31/08/2016
Pratique gestuelle pour l'opex: Quel minimum ?
Garrison Clinical Setting Inadequate for Maintenance of Procedural Skills for Emergency Medicine Physicians: A Cross-Sectional Study
Schauer SG et Al. J Spec Oper Med. 2015 Winter;15(4):67-70.
--------------------------------
Une estimation pertinente concernant les prérequis nécessaires à un médecin appelé à exercer en situation d'isolement et elle émane d'une institution dont la pierre angulaire de la prise en charge des blessés repose initialement sur le concept du paramedic.
--------------------------------
BACKGROUND:
Emergency medicine physicians (EPs) are often placed in far-forward, isolated areas in theater. Maintenance of their emergency intervention skills is vital to keep the medical forces deployment ready. The US Army suggests that working at a Military Treatment Facility (MTF) is sufficient to keep emergency procedural skills at a deployment-ready level. We sought to compare the volume of emergency procedures that providers reported necessary to maintain their skills with the number available in the MTF setting.
METHODS:
EPs were surveyed to quantify the number of procedures they reported they would need to perform yearly to stay deployment-ready. We obtained procedure data for their duty stations and compared the procedure volume with the survey responses to determine if working at an MTF is sufficient to keep providers' skills deployment ready.
RESULTS:
The reported necessary average numbers per year were as follows: tube thoracostomy (5.9), intubation (11.4), cricothyrotomy (4.2), lumbar puncture (5.2), central line (10.0), focused assessment with sonography for trauma (FAST) (21.3), reductions (10.6), splints (10.5), and sedations (11.7). None of the procedure volumes at MTFs met provider requirements with the exception of FAST examinations at the only trauma center.
CONCLUSIONS:
This suggests the garrison clinical environment is inadequate for maintaining procedure skills. Further research is needed to determine modalities that will provide adequate training volume.
Echo et voies aériennes: Mais oui, à maîtriser
The Role of Airway and Endobronchial Ultrasound in Perioperative Medicine
Vortrua J et Al. Biomed Res Int. 2015; 2015: 754626
-------------------------------
Certainement UN APPORT IMPORTANT à la gestion des voies aériennes et de la ventilation non seulement dans les blocs opératoires mais dans les situations critiques y compris hors de l'hôpital.
-------------------------------
Recent years have witnessed an increased use of ultrasound in evaluation of the airway and the lower parts of the respiratory system. Ultrasound examination is fast and reliable and can be performed at the bedside and does not carry the risk of exposure to ionizing radiation. Apart from use in diagnostics it may also provide safe guidance for invasive and semi-invasive procedures. Ultrasound examination of the oral cavity structures, epiglottis, vocal cords, and subglottic space may help in the prediction of difficult intubation. Preoperative ultrasound may diagnose vocal cord palsy or deviation or stenosis of the trachea. Ultrasonography can also be used for confirmation of endotracheal tube, double-lumen tube, or laryngeal mask placement. This can be achieved by direct examination of the tube inside the trachea or by indirect methods evaluating lung movements. Postoperative airway ultrasound may reveal laryngeal pathology or subglottic oedema. Conventional ultrasound is a reliable real-time navigational tool for emergency cricothyrotomy or percutaneous dilational tracheostomy. Endobronchial ultrasound is a combination of bronchoscopy and ultrasonography and is used for preoperative examination of lung cancer and solitary pulmonary nodules. The method is also useful for real-time navigated biopsies of such pathological structures.
| Tags : airway
Crico avec un stylo ? NON
Bystander cricothyrotomy with ballpoint pen: a fresh cadaveric feasibility study
Kisser U. et Al. Emerg Med J. 2016 Aug;33(8):553-6.
OBJECTIVE:
In motion pictures and anecdotal reports, ballpoint pens have been used for life-saving cricothyroidotomies. The objective of this study was to examine the widespread belief that ballpoint pens can perforate the skin and cricothyroid ligament and could be used as substitute tracheostomy sets in an emergency setting.
METHODS:
Three different ballpoint pens were examined regarding their inner diameter, their demountability to form a cannula and their airflow properties. Ten medical laypersons were asked to try to puncture the trachea through the skin and the cricothyroid ligament in 10 fresh cadavers just using the ballpoint pens.
