29/09/2012
L'essence du triage
Ce témoignage exprime parfaitement tous les enjeux du sauvetage au combat en montrant qu'il s'agit d'un concept de prise en charge intégrant toutes les dimensions dela traumatologie moderne (préparation, savoir faire personnel, travail en équipe: son équipe et les autres, délégation, leadership, gestion du stress).
Etre fort dans sa tête, dans son savoir pour pouvoir former ses personnels et les guider au moment de l'action en ayant pris le recul suffisant.
| Tags : triage, leadership, pédagogie, mascal
24/09/2012
MERT, PEDRO ou Dustoff ?
Pas simple de choisir les modalités d'intervention en zone de combat. Dans le document présenté une comparaison des moyens US et UK. Nous sommes entre la MERT-E UK et le PEDRO US ?
23/09/2012
Facteur VIIa: Intérêt pas prouvé !
Use of recombinant factor VIIA for control of combat-related haemorrhage.
Woodruff SI et all. Emerg Med J 2010;27:2 121-124
Ce travail met en exergue que le recours au FVIIa n'a pas d'intérêt prouvé en cas de prise en charge de traumatismes pénétrants. Ceci est d'autant plus vrai qu'il est fait alors qu'une coagulopathie sévère est installée (The utility of recombinant factor VIIa as a last resort in trauma. Mamtani R. et all. World Journal of Emergency Surgery 2012, 7(Suppl 1):S7)
----------------------------------------------
Background
Recombinant activated human coagulation factor VII (rFVIIa), an intravascular strategy to promote clotting, is being used as an adjunct to surgical control of bleeding in combat trauma patients.
Objective
To describe the initial experiences with rFVIIa administered to combat casualties at US Navy-Marine Corps medical treatment facilities in Iraq, and to comparesurvival outcomes of those treated with rFVIIa to controls not receiving rFVIIa.
Methods
Medical encounter data from the US Navy-Marine Corps Combat Trauma Registry were retrospectively reviewed to identify all battle-injured patients documented as having received rFVIIa during the period May 2004 to January 2006 of Operation Iraqi Freedom. Available clinical and injury related data are presented to characterise the patients. To assess effects of rFVIIa on survival outcomes, rFVIIa cases were matched to controls on injury severity and age.
Results
22 battle-injured patients from the Combat Trauma Registry received rFVIIa. Primarily young US Marines, these patients typically had penetrating injuries from improvised explosive devices and gunshot wounds. Injuries were often abdominal. The average dose used was similar to that reported in another study of civilian trauma patients, although dosing varies widely in the existing experimental and anecdotal literature. Over two-thirds (68%) of the rFVIIa patients surviveddan identical outcome seen for a matched control group of 22 patients.
Conclusions
Survival of seriously injured combat casualties was good, although identical to that of a control group. Methodological limitations of this retrospective study preclude making firm conclusions about the effectiveness of rFVIIa. Future controlled studies are needed for safety and efficacy testing of rFVIIa in combat trauma patients.
----------------------------------------------
| Tags : hémorragie, coagulopathie
20/09/2012
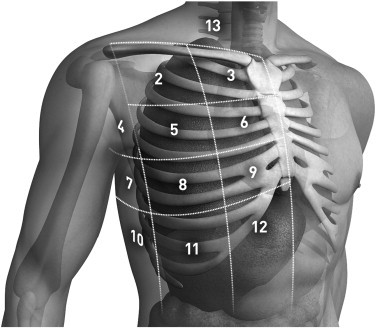
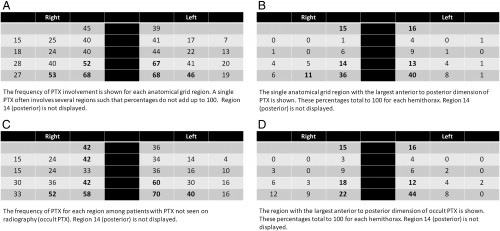
Pneumothorax: La sonde d'écho à quel endroit ?
Anatomical distribution of traumatic pneumothoraces on chest computed tomography: implicationsfor ultrasound screening in the ED
Mennicke M et alll. Am J Emerg Med 2012 Sep;30(7):1025-31
Un travail qui précise les zones optimales d'exploration de la région thoracique pour l'identiifcation optimale des pneumothorax traumatiques.
----------------------------------------------------------------------------------------
OBJECTIVES:
We sought to assess the anatomical distribution of traumatic pneumothoraces (PTXs) on chest computed tomography (CT) to develop an optimized protocol for PTX screening with ultrasound in the emergency department (ED).
METHODS:
We performed a retrospective review of all chest CTs performed in one ED between January 2005 and December 2008 according to presence, location, and size of PTX. Pneumothoraces were then measured and categorized into 14 anatomical regions for each hemithorax.
