15/09/2018
Coniotomie: Ne pas endommager le mandrin
Front-of-neck access and bougie trapping

| Tags : airway, coniotomie
18/03/2018
Control Cric: Pas mieux que la conio chirurgicale
A randomized cross-over study comparing surgical cricothyrotomy techniques by combat medics using a synthetic cadaver model
Cricothyrotomy is a complex procedure with a high rate of complications including failure to cannulate and injury to adjacent anatomy. The Control-Cric™ System and QuickTrach II™ represent two novel devices designed to optimize success and minimize complications with this procedure. This study compares these two devices against a standard open surgical technique.
METHODS:
We conducted a randomized crossover study of United States Army combat medics using a synthetic cadaver model. Participants performed a surgical cricothyrotomy using the standard open surgical technique, Control-Cric™ System, and QuickTrach II™ device in a random order. The primary outcome was time to successful cannulation. The secondary outcome was first-attempt success. We also surveyed participants after performing the procedures as to their preferences.
RESULTS:
Of 70 enrolled subjects, 65 completed all study procedures. Of those that successfully cannulated, the mean times to cannulation were comparable for all three methods: standard 51.0s (95% CI 45.2-56.8), QuickTrach II™ 39.8s (95% CI 31.4-48.2) and the Cric-Control™ 53.6 (95% CI 45.7-61.4). Cannulation failure rates were not significantly different: standard 6.2%, QuickTrach II™ 13.9%, Cric-Control™ 18.5% (p=0.106). First pass success rates were also similar (93.4%, 91.1%, 88.7%, respectively, p=0.670). Of respondents completing the post-study survey, a majority (52.3%) preferred the QuickTrach II™ device.
CONCLUSIONS:
We identified no significant differences between the three cricothyrotomy techniques with regards to time to successful cannulation or first-pass success.
| Tags : airway
11/02/2018
Airway: Prévention des complications
| Tags : airway
23/12/2017
Cricothyrotomie sans repères de surface
| Tags : airway
15/10/2017
RFE 2017 In/Extubation en anesthésie
| Tags : intubation, coniotomie, airway
12/05/2017
Membrane Cricoïdienne: Histoire de hauteur
The height of the cricothyroid membrane on computed tomography scans in trauma patients
Nutbeam T. et Al. Anaesthesia. 2017 May 2. doi: 10.1111/anae.13905.
---------------------------------
Un travail très intéressant qui met en avant le fait que la hauteur de la membrane cricoïdienne est moindre que ce que l'on pensait, qu'elle est en fait peu dépendante des conditions d'extension du cou et qu'une canule de 6 mm n'est pas celle qui sera insérée le plus facilement.
---------------------------------
Emergency cricothyrotomy is a common feature in all difficult airway algorithms. It is the final step following a ‘can’t intubate, can’t oxygenate’ scenario. It is rarely performed and has a significant failure rate. There is variation in the reported size of the cricothyroid membrane, especially across population groups. Procedural failure may result from attempting to pass a device with too large an external diameter through the cricothyroid membrane. We aimed to determine the maximum height of the cricothyroid membrane in a UK trauma population. Electronic callipers were used to measure the maximum height of the cricothyroid membrane on 482 reformatted trauma computed tomography scans, 377 (78.2%) of which were in male patients. The mean (SD) height of the cricothyroid membrane, as independently measured by two radiologists, was 7.89 (2.21) mm and 7.88 (2.22) mm in male patients, and 6.00 (1.76) mm and 5.92 (1.71) mm in female patients. The presence of concurrent tracheal intubation or cervical spine immobilisation was found not to have a significant effect on cricothyroid membrane height.
