21/06/2025
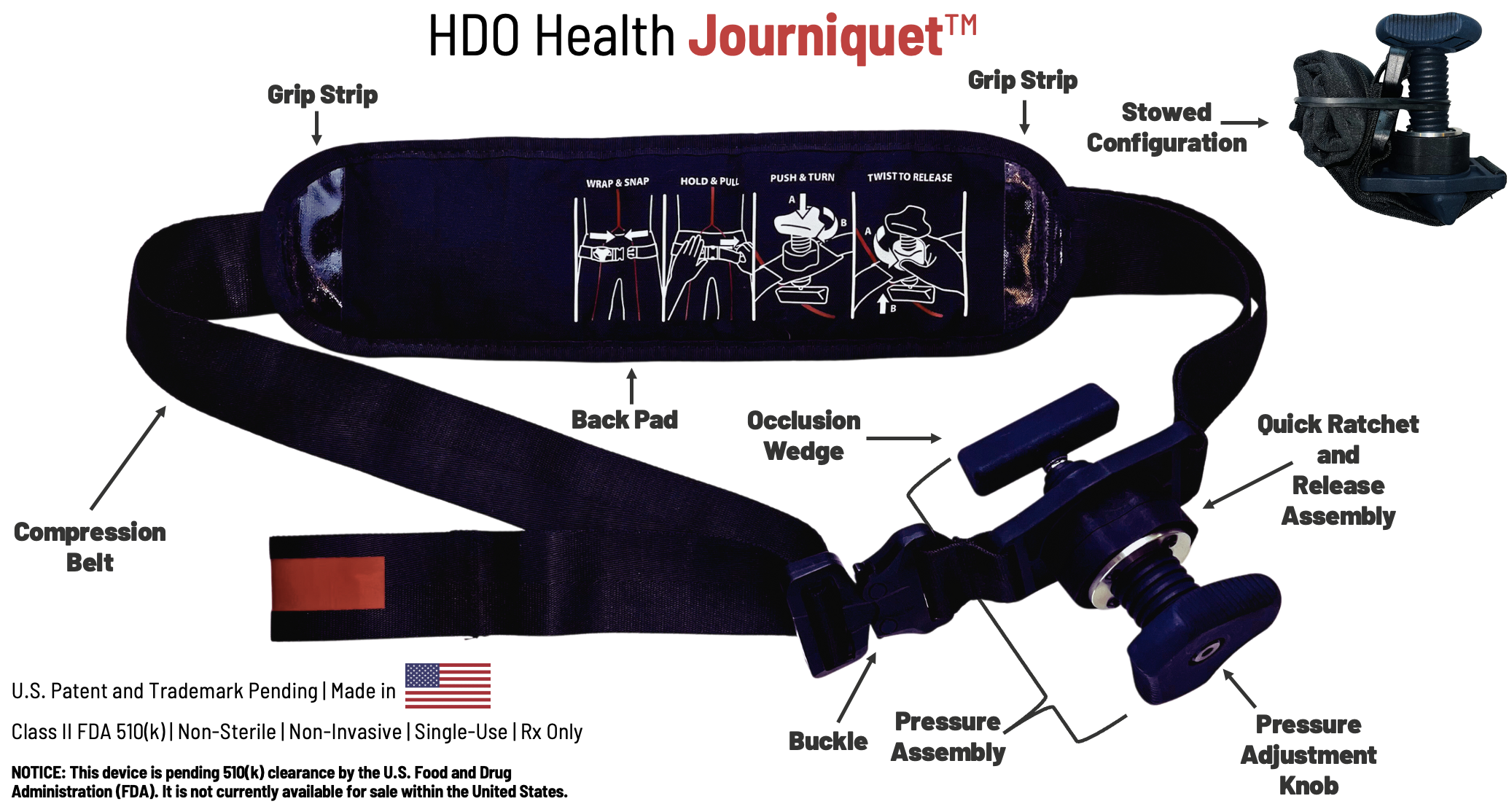
Tourniquet jonctionnel: Un nouveau venu, le Journiquet
01/05/2025
Tourniquet Abdominal: Probablement très utile.
