30/09/2016
Nustat: Un nouveau venu ?
Controlling intraoperative hemorrhage during burn surgery: A prospective, randomized trial comparing NuStat® hemostatic dressing to the historic standard of care.
INTRODUCTION:
One of the primary intraoperative challenges during burn surgery is to adequately excise the burn while avoiding massive hemorrhage. This has become increasingly important, as we see more burn patients that are older and with more medical comorbidities. While adequate excision down to healthy tissues for deep burns is essential for skin graft to take, it also leads to active bleeding that can be a challenge to control. Good hemostasis is imperative as a hematoma is the most common cause of graft loss. Several new products have become available to help control intraoperative hemorrhage. A new hemostatic dressing, NuStat®, is available and approved by FDA in United States.
METHODS:
A single institution prospective randomized control trial was completed at Regional Burn Center of the University of South Alabama comparing NuStat® with the institutional historic standard of care. Twenty such patients were included in our study. A cost analysis was also completed as part of the study retrospectively.
RESULTS:
For dressings used to treat the burn site, blood loss on the side treated with NuStat® was on average less (27g/100cm2) than the side treated with our historic standard of care (31g/100cm2), though it was not statistically significant (p=0.81). Similarly, on the donor site, blood loss on the side treated with NuStat® was on average less (14g/100cm2) than the side treated with our historic standard of care (15g/100cm2), but it was also not statistically significant (p=0.92). Average total blood loss from both excision and donor sites was also less with NuStat®(10g/100cm2) compared to the historic standard of care (12g/100cm2), but it was also not significant (p=0.77). There was no difference in the number of cycles required to achieve hemostasis for either the burn (1.15 NuStat® vs. 1.1 for historic standard of care, p=0.70) or the donor site (1 vs. 1, p=1.0). When comparing the cost of NuStat® versus the historic standard of care, the actual costs incurred for the wounds was less for the portion treated with NuStat® ($148.43) when compared to the historic standard of care ($186.45) (p<0.001).
CONCLUSIONS:
Based on these findings, NuStat® hemostatic action should be comparable to the historic standard of care, and these newerhemostatic agents evaluated further in burn surgery and bleeding during other procedures such as trauma surgery.
27/09/2016
Ceinture pelvienne improvisée
24/09/2016
Crico: Mais que fait-on ?
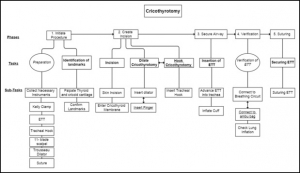
A hierarchical task analysis of cricothyroidotomy procedure for a virtual airway skills trainer simulator
Demirel D. et Al. Am J Surg. 2016 Sep;212(3):475-84
BACKGROUND:
Despite the critical importance of cricothyroidotomy (CCT) for patient in extremis, clinical experience with CCT is infrequent, and current training tools are inadequate. The long-term goal is to develop a virtual airway skills trainer that requires a thorough task analysis to determine the critical procedural steps, learning metrics, and parameters for assessment.
METHODS:
Hierarchical task analysis is performed to describe major tasks and subtasks for CCT. A rubric for performance scoring for each taskwas derived, and possible operative errors were identified.
RESULTS:
Time series analyses for 7 CCT videos were performed with 3 different observers. According to Pearson's correlation tests, 3 of the 7 major tasks had a strong correlation between their task times and performance scores.
CONCLUSIONS:
The task analysis forms the core of a proposed virtual CCT simulator, and highlights links between performance time and accuracy when teaching individual surgical steps of the procedure.
| Tags : airway
MEDEVAC: Une réanimation avancée rapporte
A review of the first 10 years of critical care aeromedical transport during operation iraqi freedom and operation enduring freedom: the importance of evacuation timing
Ingals N et Al. JAMA Surg. 2014 Aug;149(8):807-13
------------------------------------------
Ce document est très intéressant car il met en avant l'intérêt du transport des blessés de guerre par des équipes maîtrisant toutes les facettes du damage control resusictation tant au niveau médical que paramédical. Une approche très similaire est celle des MERT-E
------------------------------------------
Advances in the care of the injured patient are perhaps the only benefit of military conflict. One of the unique aspects of the military medical care system that emerged during Operation Iraqi Freedom and Operation Enduring Freedom has been the opportunity to apply existing civilian trauma system standards to the provision of combat casualty care across an evolving theater ofoperations.
OBJECTIVES:
To identify differences in mortality for soldiers undergoing early and rapid evacuation from the combat theater and to evaluate the capabilities of the Critical Care Air Transport Team (CCATT) and Joint Theater Trauma Registry databases to provide adequate data to support future initiatives for improvement of performance.
