----------------------------------------------------------------------------------------------------------------------
22/12/2014
Plus d'auscultation mais une Echo ?
Point of care ultrasound for orotracheal tube placement assessment in out-of hospital setting.
Zadel S et AL. Resuscitation. 2014 Nov 20;87C:1-6
-----------------------------------------------
A lire cet article, on comprend pourquoi l'engouement actuel pour l'échographie des voies aériennes. A coup sûr une technique à maîtriser en préhospitalier.
-----------------------------------------------
AIM OF THE STUDY:
The percentage of unrecognised orotracheal tube displacement in an out-of-hospital setting has been reported to be between 4.8% and 25%. The aim of our study was to assess the sensitivity and specificity of Point-of-Care-UltraSound (POCUS) for confirming the propertube position after an urgent orotracheal intubation in an out-of-hospital setting and the time needed for POCUS.
METHODS:
Our single-centred prospective study included all patients who needed out-of-hospital orotracheal intubation. After the intubation, bilateral chest auscultation and assessment of bilateral lung sliding and diaphragm excursion within POCUS were done. Spectrographic quantitative capnography was used as the reference standard to confirm a proper tube position.
RESULTS:
We enrolled 124 patients. For auscultation, sensitivity and negative predicted value were 100%, specificity was 90% and positive predicted value 30% (95% confidence interval).
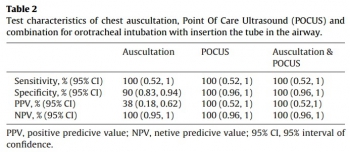
Sensitivity, specificity, positive predicted value, and negative predicted value for POCUS alone and for a combination of auscultation and POCUS were 100% (95% confidence interval). In three patients, we detected endobronchial tube displacement with auscultation and POCUS. Capnography failed to detect displacement in all three cases. The median time needed for POCUS was 30s.
CONCLUSION:
Results of our study support POCUS as an accurate and reliable method for confirming the proper orotracheal tube placement in trachea and it is feasible for out-of-hospital setting implementation. POCUS also seems to be time saving method but to make definitive conclusion more studies should be done.
| Tags : airway, intubation, échographie
19/11/2014
Une bougie dans la sonde: c'est mieux.
Comparison of Intubation Performance by Emergency Medicine Residents Using Gum Elastic Bougie versus Standard Stylet in Simulated Easy and Difficult Intubation Scenarios
Walsh RM et All. Emerg Med Australas - ; 26 (5); 446-9
Study Objectives: We sought to evaluate the success rate and time to endotracheal intubation by emergency medicine residents with stylet reinforced endotracheal tube (ETT-S) versus intubation with a gum elastic bougie (GEB) in simulated easy and difficult airways on a cadaveric model.
Methods: The study was a prospective cross-over design using a single study cohort of 29 emergency medicine residents. A fresh frozen cadaver was used in either standard positioning to facilitate a Cormack Lehane Grade 1 laryngoscopy, or with a hard cervical collar applied a Cormack Lehane Grade 3 laryngoscopy. Each participant then intubated the cadaver in each setting (Grade 1 ETT-S, Grade 1 GEB, Grade 3 ETT-S, Grade 3 GEB). The primary end-point of our investigation was the time to intubation. Secondary endpoints were: success rate of intubation, mean ratings by study participants of perceived ease of intubation for each intubation technique in each simulated degree of difficulty, and overall preference of intubation technique in each simulated degree of difficulty. To assess the effect of intubation type (GEB vs ETT-S) and difficulty on time to successful intubation and perceived ease of intubation, repeated measures ANOVAs were conducted. To examine whether success of intubation differed across the GEB and ETT-S groups we used a McNemar’s test. To examine the effect of previous experience on time to intubation, we used a mixed model ANOVA incorporating intubation type and difficulty of intubation.
Results: Mean time to intubation in all scenarios ranged from 28.8 – 116.6 seconds. Year of residency training trended toward significance but was not significant when comparing post-graduate year to time to intubation (p¼ 0.07). Time to intubation was significantly different only when comparing Grade 3 ETTS to Grade 3 GEB (p¼ 0.006). Of the 116 intubations performed in this study, a total of 36 were failed attempts. There was no significant difference in success rate when comparing Grade 1 ETT-S to Grade 1 GEB nor Grade 3 ETT-S to Grade 3 GEB (p ¼ >0.05). Across all year groups, participants perceived the Grade 1 scenario to be easier than the Grade 3 scenario. At the conclusions of the study, 55% of participants preferred using the GEB in all settings. When broken down by scenario, 41% preferred the GEB in the Grade 1 scenario while 76% preferred the GEB in the Grade 3 scenario.
Conclusions: Time to intubation in a simulated grade 3 view was significantly longer in the GEB group versus the ETT-S group. Although the differences in success rates were not statistically significant, there was a trend toward more successful intubations with the GEB in the simulated grade 3 view. This is important because in the emergency department when difficult airways can be high stress and life threatening, although the GEB group took more time, the success rates were higher.
| Tags : intubation
05/06/2014
Réflexions US sur l'accès aux voies aériennes
Advances in prehospital airway management
Jacobs PE et all. Int J Crit Illn Inj Sci. 2014 Jan-Mar; 4(1): 57–64.
