----------------------------------------------------------------------------------------------------------------------
29/05/2013
Vidéo laryngoscopie: Du bien, on n'est pas étonné
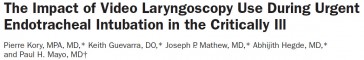
Anesth Analg 2013;XX:XX–XX
BACKGROUND:The video laryngoscope (VL) has been shown to improve laryngoscopic views and first-attempt success rates in elective operating room and simulated tracheal intubations compared with the direct laryngoscope (DL). However, there are limited data on the effectiveness of the VL compared with the DL in urgent endotracheal intubations (UEIs) in the critically ill. We assessed the effectiveness of using a VL as the primary intubating device during UEI in critically ill patients when performed by less experienced operators.
METHODS:We compared success rates of UEIs performed by Pulmonary and Critical Care Medicine (PCCM) fellows in the medical intensive care unit and medical or surgical wards. A cohort of PCCM fellows using GlideScope VL as the primary intubating device was compared with a historical cohort of PCCM fellows using a traditional Macintosh or Miller blade DL. The primary measured outcome was first-attempt intubation success rate. Secondary outcomes included total number of attempts required for successful tracheal intubation, rate of esophageal intubation, need for supervising attending intervention, duration of intubation sequence, and incidence of hypoxemia and hypotension.
RESULTS:There were 138 UEIs, with 78 using a VL and 50 using a DL as the primary intubating device. The rate of first-attempt success was superior with the VL as compared with the DL (91% vs 68%, P < 0.01). The rate of intubations requiring ≥3 attempts (4% vs 20%, P < 0.01), unintended esophageal intubations (0% vs 14%, P < 0.01), and the average number of attempts required for successful tracheal intubation (1.2 ± 0.56 vs 1.7 ± 1.1, P < 0.01) all improved significantly with use of the VL compared with the DL.
CONCLUSIONS:UEI using a VL as the primary device improved intubation success anddecreased complications compared with a DL when PCCM fellows were the primary operators. These data suggest that the VL should be used as the primary device when urgent intubations are performed by less experienced operators.
| Tags : intubation, airway
20/04/2013
Coniotomie: Avant tout de bons repères
La réalisation d'une coniotomie en conditions extrêmes n'est pas une chose si aisée que cela. Bien souvent l'opérateur peut être obnubilé par le fait de faire pénétrer un tuyau dans un trou alors que ce qui est important c'est le trou au bon endroit et de taille suffisamment large pour admettre le tuyau. Au final ce qui est FONDAMENTAL c'est donc de prendre ses repères et de vérifier le diamêtre de l'ouverture faite.
C'est ce qu'exprime ce document intéressant et très pratique dont l'un des auteurs est un des inventeurs d'une technqiue de trachéotomie percutanée.
_________________________________________
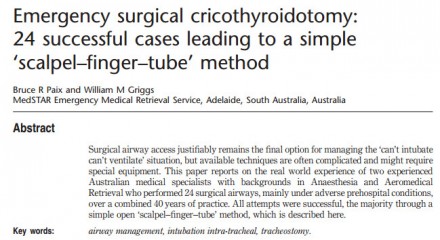
The first step of the ‘scalpel–finger–tube’ method is to stabilize the larynx with the non-dominant hand, identify the cricothyroid membrane visually and by palpation, and to incise horizontally all the way through skin and cricothyroid membrane into the laryngeal lumen in one motion (Fig. 1).
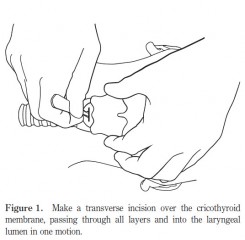
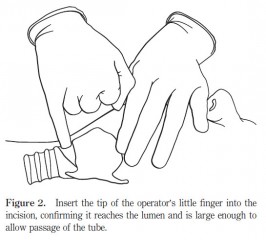
In the emergency situation, neither skin antiseptics nor local anaesthesia are used.Any suitable blade can be used, either on or off the handle. The incision is extended laterally until judgedlarge enough to accommodate the tip of the operator’s gloved little finger, that is, approximately 15 mm. The second step is to remove the scalpel and insert the tip of the operator’s little finger into the incision (Fig. 2), confirming by palpation that the incision has penetratedinto the laryngeal lumen, and that the incision is large enough to accommodate the finger, and therefore, an endotracheal tube.
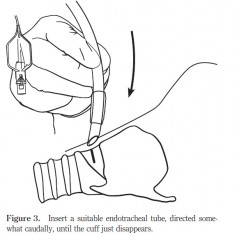
Finally, in the third step, a cuffed oral endotracheal tube is fed through the hole into the trachea, directed somewhat caudally (Fig. 3)
| Tags : airway, coniotomie
03/03/2013
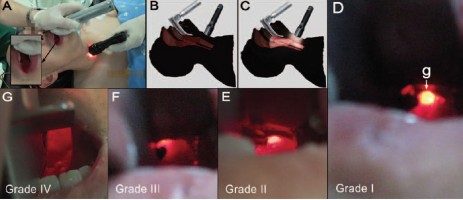
Mieux voir pour mieux intuber. Un moyen simple surtout si on débute
Retrograde Light-guided Laryngoscopy for Tracheal Intubation. Clinical Practice and Comparison with Conventional Direct Laryngoscopy
Anesthesiology 2013; 118:XXX–XXX doi: 10.1097/ALN.0b013e31828877c0.
L'intubation orotrachéale nécessite un apprentissage réel. Une cinquantaine de procédures réussies sont nécessaires pour pouvoir considérer avoir la maîtrise de ce geste. De nombreux dispositifs permettent d'augmenter le taux de réussite (bougie, stylets lumineux, dispositifs laryngés, fibroscopie, vidéolaryngoscope). Ces dernières sont cependant onéreuses et pas forcément toujours disponibles. L'illumination transtrachéale et rétrograde du plan glottique pourrait avoir une certaine utilité en améliorant la visualisation de l'orifice glottique.
--------
Compared with DL, the success rate was greater in the RLGL group for all five intubations (72% vs. 47%; rate difference, 25%; 95% CI [11.84–38.16%], P < 0.001). This was associated with a shorter time to glottic exposure (median [25th and 75th percentile]; 27 [15; 42] vs. 45 [30; 73] s, P < 0.001), shorter intubation time (66 [44; 120] vs. 120 [69; 120] s, P < 0.001), and decreased throat soreness (mean ± SD; visual analog scale, 2.1 ± 0.9 vs. 3.7 ± 1.0 cm, P = 0.001) in the RLGL group compared to the DL group.
--------
| Tags : intubation, airway
24/02/2013
Intubation: Encore une étude POUR
Comparison of Neurological Outcome between Tracheal Intubation and Supraglottic Airway Device Insertion of Out-of-hospital Cardiac Arrest Patients: A Nationwide, Population-based, Observational Study
J Emerg Med. 2013 Feb;44(2):389-97
BACKGROUND:
The effect of prehospital use of supraglottic airway devices as an alternative to tracheal intubation on long-term outcomes of patients with out-of-hospital cardiac arrest is unclear.
STUDY OBJECTIVES:
We compared the neurological outcomes of patients who underwent supraglottic airway device insertion with those who underwent tracheal intubation.