RESULTS:
Two of three pens had inner diameters of >3 mm and were both suitable as cannulas in a tracheotomy. All participants could perforate the skin with both ballpoint pens. However, almost no one could penetrate through the cricothyroid ligament or the ventral wall of the trachea, except for one participant. He performed the tracheostomy after three attempts in >5 min with a lot of patience and force.
CONCLUSIONS:
A cricothyroidotomy just with a ballpoint pen is virtually impossible. First, the airflow resistance in commercially available ballpoint pens is too high to produce effective ventilation. Second, the cricothyroid ligament is too strong to be penetrated by ballpoint pens.
| Tags : airway
30/08/2016
Crico et Echo: Pensez TACA
Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact
Kristensen MS et Al. Br. J. Anaesth. (2016) 117 (suppl 1):i39-i48
Inability to identify the cricothyroid membrane by inspection and palpation contributes substantially to the high failure rate of cricothyrotomy. This narrative review summarizes the current evidence for application of airway ultrasonography for identification of the cricothyroid membrane compared with the clinical techniques. We identified the best-documented techniques for bedside use, their success rates, and the necessary training for airway-ultrasound-naïve clinicians.

After a short but structured training, the cricothyroid membrane can be identified using ultrasound in difficult patients by previously airway-ultrasound naïve anaesthetists with double the success rate of palpation. Based on the literature, we recommend identifying the cricothyroid membrane before induction of anaesthesia in all patients. Although inspection and palpation may suffice in most patients, the remaining patients will need ultrasonographic identification; a service that we should aim at making available in all locations where anaesthesia is undertaken and where patients with difficult airways could be encountered.
| Tags : airway
Crico: Maintenir son savoir, pas gagné !
Out-of-Hospital Surgical Airway Management: Does Scope of Practice Equal Actual Practice?
Furin M. et Al. West J Emerg Med. 2016 May;17(3):372-6
------------------------------
La coniotomie est un geste dont la réalisation est rare. Il existe actuellement un regain d'intérêt pour la maîtrise de cette pratique. Encore faut il avoir la démarche d'entretenir ses pratiques. On part de loin, c'est ce que met en valeur ce travail.
------------------------------
INTRODUCTION:
Pennsylvania, among other states, includes surgical airway management, or cricothyrotomy, within the paramedic scope of practice. However, there is scant literature that evaluates paramedic perception of clinical competency in cricothyrotomy. The goal of this project is to assess clinical exposure, education and self-perceived competency of ground paramedics in cricothyrotomy.
METHODS:
Eighty-six paramedics employed by four ground emergency medical services agencies completed a 22-question written survey that assessed surgical airway attempts, training, skills verification, and perceptions about procedural competency. Descriptive statistics were used to evaluate responses.
RESULTS:
Only 20% (17/86, 95% CI [11-28%]) of paramedics had attempted cricothyrotomy, most (13/17 or 76%, 95% CI [53-90%]) of whom had greater than 10 years experience. Most subjects (63/86 or 73%, 95% CI [64-82%]) did not reply that they are well-trained to perform cricothyrotomy and less than half (34/86 or 40%, 95% CI [30-50%]) felt they could correctly perform cricothyrotomy on their first attempt. Among subjects with five or more years of experience, 39/70 (56%, 95% CI [44-68%]) reported 0-1 hours per year of practical cricothyrotomy training within the last five years.

How much and what type of training have you had in prehospital cricothyrotomy in the past 1 year and the past 5 years?
Half of the subjects who were able to recall (40/80, 50% 95% CI [39-61%]) reported having proficiency verification for cricothyrotomy within the past five years.
CONCLUSION:
Paramedics surveyed indicated that cricothyrotomy is rarely performed, even among those with years of experience. Many paramedics felt that their training in this area is inadequate and did not feel confident to perform the procedure. Further study to determine whether to modify paramedic scope of practice and/or to develop improved educational and testing methods is warranted.
| Tags : airway
29/08/2016
Anatomie cricoïdienne
Topographical anatomy of cricothyroid membrane and its relation with invasive airway access.
Develi S. et Al. Clin Anat. 2016 Aug 2. doi: 10.1002/ca.22750
-----------------------------
On enseigne que l'abord cricothyroïdien est sécuritaire, notamment concernnant le risuqe de ponctions vasculaires. Cela est vrai surtout pour sa partie inférieure et tout partiuclièrement son quadran inférieur droit.