| Device | External diameter; mm | Proportion of study population in whom the mean cricothyroid membrane height > external diameter of device |
|---|---|---|
| 6.0 mm internal diameter tracheal tube | 8.0 | 36.2% |
| 5.0 mm internal diameter tracheal tube | 6.7 | 60.5% |
| 4.0 mm internal diameter tracheal tube | 5.6 | 77.6% |
| 3.0 mm internal diameter tracheal tube | 4.2 | 93.2% |
| Shiley tracheostomy 7.5 mm internal diameter | 10.8 | 7.7% |
| Melker cricothyrotomy set | 8.2 | 34.6% |
| TracheoQuick cricothyrotomy set | 5.0 | 86.5% |
The cricothyroid membrane height in the study population was much smaller than that previously reported.Practitioners encountering patients who may require an emergency surgical airway should be aware of these data. Rescue airway equipment with variety of external diameters should be immediately available.
| Tags : airway
22/01/2017
Crico avec un opinel ? Possible
Bystander cricothyroidotomy with household devices - A fresh cadaveric feasibility study.
In various motion pictures, medical TV shows and internet chatrooms, non-medical devices were presented as tools for life-saving cricothyroidotomies. However, there is uncertainty about whether it is possible for a bystander to perform a cricothyroidotomy and maintain gas exchange using improvised household items. This study examines the ability of bystanders to carry out an emergency cricothyroidotomy in fresh human cadavers using only a pocket knife and a ballpoint pen.
MATERIALS AND METHODS:
Two commonly available pens and five different pocket knives were used. Ten participants with no or only basic anatomical knowledge had to choose one of the pens and one of the knives and were asked to perform a cricothyroidotomy as quickly as possible after a short introduction. Primary successful outcome was a correct placement of the pen barrel and was determined by the thoracic lifting in a mouth-to-pen resuscitation.
RESULTS:
Eight (80%) participants performed a successful approach to the upper airway with a thoracic lifting at the end. Five participants performed a cricothyroidotomy and three performed an unintentional tracheotomy. Injuries to muscles and cartilage were common, but no major vascular damage was seen in the post-procedural autopsy. However, mean time in the successful group was 243s.
CONCLUSION:
In this cadaveric model, bystanders with variable medical knowledge were able to establish an emergency cricothyroidotomy in 80% of the cases only using a pocketknife and a ballpoint pen. No major complications (particularly injuries of arterial blood vessels or the oesophagus) occurred. Although a pocket knife and ballpoint pen cricothyroidotomy seem a very extreme procedure for a bystander, the results of our study suggest that it is a feasible option in an extreme scenario. For a better outcome, the anatomical landmarks of the neck and the incision techniques should be taught in emergency courses.
| Tags : airway
15/01/2017
ISR: Plutôt kétamine ?
Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia.
Lyon RM et Al. Crit Care. 2015 Apr 1;19:134
-------------------------------------------
Faut-il utiliser la kétamine ou l'étomidate ? Le travail présenté milite pour l'emploi de la kétamine, mais ceci reste controversé (voir également ici)). C'est aussi le choix présenté dans la procédure du sauvetage au combat, du fait de la polyvalence d'emploi de la kétamine tant dans ses indications que de ses voies d'administration. On rappelle quand même que si l'ISR facilite grandement les conditions de l'intubation oro-trachéale en médecine préhospitalière métropolitaine, nos conditions spécifiques d'exercice ne correspondent pas à cette dernière. Avant de réaliser une telle induction, encore faut-il être valider l'indication de l'intubation au milieu de nulle part. Par ailleurs la réalisation de ce geste sous anesthésie locale doit également être envisagée. Ceci est conforme aux recommandations sur le sujet.
-------------------------------------------
INTRODUCTION:
Rapid Sequence Induction of anaesthesia (RSI) is the recommended method to facilitate emergency tracheal intubation in trauma patients. In emergency situations, a simple and standardised RSI protocol may improve the safety and effectiveness of the procedure. A crucial component of developing a standardised protocol is the selection of induction agents. The aim of this study is to compare the safety and effectiveness of a traditional RSI protocol using etomidate and suxamethonium with a modified RSI protocol using fentanyl, ketamine and rocuronium.