DESIGN, SETTING, AND PARTICIPANTS:
Retrospective review of CCATT records and the Joint Theater Trauma Registry from September 11, 2001, to December 31, 2010, for the in-theater military medicine health system, including centers in Iraq, Afghanistan, and Germany. Of 2899 CCATT transport records, those for 975 individuals had all the required data elements.
EXPOSURE:
Rapid evacuation by the CCATT.
MAIN OUTCOMES AND MEASURES:
Survival as a function of time from injury to arrival at the role IV facility at Landstuhl Regional Medical Center.
RESULTS:
The patient cohort demonstrated a mean Injury Severity Score of 23.7 and an overall 30-day mortality of 2.1%. Mortality en route was less than 0.02%. Statistically significant differences between survivors and decedents with respect to the Injury Severity Score (mean [SD], 23.4 [12.4] vs 37.7 [16.5]; P < .001), cumulative volume of blood transfused among the patients in each group who received a transfusion (P < .001), worst base deficit (mean [SD], -3.4 [5.0] vs -7.8 [6.9]; P = .02), and worst international normalized ratio (median [interquartile range], 1.2 [1.0-1.4] vs 1.4 [1.1-2.2]; P = .03) were observed. We found no statistically significant difference between survivors and decedents with respect to time from injury to arrival at definitive care.
CONCLUSIONS AND RELEVANCE:
Rapid movement of critically injured casualties within hours of wounding appears to be effective, with a minimal mortality incurred during movement and overall 30-day mortality. We found no association between the duration of time from wounding to arrival at Landstuhl Regional Medical Center with respect to mortality.
| Tags : medevac
Transfusion en vol: Sécurité assurée
Risk Management Analysis of Air Ambulance Blood Product Administration in Combat Operations
BACKGROUND:
Between June-October 2012, 61 flight-medic-directed transfusions took place aboard U.S. Army Medical Evacuation (medevac) helicopters in Afghanistan. This represents the initial experience for pre-hospital blood product transfusion by U.S. Army flight medics.
METHODS:
We performed a retrospective review of clinical records, operating guidelines, after-action reviews, decision and information briefs, bimonthly medical conferences, and medevac-related medical records.
RESULTS:
A successful program was administered at 10 locations across Afghanistan. Adherence to protocol transfusion indications was 97%. There were 61 casualties who were transfused without any known instance of adverse reaction or local blood product wastage. Shock index (heart rate/systolic blood pressure) improved significantly en route, with a median shock index of 1.6 (IQR 1.2-2.0) pre-transfusion and 1.1 (IQR 1.0-1.5) post-transfusion (P < 0.0001). Blood resupply, training, and clinical procedures were standardized across each of the 10 areas of medevacoperations.
DISCUSSION:
Potential risks of medical complications, reverse propaganda, adherence to protocol, and diversion and/or wastage of limited resources were important considerations in the development of the pilot program. Aviation-specific risk mitigation strategies were important to ensure mission success in terms of wastage prevention, standardized operations at multiple locations, and prevention of adverse clinical outcomes. Consideration of aviation risk mitigation strategies may help enable other helicopter emergency medical systems to develop remote pre-hospital transfusion capability. This pilot program provides preliminary evidence that blood product administration by medevac is safe.
| Tags : transfusion
Tourniquet: Entretien 3/mois mieux qu'1/mois
Does practice make perfect? Prospectively comparing effects of 2 amounts of practice on tourniquet use performance
---------------------------------------------
L'entretien des compétences et en particulier des gestes apparaît fondamentale et nécessite un suivi chiffré pour garantir un niveau suffisant d'expertise pour une projection opérationnelle. Ceci est parfaitement mis en avant dans le travail de schaeur et Al. (1) qui porte sur des gestes de réanimation préhospitalière. Le document proposé à votre lecture porte sur un geste essentiel: La pose du garrot. Une pratique plus régulière limite le désapprentissage.
---------------------------------------------
Although a lifesaving skill, currently, there is no consensus for the required amount of practice in tourniquet use. We compared the effect of 2 amounts of practice on performance of tourniquet use by nonmedical personnel.
METHODS:
Israeli military recruits without previous medical training underwent their standard tactical first aid course, and their initial performance in use of the Combat Application Tourniquet (CAT; Composite Resources, Rock Hill, SC) was assessed. The educational intervention was to allocate the participants into a monthly tourniquet practice program: either a single-application practice (SAP) group or a triple-application practice (TAP) group. Each group practiced according to its program. After 3 months, the participants' tourniquet use performance was reassessed. Assessments were conducted using the HapMed Leg Tourniquet Trainer (CHI Systems, Fort Washington, PA), a mannequin which measures time and pressure.