-----------------------------
Cricothyroidotomy is a surgical procedure involving penetration through the skin and cricothyroid membrane to maintain airway patency during life-threatening emergency conditions. Complications such as bleeding and laryngeal stenosis can result from it. Our aim in this study was to identify the anatomical structures located on the membrane and to ascertain whether there is a safe area on the membrane for this procedure. Thirty larynx specimens fixed with 10% formaldehyde in the Department of Anatomy were dissected. The cricothyroid artery, the cricothyroid vein, the common artery and vein formed by the cricothyroid vessels, the pyramidal lobe of the thyroid gland and lymph nodes were observed on the membrane. The cricothyroid membrane was divided into four quadrants and the most common locations of these anatomical structures on the membrane were recorded.
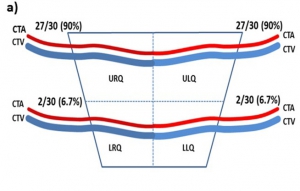
The cricothyroid artery and vein were located on the upper half of the membrane, the common vein was found in the midline, coursing to the thyroid gland, and the lobus pyramidalis and lymph nodes were located on the left side of the midline. Overall, the anatomical structures were mostly located on the upper half and lower left quadrant of the cricothyroid membrane. Thus, the lower right quadrant seems safer for invasive procedures such as needle cricothyroidotomy or other cannulation techniques. Needle puncture or cannulation through the lower right quadrant of the cricothyroid membrane will injure fewer anatomical structures so there should be fewer complications due to degradation of the vascular supply to this region
Echographie: Un outil pour la gestion des VAS
Role of upper airway ultrasound in airway management
Osman A. et Al. Osman and Sum Journal of Intensive Care (2016) 4:52
Upper airway ultrasound is a valuable, non-invasive, simple, and portable point of care ultrasound (POCUS) for evaluation of airway management even in anatomy distorted by pathology or trauma. Ultrasound enables us to identify important sonoanatomy of the upper airway such as thyroid cartilage, epiglottis, cricoid cartilage, cricothyroid membrane, tracheal cartilages, and esophagus. Understanding this applied sonoanatomy facilitates clinician to use ultrasound in assessment of airway anatomy for difficult intubation, ETT and LMA placement and depth, assessment of airway size, ultrasound-guided invasive procedures such as percutaneous needle cricothyroidotomy and tracheostomy, prediction of postextubation stridor and left double-lumen bronchial tube size, and detecting upper airway pathologies. Widespread POCUS awareness, better technological advancements, portability, and availability of ultrasound in most critical areas facilitate upper airway ultrasound to become the potential first-line non-invasive airway assessment tool in the future.
| Tags : intubation
27/08/2016
Interventions salvatrices: Bien sûr mais lesquelles ?
Major incident triage: A consensus based definition of the essential life-saving interventions during the definitive care phase of a major incident
Vassallo J. et Al. Injury, Int. J. Care Injured 47 (2016) 1898–190
-------------------------
Plus le contexte d'intervention est difficile soit du fait de l'environnement soit du fait du danger tactique et plus le choix des nterventions médicales doit être réflechi et restreint et mis en oeuvre par uintervenant pas forcément médecin mas formé spécifiquement à la pratique d'une action nécessaire à la survie. Ce travail identiife ainsi une trentaine de conduites essentielles à un réseau de traumatisés graves. Lire aussi cet article
-------------------------
Introduction: Triage is a key principle in the effective management of major incidents. The process currently relies on algorithms assigning patients to specific triage categories; there is, however, little guidance as to what these categories represent. Previously, these algorithms were validated against injury severity scores, but it is accepted now that the need for life-saving intervention is a more important outcome. However, the definition of a life-saving intervention is unclear. The aim of this study was to define what constitutes a life-saving intervention, in order to facilitate the definition of an adult priority one patient during the definitive care phase of a major incident.
Methods: We conducted a modified Delphi study, using a panel of subject matter experts drawn from the United Kingdom and Republic of South Africa with a background in Emergency Care or Major Incident Management. The study was conducted using an online survey tool, over three rounds between July and December 2013. A four point Likert scale was used to seek consensus for 50 possible interventions, with a consensus level set at 70%.