Successful Management of Battlefield Traumatic Cardiac Arrest Using the Abdominal Aortic and Junctional Tourniquet (AAJT): A Case Series
Androshchuk D et Al. Case Reports J Spec Oper Med. 2025 Apr 4;25(1):65-69.
The Russo-Ukrainian war's prolonged warfare, resource constraints, and extended evacuation times have forced significant adaptations in Ukraine's medical system - including technological advancements and strategic resource placement. This study examined if the Abdominal Aortic and Junctional Tourniquet - Stabilized (AAJT-S) could manage traumatic cardiac arrest (TCA) at forward surgical stabilization sites (FSSS) as an adjunct to damage control surgery. Six patients in severe hypovolemic shock presented at an FSSS during fighting in Bakhmut (July 2022) and Slovyansk (May 2023). Following TCA due to exsanguination, the AAJT-S was applied 2cm below the umbilicus. Cardiopulmonary resuscitation (CPR) and transfusion (blood and/or plasma) were initiated. All six patients were resuscitated. None required vasopressor support post-resuscitation. Five survived to the next level of care. One died awaiting evacuation, and another of wounds after 10 days. Four survived to discharge. Three were followed and neurologically intact, and no death records matched the fourth's name and date of birth at 18 months. Follow-up was limited, but one patient was neurologically intact at one year. The AAJT-S effectively resuscitated TCA patients. It increased mean arterial pressure, focused resuscitative efforts on the upper torso, simplified care, and preserved crucial field resources. An alternative to traditional emergency thoracotomy, AAJT-S could replace or complement resuscitative endovascular balloon occlusion of the aorta in pre-hospital settings, given its ease of application by combat medics. AAJT-S, alongside blood transfusion and CPR, achieved 100% success in return of spontaneous circulation and effectively managed TCA in a wartime FSSS.
11/02/2025
Effets du garrot: temps dépendant !
Timeline effects of tourniquets used in trauma care
Pascoe B et Al. JHTAM. 2024;6(2):26-32
"After reviewing current evidence, having evacuation protocols which ensure tourniquets are only required to be applied for an upper window of two hours would be a safe guideline to work with. Prioritising the evacuation of patients to ensure they are moved to a facility where tourniquets are able to be removed within the upper limit of two hours, would minimise the risk of serious co-morbidities and maximise the chance for full recovery. In addition to this, improving education on the correct use and application of the tourniquet would also improve patient outcomes."

17/01/2025
Conflit ukrainien: Pour de la chirurgie encore plus proche des combats
09/10/2024
REBOA préhospitalier: Attention !
Vascular complications secondary to resuscitative endovascular balloon occlusion of the aorta placement at a Level 1 Trauma Center
Tullos A et Al. J Vasc Surg. 2024 Jul;80(1):64-69
--------------------------------------------------------
Une technique dont on comprend l'intérêt théorique. Mais la vraie vie semble un peu différente. La mise en place d'un REBOA nécessite la présence d'une équipe chirurgicale très proche et ce n'est pas le cas le plus souvent en condition de combat.. L'environnement nécessaire au succès de cette technique n'est pas, le plus souvent, présent.
-------------------------------------------------------
Objective:
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is designed to manage
severe hemorrhagic shock. Popularized in medical care during military conflicts, the concept has emerged as a lifesaving technique that is utilized around the United States. Literature on risks of REBOA placement, especially vascular injuries, are not well-reported. Our goal was to assess the incidence of vascular injury from REBOA placement and the risk factors associated with injury and death among these patients at our institution.
Methods:
We performed a retrospective cohort study of all patients who underwent REBOA placement between September 2017 and June 2022 at our Level 1 Trauma Center. The primary outcome variable was the presence of an injury related to REBOA insertion or use. Secondary outcomes studied were limb loss, the need for dialysis, and mortality. Data were analyzed using descriptive statistics, χ2, and t-tests asappropriate for the variable type.