METHODS:
We performed a comparative cohort study of major trauma patients undergoing pre-hospital RSI by a physician-led Helicopter Emergency Medical Service. Group 1 underwent RSI using etomidate and suxamethonium and Group 2 underwent RSI using fentanyl, ketamine and rocuronium. Apart from the induction agents, the RSI protocol was identical in both groups. Outcomes measured included laryngoscopy view, intubation success, haemodynamic response to laryngoscopy and tracheal intubation, and mortality.
RESULTS:
Compared to Group 1 (n = 116), Group 2 RSI (n = 145) produced significantly better laryngoscopy views (p = 0.013) and resulted in significantly higher first-pass intubation success (95% versus 100%; p = 0.007). A hypertensive response to laryngoscopy and tracheal intubation was less frequent following Group 2 RSI (79% versus 37%; p < 0.0001). A hypotensive response was uncommon in both groups (1% versus 6%; p = 0.05). Only one patient in each group developed true hypotension (SBP < 90 mmHg) on induction.
CONCLUSIONS:
In a comparative, cohort study, pre-hospital RSI using fentanyl, ketamine and rocuronium produced superior intubating conditions and a more favourable haemodynamic response to laryngoscopy and tracheal intubation. An RSI protocol using fixed ratios of these agents delivers effective pre-hospital trauma anaesthesia.
25/10/2016
Coniotomie chirurgicale: Spécialiste ? Non, mais formé spécifiquement OUI
The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective.
BACKGROUND:
The insertion of a surgical airway in the presence of severe airway compromise is an uncommon occurrence in everyday civilian practice. In conflict, the requirement for insertion of a surgical airway is more common. Recent military operations in Afghanistan resulted in large numbers of severely injured patients, and a significant proportion required definitive airway management through the insertion of a surgical airway.
OBJECTIVE:
To examine the procedural success and survival rate to discharge from a military hospital over an 8-year period.
METHODS:
A retrospective database and chart review was conducted, using the UK Joint Theatre Trauma Registry and the Central Health Records Library. Patients who underwent surgical airway insertion by UK medical personnel from 2006 to 2014 were included. Procedural success, demographics, Injury Severity Score, practitioner experience and patient survival data were collected. Descriptive statistics were used for data comparison, and statistical significance was defined as p<0.05.
RESULTS:
86 patients met the inclusion criterion and were included in the final analysis. The mean patient age was 25 years, (SD 5), with a median ISS of 62.5 (IQR 42). 79 (92%) of all surgical airways were successfully inserted. 7 (8%) were either inserted incorrectly or failed to perform adequately. 80 (93%) of these procedures were performed either by combat medical technicians or General Duties Medical Officers (GDMOs) at the point of wounding or Role 1. 6 (7%) were performed by the Medical Emergency Response Team. 21 (24%) patients survived to hospital discharge.
DISCUSSION:
Surgical airways can be successfully performed in the most hostile of environments with high success rates by combat medical technicians and GDMOs. These results compare favourably with US military data published from the same conflict.
| Tags : airway, coniotomie
13/10/2016
Gestion des voies aériennes: S'améliorer est une priorité
A national survey of practical airway training in UK anaesthetic departments. Time for a national policy?
National Audit Project (NAP4) recommended airway training for trainee and trained anaesthetists. As the skills required for management of airway emergencies differ from routine skills and these events are rare, practical training is likely to require training workshops. In 2013, we surveyed all UK National Health Service hospitals to examine the current practices regarding airway training workshops. We received responses from 206 hospitals (62%) covering all regions. Regarding airway workshops, 16% provide none and 51% only for trainees. Of those providing workshops, more than half are run less than annually. Workshop content varies widely, with several Difficult Airway Society (DAS) guideline techniques not taught or only infrequently. Reported barriers to training include lack of time and departmental or individual interest. Workshop-based airway training is variable in provision, frequency and content, and is often not prioritised by departments or individual trainers.

It could be useful if guidance on workshop organisation, frequency and content was considered nationally.
| Tags : airway
05/10/2016
Conio: Apprendre 1 h, mieux que rien mais pas assez
Self-directed simulation-based training of emergency cricothyroidotomy: a route to lifesaving skills.
| Tags : airway
04/10/2016
Conio: Et encore pour la technique chirurgicale
Surgicric 2: A comparative bench study with two established emergency cricothyroidotomy techniques in a porcine model.