METHODS:
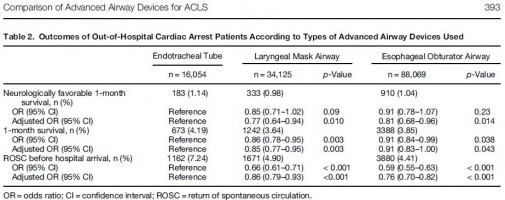
We conducted a nationwide population-based observational study using a national database containing all out-of-hospital cardiac arrest cases in Japan over a 3-year period (2005-2007). The rates of neurologically favorable 1-month survival (primary outcome) and of 1-month survival and return of spontaneous circulation before hospital arrival (secondary outcomes) were examined. Multiple logistic regression analyses were performed to adjust for potential confounders. Advanced airway devices were used in 138,248 of 318,141 patients, including an endotracheal tube (ETT) in 16,054 patients (12%), a laryngeal mask airway (LMA) in 34,125 patients (25%), and an esophageal obturator airway (EOA) in 88,069 patients (63%).
RESULTS:
The overall rate of neurologically favorable 1-month survival was 1.03% (1426/137,880). The rates of neurologically favorable 1-month survival were 1.14% (183/16,028) in the ETT group, 0.98% (333/34,059) in the LMA group, and 1.04% (910/87,793) in the EOA group. Compared with the ETT group, the rates were significantly lower in the LMA group (adjusted odds ratio 0.77, 95% confidence interval [CI] 0.64-0.94) and EOA group (adjusted odds ratio 0.81, 95% CI 0.68-0.96).
CONCLUSIONS:
Prehospital use of supraglottic airway devices was associated with slightly, but significantly, poorer neurological outcomes compared with tracheal intubation, but neurological outcomes remained poor overall.
| Tags : airway, intubation
17/11/2012
Coniotomie / Cricothyrotomie
L'accès aux voies aériennes: Plan A: liberté des voies aériennes par les manoeuvres de secourisme, la mise en place d'une guédel et l'intubation. Plan B: Je n'oublie pas que l'essentiel est de pouvoir ventiler, donc j'ai un ballon. Plan C: Si je n'arrive pas à intuber et à ventiler, je n'hésite pas à OUVRIR LE COU
| Tags : coniotomie, airway, intubation
17/07/2012
Dispositifs laryngés: Toujours pas validés !
Un retour d'expérience à méditer qui met en évidence que plus de la moitié des dispositifs laryngés posés en préhospitalier ne sont pas positionnés de manière correcte.
http://www.medicalsci.com/files/f2f__10__king_ltd_-_afmes...
Un document faisant le point sur les divers dispositifs laryngés est accessible ici
| Tags : airway
07/04/2012
Coniotomie et analyse cognitive de taches
L’analyse cognitive de tâches est une « famille de techniques de recueil de connaissances qui ont démontrées leur efficacité pour extraire les processus cognitifs, décisionnels et de jugements inobservables impliqués lors d’une performance d’expert» (Yates 2007). L’intérêt de ce groupe de techniques est de rendre accessible à la conscience l’ensemble des étapes réalisées de façon automatiques par des experts.
Cette méthode moderne d'enseignement est très certainement d'un apport capital pour l'enseignement du sauvetage au combat. Ainsi il semble qu'elle peut s'appliquer à la coniotomie. C'est du moins ce que laisse supposer l'article suivant.
The effectiveness of a cognitive task analysis informed curriculum to increase self-efficacy and improve performance for an open cricothyrotomy.
Campbell J.. et all J Surg Educ. 2011 Sep-Oct;68(5):403-7
Abstract
OBJECTIVE:
This study explored the effects of a cognitive task analysis (CTA)-informed curriculum to increase surgical skills performance and self-efficacy beliefs for medical students and postgraduate surgical residents learning how to perform an open cricothyrotomy.
METHODS:
Third-year medical students and postgraduate year 2 and 3 surgery residents were assigned randomly to either the CTA group (n = 12) or the control group (n = 14). The CTA group learned the open cricothyrotomy procedure using the CTA curriculum. The control group received the traditional curriculum.
RESULTS:
The CTA group outperformed the control group significantly based on a 19-point checklist score (CTA mean score: 17.75, standard deviation [SD] = 2.34; control mean score: 15.14, SD = 2.48; p = 0.006). The CTA group also reported significantly higher self-efficacy scores based on a 140-point self-appraisal inventory (CTA mean score: 126.10, SD = 16.90; control: 110.67, SD = 16.8; p = 0.029).
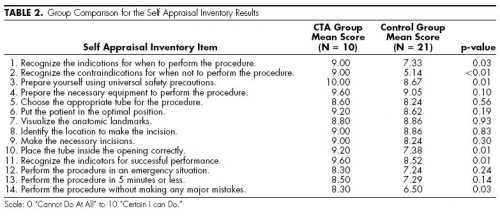
CONCLUSIONS:
The CTA curriculum was effective in increasing the performance and self-efficacy scores for postgraduate surgical residents and medical students performing an open cricothyrotomy.
| Tags : airway, coniotomie
15/02/2011
Intubation préhospitalière: Que penser de l'AIRTRAQ ?
Comme pour tout il faut s'entraîner et on n'inove pas. On rappelle que, en conditions de combat, le contrôle des voies aériennes a pour but essentiellemment de prévenir l'obstruction des voies aériennes, de prévenir l'inhalation du contenu gastrique. Le traitement d'une détresse respiratoire fait appel avant tout à l'oxygénothérapie si vous disposez d'oxygène, au traitement d'une cause spécifique (pneumo ou hémothorax, volet thoracique, plaie soufflante), à l'assistance ventilatoire au ballon par masque facial et EVENTUELLEMENT après intubation ou coniotomie sur une canule de 6 mm si les conditions tactiques le permettent.
Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: A randomized control trial
Trimmel H et all.
Crit Care Med 2011 Vol. 39, No. 3, 1-5
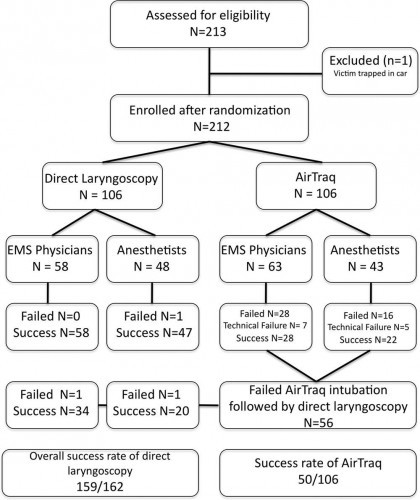
Objectives: The optical Airtraq laryngoscope (Prodol Meditec, Vizcaya, Spain) has been shown to have advantages when compared with direct laryngoscopy in difficult airway patients. Furthermore, it has been suggested that it is easy to use and handle even for inexperienced advanced life support providers. As such, we sought to assess whether the Airtraq may be a reliable alternative to conventional intubation when used in the prehospital setting.
Design, Setting, and Patients: Prospective, randomized control trial in emergency patients requiring endotracheal intubation provided by anesthesiologists or emergency physicians responding with an emergency medical service helicopter or ground unit associated with the Department of Anesthesiology, General Hospital, Wiener Neustadt, Austria.
Measurements and Main Results: During the 18-month study period, 212 patients were enrolled. When the Airtraq was used as first-line airway device (n = 106) vs. direct laryngoscopy (n =106), success rate was 47% vs. 99%, respectively (p < .001). Reasons for failed Airtraq intubation were related to the fiberoptic characteristic of this device (i.e., impaired sight due to blood and vomitus, n = 11) or to assumed handling problems (i.e., cuff damage, tube misplacement, or inappropriate visualization of the glottis, n = 24). In 54 of 56 patients where Airtraq intubation failed, direct laryngoscopy was successful on the first attempt; in the remaining two and in one additional case of failed direct laryngoscopy, the airway was finally secured employing the Fastrach laryngeal mask. There was no correlation between success rates and body mass index, age, indication for airway management, emergency medical service unit, or experience of the physicians.