Results:
We identified 99 patients who underwent REBOA placement during the study period. The mean
age of patients was 43.1 ± 17.2 years, and 67.7% (67/99) were males. The majority of injuries were from blunt trauma (79.8%; 79/99). Twelve of the patients (12.1%; 12/99) had a vascular injury related to REBOA placement. All but one required intervention. The complications included local vessel injury (58.3%; 7/12), distal embolization (16.7%; 2/12), excessive bleeding requiring vascular consult (8.3%; 1/12), pseudoaneurysm requiring intervention (8.3%; 1/12), and one incident of inability to remove the REBOA device (8.3%; 1/12). The repairs were performed by vascular surgery (75%; 9/12), interventional radiology (16.7%; 2/12), and trauma surgery (8.3%; 1/12). There was no association of age, gender, race, and blunt vs penetrating injury to REBOA-related complications. Mortality in this patient population was high (40.4%), but there was no association with REBOA-related complications. Ipsilateral limb loss occurred in two patients with REBOA-related injuries, but both were due to their injuries and not to REBOA-related ischemia.
Conclusions:
Although vascular complications are not unusual in REBOA placement, there does not appear to be an association with limb loss, dialysis, or mortality if they are addressed promptly. Close
coordination between vascular surgeons and trauma surgeons is essential in patients undergoing REBOA placement
Tourniquet en milieu froid: Des spécificités
Analysis of tourniquet pressure over military winter clothing and a short review of combat casualty care in cold weather warfare
Cold weather warfare is of increasing importance. Haemorrhage is the most common preventable cause of death in military conflicts. We analysed the pressure of the Combat Application Tourniquet® Generation 7 (CAT), the SAM® Extremity Tourniquet (SAMXT) and the SOF® Tactical Tourniquet Wide Generation 4 (SOFTT) over different military cold weather clothing setups with aleg tourniquet trainer. We conducted a selective PubMed search and supplemented this with own experiences in cold weather medicine. The CAT and the SAMXT both reached the cut off value of 180 mmHg in almost all applications. The SOFTT was unable to reach the 180 mmHg limit in less than 50% of all applications in some clothing setups. We outline the influence of cold during military operations by presenting differences between military and civilian cold exposure. We propose a classification of winter warfare and identify caveats and