Prehospital airway management is a key component of emergency responders and remains an important task of Emergency Medical Service (EMS) systems worldwide. The most advanced airway management techniques involving placement of oropharyngeal airways such as the Laryngeal Mask Airway or endotracheal tube. Endotracheal tube placement success is a common measure of out-of-hospital airway management quality. Regional variation in regard to training, education, and procedural exposure may be the major contributor to the findings in success and patient outcome. In studies demonstrating poor outcomes related to prehospital-attempted endotracheal intubation (ETI), both training and skill level of the provider are usually often low. Research supports a relationship between the number of intubation experiences and ETI success. National standards for certification of emergency medicine provider are in general too low to guarantee good success rate in emergency airway management by paramedics and physicians. Some paramedic training programs require more intense airway training above the national standard and some EMS systems in Europe staff their system with anesthesia providers instead. ETI remains the cornerstone of definitive prehospital airway management, However, ETI is not without risk and outcomes data remains controversial. Many systems may benefit from more input and guidance by the anesthesia department, which have higher volumes of airway management procedures and extensive training and experience not just with training of airway management but also with different airway management techniques and adjuncts.
| Tags : airway, intubation
01/06/2014
Pression cricoïdienne: Plus recommandé
La manoeuvre de Sellick, si classique, n'est plus recommandée ou du moins il est considéré qu'elle ne dispose plus d'assez d'arguments pour en faire une manoeuvre obligatoire.
Cliquez sur l'image qui suit pour un point actualisé
Les recommandations de l'Eastern Association for the Surgery of Trauma
| Tags : intubation
27/05/2014
Maîtrise de la coniotomie en environnement austère: Une nécessité.
Optimizing Emergent Surgical Cricothyrotomy for use in Austere Environments
HessertMJ et Al. Wilderness Environ Med. 2013 Mar;24(1):53-66
" Although cricothyrotomy is becoming less common as other alternative airway devices are introduced, such as the laryngeal mask airway, King LT-D (King Systems Corp, Noblesville, IN), and other supraglottic devices, there is, and likely always will be, a role for cricothy- rotomy in a subsection of patients with difficult airways, especially in environments in which such devices are unlikely to be available. A common emergency medicine aphorism is: “If you do one cricothyrotomy, you’re a hero; if you do two, work on your airway skills.” True perhaps in a hospital, but in an austere environment many factors besides failed ET intubation lead to early cricothyrotomy. Wilderness providers must be not only technically skilled, but also adequately trained to recognize the key indications and situational decision triggers for cricothyrotomy that differ from in-hospital practice."
| Tags : airway, coniotomie, intubation
08/04/2014
Coniotomie au Combat: Simuler pour retenir le savoir
Vincent H. et Al. Anesthesiology 2014; 120:999-1008
background:
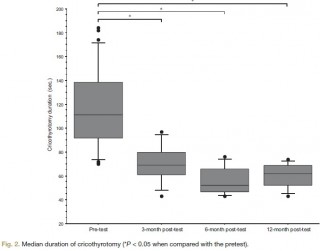
The effectiveness of simulation is rarely evaluated. The aim of this study was to assess the impact of a short training course on the ability of anesthesiology residents to comply with current difficult airway management guidelines.
METHODS:
Twenty-seven third-year anesthesiology residents were assessed on a simulator in a "can't intubate, can't ventilate" scenario before the training (the pretest) and then randomly 3, 6, or 12 months after training (the posttest). The scenario was built so that the resident was prompted to perform a cricothyrotomy. Compliance with airway management guidelines and the cricothyrotomy's duration and technical quality were assessed as a checklist score [0 to 10] and a global rating scale [7 to 35].
RESULTS:
After training, all 27 residents (100%) complied with the airway management guidelines, compared with 17 (63%) in the pretest (P < 0.005). In the pretest and the 3-, 6-, and 12-month posttests, the median [range] duration of cricothyrotomy was respectively 117 s [70 to 184], 69 s [43 to 97], 52 s [43 to 76], and 62 s [43 to 74] (P < 0.0001 vs. in the pretest), the median [range] checklist score was 3 [0 to 7], 10 [8 to 10], 9 [6 to 10], and 9 [4 to 10] (P < 0.0001 vs. in the pretest) and the median [range] global rating scale was 12 [7 to 22], 30 [20 to 35], 33 [23 to 35], and 31 [18 to 33] (P < 0.0001 vs. in the pretest). There were no significant differences between performance levels achieved in the 3-, 6-, and 12-month posttests.
CONCLUSION: The training session significantly improved the residents' compliance with guidelines and their performance of cricothyrotomy.
| Tags : airway, intubation
07/04/2014
Airway en préhospitalier US: Plus tube que dispositif glottique
An update on out-of-hospital airway management practices in the United States
Diggs LA. et Al. Resuscitation. 2014 Mar 15. pii: S0300-9572
______________________________________________________
Ce document fait le point sur la pratique préhospitalière US. Cette dernière est faite avant tout d'intubation et la prudence est de mise concernant les performances réelles des dispositifs supra-glottiques avec lesquels (excepté le tube de king) les résultats sont moins bons.
______________________________________________________
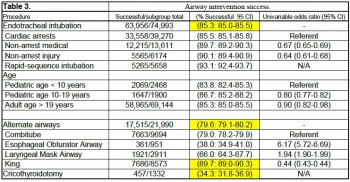
OBJECTIVE: We characterized out-of-hospital airway management interventions, outcomes, and complications using the 2012 NEMSIS Public-Release Research Data Set containing almost 20 million Emergency Medical Services activations from 40 states and two territories. We compared the outcomes with a previous study that used 2008 NEMSIS data containing 16 states with 4 million EMS activations.