Conclusions: Based on these results, the use of the Airtraq laryngoscope as a primary airway device cannot be recommended in the prehospital setting without significant clinical experience obtained in the operation room. We conclude that the clinical learning process of the Airtraq laryngoscope is much longer than reported in the anesthesia literature.
| Tags : intubation, airway
05/02/2011
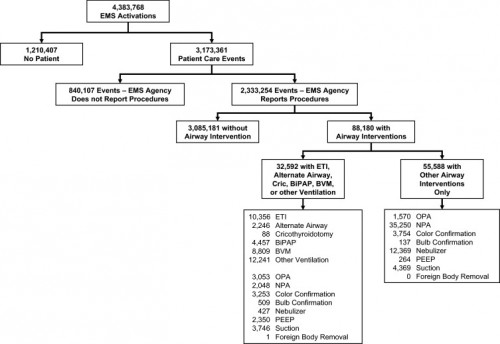
Etude NEMESIS: Out-of-hospital airway management in the United States
Un travail prospectif recensant toutes les manoeuvres de contrôle des voies aériennes aux USA vient d'être publié ( Out-of-hospital airway management in the United States - Wang HE et all. -doi:10.1016/j.resuscitation.2010.12.014). Ce document est intéressant car il confirme que l'intubation est le mode premier de contrôle de la ventilation aux USA suivi par la ventilation manuelle au ballon. Le recours à des disposiifs laryngés ne vient qu'au 4ème rang après la mise en oeuvre de technqiues de ventilation non invasive. L'apprentissage de l'intubation reste donc un objectif essentiel. Les tableaux suivant en présentent les principaux résultats.
Table 1. Prevalence of airway management interventions. Table includes only EMS agencies reporting at least one procedure in the NEMSIS 2008 data set. Percentages reflect portion of 2,333,254 total patient care events. Prevalence estimates not calculated for King LT and foreign body removal due to the small numbers of events. BiPAP = bilevel positive airway pressure. CPAP = continuous positive airway pressure. PEEP = positive end expiratory pressure.
| Intervention | N | (N per 100,000 care events; 95%CI) |
|---|---|---|
| Bag-valve-mask ventilation | 8809 | (378; 370–386) |
| Other ventilation (bag-valve, mechanical, unspecified) | 12,241 | (525; 516–534) |
| Endotracheal intubation | 10,356 | (444; 436–453) |
| Orotracheal intubation | 9130 | (392; 384–400) |
| Nasotracheal intuabtion | 1064 | (46; 43–48) |
| Rapid sequence intubation | 371 | (16; 14–18) |
| Alternate airway | 2246 | (96; 92–100) |
| Combitube | 1521 | (65; 62–69) |
| Esophageal-Obturator Airway (EOA) | 175 | (8; 6–9) |
| Laryngeal Mask Airway | 571 | (24; 23–27) |
| King LT | 4 | (Not calculated) |
| Cricothyroidotomy | 88 | (4; 3–5) |
| BiPAP/CPAP | 4456 | (191; 186–197) |
| Oropharyngeal airway | 4623 | (198; 193–204) |
| Nasopharyngeal airway | 37,298 | (160; 158–161) |
| Colorimetric tube confirmation | 7007 | (300; 294–308) |
| Bulb tube confirmation | 646 | (28; 26–30) |
| Nebulizer | 12,796 | (549; 539–558) |
| PEEP | 2614 | (112; 108–117) |
| Suction | 8115 | (348; 341–356) |
| Foreign body removal | 1 | (Not calculated) |
----------------------------------------------------------------------------------------------------------------------
Table 3. Airway intervention success. Includes only orotracheal, nasotracheal and rapid sequence intubation and alternate airway insertions where procedural success was reported. ETI success was reported for only 8418 of 10,356 ETI.
ETI = endotracheal intubation. US = United States.
a Subgroups do not add up to total because of unknown cardiac arrest status for 5244 cases. Univariable odds ratios presented for selected comparisons only.
----------------------------------------------------------------------------------------------------------------------
Abstract
-----Among 4,383,768 EMS activations, there were 10,356 ETI, 2246 alternate airways, and 88 cricothyroidotomies. ETI success rates were: overall 6482/8418 (77.0%; 95% CI: 76.1–77.9%), cardiac arrest 3494/4482 (78.0%), non-arrest medical 616/846 (72.8%), non-arrest injury 417/505 (82.6%), children <10 years 295/397 (74.3%), children 10–19 years 228/289 (78.9%), adult 5829/7552 (77.2%), and rapid-sequence intubation 289/355 (81.4%). ETI success was success was lowest in the South US census region. Alternate airway success was 1564/1794 (87.2%). Major complications included: bleeding 84 (7.0 per 1000 interventions), vomiting 80 (6.7 per 1000) and esophageal intubation 12 (1.0 per 1000).
Conclusions
In this study characterizing out-of-hospital airway management across the United States, we observed low out-of-hospital ETI success rates. These data may guide national efforts to improve the quality of out-of-hospital airway management.
| Tags : airway, intubation
31/12/2010
Intubation préhospitalière: Histoire de lame
Un article d Jabre et all décrit de manière relativement précise le quotidien de l'intubation préhospitalière
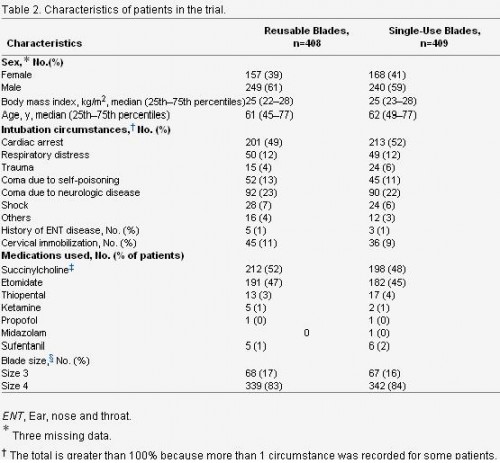
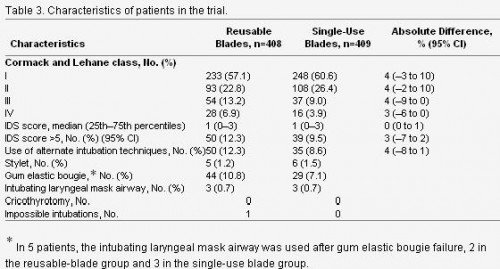
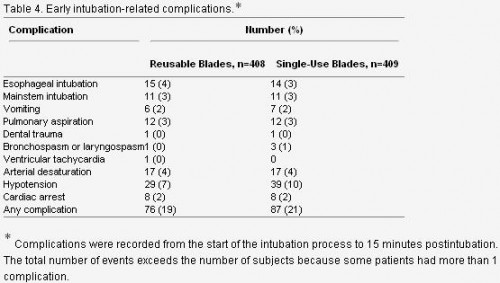
Cet article est très intéressant car il permet d'avoir une vision très claire de l'intubation telle qu'elle est réalisée en préhospitalier en France. L'objectif premier était de comparer l'intubation avec lame métallique réutilisable versus non réutilisable et de voir si il y avait une différence en matière d'intubation difficile. Ce n'est pas le cas. Parmi les autres intérêts de ce travail:
-
l'intubation préhospitalière est réalisée essentiellement lors de la prise en charge d' arrêt cardiaque ou de coma. Le contexte traumatique n'est présent que dans 4% des cas. Ce qui ne correspond pas au contexte d'emploi militaire. Le contrôle des voies aériennes ayant pour objectif essentiel le maintien de la liberté des voies aériennes, puis leur protection contre l'inhalation et enfin la possibilité de réaliser une ventilation contrôlée si les autres paramètres techniques sont accessibles (matériel, oxygène, sédation)
2. La taille de la lame utilisée est une taille 4. Le laryngoscope Truphatek Trulite en dotation est approvisionné en taille 3. Ceci a été jugé suffisant par un panel de praticiens, ce d'autant que les lames de tailles 4 sont aussi plus hautes et pas forcément toujours « insérables » dans la cavité buccale en cas de petite ouverture de bouche.