alterations of Tactical CombatCasualty Care in cold weather warfare, with a special focus on control of bleeding. The application of tourniquets over military winter clothing is successful in principle, but effectiveness may vary for different tourniquet models. Soldiers are more affected and impaired by cold than civilians. Militaryc ommanders must be made aware of medical alterations in cold weather warfare.
01/10/2024
REBOA préhospitalier: Une mortalité inchangée à 30 j, désillusion ?
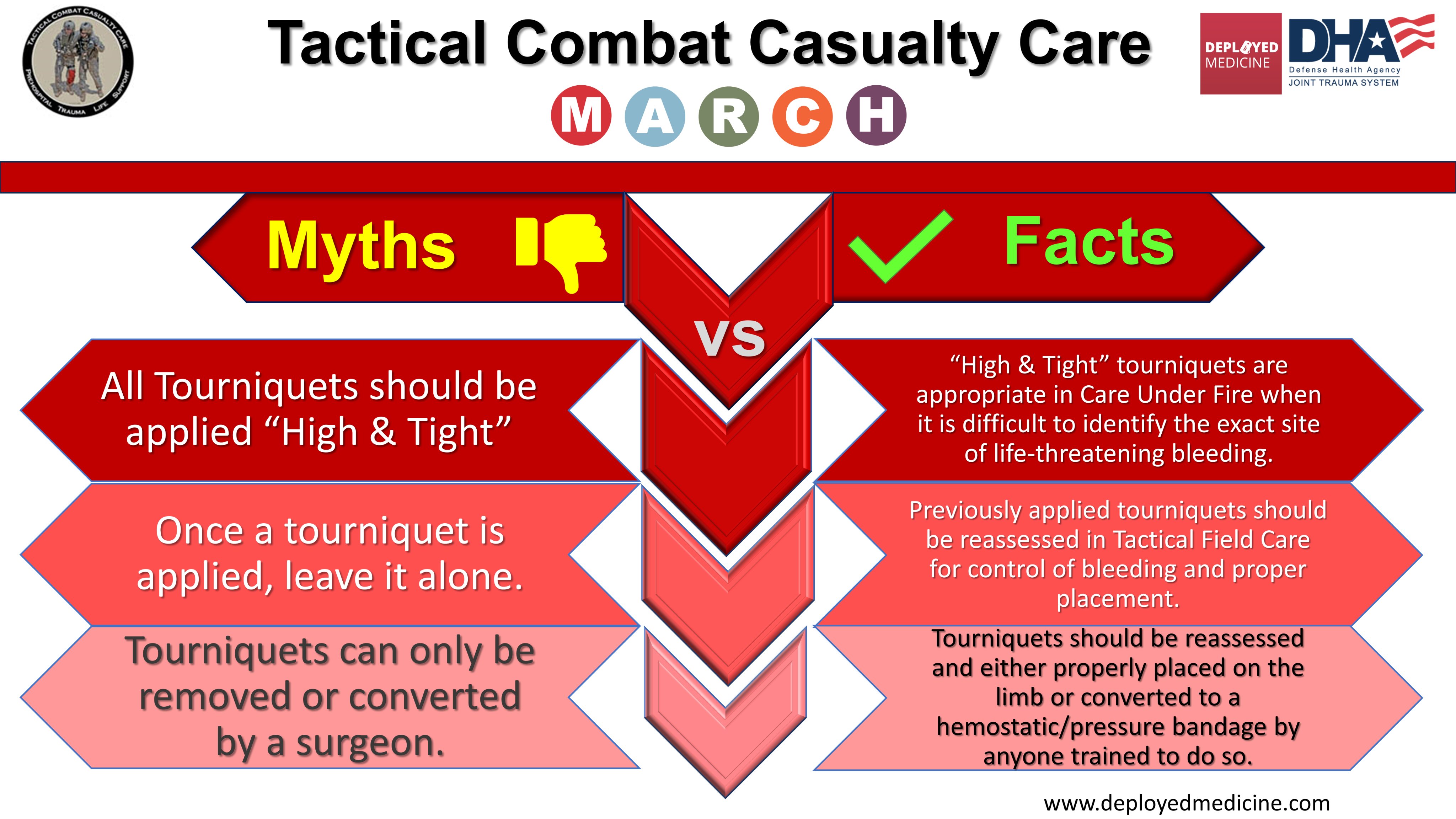
Poser un garrot: Pas n'importe comment !
Who needs a tourniquet? And who does not? Lessons learned from a review of tourniquet use in the Russo-Ukrainian war
24/09/2024
Tourniquet: Point d'étape 2023
Rethinking limb tourniquet conversion in the prehospital environment
Holcomb JB et Al. J Trauma Acute Care Surg. 2023 Dec; 95(6): e54–e60.
23/09/2024
Garrot automatique: En préhospitalier ?
Le garrot XMETIX 7
Les garrots automatiques sont quotidiennement utilisés dans les blocs opératoires, essentiellement des garrots alimentés par de petits dispositifs de compression électrique parfaitement régulés. Ce garrot miniaturisé fonctionne donc sur batterie avec une autonomie donnée pour 5 heures et générant une pression d'occlusion automatiquement régulée pouvant aller jusqu'à 300 mmHg .
C'est un garrot mécanique qui va mettre en tension une sangle grâce à un micromoteur électrique.
On ne trouve pas pour l'instant d'analyse indépendante sur la performance de ce tourniquet donc le concept est intéressant. On peut quand même se poser des questions sur la réalité de son autonomie et la qualité de la régulation automatique lors d'une MEDEVAC terrestre ou héliportée. Le niveau maximum de la pression d'occlusion parait en effet un peu bas pour une application sur un treillis.
07/12/2023
Histoires de conversion du garrot
Rethinking limb tourniquet conversion in the prehospital environment
John B Holcomb JB et Al. J Trauma Acute Care Surg . 2023 Dec 1;95(6):e54-e60.
----------------------------------------
Un plaidoyer pour un emploi large MAIS raisonné qui doit être ENSEIGNE et notamment la problématique de sa conversion. Ceci est d'autant plus important que les délais d'évacuations risquent d'être longs.
----------------------------------------
We have highlighted the issue of overuse of tourniquets and described why tourniquet conversion and replacement should be taught and done in the prehospital setting.
Clic sur l'image pour accéder au document
12/11/2023
Compression aortique transgastrique ?
