making comparisons between studies difficult and leading to many conflicting results. No single method was shown to be better than the others, but the size of the studies makes it impossible to draw firm conclusions.
Conclusions: The large majority of the studies were too small to demonstrate statistically significant differences, and the limited available evidence was of low or very low quality. That none of the techniques in these studies demonstrated better results than the others does not necessarily indicate that each is equally good, and these conclusions will likely change as new evidence becomes available
| Tags : coniotomie, airway
Voies aériennes: Avant tout une histoire de communication
Airway management: judgment and communication more than gadgets
Donati F. Can J Anesth/J Can Anesth (2013) 60:1035–1040
------------------------------------
Un éditorial publié à l'occasion de la sortie des nouvelles recommandations canadiennes sur l'intubation difficile (1 et 2). Plein de on sens et de pragmatisme et au final de rigueur scientifique dans ce document qui insiste sur le facteur humain et non le facteur matériel. . Les points essentiels sont
1. le maintien de l’oxygènation est proposé comme objectif ultime de toute manœuvre au niveau des voies aériennes
Non pas
"cannot intubate cannot ventilate"
mais
"cannot intubate cannot oxygenate"
2. Malgré la popularité croissante et l’utilisation répandue des dispositifs supraglottiques, l’intubation trachéale demeure l’étalon or et la méthode préférée pour une prise en charge stable des voies aériennes.
3. La vidéolaryngoscopie n’est pas présentée comme la solution universelle à tous les problèmes liés aux voies aériennes
4. Le nombre de tentatives, quelle que soit la technique d’intubation ou la position, devrait se limiter à trois même si n’existe aucune donnée probante solide appuyant un tel énoncé.
5. Même si il existe des données probantes selon lesquelles un accès chirurgical aux voies aériennes chirurgicales ne sauve pas toujours des vies, le groupe recommande d’essayer d’obtenir un accès chirurgical aux voies aériennes lorsque tous les autres types de tentative échouent.
05/11/2013
Coniotomie: Un nouveau set
A Comparison of Two Open Surgical Cricothyroidotomy Techniques by Military Medics Using a Cadaver Model
Mabry RL et All., Ann EmergMed. 2013;-:1-5
---------------------------------
Le taux d'échec observé est d'environ 33%. Aussi est on toujours à la recherche de dispositifs d'aide à la réalisation de ce geste considéré comme essentiel. L'originalité du kit présenté ici tient à son guide qui a une forme particulière censée améliorer la performance des combat medics. Relisez la fiche technique de la coniotomie en sachant que vous pouvez vous servir du mandrin d'eschmann comme guide d'insertion si vous avez recours à la technique chirurgicale ce qui est recommandé.
---------------------------------
Study objective: The CricKey is a novel surgical cricothyroidotomy device combining the functions of a tracheal hook, stylet, dilator, and bougie incorporated with a Melker airway cannula. This study compares surgical cricothyroidotomy with standard open surgical versus CricKey technique.
Methods: This was a prospective crossover study using human cadaveric models. Participants included US Army combat medics credentialed at the emergency medical technician–basic level. After a brief anatomy review and demonstration, participants performed in random order standard open surgical cricothyroidotomy and CricKey surgical cricothyroidotomy. The primary outcome was first-pass success, and the secondary outcome measure was procedural time.
Results: First-attempt success was 100% (15/15) for CricKey surgical cricothyroidotomy and 66% (10/15) for open surgical cricothyroidotomy (odds ratio 16.0; 95% confidence interval 0.8 to 326). Surgical cricothyroidotomy insertion was faster for CricKey than open technique (34 versus 65 seconds; median time difference 28 seconds; 95% confidence interval 16 to 48 seconds).
Conclusion: Compared with the standard open surgical cricothyroidotomy technique, military medics demonstrated faster insertion with the CricKey. First-pass success was not significantly different between the techniques
| Tags : coniotomie, airway
29/10/2013
Intubation en préhospitalier : intérêt des nouvelles techniques
IOT difficile et les nouveaux outils en situation d’urgence ( où en est-on ? )
Les procédures validées
Combes X et All. Urgences - 2013
Points essentiels
■ L’intubation en séquence rapide est la technique de sédation validée pour faciliter l’intubation en situation d’urgence.
■ La préoxygénation peut être réalisée par VNI chez le patient coopérant.
■ Les lames de laryngoscopes en plastique ne doivent pas être utilisées.
■ L’utilisation du mandrin long béquillé est parfaitement validée en situation d’urgence en cas d’intubation difficile sans difficulté de ventilation associées.
■ Le masque laryngé d’intubation Fastrach® est le dispositif de ventilation le plus utile en situation d’urgence.
■ Les vidéolaryngoscopes ne sont pas encore validées pour la prise en charge de l’intubation difficile en situation d’urgence.
■ Les dispositifs de cricothyroïdotomiee basée sur la technique de Seldinger sont à privilégier en situation d’urgence
| Tags : airway, intubation