3. Le recours à des techniques alternatives est prévu, ici le masque laryngé d'intubation qui est utilisé de manière exceptionnelle moins de 1% des cas, contrairement au mandrin d'eschmann/Frova.
4. Parmi les complications immédiates, on constate la fréquence des hypotensions près de 10% et des intubations sélectives ou oesophagiennes également près de 10% des cas. Ces taux observés pour des équipes à priori entraînées illustrent bien que l'enjeu majeur de la médicalisation de l'avant dans le contexte actuel est de disposer de personnel ayant une pratique réelle de l'accès aux voies aériennes supérieures.
| Tags : intubation, airway
17/12/2010
Quel laryngoscope ?
Le choix d'un laryngoscope "tactique" n'est pas simple. C'est un compromis entre la modalité choisie de contrôle des voies aériennes (pas d'intubation, coniotomie ou intubation ?), le poids du laryngoscope, la taille de la lame et les qualités optiques attendues.
Vous dispsoez outre de la boite d'intubation standard du laryngoscope trulite de la société truphatek.

Il a été choisi d'approvionner ce laryngoscope en lame fixe de taille 3 qui semble la plus polyvalente. Ce laryngoscope est remarquable de part sa légèreté, la présence d'un manche court et la qualité de la lumière LED fournie. Il est en principe à patient unique.
Pour pallier au problème du choix de la taille de la lame, certains proposent des produits originaux. Ainsi le duoscope de la société PARKER propose deux tailles de lame et un éclairage de grande qualité. sa manipulation est moins aisée car c'est la seconde lame qui sert de manche.
| Tags : intubation, airway
14/12/2010
Abord des voies aériennes:Que font les anglais ?
10 % des blessés évacués nécessite une intubation dont 4.7% avant l'embarquement dans le vecteur d'évacuation. Dans ce travail la limite est que nous ne savons pas ce qui relève de blessés au combat , s'il s'agit de blessés militaires, de la répartition des procédures en fonction du contexte. Dans de telles conditions la prise en charge de patients/blessés en arrêt circulatoire est vaine .
J R Army Med Corps. 2010 Sep;156(3):159-61.
Advanced airway management--a medical emergency response team perspective.
Selly Oak Hospital, Birmingham. aghaldane1@doctors.org.uk
Abstract
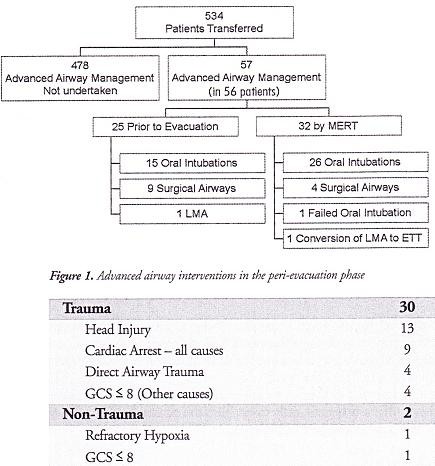
OBJECTIVES: To determine the number of medical emergency response team (MERT) patients undergoing advanced airway management in the peri-evacuation phase and to determine the indications for airway interventions undertaken in flight.
METHODS: This was a retrospective study. Data was collected from patient report and mission debrief forms completed after each MERT mission during Operation HERRICK 10 (April-October 2009). All patients that received advanced airway interventions before or during evacuation were identified.
RESULTS: MERTs were involved in the primary transfer of 534 patients during the period studied, 56 (10.5%) underwent advanced airway management, of which 31 (5.8% of total) were initiated by the MERT in the peri-evacuation phase. Twenty five cases (4.7%) underwent advanced airway management by other pre-hospital providers prior to MERT arrival. Of the 31 advanced airway interventions undertaken in-flight, cardiac arrest was the primary indication in only nine cases.
CONCLUSIONS: The figure of 56 patients requiring advanced airway management is at the higher end of the range expected from the study of historical military data. This may reflect the doctrine of "intelligent tasking", that is sending this physician-led team to the most seriously injured casualties.
Morceaux choisis
1. Intubation et coniotomie sont la base
2. Les indications diffèrent de la médecine préhospitalière civile
"..
The indications for those advanced airway interventions undertaken by the MERT is in keeping with the historical data: Head injury making the biggest group once those inrubated for post-operative resplratory support ie those transferred post-operatively from an FST location rather than direct from the point of wounding are excluded . The majoriry of the cases were trauma (93,5%) with the remaining non-traula causes (6,5%) (table 1); This figure is again similar io the recent US study [11].
.."
| Tags : airway, intubation
06/12/2010
Tube laryngé aux urgences
Clinical paper
Hichem Chenaitiaa,  ,
,  , Valéry Soulleiheta, Horace Massab, Jacques Bessereaua, Jeremy Bourennec, Pierre Micheleta and Jean-Pierre
, Valéry Soulleiheta, Horace Massab, Jacques Bessereaua, Jeremy Bourennec, Pierre Micheleta and Jean-Pierre  Auffray
Auffray a
a
Abstract
Background
Securing the airway in emergency is among the key requirements of appropriate prehospital therapy. The  Easytube
Easytube (Ezt) is a relatively new device, which combines the advantages of both an infraglottic and supraglottic airway.
(Ezt) is a relatively new device, which combines the advantages of both an infraglottic and supraglottic airway.
Aims
Our goal was to evaluate the effectiveness and the safety of use of Ezt by emergency physicians in case of difficult airway management in a prehospital setting with minimal training.
Methods
We performed a prospective multi-centre observational study of patients requiring airway management conducted in prehospital emergency medicine in France by 3 French mobile intensive care units from October 2007 to October 2008.
Results
Data were available for 239 patients who needed airway management. Two groups were individualized: the “easy airway management” group (225 patients; 94%) and the “difficult airway management” group (14 patients; 6%). All patients had a successful airway management. The Ezt was used in eight men and six women; mean age was 64 years. It was used for ventilation for a maximum of 150 min and the mean time was 65 min. It was positioned successfully at first attempt, except for two patients, one needed an adjustment because of an air leak, and in the other patient the Ezt was replaced due to complete obstruction of the Ezt during bronchial suction.
Conclusion
The present study shows that emergency physicians in cases of difficult airway management can use the EzT safely and effectively with minimal training. Because of its very high success rate in ventilation, the possibility of blind intubation, the low failure rate after a short training period. It could be introduced in new guidelines to manage difficult airway in prehospital emergency.