RESULTS:
A total of 151 participants dropped out, leaving 87 in the TAP group and 69 in the SAP group. On initial assessment, the TAP group and the SAP group performed similarly. Both groups improved their performance from the initial to the final assessment. The TAP group improved more than the SAP group in mean application time (faster by 18 vs 8 seconds, respectively; P = .023) and in reducing the proportion of participants who were unable to apply any pressure to the mannequin (less by 18% vs 8%, respectively; P = .009).
CONCLUSION:
Three applications per monthly practice session were superior to one. This is the first prospective validation of a tourniquet practice program based on objective measurements.
| Tags : tourniquet
23/09/2016
SFMU: Reco Anaphylaxie
22/09/2016
Crico: Quelques rappels qui font du bien
Evidence Is Important: Safety Considerations for Emergency Catheter Cricothyroidotomy
Marshall SD et Al. Acad Emerg Med. 2016 Sep;23(9):1074-6
Il existe un regain d'intérêt concernant la pratique de l'oxygénation après ponction de la membrane cricoÏdienne. De large débats portent sur la meilleure méthode à utiliser. En pratique il n'est pas inutile de rappeler quelques vérités pratiques. C'est ce que propose ce document dont la lecture est fort utile. Cliquez sur la référence pour accéder au document et ici pour accéder à des vidéos complémentaires
| Tags : coniotomie
SmO2: Utile ?
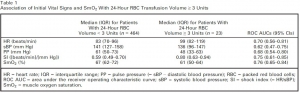
Muscle Oxygen Saturation Improves Diagnostic Association Between Initial Vital Signs and Major Hemorrhage: A Prospective Observational Study.
L'hémorragie reste la cause principale des décès évitable et l'importance de la mise en oeuvre d'une stratégie transfusionnelle précoce est actée. Mais sur quels critères. Au delà des critères cliniques simples, on peut citer le recours au suivi des lactates. Le suivi de paramètres d'oxygénation tissulaire simple est maintenant possible. Ce qu'évoque ce document est l'emploi de la SmO2, élément déjà utilisé en médecine du sport. Le recours à un tel paramètre est donc potentiellement très intéressant si cette pertinence était confirmée et sa mesure valide avec des outils simples.
OBJECTIVES:
During initial assessment of trauma patients, vital signs do not identify all patients with life-threatening hemorrhage. We hypothesized that a novel vital sign, muscle oxygen saturation (SmO2 ), could provide independent diagnostic information beyond routine vital signs for identification of hemorrhaging patients who require packed red blood cell (RBC) transfusion.
METHODS:
This was an observational study of adult trauma patients treated at a Level I trauma center. Study staff placed the CareGuide 1100 tissue oximeter (Reflectance Medical Inc., Westborough, MA), and we analyzed average values of SmO2 , systolic blood pressure (sBP), pulse pressure (PP), and heart rate (HR) during 10 minutes of early emergency department evaluation. We excluded subjects without a full set of vital signs during the observation interval. The study outcome was hemorrhagic injury and RBC transfusion ≥ 3 units in 24 hours (24-hr RBC ≥ 3). To test the hypothesis that SmO2 added independent information beyond routine vital signs, we developed one logistic regression model with HR, sBP, and PP and one with SmO2 in addition to HR, sBP, and PP and compared their areas under receiver operating characteristic curves (ROC AUCs) using DeLong's test.
RESULTS:
We enrolled 487 subjects; 23 received 24-hr RBC ≥ 3. Compared to the model without SmO2 , the regression model with SmO2 had a significantly increased ROC AUC for the prediction of ≥ 3 units of 24-hr RBC volume, 0.85 (95% confidence interval [CI], 0.75-0.91) versus 0.77 (95% CI, 0.66-0.86; p < 0.05 per DeLong's test). Results were similar for ROC AUCs predicting patients (n = 11) receiving 24-hr RBC ≥ 9.
CONCLUSIONS:
SmO2 significantly improved the diagnostic association between initial vital signs and hemorrhagic injury with blood transfusion. This parameter may enhance the early identification of patients who require blood products for life-threatening hemorrhage.
21/09/2016
Hypothermie accidentelle: Vision scandinave
Accidental hypothermia-an update : The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM).
Paal et al. Scand J Trauma Resusc Emerg Med. (2016) 24:111
BACKGROUND:
This paper provides an up-to-date review of the management and outcome of accidental hypothermia patients with and without cardiac arrest.