METHODS:
Patients who received airway management interventions including endotracheal intubation (ETI), alternate airways (Combitube, Laryngeal Mask Airway (LMA), King LT, Esophageal-Obturator Airway (EOA)), and cricothyroidotomy (needle and surgical) were identified. Using descriptive statistics, airway management success and complications were examined in the full cohort and key subsets including cardiac arrest, non-arrest medical, non-arrest injury, children<10 years, children 10-19 years, rapid sequence intubation (RSI), population setting, US census region, and US census division.
RESULTS:
Among 19,831,189 EMS activations, there were 74,993 ETIs, 21,990 alternate airways, and 1332 cricothyroidotomies. ETI success rates were: overall 63,956/74,993 (85.3%; 95% CI: 85.0-85.5), cardiac arrest 33,558/39,270 (85.5%), non-arrest medical 12,215/13,611 (89.7%), non-arrest injury (90.1%), children<10 years 2069/2468 (83.8%), children 10-19 years 1647/1900 (86.7%), adults>19 years 58,965/69,144 (85.3%), and rapid sequence intubation 5265/5658 (93.1%). Major complications included bleeding 677 (4.4 per 1000 interventions), vomiting 1221 (8 per 1000 interventions), esophageal intubation immediately detected 874 (5.7 per 1000 interventions), and esophageal intubations other 219 (1.4 per 1000 interventions).
CONCLUSIONS:
Paramedics provide life-saving emergency medical care to patients in the out-of-hospital setting. Only selected emergency medical procedures have proved to be safe and effective. The safety and efficacy profile of ETI has been challenged in the last ten years. Intubation has been the standard of care in the United States for more than thirty years and is regarded as one of the most important EMS procedures. In this study, we retrospectively examined the largest aggregate of EMS data currently available and observed low out-of-hospital ETI success rates.
ETI is a complex procedure requiring skilled choreography and numerous critical decisions and actions. In the absence of qualified personnel, or if ETI proves problematic, alternate airways are commonly employed. As more EMS systems embrace alternate airway devices in lieu of ETI, it is important to have a clear appreciation of the true success rates of airway procedures using these devices across a variety of patient characteristics and clinical settings. This study examined the most commonly used alternate airway devices including the Combitube, Esophageal Obturator Airway, Laryngeal Mask Airway, King Laryngeal Tube, and cricothyroidotomy and observed very low alternate airway success rates in the largest population sample to date. Alternate airway success rates were substantially lower than ETI success rates except for the King LT.
| Tags : airway, intubation
01/04/2014
Bougie d'intubation: Pas toutes égales
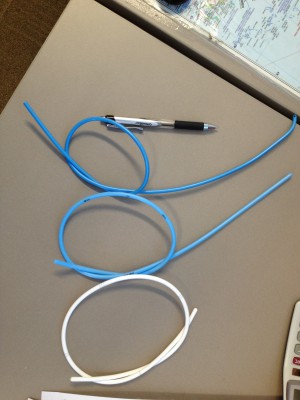
Bougie-related airway trauma: dangers of the hold-up sign
Marson BA et Al. Anaesthesia 2014, 69, 219–223
Le bon positionnement d'un mandrin d'intubation est confirmé parles sensations de ressaut quand l'extrémité de ce dernier franchit les anneaux trachéaux et par le blocage de ce dernier dans l'arbre bronchique. Ce dernier signe est appelé "the hold up sign" par les anglo-saxons. Ce blocage confirme que le mandrin n'est pas intra-oesophagien auquel cas il n'existerait pas. Cette publication attire l'attention sur le danger potentiel de traumatisme trachéal.
----------------------------------------------------------------------------
The bougie is a popular tool in difficult intubations. The hold-up sign is used to confirm tracheal placement of a bougie. This study aimed to establish the potential for airway trauma when using this sign with an Eschmann reusable bougie or a Frova single-use bougie. Airways were simulated using a manikin (hold-up force) and porcine lung model (airway perforation force). Mean (SD) hold-up force (for airway lengths over the range 25–45 cm) of 1.0 (0.4) and 5.2 (1.1) N were recorded with the Eschmann and Frova bougies, respectively (p < 0.001). The mean (SD) force required to produce airway perforation was 0.9 (0.2) N with the Eschmann bougie and 1.1 (0.3) N with the Frova bougie (p = 0.11). It is possible to apply a force at least five times greater than the force required to produce significant trauma with a Frova single-use bougie. We recommend that the hold-up sign should no longer be used with single-use bougies. Clinicians should be cautious when eliciting this sign using the Eschmann re-usable bougie.
--------------------------------------------------------------------------------------------------------------
Il existe d'autres bougies que celle d'eschmann et de Frova comme l'Introes pocket bougie ou la traffic light bougie. Cette dernière apparaît très intéressante car permettant de limiter la longueur de mandrin inséré dans la trachée et partant le risque de perforation trachéale.
| Tags : intubation
29/10/2013
Intubation en préhospitalier : intérêt des nouvelles techniques
IOT difficile et les nouveaux outils en situation d’urgence ( où en est-on ? )
Les procédures validées
Combes X et All. Urgences - 2013
Points essentiels
■ L’intubation en séquence rapide est la technique de sédation validée pour faciliter l’intubation en situation d’urgence.
■ La préoxygénation peut être réalisée par VNI chez le patient coopérant.
■ Les lames de laryngoscopes en plastique ne doivent pas être utilisées.
■ L’utilisation du mandrin long béquillé est parfaitement validée en situation d’urgence en cas d’intubation difficile sans difficulté de ventilation associées.
■ Le masque laryngé d’intubation Fastrach® est le dispositif de ventilation le plus utile en situation d’urgence.
■ Les vidéolaryngoscopes ne sont pas encore validées pour la prise en charge de l’intubation difficile en situation d’urgence.