RESULTS:
A total of 277 (3.8%) PTXs were identified, with 26 bilateral PTX, on 3636 chest CTs performed during the study period. Etiology was blunt (85%) or penetrating trauma (15%). Eighty-three (45%) PTXs were radiographically occult on initial chest x-ray. One hundred eighty-three (66%) PTX had no chest tube at the time of CT. For both hemithoraces, the distribution demonstrated increasing PTX frequency and size from lateral to medial and from superior to inferior. Region 12 (parasternal, intercostal spaces [ICS] 7-8) was involved in 68% of PTX on either side; region 9 (parasternal, ICS 5-6), in 67% on the left and in 52% on the right; and region 11 (lateral to midclavicular line, ICS 7-8), in 46% on the left and in 53% on the right. The largest anterior-to-posterior PTX dimension was seen in region 12.
CONCLUSIONS:
Our results indicate that 80.4% of right- and 83.7% of left-sided traumatic PTXs would be identified by scanning regions 9, 11, and 12. These findings suggest that a standardized protocol for PTX screening with ultrasound should include these regions.
----------------------------------------------------------------------------------------
| Tags : échographie, pneumothorax
13/09/2012
Trauma crânien et psychologique: Le point US
| Tags : ptsd, tbi, psychiatrie
08/09/2012
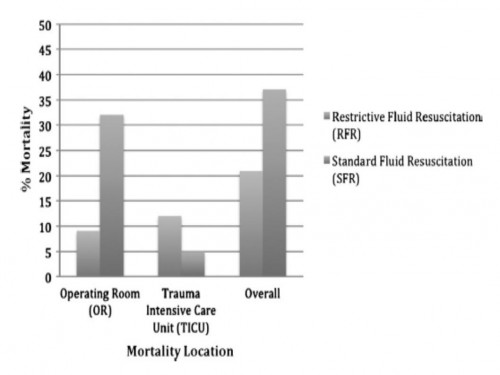
Moins remplir: Mieux ? Oui, MAIS
Restrictive fluid resuscitation in combination with damage control resuscitation: Time for adaptation.
Marquinn D et all. J Trauma Acute Care Surg. 2012;73: 674-678.
-------------------------------------------------------------------------------------------------------------
Ce travail confirme l'intérêt d'une stratégie de remplissage vasculaire parcimonieuse dès lors qu'une réanimation et une chirurgie spécialisée moderne sont accessibles. Le collectif des patients est ici celui de traumatisés thoraciques sévères arrivant dans une structure spécialisée dans des délais très courts. De telles conditions ne sont pas forcément celles de la prise en charge de blessés de guerre pour qui les délais d'évacuation sont souvent plus élevés. Il n'en demeure pas moins que cette publication milite pour une politique de remplissage vasculaire raisonnée. On rappelle que la procédure du sauvetage au combat donne pour objectif la perception d'un pouls radial perceptible.
-------------------------------------------------------------------------------------------------------------
BACKGROUND:
Damage control resuscitation (DCR) conveys a survival advantage in patients with severe hemorrhage. The role of restrictive fluid resuscitation (RFR) when used in combination with DCR has not been elucidated. We hypothesize that RFR, when used with DCR, conveys an overall survival benefit for patients with severe hemorrhage.
METHODS:
This is a retrospective analysis from January 2007 to May 2011 at a Level I trauma center. Inclusion criteria included penetrating torso injuries, systolic blood pressure less than or equal to 90 mm Hg, and managed with DCR and damage control surgery (DCS). There were two groups according to the quantity of fluid before DCS: (1) standard fluid resuscitation (SFR)greater than or equal to 150 mL of crystalloid; (2) RFR less than 150 mL of crystalloid. Demographics and outcomes were analyzed.
RESULTS:
Three hundred seven patients were included. Before DCS, 132 (43%) received less than 150 mL of crystalloids, grouped under RFR; and 175 (57%) received greater than or equal to 150 mL of crystalloids, grouped under SFR. Demographics and initial clinical characteristicswere similar between the study groups. Compared with the SFR group, RFR patients received less fluid preoperatively (129 mL vs. 2,757 mL; p G 0.001), exhibited a lower intraoperative mortality (9% vs. 32%; p G 0.001), and had a shorter hospital length of stay (13 vs. 18 days; p = 0.02). Patients in the SFR group had a lower trauma intensive care unit mortality (5 vs. 12%; p = 0.03) but exhibited a higher overall mortality. Patients receiving RFR demonstrated a survival benefit, with an odds ratio for mortality of 0.69 (95% confidence interval, 0.37Y0.91).
CONCLUSION:
To the best of our knowledge, this is the first civilian study that analyzes the impact of RFR in patients managed with DCR. Its use in conjunction with DCR for hypotensive trauma patients with penetrating injuries to the torso conveys an overall and early intraoperative survival benefit.
| Tags : remplissage, choc, hémorragie, perfusion