METHODS:
The authors reviewed the relevant literature in their specialist field. Summaries were merged, discussed and approved to produce this narrative review.
RESULTS:
The hospital use of minimally-invasive rewarming for non-arrested, otherwise healthy, patients with primary hypothermia and stable vital signs has the potential to substantially decrease morbidity and mortality for these patients. Extracorporeal life support (ECLS) has revolutionised the management of hypothermic cardiac arrest, with survival rates approaching 100 % in some cases. Hypothermic patients with risk factors for imminent cardiac arrest (temperature <28 °C, ventricular arrhythmia, systolic blood pressure <90 mmHg), and those who have already arrested, should be transferred directly to an ECLS-centre. Cardiac arrest patients should receive continuous cardiopulmonary resuscitation (CPR) during transfer. If prolonged transport is required or terrain is difficult, mechanical CPR can be helpful. Delayed or intermittent CPR may be appropriate in hypothermic arrest when continuous CPR is impossible. Modern post-resuscitation care should be implemented following hypothermic arrest. Structured protocols should be in place to optimise pre-hospital triage, transport and treatment as well as in-hospital management, including detailed criteria and protocols for the use of ECLS and post-resuscitation care.
CONCLUSIONS:
Based on new evidence, additional clinical experience and clearer management guidelines and documentation, the treatment ofaccidental hypothermia has been refined. ECLS has substantially improved survival and is the treatment of choice in the patient with unstable circulation or cardiac arrest.
| Tags : hypothermie
Trauma Jonctionnel: Quels dispositifs appliquables ?
17/09/2016
La Kétamine prévient-elle le PTSD ?
| Tags : ptsd
15/09/2016
Position intraosseuse ? Echographiez !
A Serious Adult Intraosseous Catheter Complication and Review of the Literature.
OBJECTIVE:
Current guidelines recommend the use of intraosseous access when IV access is not readily attainable. The pediatric literaturere ports an excellent safety profile, whereas only small prospective studies exist in the adult literature. We report a case of vasopressor extravasation and threatened limb perfusion related to intraosseous access use and our management of the complication. We further report our subsequent systematic review of intraosseous access in the adult population.
DATA SOURCES:
Ovid Medline was searched from 1946 to January 2015.
STUDY SELECTION:
Articles pertaining to intraosseous access in the adult population (age greater than or equal to 14 years) were selected. Search terms were "infusion, intraosseous" (all subfields included), and intraosseous access" as key words.
DATA EXTRACTION:
One author conducted the initial literature review. All authors assessed the methodological quality of the studies and consensus was used to ensure studies met inclusion criteria.
DATA SYNTHESIS:
The case of vasopressor extravasation was successfully treated with pharmacologic interventions, which reversed the effects of the extravasated vasopressors: intraosseous phentolamine, topical nitroglycerin ointment, and intraarterial verapamil and nitroglycerin. Our systematic review of the adult literature found 2,332 instances of intraosseous insertion. A total of 2,106 intraosseous insertion attempts were made into either the tibia or the humerus; 192 were unsuccessful, with an overall success rate of 91%. Five insertions were associated withserious complications. A total of 226 insertion attempts were made into the sternum; 54 were unsuccessful, with an overall success rate of 76%.
----
Color Doppler ultrasonography has been described as a method to verify placement of an intraosseous catheter. A high-frequency linear array transducer is placed near the intraosseous insertion site in either transverse or longitudinal axis. The color Doppler sample box is adjusted to include the subcutaneous compartment, the periosteum, and the intraosseous space, with the tomographic plane oriented to intersect the axis of the intraosseous needle . A 10-mL syringe filled with normal saline is attached to the intraosseous catheter and is rapidly infused with real-time ultrasonography imaging. If the intraosseous catheter is properly placed, color Doppler signal is seen in the subperiosteal (intraosseous) compartment. The presence of color Doppler signal in the extraosseous compartment indicates improper intraosseous catheter placement with extravasation.
----
CONCLUSIONS:
Intraosseous catheter insertion provides a means for rapid delivery of medications to the vascular compartment with a favorable safety profile. Our systematic literature review of adult intraosseous access demonstrates an excellent safety profile with serious complications occurring in 0.3% of attempts. We report an event of vasopressor extravasation that was potentially limb threatening. Therapy included local treatment and injection of intraarterial vasodilators. Intraosseous access complications should continue to be reported, so that the medical community will be better equipped to treat them as they arise.
| Tags : intraosseux
14/09/2016
X stat: Magique ? Et bien NON
Management of External Hemorrhage in Tactical Combat Casualty Care: The Adjunctive Use of XStat™ Compressed Hemostatic Sponges: TCCC Guidelines Change 15-03.