■ Les dispositifs de cricothyroïdotomiee basée sur la technique de Seldinger sont à privilégier en situation d’urgence
| Tags : airway, intubation
29/05/2013
Vidéo laryngoscopie: Du bien, on n'est pas étonné
Anesth Analg 2013;XX:XX–XX
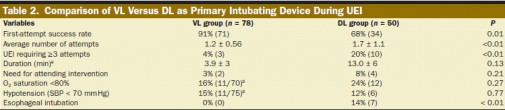
BACKGROUND:The video laryngoscope (VL) has been shown to improve laryngoscopic views and first-attempt success rates in elective operating room and simulated tracheal intubations compared with the direct laryngoscope (DL). However, there are limited data on the effectiveness of the VL compared with the DL in urgent endotracheal intubations (UEIs) in the critically ill. We assessed the effectiveness of using a VL as the primary intubating device during UEI in critically ill patients when performed by less experienced operators.
METHODS:We compared success rates of UEIs performed by Pulmonary and Critical Care Medicine (PCCM) fellows in the medical intensive care unit and medical or surgical wards. A cohort of PCCM fellows using GlideScope VL as the primary intubating device was compared with a historical cohort of PCCM fellows using a traditional Macintosh or Miller blade DL. The primary measured outcome was first-attempt intubation success rate. Secondary outcomes included total number of attempts required for successful tracheal intubation, rate of esophageal intubation, need for supervising attending intervention, duration of intubation sequence, and incidence of hypoxemia and hypotension.
RESULTS:There were 138 UEIs, with 78 using a VL and 50 using a DL as the primary intubating device. The rate of first-attempt success was superior with the VL as compared with the DL (91% vs 68%, P < 0.01). The rate of intubations requiring ≥3 attempts (4% vs 20%, P < 0.01), unintended esophageal intubations (0% vs 14%, P < 0.01), and the average number of attempts required for successful tracheal intubation (1.2 ± 0.56 vs 1.7 ± 1.1, P < 0.01) all improved significantly with use of the VL compared with the DL.
CONCLUSIONS:UEI using a VL as the primary device improved intubation success anddecreased complications compared with a DL when PCCM fellows were the primary operators. These data suggest that the VL should be used as the primary device when urgent intubations are performed by less experienced operators.
| Tags : intubation, airway
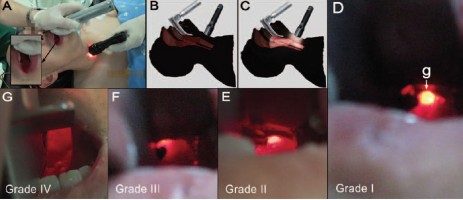
03/03/2013
Mieux voir pour mieux intuber. Un moyen simple surtout si on débute
Retrograde Light-guided Laryngoscopy for Tracheal Intubation. Clinical Practice and Comparison with Conventional Direct Laryngoscopy
Anesthesiology 2013; 118:XXX–XXX doi: 10.1097/ALN.0b013e31828877c0.
L'intubation orotrachéale nécessite un apprentissage réel. Une cinquantaine de procédures réussies sont nécessaires pour pouvoir considérer avoir la maîtrise de ce geste. De nombreux dispositifs permettent d'augmenter le taux de réussite (bougie, stylets lumineux, dispositifs laryngés, fibroscopie, vidéolaryngoscope). Ces dernières sont cependant onéreuses et pas forcément toujours disponibles. L'illumination transtrachéale et rétrograde du plan glottique pourrait avoir une certaine utilité en améliorant la visualisation de l'orifice glottique.
--------
Compared with DL, the success rate was greater in the RLGL group for all five intubations (72% vs. 47%; rate difference, 25%; 95% CI [11.84–38.16%], P < 0.001). This was associated with a shorter time to glottic exposure (median [25th and 75th percentile]; 27 [15; 42] vs. 45 [30; 73] s, P < 0.001), shorter intubation time (66 [44; 120] vs. 120 [69; 120] s, P < 0.001), and decreased throat soreness (mean ± SD; visual analog scale, 2.1 ± 0.9 vs. 3.7 ± 1.0 cm, P = 0.001) in the RLGL group compared to the DL group.
--------
| Tags : intubation, airway
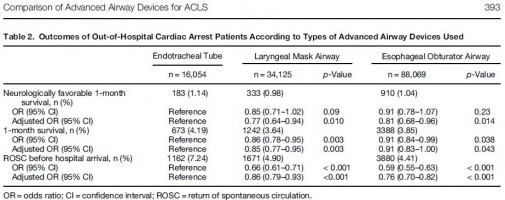
24/02/2013
Intubation: Encore une étude POUR
Comparison of Neurological Outcome between Tracheal Intubation and Supraglottic Airway Device Insertion of Out-of-hospital Cardiac Arrest Patients: A Nationwide, Population-based, Observational Study
J Emerg Med. 2013 Feb;44(2):389-97
BACKGROUND:
The effect of prehospital use of supraglottic airway devices as an alternative to tracheal intubation on long-term outcomes of patients with out-of-hospital cardiac arrest is unclear.
STUDY OBJECTIVES:
We compared the neurological outcomes of patients who underwent supraglottic airway device insertion with those who underwent tracheal intubation.