BACKGROUND:
'Can't Intubate, Can't Oxygenate' is a rare but life threatening event. Anaesthetists must be trained and have appropriate equipment available for this. The ideal equipment is a topic of ongoing debate. To date cricothyroidotomy training for anaesthetists has concentrated on cannula techniques. However cases reported to the NAP4 audit illustrated that they were associated with a high failure rate. A recent editorial by Kristensen and colleagues suggested all anaesthetists must master a surgical technique. The surgical technique for cricothyroidotomy has been endorsed as the primary technique by the recent Difficult Airway Society 2015 guidelines.
METHODS:
We conducted a bench study comparing the updated Surgicric 2 device with a scalpel-bougie-tube surgical technique, and the Melker seldinger technique, using a porcine model. Twenty six senior anaesthetists (ST5+) participated. The primary outcome was insertion time. Secondary outcomes included success rate, ease of use, device preference and tracheal trauma.
RESULTS:
There was a significant difference (P<0.001) in the overall comparisons of the insertion times. The surgical technique had the fastest median time of 62 s. The surgical and Surgicric techniques were significantly faster to perform than the Melker (both P<0.001). The surgical technique had a success rate of 85% at first attempt, and 100% within two attempts, whereas the others had failed attempts. The surgical technique was ranked first by 50% participants and had the lowest grade of posterior tracheal wall trauma, significantly less than the Surgicric 2 (P=0.002).
CONCLUSIONS:
This study supports training in and the use of surgical cricothyroidotomy by anaesthetists.
| Tags : airway
24/09/2016
Crico: Mais que fait-on ?
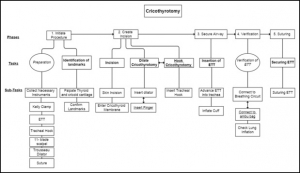
A hierarchical task analysis of cricothyroidotomy procedure for a virtual airway skills trainer simulator
Demirel D. et Al. Am J Surg. 2016 Sep;212(3):475-84
BACKGROUND:
Despite the critical importance of cricothyroidotomy (CCT) for patient in extremis, clinical experience with CCT is infrequent, and current training tools are inadequate. The long-term goal is to develop a virtual airway skills trainer that requires a thorough task analysis to determine the critical procedural steps, learning metrics, and parameters for assessment.
METHODS:
Hierarchical task analysis is performed to describe major tasks and subtasks for CCT. A rubric for performance scoring for each taskwas derived, and possible operative errors were identified.
RESULTS:
Time series analyses for 7 CCT videos were performed with 3 different observers. According to Pearson's correlation tests, 3 of the 7 major tasks had a strong correlation between their task times and performance scores.
CONCLUSIONS:
The task analysis forms the core of a proposed virtual CCT simulator, and highlights links between performance time and accuracy when teaching individual surgical steps of the procedure.
| Tags : airway
07/09/2016
Airway: S'y pencher avec sérieux
Emergency airway management – by whom and how ?
Sollid SJ et Al. Acta Anaesthesiol Scand. 2016 Oct;60(9):1185-7
---------------------------------------
Encore une publication qui insiste sur la formation à la gestion des voies aériennes et au maintien de ses compétences. Ceci n'est pas innée et s'impose tout d'abord non seulement aux praticiens peu confrontés à cette exercice, en première ligne les médecins urgentistes, mais aussi aux médecins anesthésistes compte tenu de l'essor de l'anesthésie loco-régionale et l'emploi de dispositifs supra-glottique. A lire et relire, ainsi que les références.
---------------------------------------
Procedures for advanced airway management are important for maintaining basic life functions in the unconscious patient, and can be lifesaving in critically ill or injured patients. In Acta Anaesthesiologica Scandinavica, a working group from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (SSAI) presents updated clinical guidelines on pre-hospital airway management.[1] The recommendations from the working group are important statements in the long-lasting quest to ensure that advanced airway management is managed safely pre-hospital at the right level of competence.