---------------------------
Le recours à de petites éponges comprzsées et recouvertes de chitosan apparaît fortement séduisant à tel point que l'XStat fait partie du TCCC. Cependant les bases scientifiques qui pourraient permettre de recommander ce produit paraissent très faibles. La lecture attentive du document proposé permet de s'en rendre compte. D'une part une application sur un cochon dans des conditions de laboratoire par un expert ne reproduit pas les conditions de combat. Ce produit apparaît ne pass être adapté pour un emploi intra-thoracique, abdominal ou cervical et il est prévu pour une durée d'application de 04h, ce qui ne permet pas de couvrir un certain nombre de missions vraiment spéciales ou certaine régions comme le cou (1). On comprend bien dès lors toute la prudence à avoir avec ces produits que l'industrie nous présente comme "magique". Ils le sont peut être, et ceci concerne tous les pansements hémostatiques (2), mais il faut le prouver et ne pas céder aux sirènes effrénées du marketing des laboratoires. En la matière bien réaliser un packing de plaie, ne serait qu'avec une gaze standard doit rester un objectif fondamental, le reste étant un plus mais pas le fondamental.
---------------------------
Exsanguination from wounds in the so-called junctional regions of the body (i.e., the neck, the axilla, and the groin) was responsible for 19% of the combat fatalities who died from potentially survivable wounds sustained in Afghanistan or Iraq during 2001 to 2011. The development of improved techniques and technology to manage junctional hemorrhage has been identified in the past as a high-priority item by the Committee on Tactical Combat Casualty Care (CoTCCC) and the Army Surgeon General's Dismounted Complex Blast Injury (DCBI) Task Force. Additionally, prehospital care providers have had limited options with which to manage hemorrhage resulting from deep, narrow-track, penetrating trauma. XStat™ is a new product recently approved by the US Food and Drug Administration as a hemostatic adjunct to aid in the control of bleeding from junctional wounds in the groin or axilla. XStat has now been recommended by the CoTCCC as another tool for the combat medical provider to use in the management of junctional hemorrhage. The evidence that supports adding XStat to the TCCC Guidelines for the treatment of external hemorrhage is summarized in this paper.
12/09/2016
L'hôpital de proximité: Insuffisant ?
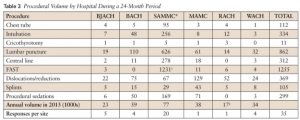
Garrison Clinical Setting Inadequate for Maintenance of Procedural Skills for Emergency Medicine Physicians: A Cross-Sectional Study
Schauer SG et Al. J Spec Oper Med. 2015 Winter;15(4):67-70
----------------------------------------
Lire également cet éditorial qui pointe l'insuffisance de l'exercice en hôpital de proximité avec le rôle important que peut jouer la simulation. Les auteurs proposent un maintien longitudinal des compétences avec des minima en termes de pratiques gestuelles avant projection.
----------------------------------------
BACKGROUND:
Emergency medicine physicians (EPs) are often placed in far-forward, isolated areas in theater. Maintenance of their emergency intervention skills is vital to okeep the medical forces deployment ready. The US Army suggests that working at a Military Treatment Facility (MTF) is sufficient t keep emergency procedural skills at a deployment-ready level. We sought to compare the volume of emergency procedures that providers reported necessary to maintain their skills with the number available in the MTF setting.
METHODS:
EPs were surveyed to quantify the number of procedures they reported they would need to perform yearly to stay deployment-ready. We obtained procedure data for their duty stations and compared the procedure volume with the survey responses to determine if working at an MTF is sufficient to keep providers' skills deployment ready.
RESULTS:
The reported necessary average numbers per year were as follows: tube thoracostomy (5.9), intubation (11.4), cricothyrotomy (4.2), lumbar puncture (5.2), central line (10.0), focused assessment with sonography for trauma (FAST) (21.3), reductions (10.6), splints (10.5), and sedations (11.7). None of the procedure volumes at MTFs met provider requirements with the exception of FAST examinations at the only trauma center.
CONCLUSIONS:
This suggests the garrison clinical environment is inadequate for maintaining procedure skills. Further research is needed to determine modalities that will provide adequate training volume.
07/09/2016
Airway: S'y pencher avec sérieux
Emergency airway management – by whom and how ?