Article Outline
- 1.
- Introduction
- 2.
- Material and methods
- 2.1. Study design
- 2.2. Setting
- 2.3. Protocol
- 2.4. Data collection and measurements
- 3.
- Results
- 4.
- Discussion
- 5.
- Conclusion
- Appendix A.
- Supplementary data
1. Introduction
Securing the airway in emergency patients is among the key requirements of appropriate prehospital therapy. Endotracheal intubation (ETI) is currently the “gold standard” for airway management in a prehospital setting, but this is a complex technique requiring practice and experience. As failure to secure airway can increase morbidity and mortality within a very short time, and as multiple failed intubation attempts can lead to additional trauma [1], knowledge and availability of alternative procedures are essential for every emergency physician.The European Resuscitation Council Guidelines for Cardiopulmonary Resuscitation 2005 recommend that tracheal intubation should be attempted only by trained personnel with adequate ongoing experience, and in cases of failure to intubate the trachea using an endotracheal tube (ETT), the Combitube is an acceptable alternative [2].
The  Easytube
Easytube (Ezt, Teleflex Medical Ruesch) is a 0relatively new device (Fig. 1). It is a sterile, disposable airway device, approved by the European Union in 2003 and by the U.S. Food and Drug Administration in 2005. The Ezt is a two-lumen tube with a pharyngeal proximal cuff and a distal cuff. One lumen of the Ezt opens at the distal end and the other lumen serves as a supraglottic ventilation aperture between the two cuffs. It is latex free and available in two sizes to be used in patients with a height of 90–130 cm (size 28 Fr [French]) or over 130 cm (size 41 Fr). The distal end of the Ezt is designed like a standard ETT with a tip diameter of 7.5 mm (size 41 Fr) or 5.5 mm (size 28 Fr). It includes a Murphy eye at its tip. The design of the pharyngeal aperture allows insertion of a flexible fiberoptic bronchoscope, bougie or suction catheter with a maximum external diameter of 3.9 mm into the trachea.
(Ezt, Teleflex Medical Ruesch) is a 0relatively new device (Fig. 1). It is a sterile, disposable airway device, approved by the European Union in 2003 and by the U.S. Food and Drug Administration in 2005. The Ezt is a two-lumen tube with a pharyngeal proximal cuff and a distal cuff. One lumen of the Ezt opens at the distal end and the other lumen serves as a supraglottic ventilation aperture between the two cuffs. It is latex free and available in two sizes to be used in patients with a height of 90–130 cm (size 28 Fr [French]) or over 130 cm (size 41 Fr). The distal end of the Ezt is designed like a standard ETT with a tip diameter of 7.5 mm (size 41 Fr) or 5.5 mm (size 28 Fr). It includes a Murphy eye at its tip. The design of the pharyngeal aperture allows insertion of a flexible fiberoptic bronchoscope, bougie or suction catheter with a maximum external diameter of 3.9 mm into the trachea.
| Full-size image (26K) |
It is fairly similar to the Combitube. Both the Combitube and the Ezt can be used as infraglottic or supraglottic airways. They enable sufficient ventilation whether they are inserted into the oesophagus or the trachea [3], [4]and [5]. The Ezt was developed for in-hospital and out-of-hospital use in all patients with anticipated or unanticipated airway difficulties [1], [2], [3], [4] and [5].
The French prehospital Emergency Medical System (EMS) is based on a national phone number (15 or 112). A physician screens each call. In cases of vital distress, a mobile intensive care unit (MICU) consisting of an emergency physician, a nurse and an ambulance driver is sent to the scene within minutes.
The aim of this study was to evaluate the effectiveness and the safety of use of Ezt by emergency physicians in case of difficult airway management in a prehospital setting with minimal training.
2. Material and methods
2.1. Study design
This study was a prospective multi-centre study of patients requiring airway management conducted in a French prehospital EMS (SAMU 13) in the city of Marseille, by 3 French MICUs over a 12-month period.
The primary outcome measurement was airway management success. Our hypothesis was that emergency physicians would be able to successfully perform prehospital airway management using the Ezt in cases of difficult airway management with minimal training.
2.2. Setting
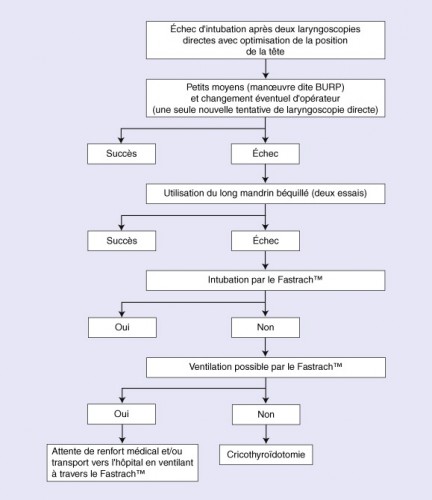
In order to evaluate the Ezt, all emergency physicians used the same algorithm for airway management (Fig. 2). It included 3 MICUs distributed in different parts of the city.
| Full-size image (23K) |
Emergency physicians were trained in the use of Ezt on manikins. Ten consecutive successful intubations were required for every physician before beginning the evaluation of Ezt.
The inclusion criteria were: all the patients with a height above 90 cm and an indication for prehospital airway management.
The exclusion criteria were a contraindication to the use of Ezt: patients with a height less than 90 cm, patients suffering from upper airway obstruction, and patients suffering from oesophageal diseases or ingestion of caustic substances.
2.3. Protocol
During the study period, all patients were managed with the same airway management protocol (Fig. 2). Our protocol complies with the guidelines of the French Society of Anaesthesia and Resuscitation (SFAR) and received ethical approval from Marseille University Hospital's Emergency Committee.
The SFAR defines difficult intubation (DI) as more than two failed intubation attempts under direct laryngoscopy with an optimal head position.
We prospectively separated patients into 2 groups: “easy airway management”: less than 2 ETI attempts and “difficult airway management”: more than 2 ETI attempts or use of EZT in accordance with the protocol.
In our study, before ETI we also systematically evaluate predictive signs of DI (short neck, restricted mouthopening <3 cm, estimated thyromental distance <6 cm, morbid obesity with body mass index estimated more than 40 and cervico-facial trauma).
For a patient with vital distress on arrival of the prehospital medical team on-site and after evaluation of the situation, the emergency physician decides if intubation is necessary.
The patients were preoxygenated by Bag–Valve–Mask (BVM) with 100% oxygen for 3 min, except in the case of cardio-respiratory arrest or if there was an immediate indication of intubation.
During airway management, patients were monitored continuously by electrocardiogram, cutaneous pulse oximetry and non-invasive arterial pressure.
A Rapid Sequence Induction (RSI) with etomidate (0.3 mg/kg) and succinylcholine (1 mg/kg) was performed in patients with cardiac activity. Arrest patients were intubated without giving any medications.
If there was no predictive sign of DI, ETI was attempted with an ETT and by a direct laryngoscopy, with or without a stylet.
Whatever the attempted airway management, this is always limited to 40 s.
If ETI failed, ventilation by BVM with 100% oxygen was resumed, or in the event of a predictive sign of DI, an attempt at ETI was recommended but with measures taken to facilitate intubation: place the head in the modified Jackson position or “sniffing position”, if no cervico-facial trauma, bend the tube into a “hockey stick” shape with a stylet and have an assistant perform the BURP (backward upward rightward pressure) maneuver to move the larynx closer to the visual axis for intubation.