METHODS:
We conducted a nationwide population-based observational study using a national database containing all out-of-hospital cardiac arrest cases in Japan over a 3-year period (2005-2007). The rates of neurologically favorable 1-month survival (primary outcome) and of 1-month survival and return of spontaneous circulation before hospital arrival (secondary outcomes) were examined. Multiple logistic regression analyses were performed to adjust for potential confounders. Advanced airway devices were used in 138,248 of 318,141 patients, including an endotracheal tube (ETT) in 16,054 patients (12%), a laryngeal mask airway (LMA) in 34,125 patients (25%), and an esophageal obturator airway (EOA) in 88,069 patients (63%).
RESULTS:
The overall rate of neurologically favorable 1-month survival was 1.03% (1426/137,880). The rates of neurologically favorable 1-month survival were 1.14% (183/16,028) in the ETT group, 0.98% (333/34,059) in the LMA group, and 1.04% (910/87,793) in the EOA group. Compared with the ETT group, the rates were significantly lower in the LMA group (adjusted odds ratio 0.77, 95% confidence interval [CI] 0.64-0.94) and EOA group (adjusted odds ratio 0.81, 95% CI 0.68-0.96).
CONCLUSIONS:
Prehospital use of supraglottic airway devices was associated with slightly, but significantly, poorer neurological outcomes compared with tracheal intubation, but neurological outcomes remained poor overall.
| Tags : airway, intubation
17/11/2012
Coniotomie / Cricothyrotomie
L'accès aux voies aériennes: Plan A: liberté des voies aériennes par les manoeuvres de secourisme, la mise en place d'une guédel et l'intubation. Plan B: Je n'oublie pas que l'essentiel est de pouvoir ventiler, donc j'ai un ballon. Plan C: Si je n'arrive pas à intuber et à ventiler, je n'hésite pas à OUVRIR LE COU
| Tags : coniotomie, airway, intubation
18/04/2012
Conférence Experts: Intubation difficile
| Tags : intubation
15/02/2011
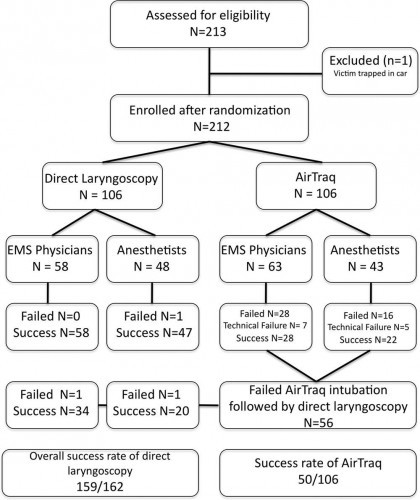
Intubation préhospitalière: Que penser de l'AIRTRAQ ?
Comme pour tout il faut s'entraîner et on n'inove pas. On rappelle que, en conditions de combat, le contrôle des voies aériennes a pour but essentiellemment de prévenir l'obstruction des voies aériennes, de prévenir l'inhalation du contenu gastrique. Le traitement d'une détresse respiratoire fait appel avant tout à l'oxygénothérapie si vous disposez d'oxygène, au traitement d'une cause spécifique (pneumo ou hémothorax, volet thoracique, plaie soufflante), à l'assistance ventilatoire au ballon par masque facial et EVENTUELLEMENT après intubation ou coniotomie sur une canule de 6 mm si les conditions tactiques le permettent.
Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: A randomized control trial
Trimmel H et all.
Crit Care Med 2011 Vol. 39, No. 3, 1-5
Objectives: The optical Airtraq laryngoscope (Prodol Meditec, Vizcaya, Spain) has been shown to have advantages when compared with direct laryngoscopy in difficult airway patients. Furthermore, it has been suggested that it is easy to use and handle even for inexperienced advanced life support providers. As such, we sought to assess whether the Airtraq may be a reliable alternative to conventional intubation when used in the prehospital setting.
Design, Setting, and Patients: Prospective, randomized control trial in emergency patients requiring endotracheal intubation provided by anesthesiologists or emergency physicians responding with an emergency medical service helicopter or ground unit associated with the Department of Anesthesiology, General Hospital, Wiener Neustadt, Austria.
Measurements and Main Results: During the 18-month study period, 212 patients were enrolled. When the Airtraq was used as first-line airway device (n = 106) vs. direct laryngoscopy (n =106), success rate was 47% vs. 99%, respectively (p < .001). Reasons for failed Airtraq intubation were related to the fiberoptic characteristic of this device (i.e., impaired sight due to blood and vomitus, n = 11) or to assumed handling problems (i.e., cuff damage, tube misplacement, or inappropriate visualization of the glottis, n = 24). In 54 of 56 patients where Airtraq intubation failed, direct laryngoscopy was successful on the first attempt; in the remaining two and in one additional case of failed direct laryngoscopy, the airway was finally secured employing the Fastrach laryngeal mask. There was no correlation between success rates and body mass index, age, indication for airway management, emergency medical service unit, or experience of the physicians.
Conclusions: Based on these results, the use of the Airtraq laryngoscope as a primary airway device cannot be recommended in the prehospital setting without significant clinical experience obtained in the operation room. We conclude that the clinical learning process of the Airtraq laryngoscope is much longer than reported in the anesthesia literature.
| Tags : intubation, airway
05/02/2011
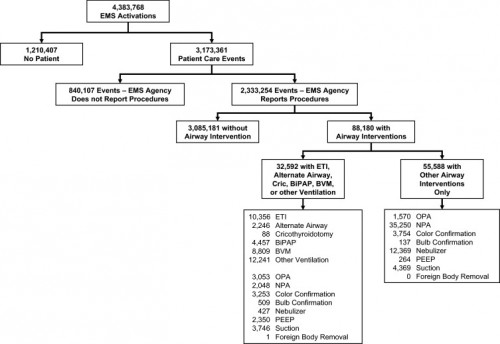
Etude NEMESIS: Out-of-hospital airway management in the United States
Un travail prospectif recensant toutes les manoeuvres de contrôle des voies aériennes aux USA vient d'être publié ( Out-of-hospital airway management in the United States - Wang HE et all. -doi:10.1016/j.resuscitation.2010.12.014). Ce document est intéressant car il confirme que l'intubation est le mode premier de contrôle de la ventilation aux USA suivi par la ventilation manuelle au ballon. Le recours à des disposiifs laryngés ne vient qu'au 4ème rang après la mise en oeuvre de technqiues de ventilation non invasive. L'apprentissage de l'intubation reste donc un objectif essentiel. Les tableaux suivant en présentent les principaux résultats.