Sollid SJ et Al. Acta Anaesthesiol Scand. 2016 Oct;60(9):1185-7
---------------------------------------
Encore une publication qui insiste sur la formation à la gestion des voies aériennes et au maintien de ses compétences. Ceci n'est pas innée et s'impose tout d'abord non seulement aux praticiens peu confrontés à cette exercice, en première ligne les médecins urgentistes, mais aussi aux médecins anesthésistes compte tenu de l'essor de l'anesthésie loco-régionale et l'emploi de dispositifs supra-glottique. A lire et relire, ainsi que les références.
---------------------------------------
Procedures for advanced airway management are important for maintaining basic life functions in the unconscious patient, and can be lifesaving in critically ill or injured patients. In Acta Anaesthesiologica Scandinavica, a working group from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (SSAI) presents updated clinical guidelines on pre-hospital airway management.[1] The recommendations from the working group are important statements in the long-lasting quest to ensure that advanced airway management is managed safely pre-hospital at the right level of competence.
Technically, many of the procedures for advanced airway management of the average patient in controlled situations are easy to learn. Yet, a German study found that at least 200 intubation attempts were required to reach a 95% success rate.[2] The challenge, however, lies in assessing and managing the difficult airway cases. Emergency physicians with anaesthesiology background seem to be better at predicting difficult intubations than emergency physicians with other backgrounds, in addition to having significantly lower incidence of intubation problems and more experience in decisions on whether to intubate.[3]
Data from the UK show that the majority of complications in airway management occur in the emergency department and the intensive care unit. One of the reasons is the relatively low exposure to such procedures in these settings.[4] Studies on pre-hospital airway management also indicate that the rate of complications in this setting is high, and also that it is greatly dependent on the competence of the provider.[5] There is sufficient evidence to support that pre-hospital advanced airway management in the hands of trained anaesthesiologists is a safe procedure.[6-8] However, as other authors have pointed out, being a proficient provider of airway management is not equivalent with being an anaesthesiologist.[9] The combination of competencies to assess the situation, practical skills and ability to manage complications are more important than the name of the provider's speciality. In a physician-staffed helicopter emergency medical service in the UK, where doctors are a mix of anaesthesiologists and emergency physicians, the success rates are still high and complications are low.[10] This is probably related to the strict training and highly standardised operating procedures that all doctors must adhere to.
Based on this, advanced airway management seems to be safe if the providers have a large volume of clinical experience (anaesthesiologists) or alternatively, operate under strict clinical guidance and protocol rule (non-anaesthesiologists). Intuitively, a combination of both could probably improve safety further and would be useful in clinical environments, and particularly when airway management occurs as unplanned events with little or no time for individual planning and screening of the patient.
The most recent consensus-based European Guidelines for Postgraduate Training in Anaesthesiology recommend the change from duration of training and number of procedures into competence-based training.[11] These competences include advanced airway management skills. Some of this training can be done in simulation settings, but simulation cannot replace real-life situations.[12, 13] Once learnt, competences must be maintained. That requires regular exposure to the procedure. As the use of laryngeal masks and regional blocks increases at the expense of anaesthesia procedures including endotracheal intubation, the training opportunities for all providers, including anaesthesia personnel is being reduced. That is one of the reasons why the Section and Board of Anaesthesiology of the European Union of Medical Specialists recommended a multispecialty approach to emergency medicine.[14] Like the Scandinavian Society of Anaesthesiology and Intensive Care recommended in 2010,[15] the European Society of Anaesthesiology is increasingly using the term ‘Critical Emergency Medicine’ for the part of the anaesthesiology speciality that all anaesthesiologists should command.