Results: 24 participants completed all three rounds of the Delphi, with 32 life-saving interventions reaching consensus.
Conclusions: This study provides a consensus definition of what constitutes a life-saving intervention in the context of an adult, priority one patient during the definitive care phase of a major incident. The definition will contribute to further research into major incident triage, specifically in terms of validation of an adult major incident triage tool.
| Results of the Delphi Process – Life-Saving Interventions. | |
| 1 | Intubation for actual airway obstruction |
| 2 | Intubation for impending airway obstruction |
| 3 | Surgical airway for airway obstruction |
| 4 | Surgical airway for impending airway obstruction |
| 5 | Needle thoracocentesis |
| 6 | Finger thoracostomy |
| 7 | Tube thoracostomy |
| 8 | Application of a chest seal (commercial/improvised) |
| 9 | Positive Pressure Ventilation for ventilatory inadequacy |
| 10 | Application of a tourniquet for haemorrhage control |
| 11 | Use of haemostatic agents for haemorrhage control |
| 12 | Insertion of an intra-osseous device for resuscitation purposes |
| 13 | Receiving uncross-matched blood |
| 14 | Receiving≥4 units of blood/blood products |
| 15 | Administration of tranexamic acid |
| 16 | Laparotomy for trauma |
| 17 | Thoracotomy for trauma |
| 18 | Pericardial window for trauma |
| 19 | Surgery to gain proximal vascular control |
| 20 | Interventional radiology for haemorrhage control |
| 21 | Application of a pelvic binder |
| 22 | ALS/ACLS protocols for a patient in a peri-arrest situation |
| 23 | ALS/ACLS protocols for a patient in cardiac arrest |
| 24 | Neurosurgery for the evacuation of an intra-cranial haematoma |
| 25 | Craniotomy |
| 26 | Burr Hole Insertion |
| 27 | Spinal nursing for a C1-3 fracture |
| 28 | Administration of a seizure-terminating medication |
| 29 | Active rewarming for initial core temp<32° celcius |
| 30 | Passive rewarming for initial core temp<32° celcius |
| 31 | Correction of low blood glucose |
| 32 | Administration of chemical antidotes |
| Tags : triage
25/08/2016
Réchauffer une perfusion: La tubulure +++
An Analysis of the Temperature Change in Warmed Intravenous Fluids during Administration in a Cold Environment at Temperatures of Less than 0
2016 Critical Care Transport Medicine Conference Scientific Forum
SIngleton W et Al. Air Medical Journal 35 (2016) 205-207
Objective: This is a non-human simulation study determining the decrease in temperature that occurred to 1L bags of Normal Saline in an austere environment. The bags were warmed to 38°C (100°F), administered through standard intravenous tubing at a set flow rate, while in an environment with ambient temperatures of less than 0°C (32°F). The goal was to determine if there was a significant decrease in fluid temperature from the IV bag through the tubing to the IV catheter administration site.
Methods/Materials: Three trials were run at four different temperatures, 0°C (32°F), -7 °C (20°F), -12°C (10°F ) and 33°C (72°F control ). Each bag of normal saline was warmed to the same temperature 38°C (100°F) utilizing the Soft Sack IV Fluid Warmer. Three of the bags were then placed in a cold austere environment (freezer) at each of the specified temperatures. The remaining bag was kept in the ambient temperature 33°C (72°F control). The fluid was administered through standard intravenous tubing (18 gauge catheter, 20 drop set, 211 cm in length) at a flow rate of 999ml/hr in temperatures less than 0°C (32°F). Fluid was collected in a glass container outside the austere environment with the temperature being recorded at 5 minute intervals.
Results: The results demonstrated a statistically significant (p> 0.05) change in temperature between the IV bag and the administration site. The most rapid change occurred within the first 5 minutes. The temperature change was more significant with the colder ambient temperatures, with an average of 50° difference at -7°C (20°F) and -12°C (10°F ). This is compared to a 27° difference at 0°C and the control temperature of 33°C (72°F control). The temperature of the fluid remaining within the IV bag also decreased an average of 15°C at the control temperature of 33°C (72°F control) and 0°C (32°F), which is statistically significant. The temperature in the bag decreased an average of 35°C at -7°C (20°F) and -12°C (10°F), which was statistically significant (p>0.05).