If ETI failed again, ventilation by BVM with 100% oxygen was resumed and a further attempt with Ezt was recommended, respecting any contraindications.
If a “cannot intubate, cannot ventilate” situation occurred and as no time could be wasted in further intubation attempts, immediate use of Ezt was allowed because the Combitube and the Ezt are listed as a rescue method in “cannot ventilate–cannot intubate” situations by the American Society of Anaesthesiologists [6].
Laryngoscopic insertion of Ezt is very similar to the use of a standard ETT, and if an ETI by Ezt is finally possible, the patient is ventilated through the transparent lumen.
If ETI is not possible, the tip of the EzT can be inserted into the esophagus under visual guidance with the help of a laryngoscope or blindly.
If it is inserted blindly, the patient's head must be in neutral position. Manually opening the patient's mouthand pressing the tongue gently toward the mandible, the tube is inserted parallel to the frontal axis of the patient until the proximal black ring mark is positioned at the level of the incisors. If the EzT is inserted blindly, the tip is likely to be positioned in the esophagus with a probability of more than 95% [3]. Ventilation of the patient should be performed using a colored lumen, and the transparent lumen can then be used to insert a gastric tube or to drain gastric contents.
The colored pharyngeal proximal cuff and the transparent distal cuff are subsequently inflated with 80 and 10 ml of air, using two pre-filled syringes in the package. Inflation of the pharyngeal cuff occludes theoropharynx and should prevent inhalation of blood or secretions from the oral or nasal cavity. The transparentdistal cuff seals the oesophagus and should prevent inhalation of gastric contents.
Correct insertion of Ezt was defined as efficient ventilation of the patient assessed by three square-wave capnograph traces during manual ventilation, symmetric auscultation with no audible gastric insufflations or air leak.
If all of these methods failed, ventilation by BVM with 100% oxygen was resumed and a “Failed Airway Algorithm” was applied to the patients by performing a cricothyrotomy with the “Quick-Trach Emergency Cricothyrotomy Device.”
After airway management, anaesthesia was maintained with Midazolam (0.1 mg/kg/h) and Fentanyl(1 μg/kg/h). The patients underwent positive pressure ventilation in a pressure-controlled mode; the limit was set at 30 cm H2O airway pressure; the targeted tidal volume was 7 mL/kg; inspired oxygen concentration (FIO2) at 1; respiratory rate was set to achieve an End-Tidal CO2 (ETCO2) concentration of 35–45 mmHg. The patients were continuously monitored by standard non-invasive measures including electrocardiogram, cutaneous pulse oximetry, non-invasive blood pressure measurement (every 5 min) and capnography.
Subsequently, the patients were rapidly admitted to intensive care unit (ICU). The Ezt was replaced by an ETT in ICU, with an airway exchange catheter as soon as possible.
2.4. Data collection and measurements
The emergency physicians filled the study forms immediately after each airway management. The study form included patient's age and sex, Glasgow coma scale (GCS) score, approximate height (less or more than 130 cm), clinical status and indication for intubation (cardio-respiratory arrest, severe neurological distress, severe respiratory distress or other). The forms were anonymous. Predictive signs of DI (short neck, restricted mouth opening <3 cm, estimated thyromental distance <6 cm, morbid obesity and cervico-facialtrauma) and number of intubation attempts were also noted. Incidents and complications of intubation were reported by means of open-ended questions. All the data were then managed in a computer database.
3. Results
During the study period, 239 patients needed prehospital airway management and no patient was excluded.
These 239 patients were divided into 2 groups: 225 (94%) patients in “easy airway management” and 14 (6%) patients in “difficult airway management”. The characteristics for both groups are illustrated in Table 1.
| Easy airway management | Difficult airway management | |
|---|---|---|
| Patients per group | 225 (94%) | 14 (6%) |
| Sex: female/male ratio | 78/147 | 6/8 |
| Mean age [range age] | 54 years [16 days to 96 years] | 64 years [45–93 years] |
| Mean initial GCS score | 5 | 4 |
| Mean intervention time of MICU [range time] | 72 min [20–145 min] | 65 min [25–150 min] |
| Predictive DI signs | 51 (23%) | 10 (71%) |
| Use stylet | 39 (17%) | 14 (100%) |
| Scene intervention | ||
| At home | 108 (48%) | 8 (57%) |
| Outside | 45 (20%) | 2 (14%) |
| Hospital or care place | 72 (32%) | 4 (29%) |
| Intubations indications | ||
| CRA | 84 (38%) | 8 (57%) |
| Respiratory distress | 36 (16%) | 4 (29%) |
| Neurologic distress | 81 (36%) | 2 (14%) |
| Others: voluntary drug poisoning | 24 (10%) | 0 |
| Intubations complications | ||
| Dental trauma | 1 (0.4%) | 0 |
| Macroscopic inhalationa | 7 (3%) | 2 (14%) |
| Oesophageal intubationa | 13 (6%) | 3 (21%) |
| Selective intubation | 12 (5%) | 0 |
| Collapse post-intubation | 33 (15%) | 0 |
| ACR | 0 | 0 |
| Mean intubations attempts | 1.25 | 3 |
| [range attempts] | [1–2] | [2–5] |
GCS: Glasgow coma scale; MICU: mobile intensive care unit; DI: difficult intubation; CRA: cardio-respiratory arrest.
a Only during ETI attempts.All the patients had successful airway management, and no patient required a surgical airway management. We did not encounter a “cannot ventilate–cannot intubate” situation in our study.
Among the 239 cases of airway management in a prehospital setting, the Ezt was used 14 times. It was used in eight men and six women; the male-to-female ratio was 1.33. The age range was 45–93 years; mean age was 64 years.
The Ezt was used for ventilation for a maximum of 150 min, intervention time by MICUs in prehospital situations was 25–150 min, and the mean time was 65 min.
Only Ezt size 41 Fr was used during the study because no patient in the height range 90–130 (Ezt of size 28 Fr) presented difficult airway management.
The Ezt was positioned successfully at first attempt, except for two patients: one needed an adjustment because of air leaks, and for the other patient, the Ezt was replaced due to a complete obstruction of the Ezt during bronchial suction after aspiration of gastric contents.
Predictive signs of DI were found in 61 patients of the 239 airway management cases; this represents 25% of patients with airway management in prehospital situations. The predictive signs of DI are shown in Table 2. The study shows the presence of predictive signs of DI in 71% of cases of the “difficult airway management” group.
| Predictive signs of difficult intubation | Numbers (%) |
|---|---|
| Morbid obesity | 26 (42%) |
| Cervico-facial trauma | 16 (26%) |
| Short neck | 11(18%) |
| Restricted mouth opening <3 cm | 7 (12%) |
| Thyromental distance <6 cm | 1 (2%) |
| Total | 61 |
4. Discussion
A number of previous studies show that the EzT is comparable to the ETT with respect to oxygenation and ventilation, and might even have minor advantages, as the EzT can be inserted slightly more quickly and easily than the ETT [4] and [7].
Our results are in agreement with other studies showing that a short learning period may be sufficient to train emergency physicians since the success rate is high [4] and [7].
In our study, the insertion of the Ezt was successful at the first attempt in all cases. These results are in agreement with other studies carried out which show a very low insertion failure rate [5].
During this study, we noted one specific complication associated with Ezt, to our knowledge never described. This was complete obstruction of the Ezt during bronchial suction after aspiration of gastric contents. The aspiration occurred after 2 failed ETI attempts. The first Ezt was removed and a second Ezt was used without complication.