Gastroesophageal resuscitative occlusion of the aorta: Physiologic tolerance in a swine model of hemorrhagic shock
Revue des moyens d'hémostase des hémorragies non compressibles
Perspectives on the management of non-compressible torso hemorrhage: A narrative review
Leclerc S et Al. Journal of Military, Veteran and Family Health 8(s2) 2022: 73-36
Hemorrhage is one of the leading causes of death after trauma. A significant proportion of these fatalities could be prevented with appropriate bleeding control. This is more easily achieved with direct pressure in compressible areas such as the extremities or major joints. However, bleeding in the chest, abdomen, or pelvis cannot be as easily controlled without advanced procedures that are only available in hospitals. This article describes several technologies to control bleeding in the chest, abdomen, and pelvis that are potentially applicable in combat and pre-hospital settings. However, a review of existing studies quickly shows that convincing clinical evidence is lacking to support most pre-existing technologies, and the majority of studies are in the investigational stage. A universal, effective, and life-saving solution has not yet been identified. Accordingly, research in this area should continue to focus on both refining existing technologies and developing new approaches.
More than 50% of combat casualty deaths on the battlefield occur minutes to hours after a person has been wounded. Approximately 25% of those fatalities could potentially be prevented if rapid hemorrhage control or temporization were feasible. Despite several technologies to temporize non-compressible torso hemorrhage (NCTH), an ideal device and method have not yet been developed, particularly for Role 1 military medical treatment facilities and civilian pre-hospital settings. This article summarizes the devices and adjunct methods currently available to temporize NCTH when surgical and interventional radiology control are not readily accessible. New technologies under investigation are also discussed.
03/04/2023
Sang de banque sur pied: Mieux si on est entraîné
A prospective assessment of the medic autologous blood transfusion skills for field transfusion preparation
Steven G Schauer SG et Al. Transfusion. 2023 Mar 27. doi: 10.1111/trf.17325.
Background: Data demonstrate benefit from blood product administration near point-of-injury (POI). Fresh whole blood transfusion from a pre-screened donor provides a source of blood at the POI when resources are constrained. We captured transfusion skills data for medics performing autologous blood transfusion training.
Methods: We conducted a prospective, observational study of medics with varying levels of experience. Inexperienced medics were those with minimal or no reported experience learning the autologous transfusion procedures, versus reported experience among special operations medics. When available, medics were debriefed after the procedure for qualitative feedback. We followed them up to 7 days for adverse events.
Results: The median number of attempts for inexperienced and experienced medics was 1 versus 1 (interquartile range 1-1 for both, p=0.260). The inexperienced medics had a slower median time to needle venipuncture access for donation of 7.3 versus 1.5 minutes, needle removal after clamping time of 0.3 versus 0.2 minutes, time to bag preparation of 1.9 versus 1.0 minutes, time to IV access for reinfusion of 6.0 versus 3.0 minutes, time to transfusion completion of 17.3 versus 11.0 minutes, and time to IV removal of 0.9 versus 0.3 minutes (all p<0.05). We noted one administrative safety event in which allogeneic transfusion occurred. No major adverse events occurred. Qualitative data saturated around the need for quarterly training.
Conclusions: Inexperienced medics have longer procedure times when training autologous whole blood transfusion skills. This data will help establish training measures of performance for skills optimization when learning this procedure.
19/01/2023
Garrot: Moins de 2h OK mais pb après 4h
Impact of Time and Distance on Outcomes Following Tourniquet Use in Civilian and Military Settings: a Scoping Review
Joarder M et Al. https://doi.org/10.1016/j.injury.2023.01.031
Background: The last two decades have seen the reintroduction of tourniquets into guidelines for the management of acute limb trauma requiring haemorrhage control. Evidence supporting tourniquet application has demonstrated low complication rates in modern military settings involving rapid evacuation timeframes. It is unclear how these findings translate to patients who have prolonged transport times from injury in rural settings. This scoping review investigates the relationship between time and distance on metabolic complications, limb salvage and mortality following tourniquet use in civilian and military settings.
Methods: A systematic search strategy was conducted using PubMed, Embase, and SafetyLit databases. Study characteristics, setting, mechanism of injury, prehospital time, tourniquet time, distance, limb salvage, metabolic response, mortality, and tourniquet removal details were extracted from eligible studies. Descriptive statistics were recorded, and studies were grouped by ischemia time (< 2 hours, 2-4 hours, or > 4 hours).