A Nordic working group published a literature review in 2008 on pre-hospital airway management, and proposed an evidence-based guideline.[16] This position paper concludes unanimously that pre-hospital emergency airway management in the appropriate patient groups should be achieved by rapid sequence induction and endotracheal intubation, provided the physician is an anaesthesiologist. Other providers should treat the same patient group in the lateral trauma recovery position and if necessary, provide assisted bag-valve-mask ventilation. Supraglottic airway devices were recommended for non-anaesthesiologists in cardiac arrest with a need for supine positioning of the patient, and as a backup device for anaesthesiologists. These findings have been reaffirmed in the new SSAI clinical practice guideline published in August issue.[1]
A similar paper concerning Scandinavian clinical practice guidelines on general anaesthesia for emergency situations underlines the dangers associated with administering anaesthesia outside the operating theatre. They too advocate that anaesthesia for emergency patients should be given by, or under very close supervision by, experienced anaesthesiologists, and stress that problems with the airway are to be anticipated.[17]
Emergency airway management outside the operating theatres carries a high risk of difficult intubation, in a recent study 10.3%, and these patients have a high risk of complications.[18] This demonstrate the need for particular vigilance in and training for these settings, and provides another argument for using supraglottic approaches for those patients in the hands of non-anaesthesiologists. A recent report from the Johns Hopkins Hospital describes a successful attempt to mitigate difficult airway situations arising within this highly specialised hospital. By the formation of a difficult airway response team, the researchers conquered difficult airway situations which until the intervention ranked among the top five adverse events in Maryland.[19]
In conclusion, emergency airway management carries a high risk of patient injury, even among highly trained and skilled anaesthesiologists. Airway management can be learned, and emergency airway handling can be performed with maintained safety also by non-anaesthesiologists, provided they operate in a highly supervised and algorithm-based environment.[9] In this light, the emerging new emergency medical specialty in the Scandinavian countries is of concern, if these acute or emergency physicians are supposed to perform emergency airway procedures independent of their anaesthesiologist colleagues. Whoever manages the compromised airway in the pre-hospital setting is required to do so with the highest level of quality, attainable through a combination of clinical experience and clinical governance. It is difficult to see how this can be achieved and maintained outside the specialty of anaesthesiology. In the end, this is a matter of patient safety, not competition for airways.
| Tags : airway
04/09/2016
Garrot: Mais l'occlusion dans le temps ?
Different Width and Tightening System: Emergency Tourniquets on Distal Limb Segments
BACKGROUND:
Tourniquets are used on distal limb segments. We examined calf and forearm use of four thigh-effective, commercial tourniquetswith different widths and tightening systems: 3.8 cm windlass Combat Application Tourniquet® (CAT, combattourrniquet.com) and Special Operations Forces® Tactical Tourniquet-Wide (SOFTTW, www.tacmedsolutions.com), 3.8 cm ratchet Ratcheting Medical Tourniquet - Pediatric (RMT-P, www.ratchetingbuckles. com), and 10.4 cm elastic Stretch-Wrap-And-Tuck Tourniquet® (SWATT, www.swattourniquet.com).
METHODS:
From Doppler-indicated occlusion, windlass completion was the next securing opportunity; ratchet completion was one additional tooth advance; elastic completion was end tucked under a wrap.
RESULTS:
All applications on the 16 recipients achieved occlusion. Circumferences were calf 38.1±2.5 cm and forearm 25.1±3.0 cm (p<.0001, t-test, mean±SD). Pressures at Occlusion, Completion, and 120-seconds after Completion differed within each design (p<.05, one-way ANOVA; calf: CAT 382±100, 510±108, 424±92 mmHg; SOFTT-W 381±81, 457±103, 407±88 mmHg; RMT-P 295±35, 350±38, 301±30 mmHg; SWATT 212±46, 294±59, 287±57 mmHg; forearm: CAT 301±100, 352±112, 310±98 mmHg; SOFTT-W 321±70, 397±102, 346±91 mmHg; RMT-P 237±48, 284±60, 256±51 mmHg; SWATT 181±34, 308±70, 302±70 mmHg). Comparing designs, pressures at each event differed (p<.05, one-way ANOVA), and the elastic design had the least pressure decrease over time (p<.05, one-way ANOVA). Occlusion losses differed among designs on the calf (p<.05, χ²; calf: CAT 1, SOFTT-W 5, RMT-P 1, SWATT 0; forearm: CAT 0, SOFTT-W 1, RMT-P 2, SWATT 0).
CONCLUSIONS:
All four designs can be effective on distal limb segments, the SWATT doing so with the lowest pressures and least pressure losses over time. The pressure change from Occlusion to Completion varies by tourniquet tightening system and can involve a pressure decrease with the windlass tightening systems. Pressure losses occur in as little as 120 seconds following Completion and so can loss of Occlusion. This is especially true for nonelastic strap tourniquet designs.
| Tags : tourniquet
2 garrots: Côte à côte SVP, mais attention
Pressures Under 3.8cm, 5.1cm, and Side-by-Side 3.8cm-Wide Tourniquets
-----------------------------
Plus un garrot est large et plus efficace il est. parmi les garrots en dotation le Garrot Delfi est le plus performant en terme d'occlusion. Néanmoins son emploi en première intention et hors un vecteur d'évacuation est difficilement envisageable. Aussi l'association de deux garrots apparaît elle très pertinente surtout si ces derniers sont posés côte à côte. Ce n'est pas pour autant une sécurité car en permettant l'obtention d'une pression d'occlusion plus basse, cette méthode expose à une occlusion insuffisante . Cette publication a par ailleurs comme intérêt de montrer que la pression d'occlusion baisse avec le temps et ce dès les premières minutes. Il est fondamental d'apprécier TRES régulièrement l'efficacité du garrot. Donc plutôt un garrot large d'emblée mais si l'on doit compléter poser le second à côté du premier. A noter que le garrot utilisé n'est pas en dotation dans l'armées US mais qu'il s'agit d'un des meilleurs garrots de dernière génération.