The main advantages of the Ezt are: shorter insertion time for Ezt than for ETI, better protection against aspiration than a laryngeal mask and the possibility of blind insertion of the Ezt in patients trapped in a sitting position (car crash) [5], [6] and [7].
Unfortunately, in our study, we were unable to assess the time needed to establish an airway for ethical reasons as we were acting in severe emergency cases.
Our difficult intubation rate was 6%, compared with 2.7–12.3% cited in the emergency medicine literature [8],[9], [10], [11], [12] and [13].
Our study showed that prehospital airway difficulties can be predicted in 71% of cases, with easily identifiable predictive signs of DI (morbid obesity, cervico-facial trauma, short neck, restricted mouth opening <3 cm, thyromental distance <6 cm), and we found only 29% unanticipated airway difficulties in prehospital settings.
Our findings suggest that in prehospital emergencies, except for cervico-facial trauma injuries (26% of patients), the most frequent causes of DI are similar to those encountered in clinical practice: morbid obesityand short neck [14].
Rapid evaluation of predictive signs of DI could make airway difficulties possible to anticipate before performing laryngoscopy, to plan alternatives to direct laryngoscopy and to preclude multiple attempts.
However, our study highlights that the stylet is not used enough in French practice, even when there were predictive signs of DI, despite our protocol's recommendations and international guidelines (only 17% of overall ETI and 76% in cases of anticipated airway difficulties).
Nevertheless this prospective observational study had several limitations. No study details optimal training in Ezt use or that Ezt training on manikins is transferable to real patients, thus training in the use of Ezt was not based on evidence-based medicine. Incomplete forms were the most common problem, requiring a supplementary search of the medical files to complete the forms. Selective intubation (no lung expansion visible and absence of sounds during auscultation, reversible situation after moving ETT) was investigated only if it was identified on-site and thus the incidence may have been underestimated in this study. Another limitation of our study is that the data were self-reported by the persons who performed the intubations and hence the number of attempts or complications may have been underestimated.
5. Conclusion
It is essential that emergency physicians receive rigorous training in difficult airway management as well as how to investigate predictive signs of DI in order to plan alternatives to ETI and to avoid potential complications that may arise with several attempts.
Despite the wide range of available techniques for the management of DI, not all are suitable for use in prehospital emergency airway management. The Ezt may be recommended because of the very high success rate of ventilation and the possibility of blind intubation. The low failure rate after a short training period demonstrates that it is easy to use and has a steep learning curve.
Clinical evaluations of the Ezt in prehospital situations are scarce, but these results show that emergency physicians with minimal training, in cases of difficult airway management and in prehospital emergency medicine, can use the EzT safely and effectively. It could be proposed as the first-line alternative technique in difficult airway management in prehospital.
| Tags : airway
Protection des voies aériennes en urgence: Une synthèse à lire
Protection des voies aériennes en médecine d’urgence
Journal Européen des Urgences (2010) 23, 44—56
X. Combes, P. Jabre, F. Soupizet
Le résumé
Le contrôle des voies aériennes des patients présentant une détresse vitale est très souvent nécessaire en médecine d’urgence. L’intubation orotrachéale est la technique de référence pour le contrôle des voies aériennes. En dehors du cadre de la réanimation de l’arrêt cardiaque, l’intubation trachéale doit être reéalisée sur un patient sédaté et curarisé selon la technique d’intubation en séquence rapide. L’intubation en urgence est une intubation à risques. L’inhalation pulmonaire et les épisodes de désaturation artérielle profonde sont les deux complications les plus fréquemment associées à ce geste. En médecine d’urgence, l’intubation difficile, rarement prévisible, est plus fréquente qu’au bloc opératoire. La prise en charge de
l’intubation difficile survenant dans le cadre de la médecine d’urgence repose sur l’utilisation de techniques alternatives efficaces. Ces techniques doivent être utilisées selon un algorithme précis. Les mandrins longs béquillés et le masque laryngé d’intubation de type Fastrach TM permettent de résoudre la majorité des cas d’intubation difficile. En cas d’échec de ces deux techniques, une cricothyroïdotomie permettant un abord trachéal direct doit être réalisée chez les patients impossibles à ventiler.
Morceaux choisis
1. On considère qu’un médecin exerçant en SMUR intube annuellement de 15 à 20 patients. Ces chiffres sont à mettre en parallèle avec les données disponibles pour l’activité anesthésique nationale où environ trois millions de patients sont intubés tous les ans au bloc opératoire par des médecins anesthésistes qui intubent chacun en moyenne plus de 300 patients par an.
Un minimum de 40 intubations pour apprendre l'intubation est nécessaire et 20 par an sont nécessaires pour entretenir cette compétence. Cela signifie que la maîtrise de l'abord des VAS est l'objectif principal de la formation continue du médecin d'unité de telle sorte qu'il soit toujours en capacité de faire face à une obstruction des VAS en condition de combat.
2. Les dispositifs laryngés sont probablement plus faciles à insérer pour des opérateurs non médecins que la sonde d’intubation. Les deux problèmes majeurs rencontrés lors de l’utilisation de ce type de matériel sont le risque d’inhalation pulmonaire et le risque de perforation œsophagienne. En effet, ces dispositifs n’assurent pas une protection complète des voies aériennes en cas de vomissement et le risque d’inhalation est alors réel. Plusieurs cas de déchirure du tiers supérieur de l’œsophage ont été rapportés lors de l’utilisation du Combitube®, liés à la surpression régnant dans le ballonnet œsophagien de ce dispositif.
3. En médecine préhospitalière, les circonstances font que très souvent les patients qui nécessitent une intubation en urgence sont pris en charge alors qu’ils sont allongés sur le sol. L’intubation d’un patient au sol présente quelques difficultés particulières. L’opérateur est en effet dans une position le plus souvent pénible pour réaliser son geste et l’intubation est rendue plus difficile. Une technique de positionnement de l’opérateur visant à limiter les difficultés d’intubation a été décrite récemment. Elle consiste à positionner la personne qui va intuber en décubitus latéral. Dans cette position, l’axe visuel de l’opérateur est abaissé et la visualisation glottique, indispensable pour réaliser l’intubation, est rendue beaucoup plus aisée.
4. Parmi les dispositifs laryngés utilisables en préhospitalier, il faut choisir le FASTRACH car son emploi est documenté et qu'il permet l'intubation orotrachéale.
5. La cricothyroïdotomie représente la technique ultime de contrôle des voies aériennes proposée dans le cas où l’intubation et la ventilation du patient restent impossibles malgré l’utilisation des autres techniques alternatives que sont les mandrins et les dispositifs supraglottiques. ......Cette technique est de réalisation très rapide et permet une ventilation efficace dans plus de 95 % des cas.