Technically, many of the procedures for advanced airway management of the average patient in controlled situations are easy to learn. Yet, a German study found that at least 200 intubation attempts were required to reach a 95% success rate.[2] The challenge, however, lies in assessing and managing the difficult airway cases. Emergency physicians with anaesthesiology background seem to be better at predicting difficult intubations than emergency physicians with other backgrounds, in addition to having significantly lower incidence of intubation problems and more experience in decisions on whether to intubate.[3]
Data from the UK show that the majority of complications in airway management occur in the emergency department and the intensive care unit. One of the reasons is the relatively low exposure to such procedures in these settings.[4] Studies on pre-hospital airway management also indicate that the rate of complications in this setting is high, and also that it is greatly dependent on the competence of the provider.[5] There is sufficient evidence to support that pre-hospital advanced airway management in the hands of trained anaesthesiologists is a safe procedure.[6-8] However, as other authors have pointed out, being a proficient provider of airway management is not equivalent with being an anaesthesiologist.[9] The combination of competencies to assess the situation, practical skills and ability to manage complications are more important than the name of the provider's speciality. In a physician-staffed helicopter emergency medical service in the UK, where doctors are a mix of anaesthesiologists and emergency physicians, the success rates are still high and complications are low.[10] This is probably related to the strict training and highly standardised operating procedures that all doctors must adhere to.
Based on this, advanced airway management seems to be safe if the providers have a large volume of clinical experience (anaesthesiologists) or alternatively, operate under strict clinical guidance and protocol rule (non-anaesthesiologists). Intuitively, a combination of both could probably improve safety further and would be useful in clinical environments, and particularly when airway management occurs as unplanned events with little or no time for individual planning and screening of the patient.
The most recent consensus-based European Guidelines for Postgraduate Training in Anaesthesiology recommend the change from duration of training and number of procedures into competence-based training.[11] These competences include advanced airway management skills. Some of this training can be done in simulation settings, but simulation cannot replace real-life situations.[12, 13] Once learnt, competences must be maintained. That requires regular exposure to the procedure. As the use of laryngeal masks and regional blocks increases at the expense of anaesthesia procedures including endotracheal intubation, the training opportunities for all providers, including anaesthesia personnel is being reduced. That is one of the reasons why the Section and Board of Anaesthesiology of the European Union of Medical Specialists recommended a multispecialty approach to emergency medicine.[14] Like the Scandinavian Society of Anaesthesiology and Intensive Care recommended in 2010,[15] the European Society of Anaesthesiology is increasingly using the term ‘Critical Emergency Medicine’ for the part of the anaesthesiology speciality that all anaesthesiologists should command.
A Nordic working group published a literature review in 2008 on pre-hospital airway management, and proposed an evidence-based guideline.[16] This position paper concludes unanimously that pre-hospital emergency airway management in the appropriate patient groups should be achieved by rapid sequence induction and endotracheal intubation, provided the physician is an anaesthesiologist. Other providers should treat the same patient group in the lateral trauma recovery position and if necessary, provide assisted bag-valve-mask ventilation. Supraglottic airway devices were recommended for non-anaesthesiologists in cardiac arrest with a need for supine positioning of the patient, and as a backup device for anaesthesiologists. These findings have been reaffirmed in the new SSAI clinical practice guideline published in August issue.[1]
A similar paper concerning Scandinavian clinical practice guidelines on general anaesthesia for emergency situations underlines the dangers associated with administering anaesthesia outside the operating theatre. They too advocate that anaesthesia for emergency patients should be given by, or under very close supervision by, experienced anaesthesiologists, and stress that problems with the airway are to be anticipated.[17]
Emergency airway management outside the operating theatres carries a high risk of difficult intubation, in a recent study 10.3%, and these patients have a high risk of complications.[18] This demonstrate the need for particular vigilance in and training for these settings, and provides another argument for using supraglottic approaches for those patients in the hands of non-anaesthesiologists. A recent report from the Johns Hopkins Hospital describes a successful attempt to mitigate difficult airway situations arising within this highly specialised hospital. By the formation of a difficult airway response team, the researchers conquered difficult airway situations which until the intervention ranked among the top five adverse events in Maryland.[19]
In conclusion, emergency airway management carries a high risk of patient injury, even among highly trained and skilled anaesthesiologists. Airway management can be learned, and emergency airway handling can be performed with maintained safety also by non-anaesthesiologists, provided they operate in a highly supervised and algorithm-based environment.[9] In this light, the emerging new emergency medical specialty in the Scandinavian countries is of concern, if these acute or emergency physicians are supposed to perform emergency airway procedures independent of their anaesthesiologist colleagues. Whoever manages the compromised airway in the pre-hospital setting is required to do so with the highest level of quality, attainable through a combination of clinical experience and clinical governance. It is difficult to see how this can be achieved and maintained outside the specialty of anaesthesiology. In the end, this is a matter of patient safety, not competition for airways.