Table 1. Prevalence of airway management interventions. Table includes only EMS agencies reporting at least one procedure in the NEMSIS 2008 data set. Percentages reflect portion of 2,333,254 total patient care events. Prevalence estimates not calculated for King LT and foreign body removal due to the small numbers of events. BiPAP = bilevel positive airway pressure. CPAP = continuous positive airway pressure. PEEP = positive end expiratory pressure.
| Intervention | N | (N per 100,000 care events; 95%CI) |
|---|---|---|
| Bag-valve-mask ventilation | 8809 | (378; 370–386) |
| Other ventilation (bag-valve, mechanical, unspecified) | 12,241 | (525; 516–534) |
| Endotracheal intubation | 10,356 | (444; 436–453) |
| Orotracheal intubation | 9130 | (392; 384–400) |
| Nasotracheal intuabtion | 1064 | (46; 43–48) |
| Rapid sequence intubation | 371 | (16; 14–18) |
| Alternate airway | 2246 | (96; 92–100) |
| Combitube | 1521 | (65; 62–69) |
| Esophageal-Obturator Airway (EOA) | 175 | (8; 6–9) |
| Laryngeal Mask Airway | 571 | (24; 23–27) |
| King LT | 4 | (Not calculated) |
| Cricothyroidotomy | 88 | (4; 3–5) |
| BiPAP/CPAP | 4456 | (191; 186–197) |
| Oropharyngeal airway | 4623 | (198; 193–204) |
| Nasopharyngeal airway | 37,298 | (160; 158–161) |
| Colorimetric tube confirmation | 7007 | (300; 294–308) |
| Bulb tube confirmation | 646 | (28; 26–30) |
| Nebulizer | 12,796 | (549; 539–558) |
| PEEP | 2614 | (112; 108–117) |
| Suction | 8115 | (348; 341–356) |
| Foreign body removal | 1 | (Not calculated) |
----------------------------------------------------------------------------------------------------------------------
Table 3. Airway intervention success. Includes only orotracheal, nasotracheal and rapid sequence intubation and alternate airway insertions where procedural success was reported. ETI success was reported for only 8418 of 10,356 ETI.
ETI = endotracheal intubation. US = United States.
a Subgroups do not add up to total because of unknown cardiac arrest status for 5244 cases. Univariable odds ratios presented for selected comparisons only.
----------------------------------------------------------------------------------------------------------------------
Abstract
-----Among 4,383,768 EMS activations, there were 10,356 ETI, 2246 alternate airways, and 88 cricothyroidotomies. ETI success rates were: overall 6482/8418 (77.0%; 95% CI: 76.1–77.9%), cardiac arrest 3494/4482 (78.0%), non-arrest medical 616/846 (72.8%), non-arrest injury 417/505 (82.6%), children <10 years 295/397 (74.3%), children 10–19 years 228/289 (78.9%), adult 5829/7552 (77.2%), and rapid-sequence intubation 289/355 (81.4%). ETI success was success was lowest in the South US census region. Alternate airway success was 1564/1794 (87.2%). Major complications included: bleeding 84 (7.0 per 1000 interventions), vomiting 80 (6.7 per 1000) and esophageal intubation 12 (1.0 per 1000).
Conclusions
In this study characterizing out-of-hospital airway management across the United States, we observed low out-of-hospital ETI success rates. These data may guide national efforts to improve the quality of out-of-hospital airway management.