Conclusion: Based on these results, it appears that the most significant heat loss occurs through the IV tubing itself, the loss occurs rapidly, and is more pronounced at colder ambient air temperatures. Therefore, it may be beneficial to insulate the tubing on a trauma patient receiving warmed IV fluids in a cold environment of less than 0°C (32°F) to help prevent hypothermia.
11/08/2016
Transfusion, Thrombosis and Bleeding Management
Special Issue: Transfusion, Thrombosis and Bleeding Management
January 2015 - Volume 70, Issue Supplement s1 - Pages 1–e41
Clic sur l'image pour accéder au numéro en ligne
Blood – the most important humour? (pages 1–e1)
C. R. Bailey, A. A. Klein and B. J. Hunt
Version of Record online: 1 DEC 2014 | DOI: 10.1111/anae.12930
Review Articles
L. Green, S. Allard and R. Cardigan
☛ CPD available at http://www.learnataagbi.org
Corrected by:
Corrigendum: Modern banking, collection, compatibility testing and storage of blood and blood components
Vol. 70, Issue 3, 373, Version of Record online: 11 FEB 2015
Evidence and triggers for the transfusion of blood and blood products (pages 10–e3)
A. Shah, S. J. Stanworth and S. McKechnie
Pre-operative anaemia (pages 20–e8)
B. Clevenger and T. Richards
The pathophysiology and consequences of red blood cell storage (pages 29–e12)
D. Orlov and K. Karkouti
Red cell transfusion and the immune system (pages 38–e16)
S. Hart, C. M. Cserti-Gazdewich and S. A. McCluskey
The current place of aprotinin in the management of bleeding (pages 46–e17)
D. Royston
The current place of tranexamic acid in the management of bleeding (pages 50–e18)
B. J. Hunt
Practical management of major blood loss (pages 54–e20)
R. Gill
Management of peri-operative anti-thrombotic therapy (pages 58–e23)
J. J. van Veen and M. Makris
Laboratory monitoring of haemostasis (pages 68–e24)
A. Fowler and D. J. Perry
Point-of-care monitoring of haemostasis (pages 73–e26)
S. V. Mallett and M. Armstrong
Haemostatic management of obstetric haemorrhage (pages 78–e28)
R. E. Collis and P. W. Collins
Haemostatic management of cardiac surgical haemorrhage (pages 87–e31)
M. W. Besser, E. Ortmann and A. A. Klein
The pathogenesis of traumatic coagulopathy (pages 96–e34)
A. Cap and B. J. Hunt
Management of traumatic haemorrhage – the European perspective (pages 102–e37)
H. Schöchl, W. Voelckel and C. J. Schlimp
Management of traumatic haemorrhage – the US perspective (pages 108–e38)
R. P. Dutton
Surgery in patients with inherited bleeding disorders (pages 112–e40)
P. K. Mensah and R. Gooding
The management of abnormal haemostasis in the ICU (pages 121–e41)
A. Retter and N. A. Barrett
05/08/2016
Echo pour abord vasculaire: Intérêt modéré ?
Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization
Cochrane Database Syst Rev. 2015 Jan 9;1:CD011447. doi: 10.1002/14651858.CD011447.
-------------------------------------
La mise en place d'un abord veineux central est une éventualité peu fréquente en médecine tactique. La maîtrise de l'abord vasculaire périphérique et l'apport de la perfusion intraosseuse suffisent le plus souvent à répondre aux besoins. Néanmoins ce besoin ne peut être écarté. Alors que la majorité des sociétés savantes recommandent le recours à la pose échoguidée, il semblerait qu'une analyse critique de l'intérêt d'une telle pratique ne soit pas encore complètement en faveur de telles recommandations (???). Même si de très grandes avancées technologiques ont lieu et permettent de disposer d'appareil et de sondes adhoc utilisables hors de l'hôpital, dans nos conditions d'exercice et donc in fine de notre aptitude à cette pratique sans échographe.
-------------------------------------
BACKGROUND:
Central venous catheters can help with diagnosis and treatment of the critically ill. The catheter may be placed in a large vein in the neck (internal jugular vein), upper chest (subclavian vein) or groin (femoral vein). Whilst this is beneficial overall, inserting the catheter risks arterial puncture and other complications and should be performed in as few attempts as possible.In the past, anatomical 'landmarks' on the body surface were used to find the correct place to insert these catheters, but ultrasound imaging is now available. A Doppler mode is sometimes used to supplement plain 'two-dimensional' ultrasound.