| Tags : airway
01/09/2016
Pensez, efficace et peu couteux
Cognitive skills analysis, kinesiology, and mental imagery in the acquisition of surgical skills
Bathalon S. et Al. J Otolaryngol. 2005 Oct;34(5):328-32.
--------------------------------------------
Un moyen simple pour améliorer sa performance
--------------------------------------------
GOAL:
Isolate and evaluate the impact of mental imagery on the acquisition of an emergency surgical technique.
METHOD:
We studied 44 first-year medical students performing a cricothyrotomy on a mannequin to determine the impact of teaching usingmental imagery (MI) and/or kinesiology (KG) compared to the standard Advandec Trauma Life Support (ATLS) approach. Students were randomly assigned to one of three groups: MI and KG, KG alone or control (ATLS). Two weeks after the one-hour teaching session, they were evaluated with an OSCE testing the performance of the different steps of the technique, the time required and its fluidity.
RESULTS:
Total results (maximum: 25 marks) are as follows: KG + MI = 20.3 +/- 1.5 ; KG = 19.3 +/- 2.9 ; ATLS = 18.2 +/- 2.5. The only statistically significant difference for total results was in the use of MI and KG compared to the control group. Kinesiology alone or with mental imageryimproved the fluidity of the performance.
CONCLUSION:
Many factors influence the acquisition of a surgical technique. This study showed that acquisition and performance of an emergency procedure (cricothyrotomy) was improved when mental imagery and kinesiology were combined to teach it.
31/08/2016
Echo et voies aériennes: Mais oui, à maîtriser
The Role of Airway and Endobronchial Ultrasound in Perioperative Medicine
Vortrua J et Al. Biomed Res Int. 2015; 2015: 754626
-------------------------------
Certainement UN APPORT IMPORTANT à la gestion des voies aériennes et de la ventilation non seulement dans les blocs opératoires mais dans les situations critiques y compris hors de l'hôpital.
-------------------------------
Recent years have witnessed an increased use of ultrasound in evaluation of the airway and the lower parts of the respiratory system. Ultrasound examination is fast and reliable and can be performed at the bedside and does not carry the risk of exposure to ionizing radiation. Apart from use in diagnostics it may also provide safe guidance for invasive and semi-invasive procedures. Ultrasound examination of the oral cavity structures, epiglottis, vocal cords, and subglottic space may help in the prediction of difficult intubation. Preoperative ultrasound may diagnose vocal cord palsy or deviation or stenosis of the trachea. Ultrasonography can also be used for confirmation of endotracheal tube, double-lumen tube, or laryngeal mask placement. This can be achieved by direct examination of the tube inside the trachea or by indirect methods evaluating lung movements. Postoperative airway ultrasound may reveal laryngeal pathology or subglottic oedema. Conventional ultrasound is a reliable real-time navigational tool for emergency cricothyrotomy or percutaneous dilational tracheostomy. Endobronchial ultrasound is a combination of bronchoscopy and ultrasonography and is used for preoperative examination of lung cancer and solitary pulmonary nodules. The method is also useful for real-time navigated biopsies of such pathological structures.
| Tags : airway
Crico avec un stylo ? NON
Bystander cricothyrotomy with ballpoint pen: a fresh cadaveric feasibility study
Kisser U. et Al. Emerg Med J. 2016 Aug;33(8):553-6.