6. Un algorithme
| Tags : intubation, airway, coniotomie
26/10/2010
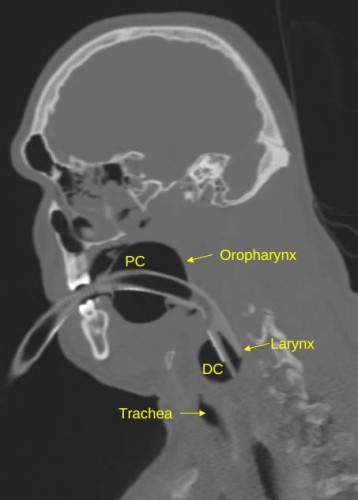
Coniotomie: Connaître l'anatomie aide
Une publication récente résume de manière simple ce qu'il faut savoir, et tout cela en anglais bien sûr.
| Tags : airway, coniotomie
16/10/2010
Alternative à l'intubation; La coniotomie chirurgicale
Il existe un grand débat concernant les alternatives à l'intubation préhospitalière. Si les dispositifs laryngés apparaissent une alternative du fait de taux d'insertion satisfaisant en particulier le tube KING LT, il n'en demeure toujours pas moins qu'il ne représente toujours pas une solution réelle en conditions de combat du fait de la nécessité de réaliser une anesthésie générale, de l'absence de protection contre le risque d'inhalation, et de limitations importantes en terme de ventilation (pression et déplacement de tube pendant le transport). Ces dispositifs sont par ailleurs relativement volumineux. La recommandation en condition de combat est de privilégier la coniotomie chirurgicale sous AL.
-------------------------------------------------------------------
Prehosp Emerg Care. 2010 Oct-Dec;14(4):515-30.
A meta-analysis of prehospital airway control techniques part II: alternative airway devices and cricothyrotomy success rates.
Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW.
Emergency Medical Care Program, 122 Moore Building, Western Carolina University, Cullowhee, NC 28723, USA. mhubble@email.wcu.edu
Abstract
BACKGROUND: Airway management is a key component of prehospital care for seriously ill and injured patients. Oral endotracheal intubation (OETI) is the definitive airway of choice in most emergency medical services (EMS) systems. However, OETI may not be an approved skill for some clinicians or may prove problematic in certain patients because of anatomic abnormalities, trauma, or inadequate relaxation. In these situations alternative airways are frequently employed. However, the reported success rates for these devices vary widely, and established benchmarks are lacking.
OBJECTIVE: We sought to determine pooled estimates of the success rates of alternative airway devices (AADs) and needle cricothyrotomy (NCRIC) and surgical cricothyrotomy (SCRIC) placement through a meta-analysis of the literature.
METHODS: We performed a systematic literature search for all English-language articles reporting success rates for AADs, SCRIC, and NCRIC. Studies of field procedures performed by prehospital personnel from any nation were included. All titles were reviewed independently by two authors using prespecified inclusion criteria. Pooled estimates of success rates for each airway technique were calculated using a random-effects meta-analysis model.
RESULTS: Of 2,005 prehospital airway titles identified, 35 unique studies were retained for analysis of AAD success rates, encompassing a total of 10,172 prehospital patients. The success rates for SCRIC and NCRIC were analyzed across an additional 21 studies totaling 512 patients. The pooled estimates (and 95% confidence intervals [CIs]) for intervention success across all clinicians and patients were as follows: esophageal obturator airway-esophageal gastric tube airway (EOA-EGTA) 92.6% (90.1%-94.5%); pharyngeotracheal lumen airway (PTLA) 82.1% (74.0%-88.0%); esophageal-tracheal Combitube (ETC) 85.4% (77.3%-91.0%); laryngeal mask airway (LMA) 87.4% (79.0%-92.8%); King Laryngeal Tube airway (King LT) 96.5% (71.2%-99.7%); NCRIC 65.8% (42.3%-83.59%); and SCRIC 90.5% (84.8%-94.2%).
CONCLUSIONS: We provide pooled estimates for prehospital AAD, NCRIC, and SCRIC airway interventions. Of the AADs, the King LT demonstrated the highest insertion success rate (96.5%), although this estimate is based on limited data, and data regarding its ventilatory effectiveness are lacking; more data are available for the ETC and LMA. The ETC, LMA, and PTLA all had similar-but lower-success rates (82.1%-87.4%). NCRIC has a low rate of success (65.8%); SCRIC has a much higher success rate (90.5%) and should be considered the preferred percutaneous rescue airway.
-------------------------------------------------------------------
| Tags : airway
Intubation préhospitalière: Comment ?
On peut intuber en pré-hospitalier sans anesthésie (sous AL de glotte) mais c'est mieux avec des agents de sédation et encore mieux avec un protocole d'intubation en séquence rapide. L'intubation nasotrachéale: C'est moins bien, voire sujet à caution.
Prehosp Emerg Care. 2010 Jul-Sep;14(3):377-401.
A meta-analysis of prehospital airway control techniques part I: orotracheal and nasotracheal intubation success rates.
Hubble MW, Brown L, Wilfong DA, Hertelendy A, Benner RW, Richards ME.
Emergency Medical Care Program, Western Carolina University, Cullowhee, North Carolina 28723, USA. mhubble@email.wcu.edu
Abstract
BACKGROUND: Airway management is a key component of prehospital care for seriously ill and injured patients. Although endotracheal intubation has been a commonly performed prehospital procedure for nearly three decades, the safety and efficacy profile of prehospital intubation has been challenged in the last decade. Reported intubation success rates vary widely, and established benchmarks are lacking.
OBJECTIVE: We sought to determine pooled estimates for oral endotracheal intubation (OETI) and nasotracheal intubation (NTI) placement success rates through a meta-analysis of the literature.
METHODS: We performed a systematic literature search for all English-language articles reporting placement success rates for prehospital intubation. Studies of field procedures performed by prehospital personnel from any nation were included. All titles were reviewed independently by two authors using prespecified inclusion criteria. Pooled estimates of success rates for each airway technique, including drug-facilitated intubation (DFI) and rapid-sequence intubation (RSI), were calculated using a random-effects model. Historical trends were evaluated using meta-regression.
RESULTS: Of 2,005 identified titles reviewed, 117 studies addressed OETI and 23 addressed NTI, encompassing a total of 57,132 prehospital patients. There was substantial interrater reliability in the review process (kappa = 0.81). The pooled estimates (and 95% confidence intervals [CIs]) for intervention success for nonphysician clinicians were as follows: overall non-RSI/non-DFI OETI success rate: 86.3% (82.6%-89.4%); OETI for non-cardiac arrest patients: 69.8% (50.9%-83.8%); DFI 86.8% (80.2%-91.4%); and RSI 96.7% (94.7%-98.0%). For pediatric patients, the paramedic OETI success rate was 83.2% (55.2%-95.2%). The overall NTI success rate for nonphysician clinicians was 75.9% (65.9%-83.7%). The historical trend of OETI reflects a 0.49% decline in success rates per year.
CONCLUSIONS: We provide pooled estimates of placement success rates for prehospital airway interventions. For some patient and clinician characteristics, OETI has relatively low success rates. For nonarrest patients, DFI and RSI appear to increase success rates. Across all clinicians, NTI has a low rate of success, raising questions about the safety and efficacy of this procedure.
------------------------------------------------------------------------------------------------------------------------------------------------------
| Tags : airway
11/10/2010
Coniotomie: Avec un guide !
La coniotmie ou cricothyrotomie est unetechnique essentielle à maîtriser pour une prise en charge optimale des blessés de la face présentant une obstruction des voies aériennes ( le A du SAFE ABC MARCHE). ICI vous est présenté une technique qu'il faut connaître.
| Tags : airway, coniotomie
17/09/2010
EVASAN Hélico: Intubation=Perte de temps ?
Intuber en préhospitalier fait perdre en moyennne 8 minutes sur les délais d'évacuation. C'est du moins ce qui est présenté dans cet article. Il s'agit donc d'une prise de risque majeure pour les équipages et pas forcément ungain de chance pour le blessé compte tenu de la brièveté actuelle des durées de vol en afghanistan.
| Tags : airway, intubation