OBJECTIVES:
The primary objective of this review was to evaluate the effectiveness and safety of two-dimensional ultrasound (US)- or Dopplerultrasound (USD)-guided puncture techniques for subclavian vein, axillary vein and femoral vein puncture during central venous catheter insertion in adults and children. We assessed whether there was a difference in complication rates between traditional landmark-guided and any ultrasound-guided central vein puncture.When possible, we also assessed the following secondary objectives: whether a possible difference could be verified with use of the US technique versus the USD technique; whether there was a difference between using ultrasound throughout the puncture ('direct') and using it only to identify and mark the vein before starting the puncture procedure ('indirect'); and whether these possible differences might be evident in different groups of patients or with different levels of experience among those inserting the catheters.
SEARCH METHODS:
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 1), MEDLINE (1966 to 15 January 2013), EMBASE (1966 to 15 January 2013), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 15 January 2013), reference lists of articles, 'grey literature' and dissertations. An additional handsearch focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings. We attempted to identify unpublished or ongoing studies by contacting companies and experts in the field, and we searched trial registers. We reran the search in August 2014. We will deal with any studies of interest when we update the review.
SELECTION CRITERIA:
Randomized and quasi-randomized controlled trials comparing two-dimensional ultrasound or Doppler ultrasound versusan anatomical 'landmark' technique during insertion of subclavian or femoral venous catheters in both adults and children.
DATA COLLECTION AND ANALYSIS:
Three review authors independently extracted data on methodological quality, participants, interventions and outcomes of interest using a standardized form. We performed a priori subgroup analyses.
MAIN RESULTS:
Altogether 13 studies enrolling 2341 participants (and involving 2360 procedures) fulfilled the inclusion criteria. The quality of evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most of the trials had unclear risk of bias across the six domains, and heterogeneity among the studies was significant. For the subclavian vein (nine studies, 2030 participants, 2049 procedures), two-dimensional ultrasound reduced the risk of inadvertent arterial puncture (three trials, 498 participants, risk ratio (RR) 0.21, 95% confidence interval (CI) 0.06 to 0.82; P value 0.02, I² = 0%) and haematoma formation (three trials, 498 participants, RR 0.26, 95% CI 0.09 to 0.76; P value 0.01, I² = 0%). No evidence was found of a difference in total or other complications (together, US, USD), overall (together, US, USD), number of attempts until success (US) or first-time (US) success rates or time taken to insert the catheter (US). For the femoral vein, fewer data were available for analysis (four studies, 311 participants, 311 procedures). No evidence was found of a difference in inadvertent arterial puncture or other complications. However, success on the first attempt was more likely with ultrasound (three trials, 224 participants, RR 1.73, 95% CI 1.34 to 2.22; P value < 0.0001, I² = 31%), and a small increase in the overall success rate was noted (RR 1.11, 95% CI 1.00 to 1.23; P value 0.06, I² = 50%). No data on mortality or participant-reported outcomes were provided.
AUTHORS' CONCLUSIONS:
On the basis of available data, we conclude that two-dimensional ultrasound offers small gains in safety and quality when compared with an anatomical landmark technique for subclavian (arterial puncture, haematoma formation) or femoral vein (success on the first attempt) cannulation for central vein catheterization. Data on insertion by inexperienced or experienced users, or on patients at high risk for complications, are lacking. The results for Doppler ultrasound techniques versus anatomical landmark techniques are uncertain.
04/08/2016
Le cône d'apprentissage de Dale: Quèsaco ?
J'entends et j'oublie,
Je vois et je me souviens,
Je fais et je comprends

03/08/2016
Echographie clinique en médecine d'urgence
Premier niveau de compétence pour l'échographie clinique en médecine d’urgence
Recommandations de la Société française de médecine d’urgence par consensus formalisé.
Société française de médecine d’urgence 2016
clic sur l'image pour accéder au document
| Tags : échographie
01/08/2016
La guerre, et après ?
| Tags : ptsd

1365-2044/asset/olbannerleft.gif?v=1&s=bd83df57543a1d11ffc15f630bb1301f0be80859)