OBJECTIVE:
In motion pictures and anecdotal reports, ballpoint pens have been used for life-saving cricothyroidotomies. The objective of this study was to examine the widespread belief that ballpoint pens can perforate the skin and cricothyroid ligament and could be used as substitute tracheostomy sets in an emergency setting.
METHODS:
Three different ballpoint pens were examined regarding their inner diameter, their demountability to form a cannula and their airflow properties. Ten medical laypersons were asked to try to puncture the trachea through the skin and the cricothyroid ligament in 10 fresh cadavers just using the ballpoint pens.
RESULTS:
Two of three pens had inner diameters of >3 mm and were both suitable as cannulas in a tracheotomy. All participants could perforate the skin with both ballpoint pens. However, almost no one could penetrate through the cricothyroid ligament or the ventral wall of the trachea, except for one participant. He performed the tracheostomy after three attempts in >5 min with a lot of patience and force.
CONCLUSIONS:
A cricothyroidotomy just with a ballpoint pen is virtually impossible. First, the airflow resistance in commercially available ballpoint pens is too high to produce effective ventilation. Second, the cricothyroid ligament is too strong to be penetrated by ballpoint pens.
| Tags : airway
30/08/2016
Crico et Echo: Pensez TACA
Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact
Kristensen MS et Al. Br. J. Anaesth. (2016) 117 (suppl 1):i39-i48
Inability to identify the cricothyroid membrane by inspection and palpation contributes substantially to the high failure rate of cricothyrotomy. This narrative review summarizes the current evidence for application of airway ultrasonography for identification of the cricothyroid membrane compared with the clinical techniques. We identified the best-documented techniques for bedside use, their success rates, and the necessary training for airway-ultrasound-naïve clinicians.

After a short but structured training, the cricothyroid membrane can be identified using ultrasound in difficult patients by previously airway-ultrasound naïve anaesthetists with double the success rate of palpation. Based on the literature, we recommend identifying the cricothyroid membrane before induction of anaesthesia in all patients. Although inspection and palpation may suffice in most patients, the remaining patients will need ultrasonographic identification; a service that we should aim at making available in all locations where anaesthesia is undertaken and where patients with difficult airways could be encountered.
| Tags : airway
Crico: Maintenir son savoir, pas gagné !
Out-of-Hospital Surgical Airway Management: Does Scope of Practice Equal Actual Practice?
Furin M. et Al. West J Emerg Med. 2016 May;17(3):372-6
------------------------------
La coniotomie est un geste dont la réalisation est rare. Il existe actuellement un regain d'intérêt pour la maîtrise de cette pratique. Encore faut il avoir la démarche d'entretenir ses pratiques. On part de loin, c'est ce que met en valeur ce travail.
------------------------------
INTRODUCTION:
Pennsylvania, among other states, includes surgical airway management, or cricothyrotomy, within the paramedic scope of practice. However, there is scant literature that evaluates paramedic perception of clinical competency in cricothyrotomy. The goal of this project is to assess clinical exposure, education and self-perceived competency of ground paramedics in cricothyrotomy.
METHODS:
Eighty-six paramedics employed by four ground emergency medical services agencies completed a 22-question written survey that assessed surgical airway attempts, training, skills verification, and perceptions about procedural competency. Descriptive statistics were used to evaluate responses.
RESULTS:
Only 20% (17/86, 95% CI [11-28%]) of paramedics had attempted cricothyrotomy, most (13/17 or 76%, 95% CI [53-90%]) of whom had greater than 10 years experience. Most subjects (63/86 or 73%, 95% CI [64-82%]) did not reply that they are well-trained to perform cricothyrotomy and less than half (34/86 or 40%, 95% CI [30-50%]) felt they could correctly perform cricothyrotomy on their first attempt. Among subjects with five or more years of experience, 39/70 (56%, 95% CI [44-68%]) reported 0-1 hours per year of practical cricothyrotomy training within the last five years.