-----------------------------
BACKGROUND:
Applications of wider tourniquet are expected to occlude arterial flow at lower pressures. We examined pressures under 3.8cm-wide, 5.1cm-wide, and side-by-side-3.8cm-wide nonelastic strap-based tourniquets.
METHODS:
Ratcheting Medical Tourniquets (RMT) were applied mid-thigh and mid-arm for 120 seconds with Doppler-indicated occlusion. The RMTs were a Single Tactical RMT (3.8cm-wide), a Wide RMT (5.1cm-wide), and Paired Tactical RMTs (7.6cm-total width). Tightening completion was measured at one-tooth advance past arterial occlusion, and paired applications involved alternating tourniquet tightening.
RESULTS:
All 96 applications on the 16 recipients reached occlusion. Paired tourniquets had the lowest occlusion pressures (ρ < .05). All pressures are given as median mmHg, minimum-maximum mmHg. Thigh application occlusion pressures were Single 256, 219-299; Wide 259, 203-287; Distal of Pair 222, 183-256; and Proximal of Pair 184, 160-236. Arm application occlusion pressures were Single 230, 189-294; Wide 212, 161-258; Distal of Pair 204, 193-254, and Proximal of Pair 168, 148-227. Pressure increases with the final tooth advance were greater for the 2 teeth/cm Wide than for the 2.5 teeth/cm Tacticals (ρ < .05). Thigh final tooth advance pressure increases were Single 40, 33-49; Wide 51, 37-65; Distal of Pair 13, 1-35; and Proximal of Pair 15, 0-30. Arm final tooth advance pressure increases were Single 49, 41-71; Wide 63, 48-77; Distal of Pair 3, 0-14; and Proximal of Pair 23, 2-35. Pressure decreases occurred under all tourniquets over 120 seconds. Thigh pressure decreases were Single 41, 32-75; Wide 43, 28-62; Distal of Pair 25, 16-37; and Proximal of Pair 22, 15-37. Arm pressure decreases were Single 28, 21-43; Wide 26, 16-36; Distal of Pair 16, 12-35; and Proximal of Pair 12, 5-24. Occlusion losses before 120 seconds occurred predominantly on the thigh and with paired applications (ρ < .05). Occlusion losses occurred in six Paired thigh applications, two Single thigh applications, and one Paired arm application.
CONCLUSIONS:
Side-by-side tourniquets achieve occlusion at lower pressures than single tourniquets. Additionally, pressure decreases undertourniquets over time; so all tourniquet applications require reassessments for continued effectiveness.
| Tags : tourniquet
01/09/2016
Pensez, efficace et peu couteux
Cognitive skills analysis, kinesiology, and mental imagery in the acquisition of surgical skills
Bathalon S. et Al. J Otolaryngol. 2005 Oct;34(5):328-32.
--------------------------------------------
Un moyen simple pour améliorer sa performance
--------------------------------------------
GOAL:
Isolate and evaluate the impact of mental imagery on the acquisition of an emergency surgical technique.
METHOD:
We studied 44 first-year medical students performing a cricothyrotomy on a mannequin to determine the impact of teaching usingmental imagery (MI) and/or kinesiology (KG) compared to the standard Advandec Trauma Life Support (ATLS) approach. Students were randomly assigned to one of three groups: MI and KG, KG alone or control (ATLS). Two weeks after the one-hour teaching session, they were evaluated with an OSCE testing the performance of the different steps of the technique, the time required and its fluidity.
RESULTS:
Total results (maximum: 25 marks) are as follows: KG + MI = 20.3 +/- 1.5 ; KG = 19.3 +/- 2.9 ; ATLS = 18.2 +/- 2.5. The only statistically significant difference for total results was in the use of MI and KG compared to the control group. Kinesiology alone or with mental imageryimproved the fluidity of the performance.
CONCLUSION:
Many factors influence the acquisition of a surgical technique. This study showed that acquisition and performance of an emergency procedure (cricothyrotomy) was improved when mental imagery and kinesiology were combined to teach it.
Médecine de catastrophe en France