| Tags : airway, intubation
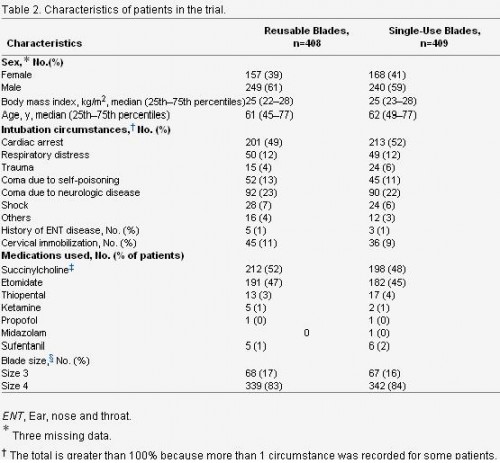
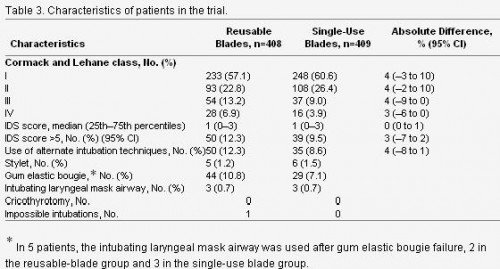
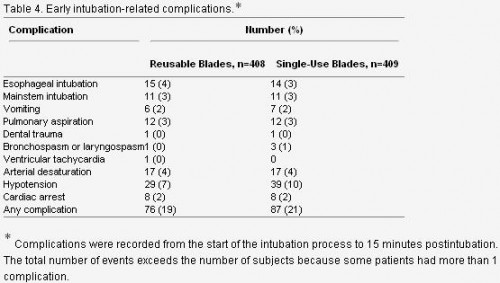
31/12/2010
Intubation préhospitalière: Histoire de lame
Un article d Jabre et all décrit de manière relativement précise le quotidien de l'intubation préhospitalière
Cet article est très intéressant car il permet d'avoir une vision très claire de l'intubation telle qu'elle est réalisée en préhospitalier en France. L'objectif premier était de comparer l'intubation avec lame métallique réutilisable versus non réutilisable et de voir si il y avait une différence en matière d'intubation difficile. Ce n'est pas le cas. Parmi les autres intérêts de ce travail:
-
l'intubation préhospitalière est réalisée essentiellement lors de la prise en charge d' arrêt cardiaque ou de coma. Le contexte traumatique n'est présent que dans 4% des cas. Ce qui ne correspond pas au contexte d'emploi militaire. Le contrôle des voies aériennes ayant pour objectif essentiel le maintien de la liberté des voies aériennes, puis leur protection contre l'inhalation et enfin la possibilité de réaliser une ventilation contrôlée si les autres paramètres techniques sont accessibles (matériel, oxygène, sédation)
2. La taille de la lame utilisée est une taille 4. Le laryngoscope Truphatek Trulite en dotation est approvisionné en taille 3. Ceci a été jugé suffisant par un panel de praticiens, ce d'autant que les lames de tailles 4 sont aussi plus hautes et pas forcément toujours « insérables » dans la cavité buccale en cas de petite ouverture de bouche.
3. Le recours à des techniques alternatives est prévu, ici le masque laryngé d'intubation qui est utilisé de manière exceptionnelle moins de 1% des cas, contrairement au mandrin d'eschmann/Frova.
4. Parmi les complications immédiates, on constate la fréquence des hypotensions près de 10% et des intubations sélectives ou oesophagiennes également près de 10% des cas. Ces taux observés pour des équipes à priori entraînées illustrent bien que l'enjeu majeur de la médicalisation de l'avant dans le contexte actuel est de disposer de personnel ayant une pratique réelle de l'accès aux voies aériennes supérieures.
| Tags : intubation, airway
17/12/2010
Quel laryngoscope ?
Le choix d'un laryngoscope "tactique" n'est pas simple. C'est un compromis entre la modalité choisie de contrôle des voies aériennes (pas d'intubation, coniotomie ou intubation ?), le poids du laryngoscope, la taille de la lame et les qualités optiques attendues.
Vous dispsoez outre de la boite d'intubation standard du laryngoscope trulite de la société truphatek.

Il a été choisi d'approvionner ce laryngoscope en lame fixe de taille 3 qui semble la plus polyvalente. Ce laryngoscope est remarquable de part sa légèreté, la présence d'un manche court et la qualité de la lumière LED fournie. Il est en principe à patient unique.
Pour pallier au problème du choix de la taille de la lame, certains proposent des produits originaux. Ainsi le duoscope de la société PARKER propose deux tailles de lame et un éclairage de grande qualité. sa manipulation est moins aisée car c'est la seconde lame qui sert de manche.
| Tags : intubation, airway
14/12/2010
Abord des voies aériennes:Que font les anglais ?
10 % des blessés évacués nécessite une intubation dont 4.7% avant l'embarquement dans le vecteur d'évacuation. Dans ce travail la limite est que nous ne savons pas ce qui relève de blessés au combat , s'il s'agit de blessés militaires, de la répartition des procédures en fonction du contexte. Dans de telles conditions la prise en charge de patients/blessés en arrêt circulatoire est vaine .
J R Army Med Corps. 2010 Sep;156(3):159-61.
Advanced airway management--a medical emergency response team perspective.
Selly Oak Hospital, Birmingham. aghaldane1@doctors.org.uk
Abstract
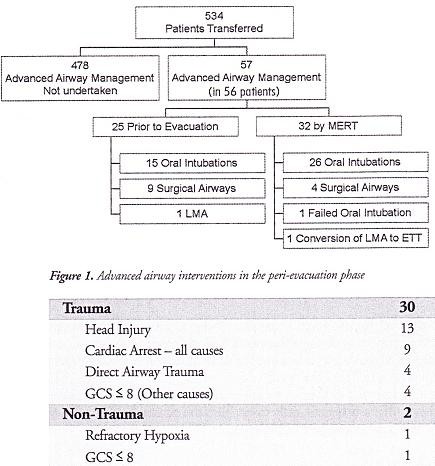
OBJECTIVES: To determine the number of medical emergency response team (MERT) patients undergoing advanced airway management in the peri-evacuation phase and to determine the indications for airway interventions undertaken in flight.
METHODS: This was a retrospective study. Data was collected from patient report and mission debrief forms completed after each MERT mission during Operation HERRICK 10 (April-October 2009). All patients that received advanced airway interventions before or during evacuation were identified.
RESULTS: MERTs were involved in the primary transfer of 534 patients during the period studied, 56 (10.5%) underwent advanced airway management, of which 31 (5.8% of total) were initiated by the MERT in the peri-evacuation phase. Twenty five cases (4.7%) underwent advanced airway management by other pre-hospital providers prior to MERT arrival. Of the 31 advanced airway interventions undertaken in-flight, cardiac arrest was the primary indication in only nine cases.