How much and what type of training have you had in prehospital cricothyrotomy in the past 1 year and the past 5 years?
Half of the subjects who were able to recall (40/80, 50% 95% CI [39-61%]) reported having proficiency verification for cricothyrotomy within the past five years.
CONCLUSION:
Paramedics surveyed indicated that cricothyrotomy is rarely performed, even among those with years of experience. Many paramedics felt that their training in this area is inadequate and did not feel confident to perform the procedure. Further study to determine whether to modify paramedic scope of practice and/or to develop improved educational and testing methods is warranted.
| Tags : airway
23/07/2016
Moins d'expérience ? Alors la conio chirurgicale
Emergency Cricothyrotomy Performed by Surgical Airway–naive Medical Personnel
Heymans F. et Al. Anesthesiology 2016; 125:295-303
BACKGROUND:
When conventional approaches to obtain effective ventilation and return of effective spontaneous breathing fail, surgical airway is the last rescue option. Most physicians have a limited lifetime experience with cricothyrotomy, and it is unclear what method should be taught for this lifesaving procedure. The aim of this study is to compare the performance of medical personnel, naive to surgical airway techniques, in establishing an emergency surgical airway in cadavers using three commonly used cricothyrotomy techniques.
METHODS:
Twenty medical students, without previous knowledge of surgical airway techniques, were randomly selected from their class. After training, they performed cricothyrotomy by three techniques (surgical, Melker, and QuickTrach II) in a random order on 60 cadavers with comparable biometrics. The time to complete the procedure, rate of success, and number of complications were recorded. A success was defined as the correct placement of the cannula within the trachea in 3 min.
RESULTS:
The success rates were 95, 55, and 50% for surgical cricothyrotomy, QuickTrach, and Melker, respectively (P = 0.025). The majority of failures were due to cannula misplacement (15 of 20). In successful procedures, the mean procedure time was 94 ± 35 s in the surgical group, 77 ± 34 in the QuickTrach II group, and 149 ± 24 in the Melker group (P < 0.001). Few significant complications were found in successful procedures. No cadaver biometric parameters were correlated with success of the procedure.
| Surgical Technique | QuickTrach II | Melker | ||
| Success rate (%)) ) | 19 (95 | 11 (55) | 10 (50 | 0.025 |
| Failure due to time limitation (%) | 0 | 1 (5) | 4 (20) | 0.203 |
| Incorrect placement (%) | 1 (5) | 8 (40) ) | 6 (30) | 0.106 |
| Cricothyrotomy time over 3 min | 0 | 3 | 6 | 0.257 |
| Time to complete the procedure—mean (s) | 94±35 | 149±24 | < 0.001 | |
| Total complications in successful procedures | 1 | 4 | 1 | 0.018 |
| SPC: posterior tracheal wall lesion | 1 | 3 | 1 | |
| SPC: esophageal perforation 1 | 10 (50 | |||
| Total complications in failed procedures | 1 | 8 | 6 | 0.205 |
| FPC: esophageal intubation | 1 | 2 | 1 | |
| FPC: pretracheal false passage | 4 | 3 | ||
| FPC: cannula in pharynx 1 2 | 1 | 2 | ||
| FPC: broken device 1 | 1 | |||
| FPC = failed procedure complications; SPC = successful procedure complications. |
"....In conclusion, our results indicate that medical personnel naive to surgical airway techniques establish a surgical airway more efficiently using surgical cricothyroidotomy. Since the vast majority of clinicians perform emergency airway infrequently, our observation might apply to the majority of them. Whether surgical cricothyrotomy remains superior in advance-trained medical personnel requires further study......"
CONCLUSION:
Surgical airway-naive medical personnel establish emergency cricothyrotomy more efficiently and safely with the surgical procedure than with the other two commonly used techniques.
| Tags : airway