Results: The search identified 3103 studies, from which 86 of studies were included in this scoping review. Of 86 studies, 55 studies were primarily civilian environments and 32 were based in military settings. One study included both settings. Blast injury was the most common mechanism of injury sustained by patients in military settings (72.8% [5968/8200]) followed by penetrating injury (23.5% [1926/8200]). In contrast, in civilian settings penetrating injury was the most common mechanism (47.7% [1633/3426]) followed by blunt injury (36.4% [1246/3426]).
Tourniquet time was reported in 66/86 studies. Tourniquet time over four hours was associated with reduced limb salvage rates (57.1%) and higher mortality rates (7.1%) compared with a tourniquet time of less than two hours. The overall limb salvage and mortality rates were 69.6% and 6.7% respectively. Metabolic outcomes were reported in 28/86 studies with smaller sample sizes and inconsistencies in which parameters were reported.
Conclusion: This scoping review presents literature describing comparatively safe tourniquet application when used for less than two hours duration. However, there is limited research describing prolonged tourniquet application or when used for protracted distances, such that the impact of tourniquet release time on metabolic outcomes and complications remains unclear. Prospective studies utilising the development of an international database to provide this dataset is required.
| Tags : tourniquet
25/11/2022
Point sur les matériaux hémostatiques
Emerging hemostatic materials for non-compressible hemorrhage control
Dong R. et Al. ,Natl Sci Rev. 2022 Aug 17;9(11):nwac162.
Non-compressible hemorrhage control is a big challenge in both civilian life and the battlefield, causing a majority of deaths among all traumatic injury mortalities. Unexpected non-compressible bleeding not only happens in pre-hospital situations but also leads to a high risk of death during surgical processes throughout in-hospital treatment. Hemostatic materials for pre-hospital treatment or surgical procedures for non-compressible hemorrhage control have drawn more and more attention in recent years and several commercialized products have been developed. However, these products have all shown non-negligible limitations and researchers are focusing on developing more effective hemostatic materials for non-compressible hemorrhage control. Different hemostatic strategies (physical, chemical and biological) have been proposed and different forms (sponges/foams, sealants/adhesives, microparticles/powders and platelet mimics) of hemostatic materials have been developed based on these strategies. A summary of the requirements, state-of-the-art studies and commercial products of non-compressible hemorrhage-control materials is provided in this review with particular attention on the advantages and limitations of their emerging forms, to give a clear understanding of the progress that has been made in this area and the promising directions for future generations.
04/10/2022
Pansement hémostatique et altitude: C'est OK
Hemostatic Effects of Bio-Zeolite Gauze and QuikClot Combat Gauze on Major Bleeding in Rabbits Acutely Exposed to High Altitude
Yi-jun J et Al. Prehosp Emerg Care. 2022 Sep 28;1-8
Objective:
Hemostatic gauze application is an effective way to control major bleeding, which is the most common cause of death in trauma in both civilian and military settings. Coagulation derangement after acute exposure to high altitude might alter the effects of hemostatic gauzes. The present study aimed to observe the hemostatic effects of bio-zeolite gauze (BZG) and QuikClot Combat Gauze® (QCG) on major bleeding in rabbits acutely exposed to high altitude.
Methods:
Sixty rabbits were randomly and evenly divided into six groups. Animal models of simulated blast- and fragment-induced inguinal major bleeding were prepared in lower altitude and high-altitude areas, and BZG, QCG, and ordinary gauze without hemostatic material were used to control bleeding. The primary outcomes included immediate hemostasis rate, blood loss, and survival rate, while the secondary outcomes included hemodynamic parameters, laboratory examinations, and coagulation-relevant markers.
Results:
The overall effects of BZG and QCG were better than those of ordinary gauze, with a higher immediate hemostatic rate, less blood loss, and higher survival rate at 90 min after gauze application and higher red blood cell and platelet counts and lower creatinine level at 30 min after gauze application in lower altitude. The concentrations of coagulation factor XII and factor X in rabbits acutely exposed to high altitude were significantly lower than those in lower altitude. At high altitude, the hemostatic effects of BZG did not decrease significantly compared to those in the lower altitude, whereas those of ordinary gauze and QCG decreased significantly at high altitude compared to those in the lower altitude.