CONCLUSIONS: The figure of 56 patients requiring advanced airway management is at the higher end of the range expected from the study of historical military data. This may reflect the doctrine of "intelligent tasking", that is sending this physician-led team to the most seriously injured casualties.
Morceaux choisis
1. Intubation et coniotomie sont la base
2. Les indications diffèrent de la médecine préhospitalière civile
"..
The indications for those advanced airway interventions undertaken by the MERT is in keeping with the historical data: Head injury making the biggest group once those inrubated for post-operative resplratory support ie those transferred post-operatively from an FST location rather than direct from the point of wounding are excluded . The majoriry of the cases were trauma (93,5%) with the remaining non-traula causes (6,5%) (table 1); This figure is again similar io the recent US study [11].
.."
| Tags : airway, intubation
06/12/2010
Protection des voies aériennes en urgence: Une synthèse à lire
Protection des voies aériennes en médecine d’urgence
Journal Européen des Urgences (2010) 23, 44—56
X. Combes, P. Jabre, F. Soupizet
Le résumé
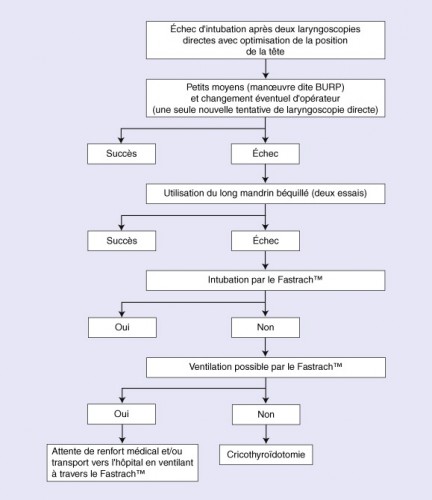
Le contrôle des voies aériennes des patients présentant une détresse vitale est très souvent nécessaire en médecine d’urgence. L’intubation orotrachéale est la technique de référence pour le contrôle des voies aériennes. En dehors du cadre de la réanimation de l’arrêt cardiaque, l’intubation trachéale doit être reéalisée sur un patient sédaté et curarisé selon la technique d’intubation en séquence rapide. L’intubation en urgence est une intubation à risques. L’inhalation pulmonaire et les épisodes de désaturation artérielle profonde sont les deux complications les plus fréquemment associées à ce geste. En médecine d’urgence, l’intubation difficile, rarement prévisible, est plus fréquente qu’au bloc opératoire. La prise en charge de
l’intubation difficile survenant dans le cadre de la médecine d’urgence repose sur l’utilisation de techniques alternatives efficaces. Ces techniques doivent être utilisées selon un algorithme précis. Les mandrins longs béquillés et le masque laryngé d’intubation de type Fastrach TM permettent de résoudre la majorité des cas d’intubation difficile. En cas d’échec de ces deux techniques, une cricothyroïdotomie permettant un abord trachéal direct doit être réalisée chez les patients impossibles à ventiler.
Morceaux choisis
1. On considère qu’un médecin exerçant en SMUR intube annuellement de 15 à 20 patients. Ces chiffres sont à mettre en parallèle avec les données disponibles pour l’activité anesthésique nationale où environ trois millions de patients sont intubés tous les ans au bloc opératoire par des médecins anesthésistes qui intubent chacun en moyenne plus de 300 patients par an.
Un minimum de 40 intubations pour apprendre l'intubation est nécessaire et 20 par an sont nécessaires pour entretenir cette compétence. Cela signifie que la maîtrise de l'abord des VAS est l'objectif principal de la formation continue du médecin d'unité de telle sorte qu'il soit toujours en capacité de faire face à une obstruction des VAS en condition de combat.
2. Les dispositifs laryngés sont probablement plus faciles à insérer pour des opérateurs non médecins que la sonde d’intubation. Les deux problèmes majeurs rencontrés lors de l’utilisation de ce type de matériel sont le risque d’inhalation pulmonaire et le risque de perforation œsophagienne. En effet, ces dispositifs n’assurent pas une protection complète des voies aériennes en cas de vomissement et le risque d’inhalation est alors réel. Plusieurs cas de déchirure du tiers supérieur de l’œsophage ont été rapportés lors de l’utilisation du Combitube®, liés à la surpression régnant dans le ballonnet œsophagien de ce dispositif.
3. En médecine préhospitalière, les circonstances font que très souvent les patients qui nécessitent une intubation en urgence sont pris en charge alors qu’ils sont allongés sur le sol. L’intubation d’un patient au sol présente quelques difficultés particulières. L’opérateur est en effet dans une position le plus souvent pénible pour réaliser son geste et l’intubation est rendue plus difficile. Une technique de positionnement de l’opérateur visant à limiter les difficultés d’intubation a été décrite récemment. Elle consiste à positionner la personne qui va intuber en décubitus latéral. Dans cette position, l’axe visuel de l’opérateur est abaissé et la visualisation glottique, indispensable pour réaliser l’intubation, est rendue beaucoup plus aisée.
4. Parmi les dispositifs laryngés utilisables en préhospitalier, il faut choisir le FASTRACH car son emploi est documenté et qu'il permet l'intubation orotrachéale.
5. La cricothyroïdotomie représente la technique ultime de contrôle des voies aériennes proposée dans le cas où l’intubation et la ventilation du patient restent impossibles malgré l’utilisation des autres techniques alternatives que sont les mandrins et les dispositifs supraglottiques. ......Cette technique est de réalisation très rapide et permet une ventilation efficace dans plus de 95 % des cas.
6. Un algorithme
| Tags : intubation, airway, coniotomie