Conclusions:
Coagulation derangement after acute exposure to high altitude has negative effects on ordinary gauze and QCG but has no significant negative hemostatic effects on BZG.
05/12/2021
Garrot abdominal: A bien regarder !!!!
Abdominal Aortic Junctional Tourniquet - Stabilized (AAJTS) can be applied both successfully and rapidly by Combat Medical Technicians (CMTs)
Smith TM et Al. BMJ Mil Health. 2021 Nov 30;e001881.
-----------------------------------------
On parle beaucoup du REBOA, mais ce dispositif est une alternative certainement plus simple à mettre en oeuvre
-----------------------------------------
Background
‘Non-compressible’ haemorrhage is the leading cause of preventable battlefield death, often requiring surgical or radiological intervention, which is precluded in the pre-hospital environment. One-fifth of such bleeds are junctional and therefore potentially survivable. We examine the use of the Abdominal Aortic Junctional Tourniquet - Stabilized (AAJTS) among UK Combat Medical Technicians (CMTs) as a device to control junctional haemorrhage with external compression of the abdominal aorta—compression of junctional haemorrhage previously considered ‘non-compressible.’ This follows animal studies showing that the AAJTS achieves control of haemorrhage and improves physiological parameters.
Methods
CMTs were selected and applied the AAJTS to each other following a 1-hour training package. A consultant radiologist-operated hand-held ultrasound monitored flow changes in the subjects’ common femoral artery. CMTs were then surveyed for their opinions as to utility and function.
Results
21 CMTs were screened and 17 CMTs participated with 34 total applications (16 day and 18 low-light). 27/34 (79%) achieved a successful application. The median application time was 75 s in daylight and 57 s in low-light conditions. There was no significant difference in Body Mass Index (p=0.23), median systolic blood pressure (p=0.19), nor class of CMT (p=0.10) between successful and unsuccessful applications. Higher systolic blood pressure was associated with longer application times (p=0.03). Users deemed the device easy to use (median score 4.4 on a 5-point Likert scale).
Conclusion
CMTs can use AAJTS successfully after a 1-hour training session in the majority of applications. Application was successful in both daylight and low-light conditions. Self-reported usability ratings were high.
16/11/2021
PLP: A ne pas mettre au rebus !
Contemporary utility of diagnostic peritoneal aspiration in trauma
Morgan Schellenberg M et Al. J Trauma Acute Care Surg. 2021 Nov 1;91(5):814-819.
Background: Focused Assessment with Sonography for Trauma (FAST) has supplanted diagnostic peritoneal lavage (DPL) as the preferred bedside evaluation for traumatic hemoperitoneum. Diagnostic peritoneal aspiration (DPA) is a simpler, faster modification of DPL with an unclear role in contemporary practice. This study delineated modern roles for DPA and defined its diagnostic yield.
Methods: All trauma patients presenting to our Level I center who underwent DPA were included (May 2015 to May 2020). Demographics, comorbidities, clinical/injury data, and outcomes were collected. The diagnostic yield and accuracy of DPA were calculated against the criterion standard of hemoperitoneum at exploratory laparotomy or computed tomography scan.
Results: In total, 41 patients underwent DPA, typically after blunt trauma (n = 37, 90%). Patients were almost exclusively hypotensive (n = 20, 49%) or in arrest (n = 18, 44%). Most patients had an equivocal or negative FAST and hypotension or return of spontaneous circulation after resuscitative thoracotomy (n = 32, 78%); or had a positive FAST and known cirrhosis (n = 4, 10%). In two (5%) patients, one obese, the catheter failed to access the peritoneal cavity. Diagnostic peritoneal aspiration sensitivity, specificity, positive predictive value, and negative predictive value were 80%, 100%, 100%, and 90%, with an accuracy of 93%. One (2%) complication, a small bowel injury, occurred.
Conclusion: Despite near ubiquitous FAST availability, DPA remains important in diagnosing or excluding hemoperitoneum with exceedingly low rates of failure and complications. Diagnostic peritoneal aspiration is most conclusive when positive, without false positives in this study. Diagnostic peritoneal aspiration was most used among blunt hypotensive or postarrest patients who had an equivocal or negative FAST, in whom the preliminary diagnosis of hemoperitoneum is a critically important decision making branch point.
25/09/2021
Olaes Bandage: En mieux